alternative medicine
As though the UK does not have plenty of organisations promoting so-called alternative medicine (SCAM)! Obviously not – because a new one is about to emerge.
In mid-January, THE COLLEGE OF MEDICINE AND INTEGRATED HEALTH (COMIH) will launch the Integrated Medicine Alliance bringing together the leaders of many complementary health organisations to provide patients, clinicians and policy makers with information on the various complementary modalities, which will be needed in a post COVID-19 world, where:
- patient choice is better respected,
- requirements for evidence of efficacy are more proportionate to the seriousness of the disease and the safety of the intervention,
- and where benefit versus risk are better balanced.
We already saw this in 2020 with the College advocating from the very beginning of the year that people should think about taking Vitamin D, while the National Institute for Clinical Excellence continued to say the evidence was insufficient, but the Secretary of State has now supported it being given to the vulnerable on the basis of the balance between cost, benefit and safety.
Elsewhere we learn more about the Integrated Medicine Alliance (IMA):
The IMA is a group of organisations and individuals that have been brought together for the purpose of encouraging and optimising the best use of complementary therapies alongside conventional healthcare for the benefit of all.
The idea for this group was conceived by Dr Michael Dixon in discussion with colleagues associated with the College of Medicine, and the initial meeting to convene the group was held in February 2019.
The group transitioned through a number of titles before settling on the ‘Integrated Medicine Alliance’ and began work on developing a patient leaflet and a series of information sheets on the key complementary therapies.
It was agreed that in the first instance the IMA should exist under the wing of the College of Medicine, but that in the future it may develop into a formal organisation in its own right, but inevitably maintaining a close relationship with the College of Medicine.
The IMA also offers ‘INFORMATION SHEETS’ on the following modalities:
- Acupuncture
- Alexander Technique
- Aromatherapy
- Herbal Medicine
- Homeopathy
- Hypnotherapy
- Massage
- Naturopathy
- Reflexology
- Reiki
- Tai Chi
- Yoga Therapy
I find those leaflets revealing. They tell us, for example that the Reiki practitioner channels universal energy through their hands to help rebalance each of the body’s energy centres, known as chakras. About homeopathy, we learn that a large corpus of evidence has accumulated which stands the most robust tests of modern science. And about naturopathy, we learn that it includes ozone therapy but is perfectly safe.
Just for the fun of it – and free of charge – let me try to place a few corrections here:
- Reiki healers use their hands to perform what is little more than a party trick.
- The universal energy they claim to direct does not exist.
- The body does not have energy centres.
- Chakras are a figment of imagination.
- The corpus of evidence on homeopathy is by no means large.
- The evidence is flimsy.
- The most robust tests of modern science fail to show that homeopathy is effective beyond placebo.
- Naturopathy is a hotchpotch of treatments most of which are neither natural nor perfectly safe.
One does wonder who writes such drivel for the COMIH, and one shudders to think what else the IMA might be up to.
I was criticised for not referencing this article in a recent post on adverse effects of spinal manipulation. In fact the commentator wrote: Shame on you Prof. Ernst. You get an “E” for effort and I hope you can do better next time. The paper was published in a third-class journal, but I will nevertheless quote the ‘key messages’ from this paper, because they are in many ways remarkable.
- Adverse events from manual therapy are few, mild, and transient. Common AEs include local tenderness, tiredness, and headache. Other moderate and severe adverse events (AEs) are rare, while serious AEs are very rare.
- Serious AEs can include spinal cord injuries with severe neurological consequences and cervical artery dissection (CAD), but the rarity of such events makes the provision of epidemiological evidence challenging.
- Sports-related practice is often time sensitive; thus, the manual therapist needs to be aware of common and rare AEs specifically associated with spinal manipulative therapy (SMT) to fully evaluate the risk-benefit ratio.
The author of this paper is Aleksander Chaibi, PT, DC, PhD who holds several positions in the Norwegian Chiropractors’ Association, and currently holds a position as an expert advisor in the field of biomedical brain research for the Brain Foundation of the Netherlands. I feel that he might benefit from reading some more critical texts on the subject. In fact, I recommend my own 2020 book. Here are a few passages dealing with the safety of SMT:
Relatively minor AEs after SMT are extremely common. Our own systematic review of 2002 found that they occur in approximately half of all patients receiving SMT. A more recent study of 771 Finish patients having chiropractic SMT showed an even higher rate; AEs were reported in 81% of women and 66% of men, and a total of 178 AEs were rated as moderate to severe. Two further studies reported that such AEs occur in 61% and 30% of patients. Local or radiating pain, headache, and tiredness are the most frequent adverse effects…
A 2017 systematic review identified the characteristics of AEs occurring after cervical spinal manipulation or cervical mobilization. A total of 227 cases were found; 66% of them had been treated by chiropractors. Manipulation was reported in 95% of the cases, and neck pain was the most frequent indication for the treatment. Cervical arterial dissection (CAD) was reported in 57%, and 46% had immediate onset symptoms. The authors of this review concluded that there seems to be under-reporting of cases. Further research should focus on a more uniform and complete registration of AEs using standardized terminology…
In 2005, I published a systematic review of ophthalmic AEs after SMT. At the time, there were 14 published case reports. Clinical symptoms and signs included:
- central retinal artery occlusion,
- nystagmus,
- Wallenberg syndrome,
- ptosis,
- loss of vision,
- ophthalmoplegia,
- diplopia,
- Horner’s syndrome…
Vascular accidents are the most frequent serious AEs after chiropractic SMT, but they are certainly not the only complications that have been reported. Other AEs include:
- atlantoaxial dislocation,
- cauda equina syndrome,
- cervical radiculopathy,
- diaphragmatic paralysis,
- disrupted fracture healing,
- dural sleeve injury,
- haematoma,
- haematothorax,
- haemorrhagic cysts,
- muscle abscess,
- muscle abscess,
- myelopathy,
- neurologic compromise,
- oesophageal rupture
- pneumothorax,
- pseudoaneurysm,
- soft tissue trauma,
- spinal cord injury,
- vertebral disc herniation,
- vertebral fracture…
In 2010, I reviewed all the reports of deaths after chiropractic treatments published in the medical literature. My article covered 26 fatalities but it is important to stress that many more might have remained unpublished. The cause usually was a vascular accident involving the dissection of a vertebral artery (see above). The review also makes the following important points:
- … numerous deaths have been associated with chiropractic. Usually high-velocity, short-lever thrusts of the upper spine with rotation are implicated. They are believed to cause vertebral arterial dissection in predisposed individuals which, in turn, can lead to a chain of events including stroke and death. Many chiropractors claim that, because arterial dissection can also occur spontaneously, causality between the chiropractic intervention and arterial dissection is not proven. However, when carefully evaluating the known facts, one does arrive at the conclusion that causality is at least likely. Even if it were merely a remote possibility, the precautionary principle in healthcare would mean that neck manipulations should be considered unsafe until proven otherwise. Moreover, there is no good evidence for assuming that neck manipulation is an effective therapy for any medical condition. Thus, the risk-benefit balance for chiropractic neck manipulation fails to be positive.
- Reliable estimates of the frequency of vascular accidents are prevented by the fact that underreporting is known to be substantial. In a survey of UK neurologists, for instance, under-reporting of serious complications was 100%. Those cases which are published often turn out to be incomplete. Of 40 case reports of serious adverse effects associated with spinal manipulation, nine failed to provide any information about the clinical outcome. Incomplete reporting of outcomes might therefore further increase the true number of fatalities.
- This review is focussed on deaths after chiropractic, yet neck manipulations are, of course, used by other healthcare professionals as well. The reason for this focus is simple: chiropractors are more frequently associated with serious manipulation-related adverse effects than osteopaths, physiotherapists, doctors or other professionals. Of the 40 cases of serious adverse effects mentioned above, 28 can be traced back to a chiropractor and none to a osteopath. A review of complications after spinal manipulations by any type of healthcare professional included three deaths related to osteopaths, nine to medical practitioners, none to a physiotherapist, one to a naturopath and 17 to chiropractors. This article also summarised a total of 265 vascular accidents of which 142 were linked to chiropractors. Another review of complications after neck manipulations published by 1997 included 177 vascular accidents, 32 of which were fatal. The vast majority of these cases were associated with chiropractic and none with physiotherapy. The most obvious explanation for the dominance of chiropractic is that chiropractors routinely employ high-velocity, short-lever thrusts on the upper spine with a rotational element, while the other healthcare professionals use them much more sparingly.
Another review summarised published cases of injuries associated with cervical manipulation in China. A total of 156 cases were found. They included the following problems:
- syncope (45 cases),
- mild spinal cord injury or compression (34 cases),
- nerve root injury (24 cases),
- ineffective treatment/symptom increased (11 cases),
- cervical spine fracture (11 cases),
- dislocation or semi-luxation (6 cases),
- soft tissue injury (3 cases),
- serious accident (22 cases) including paralysis, deaths and cerebrovascular accidents.
Manipulation including rotation was involved in 42% of all cases. In total, 5 patients died…
To sum up … chiropractic SMT can cause a wide range of very serious complications which occasionally can even be fatal. As there is no AE reporting system of such events, we nobody can be sure how frequently they occur.
[references from my text can be found in the book]The New Year is a good occasion to thank all commentators for their participation. Your contributions are essential and much appreciated. Sadly, the tone used by several of us (me included) has deteriorated in recent months. Therefore, I would like to take this opportunity to update the rules for contributing to this blog and let you know that I plan to enforce them.
I do like clearly and concisely expressed views and am often as outspoken as politeness allows. I hope that commentators will do the same, no matter whether they agree or disagree with me. However, I will now insist that we all observe a minimum of courtesy towards each other.
Twelve simple rules must be observed when commenting on my blog.
- All posts should be in understandable English; with rare exceptions, I will not post comments that I find incomprehensible.
- Libellous statements will not be posted.
- Personal insults will not be posted.
- People who keep insulting others will be permanently banned from posting on my blog.
- Comments must be on-topic.
- Nothing published here must be taken as medical advice.
- All my statements are comments in a legal sense.
- Conflicts of interest should always be disclosed.
- I will stop discussions on any particular topic if I feel that enough has been said and things are getting boring or repetitive.
- I will not post comments which are overtly nonsensical.
- I will prevent commentators from monopolizing the discussion.
- Please use the same name you’ve used before when commenting — it doesn’t have to be your real name, but it helps others who are trying to follow the discussions.
Please do let me know if you feel that I or someone else has broken any of these rules.

2020 was certainly a difficult year (please note, I am trying a British understatement here). From the point of view of running this blog, it was sad to lose James Randi (1928 – 2020) who had been the hero of so many sceptics worldwide, and to learn of the passing of Frank Odds (1945-2020) who was a regular, thoughtful commentator here.
Reviewing the topics we tackled, I could mention dozens. But let me pick out just a few themes that I feel might be important.
HOMEOPATHY
Homeopathy continued to have a rough time; the German medical profession has finally realised that homeopathy is treatment with placebos and the German Green Party no longer backs homeopathy. In India, the Supreme Court ruled: Homeopathy must not be sold as a cure of Covid-19, and in the US improved labeling on homeopathic products were introduced. To make matters worse I issued A CHALLENGE FOR ALL HOMEOPATHS OF THE WORLD.
NOVEL SCAMs
On this blog, I like to write about new so-called alternative medicines (SCAMs) that I come accross. Blood letting is not exactly new, but Oh look! Bloodletting is back! Many other ‘innovations’ were equally noteworthy. Here is merely a very short selection of modalities that were new to me:
- Hydrogen-rich water: the new wonder drug?
- Dr. Robin A. Bernhoft and his ‘Bioidentical Hormone Replacement Therapy’ (BHRT)
- The ‘OBERON’: revolutionary invention or dangerous con?
- Qi technology: “scientifically proven to provide EMF Protection” (edzardernst.com)
- ‘DRX9000’ for back pain: a nice little earner for chiropractors and other back pain quacks
- Vibroacoustic Sound Therapy: introducing the ‘healthy vibration of cells’ into the body
- Lakhovsky’s oscillator, the ‘cure all’ that the world forgot
COVID-19
Unquestionably the BIG subject (not just) in SCAM was – is and will be for a while – the pandemic. It prompted quacks of any type to crawl out of the woodwork misleading the public about their offerings. On 24 January, I wrote for the first time about it: Coronavirus epidemic: Why don’t they ask the homeopaths for help? Thereafter, every charlatan seemed to jump on the COVID bandwaggon, even Trump: Trump seems to think that UV might be the answer to the corona-pandemic – could he mean “ultraviolet blood irradiation”? It became difficult to decide who was making a greater fool of themselves, Trump or the homeopaths (Is this the crown of the Corona-idiocy? Nosodes In Prevention And Management Of COVID -19). Few SCAM entrepreneurs (Eight new products aimed at mitigating COVID-19. But do they really work?) were able to resist the opportunity. Snakeoil salesmen were out in force and view COVID-19 as an ‘opportunity’. It is impossible to calculate what impact all this COVID-quackery had, but I fear that many people lost their lives at least in part because of it.
VACCINATION
The unavoidable consequence of the pandemic was that the anti-vaxx brigade sensed that their moment had arrived. Ex-doctor Andrew Wakefield: “Better to die as a free man than live as a slave” (and get vaccinated against Covid-19). Again the ‘charlatan in chief’ made his influence felt through the ‘Trump-Effect’ on vaccination attitudes. Unsurprisingly, the UK ‘Society of Homeopath’ turned out to be an anti-vaxx hub that endangers public health. And where there is anti-vaxx, chiropractors are seldom far: Ever wondered why so many chiropractors are profoundly anti-vax?. All this could be just amusing, but sadly it has the potential to cost lives through Vaccine hesitancy due to so-called alternative medicine (SCAM).
ETHICS
I happen to believe that ethics in SCAM are an important, yet much neglected topic. It is easy to understand why this should be so: adhering to the rules of medical ethics would all but put an end to SCAM. This applies to chiropractic (The lack of chiropractic ethics: “valid consent was not obtained in a single case”), to homeopaths (Ethical homeopathy) and to most other SCAM professions. If I had a wish for the next year(s), it would be that funding agencies focus on research into the many ethical problems posed by the current popularity of SCAM.
CONCLUSION
If I had another wish, it would be that critical thinking becomes a key subject in schools, universities and adult education. Why do so many people make irrational choices? One answer to this question is, because we fail to give this subject the importance it demands. The lack of critical thinking is the reason why we elect leaders who are compulsory lyers, make wrong choices about healthcare, and continue to destroy the planet as though there is no tomorrow. It is high time that we, as a society, realise how fundamentally important critical thinking truly is.
OUTLOOK
Yes, 2020 was difficult: Brexit, COVID-19, anti-vaxx, etc. But it was not all bad (certainly not for me personally), and there is good reason for hope: the globally malign influence of Trump is about to disappear, and we now have several effective vaccines. Common sense, decency and science might triumph after all.
HEALTHY NEW YEAR EVERYONE!
There are of course 2 types of osteopaths: the US osteopaths who are very close to real doctors, and the osteopaths from all other countries who are practitioners of so-called alternative medicine. This post, as all my posts on this subject, is about the latter category.
I was alerted to a paper entitled ‘Osteopathy under scrutiny’. It goes without saying that I thought it relevant; after all, scrutinising so-called altermative medicine (SCAM), such as osteopathy is one of the aims of this blog. The article itself is in German, but it has an English abstract:
Osteopathic medicine is a medical specialty that enjoys a high level of recognition and increasing popularity among patients. High-quality education and training are essential to ensure good and safe patient treatment. At a superficial glance, osteopathy could be misunderstood as a myth; accurately considered, osteopathic medicine is grounded in medical and scientific knowledge and solid theoretical and practical training. Scientific advances increasingly confirm the empirical experience of osteopathy. Although more studies on its efficacy could be conducted, there is sufficient evidence for a reasonable application of osteopathy. Current scientific studies show how a manually executed osteopathic intervention can induce tissue and even cellular reactions. Because the body actively responds to environmental stimuli, osteopathic treatment is considered an active therapy. Osteopathic treatment is individually applied and patients are seen as an integrated entity. Because of its typical systemic view and scientific interpretation, osteopathic medicine is excellently suited for interdisciplinary cooperation. Further work on external evidence of osteopathy is being conducted, but there is enough knowledge from the other pillars of evidence-based medicine (EBM) to support the application of osteopathic treatment. Implementing careful, manual osteopathic examination and treatment has the potential to cut healthcare costs. To ensure quality, osteopathic societies should be intimately involved and integrated in the regulation of the education, training, and practice of osteopathic medicine.
This does not sound as though the authors know what scutiny is. In fact, the abstract reads like a white-wash of quackery. Why might this be so? To answer this question, we need to look no further than to the ‘conflicts of interest’ where the authors state (my translation): K. Dräger and R. Heller state that, in addition to their activities as further education officers/lecturers for osteopathy (Deutsche Ärztegesellschaft für Osteopathie e. V. (DÄGO) and the German Society for Osteopathic Medicine e. V. (DGOM)) there are no conflicts of interest.
But, to tell you the truth, the article itself is worse, much worse that the abstract. Allow me to show you a few quotes (all my [sometimes free] translations).
- Osteopathic medicine is a therapeutic method based on the scientific findings from medical research.
- [The osteopath makes] diagnostic and therapeutic movements with the hands for evaluating limitations of movement. Thereby, a blocked joint as well as a reduced hydrodynamic or vessel perfusion can be identified.
- The indications of osteopathy are comparable to those of general medicine. Osteopathy can be employed from the birth of a baby up to the palliative care of a dying patient.
- Biostatisticians have recognised the weaknesses of RCTs and meta-analyses, as they merely compare mean values of therapeutic effects, and experts advocate a further evidence level in which statictical correlation is abandonnened in favour of individual causality and definition of cause.
- In ostopathy, the weight of our clinical experience is more important that external evidence.
- Research of osteopathic medicine … the classic cause/effect evaluation cannot apply (in support of this statement, the authors cite a ‘letter to the editor‘ from 1904; I looked it up and found that it does in no way substantiate this claim)
- Findings from anatomy, embryology, physiology, biochemistry and biomechanics which, as natural sciences, have an inherent evidence, strengthen in many ways the plausibility of osteopathy.
- Even if the statistical proof of the effectiveness of neurocranial techniques has so far been delivered only in part, basic research demonstrates that the effects of traction or compression of bogily tissue causes cellular reactions and regulatory processes.
What to make of such statements? And what to think of the fact that nowhere in the entire paper even a hint of ‘scrutiny’ can be detected? I don’t know about you, but for me this paper reflects very badly on both the authors and on osteopathy as a whole. If you ask me, it is an odd mixture of cherry-picking the evidence, misunderstanding science, wishful thinking and pure, unadulterated bullshit.
You urgently need to book into a course of critical thinking, guys!
Thirty years ago, I had just been appointed chair of PHYSICAL MEDICINE AND REHABILITATION at the University of Vienna and was about to move – as the first clinical department – into the brand new AKH (General Hospital) of Vienna thus gradually enlarging the team I had taken over from about 20 to 120 co-workers. During this period, I found little time to do original research; however, I did manage to finally write up and publish a study, we had conducted several years before while I was still in Munich. As it is (almost) on the subject of so-called alternative medicine (SCAM), and as it relates to the prevention of a viral infection, I think it might be of interest to give it another outing.
Here is its abstract:
The high morbidity of common colds means that their economic importance is considerable, with colds causing more loss of productivity than any other infection. As no effective prophylaxis is available, this trial was to test the hypothesis that sauna bathing can reduce the incidence of common colds. Twenty-five volunteers were submitted to sauna bathing, with 25 controls abstaining from this or comparable procedures. In both groups the frequency, duration and severity of common colds were recorded for six months. There were significantly fewer episodes of common cold in the sauna group. This was found particularly during the last three months of the study period when the incidence was roughly halved compared to controls. The mean duration and average severity of common colds did not differ significantly between the groups. It is concluded that regular sauna bathing probably reduces the incidence of common colds, but further studies are needed to prove this.
In the discussion section of the paper, we stated the following:
Preventive methods with comparable efficacy have not been described in the literature (2, 12). Vitamin C is of doubtful value (7, 15, 16); vaccination is not feasible since far too many virus types exist (2, 17); virucidal kerchiefs are effective (8, 18) but not available commercially and protect only the environment of a common cold sufferer rather than the sufferer him-/herself.
I believe most of this is still true today (but I might be wrong, as I did not keep up with this particular line of research). Re-reading the paper, I find that our trial was far from optimal:
- we had to conduct it with zero funding,
- it was small,
- it was not randomised,
- it lacked objective endpoints.
Anyway, sauna bathing is most agreeable, and I can recommend it just for this reason. However, I would doubt that public saunas are a good idea during the present health crisis.
Please, stay safe!
We are living in difficult times, and few things are more difficult than spending the holidays in confinement alone or (possibly worse) with close family. If you do, you need all the help you can get. Here are a few homeopathic remedies (all available from Her Majesty’s homeopathic pharmacy) which, according to the ‘like cures like’ (LCL) axiom of homeopathy, might come in handy:
- Aspirin (Acetylsalicylic Acid) Aspirin is effective for many conditions, for instance, headache. So, taking a high potency homeopathic Aspirin should, according to LCL, give you a headache. It might therefore be helpful for being excused from spending yet another afternoon watching TV with your mother in law. Alternatively, you could, of course, smuggle some drops in her food and solve your problem in this somewhat unethical way.
- Latex vulcani (Latex (condom) In case you want to use the confinement to start a family, this remedy should make it easier to conceive.
- Penicillinum Penicillin kills bacteria, as we all know. Taking homeopathic Penicillium would therefore make you catch a bacterial infection. This could be a welcome change from all this endless talk about viral disease, I am sure.
- Semen humanum In case you do not want to get pregnant, this seems to be the remedy of choice for you.
- Sunlight Blue (Prismatic blue from sunlight) Sunlight Green (Prismatic green from sunlight) Sunlight Orange (Prismatic orange from sunlight) Sunlight Purple (Prismatic purple from sunlight) Sunlight Red (Prismatic Red from Sunlight) Sunlight Yellow (Prismatic yellow from sunlight) Lots of people swear by vitamin D to protect themselves against COVID-19. It is easy to over-dose on this vitamin, and many people will therefore be now suffering from a vitamin D hypervitaminosis with potentially dangerous consequences. If you are worried, I recommend you take all the above remedies. As sunlight normally generates vitamin D in your body, these homeopathics should stop any hypervitaminosis D in its tracks.
- Umbilicus humanus (Umbilical Cord Humanus) Many people have to spend this holiday without their mother. If that affects you deeply, try this remedy.
- Vitamin D (Vitamin D2 + Vitamin D3) Vitamin D2 (Ergocalciferol) Vitamin D3 (Cholecalciferol) If you don’t want to take the sunlight remedies mentioned above for your vitamin D hypervitaminosis (remember: too strong sunlight can cause skin cancer!), try the more direct method of administering homeopathic vitamin D.
So, do take good care of yourselves, stay healthy, don’t over-dose the brandy butter, port, or anything else, and
MERRY CHRISTMAS!
The Indian Supreme Court has ruled this week that homeopathic, ayurvedic and unani practitioners must not prescribe their respective so-called alternative medicines (SCAMs) as a cure for Covid-19.

Specifically, the judges noted that, according to the guidelines issued by the Ayush ministry in March, homeopaths are permitted only to prescribe certain homeopathic medicines as “…preventive, prophylactic, symptom management of Covid-19-like illnesses and add-on interventions to the conventional care”, but not as a cure.
“The high court, however, is right in its observation that no medical practitioner can claim that it can cure Covid-19. There is no such claim in other therapy including allopathy. The high court is right in observing that no claim for cure can be made in homeopathy. Homeopathy is contemplated to be used in preventing and mitigating Covid-19 as is reflected by the advisory and guidelines issued by the ministry of Ayush…,” Justices Ashok Bhushan, R. Subhash Reddy and M.R. Shah stated.
The Supreme Court passed the ruling while disposing of an appeal filed by the Kerala-based Dr AKB Sadbhavana Mission School of Homeo Pharmacy that was aggrieved by Kerala High Court’s direction on August 21 for action against homeopaths who claim cure in homeopathy for Covid-19 patients. However, the Supreme Court judgment established that the Ayush ministry guidelines clearly refer to certain homeopathy medicines as preventive, prophalytic and add-on interventions to the conventional therapy. “The above guidelines refer to homeopathy medicines as medicines for prophylaxis, amelioration and mitigation. The guidelines, however, specifically provide that ‘the prescription has to be given only by institutionally qualified practitioners’,” the bench said.
According to the court, homeopathic practitioners are bound by rules from prescribing medicines as cure for Covid-19. “When statutory regulations themselves prohibit advertisement, there is no occasion for homeopathic medical practitioners to advertise that they are competent to cure Covid-19 disease. When the scientists of the entire world are engaged in research to find out proper medicine/vaccine for Covid-19, there is no occasion for making any observation as contained in the paragraph with regard to homeopathic medical practitioners,the judges stated.
_________________________________
Meanwhile, the number of COVID-19 cases in India exceeds 10 million, and that of COVID-related death is almost 150 000. If you ask me, promoters of homeopathic remedies should not be allowed to advertise or sell their placebos pretending they are effective for any purpose in connection with COVID-19 (or any other serious disease for that matter) – not as a curative therapy, not for prevention, and not as a symptomatic treatment either.
Who does not like a nice fragrance?
Who would object to aromatherapy?
Nobody, I suppose.
But, if its called THERAPY, we surely must ask whether it is therapeutic. And is aromatherapy therapeutic? Let’s see:
This randomized, placebo-controlled clinical trial tested whether patients with post-dural puncture headache (PDPH) caused by spinal anesthesia would benefit from aromatherapy. A total od 50 patients received 15-minute inhalations of either lavender oil or liquid paraffin as placebo. The severity of headache was scored before (baseline) and after the intervention – immediately, 30, 60, 90, and 120 minutes after – using a visual analog scale. In addition, the dosage and frequency of the pain killers as well as adverse effects of the intervention were recorded.
Both groups showed a reduction in headache scores post intervention. However, the headache scores between the groups was significantly different immediately after the intervention in favor of lavender oil (difference: 1.60 ± 0.63, P = .015). Furthermore, it was observed that the mean changes of the headache scores compared to the baseline were significant at each time interval in favor of the placebo group (P < .05), except immediately after the intervention. No significant difference was observed in Diclofenac intake between groups (P = .440), and no adverse effects were noted.
The authors concluded that aromatherapy with lavender oil was observed to reduce the severity of PDPH only immediately after the intervention, while only minimal effects were observed at successive time intervals. However, it is noted that the study was likely underpowered and further studies are recommended to better understand the effects of lavender oil on PDPH and compare its effects to other herbal products or pharmacological agents commonly used for managing headaches.
I find it laudable that some researchers conduct clinical trials even of so-called alternative medicines (SCAMs) which many of us might view as trivial. I find it more laudable that they try to do this rigorously by adding a placebo control group to the study. And I would find it even more laudable, if they did this adequately.
Considering parafin oil to be a placebo in a study of lavender oil inhalation can hardly be called adequate. Placebos are used in clinical trials mostly to account for the expectation of patients. This means that, whenever possible, patients need to be blinded to the group aloocation and the placebo must be indistinguishable from the verum. In the present trial, the patients could obviously tell the difference between the smell of lavender and the absence of any smell in the control group. Thus, their expectation could easily suffice to bring about the findings observed in the study. This means that the trial does not neccessarily demonstrate the effects of armoatherapy, but might (and most probably does) merely show the power of expectation.
How can one design such a trial more rigorously? you will ask.
There are several options. For instance, for the control group, one could use an artificial fragrance not made from natural lavender. Alternatively, one could include only patients who are unfamiliar with the smell of lavender and use a similaryly pleasant fragrance from a different plant as the control intervention.
As it stands, the study – even though aimed at testing the hypothesis that aromatherpy with lavender has specific effects on pain – tells us next to nothing.
… except, of course that it is always worth thinking very carefully about the adequate way to conduct a clinical trial.
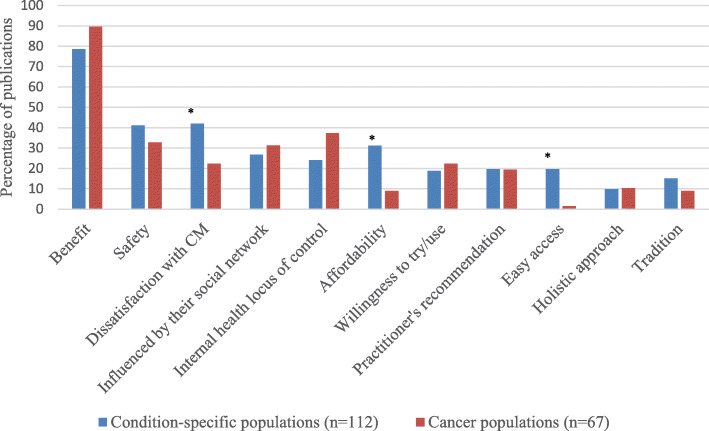
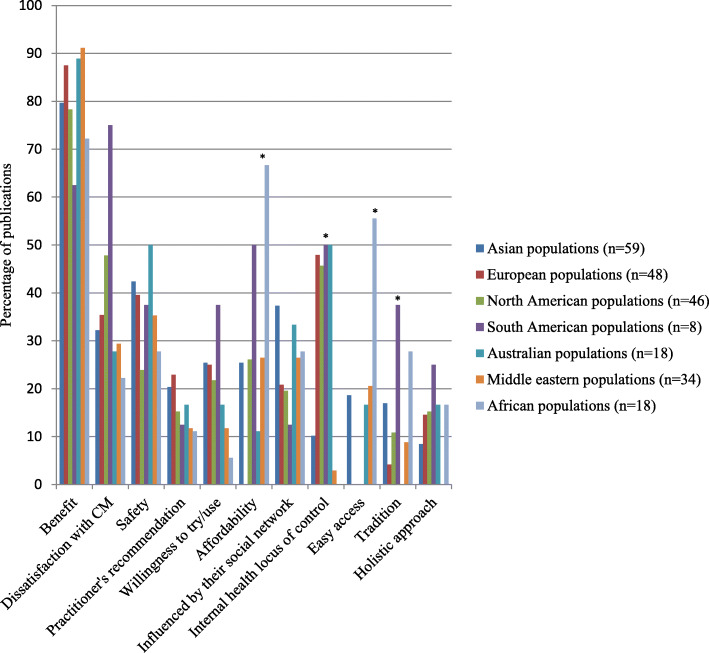
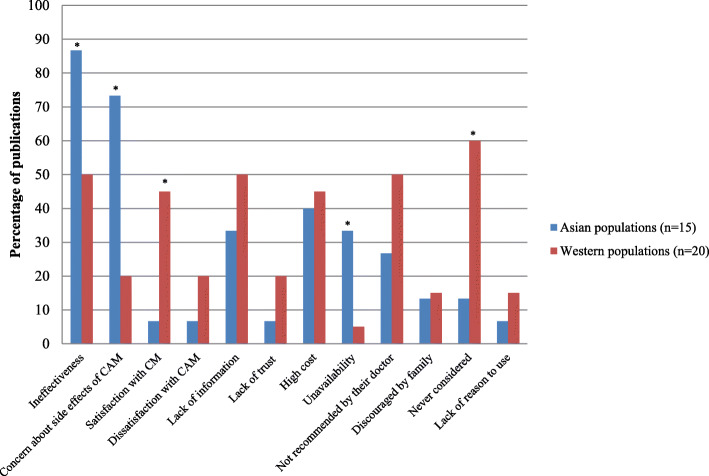
The authors of this review wanted to determine similarities and differences in the reasons for using or not using so-called alternative medicine (SCAM) amongst general and condition-specific populations, and amongst populations in each region of the globe.
Quantitative or qualitative original articles in English, published between 2003 and 2018 were reviewed. Conference proceedings, pilot studies, protocols, letters, and reviews were excluded. Papers were appraised using valid tools and a ‘risk of bias’ assessment was also performed. Thematic analysis was conducted. Reasons were coded in each paper, then codes were grouped into categories. If several categories reported similar reasons, these were combined into a theme. Themes were then analysed using χ2 tests to identify the main factors related to reasons for CAM usage.
A total of 231 publications were included. Reasons for SCAM use amongst general and condition-specific populations were similar. The top three reasons were:
- (1) having an expectation of benefits of SCAM (84% of publications),
- (2) dissatisfaction with conventional medicine (37%),
- (3) the perceived safety of SCAM (37%).
Internal health locus of control as an influencing factor was more likely to be reported in Western populations, whereas the social networks was a common factor amongst Asian populations (p < 0.05). Affordability, easy access to SCAM and tradition were significant factors amongst African populations (p < 0.05). Negative attitudes towards SCAM and satisfaction with conventional medicine were the main reasons for non-use (p < 0.05).
The authors concluded that dissatisfaction with conventional medicine and positive attitudes toward SCAM, motivate people to use SCAM. In contrast, satisfaction with conventional medicine and negative attitudes towards SCAM are the main reasons for non-use.
At this point, I thought: so what? This is all very obvious and does not necessitate an extensive review of the published literature. What it actually shows is that the realm of SCAM is obsessed with conducting largely useless surveys, a phenomenon, I once called ‘survey mania‘. But a closer look at the review does reveal some potentially interesting findings.
In less developed parts of the world, like Africa, SCAM use seems to be determined by affordability, accessibility and tradition. This makes sense and ties in with my impression that consumers in such countries would give up SCAM as soon as they can afford proper medicine.
This notion seems to be further supported by the reasons for not using SCAM. Asian consumers claim overwhelmingly that this is because they consider SCAM ineffective and unsafe.
In our review of 2011 (not cited in the new review), we looked at some of the issues from a slightly different angle and evaluated the expectations of SCAM users. Seventy-three articles met our inclusion criteria of our review. A wide range of expectations emerged. In order of prevalence, they included:
- the hope to influence the natural history of the disease;
- the desire to prevent disease and promote health/general well-being;
- the hope of fewer side effects;
- the wish to be in control over one’s health;
- the hope for symptom relief;
- the ambition to boost the immune system;
- the hope to receive emotional support;
- the wish to receive holistic care;
- the hope to improve quality of life;
- the expectation to relief of side effects of conventional medicine;
- the desire for a good therapeutic relationship;
- the hope to obtain information;
- the hope of coping better with illness;
- the expectation of supporting the natural healing process;
- the availability of SCAM.
All of these aspects, issues and notions might be interesting, even fascinating to some, but we should not forget three important caveats:
- Firstly, SCAM is such a diverse area that any of the above generalisations are highly problematic; the reasons and expectations of someone trying acupuncture may be entirely different from those of someone using homeopathy, for instance.
- Secondly (and more importantly), the ‘survey mania’ of SCAM researchers has not generated the most reliable data; in fact, most of the papers are hardly worth the paper they were printed on.
- Thirdly (and even more importantly, in my view), why should any of this matter? We have known about some of these issues for at least 3 decades. Has this line of research changed anything? Has it prevented consumers getting exploited by scrupulous SCAM entrepreneurs? Has it made consumers, politicians or anyone else more aware of the risks associated with SCAM? Has it saved many lives? I doubt it!