Monthly Archives: November 2018
After 25 years of full-time research into alternative medicine, I thought that I have seen it all. But I was wrong! Here is an article that surpasses every irresponsible stupidity I can remember. It is entitled ‘Ginger is the monumentally superior alternative to chemotherapy‘:
Let’s say that your doctor has given you a cancer diagnosis. Let’s revisit animal wisdom. If a squirrel was looking over a tasty morsel of ginger on one side, or a vial full of Mehotrexate, Danorubicin or Tioguanine on the other, what would that intelligent squirrel choose? The answer is obvious. And it’s the right answer, because ginger roots, after being dried and cooked, manifest an ingredient called 6-shogaol.
This naturally occurring element is up to 10,000 times more effective at killing cancer cells than those vials of destructive drugs, reports David Guiterrez from Natural News, who states that “researchers found that 6-shogaol is active against cancer stem cells at concentrations that are harmless to healthy cells. This is dramatically different from conventional chemotherapy, which has serious side effects largely because it kills healthy as well as cancerous cells.”
END OF QUOTE
As David Guiterrez from Natural News might not be the most reliable of sources, I did a bit of searching for evidence. This is what I found:
A study examining the efficacy of ginger, as an adjuvant drug to standard antiemetic therapy, in ameliorating acute and delayed CINV in patients with lung cancer receiving cisplatin-based regimens. It concluded that as an adjuvant drug to standard antiemetic therapy, ginger had no additional efficacy in ameliorating CINV in patients with lung cancer receiving cisplatin-based regimens.
A randomized, double-blind, placebo-controlled, multicenter study in patients planned to receive ≥2 chemotherapy cycles with high dose (>50 mg/m2) cisplatin. Patients received ginger 160 mg/day (with standardized dose of bioactive compounds) or placebo in addition to the standard antiemetic prophylaxis for CINV, starting from the day after cisplatin administration. The authors found that in patients treated with high-dose cisplatin, the daily addition of ginger, even if safe, did not result in a protective effect on CINV.
Yes, there are also a few trials to suggest that ginger is effective for reducing nausea and vomiting after chemotherapy, but by and large they are older and less rigorous. And anyway, this is besides the point. The question here is not whether there is good evidence to show that ginger is helpful against chemo-induced nausea; the question is whether Ginger is clinically effective in ‘killing cancer cells’. And the answer is an emphatic
NO!!!
And this means the above-quoted article irresponsible, unethical, perhaps even criminal to the extreme. I shudder to think how many cancer patients have read it and consequently given up their conventional treatments opting for Ginger instead.
Many people seem to be amazed at my continued activities (e. g. blog, books, lectures, interviews) aimed at telling the truth about homeopathy and other alternative modalities. They ask themselves: why does he do it? And sometimes I ask myself the same question. I certainly don’t do it because I receive any money for my work (as many of my critics have assumed in the past).
So, why?
Let me briefly offer just 7 of the most obvious reasons why I feel it is important to tell the truth about homeopathy and similar treatments:
1. The truth is invaluable
I probably do not need to explain this at all. For any responsible person the truth has an intrinsic value that cannot be doubted. In our book, we conclude that “the truth-violating nature of CAM renders it immoral in both theory and practice.”
2. Untruths make a mockery of EBM
If we accept that, in the realm of alternative medicine, it is permissible to apply a different standard than in evidence-based medicine (EBM), we make a mockery of EBM. Double standards are hugely counter-productive and not in the interest of patients.
3. The truth promotes rationality
If the proponents of a modality such as homeopathy promote concepts that fly in the face of science, they undermine rational thinking. Believing in a vital force or energy is just one of many examples for this phenomenon. Undermining rationality can have negative effects far beyond healthcare and reminds me of Voltaire’s bon mot: “Those who make you believe in absurdities can make you commit atrocities.”
4. It is ethical
Healthcare have the ethical duty to work towards patients receiving the best treatments available. If a therapy like homeopathy fails to be demonstrably effective, it cannot possibly fall into this category. Therefore, responsible healthcare professionals must help to improve healthcare by disclosing the evidence against homeopathy.
5. It might save money
The money spent on homeopathy and other ineffective alternative treatments is considerable. Disclosing the fact that they are not effective will help stopping people to waste their money on them. Telling the truth about homeopathy and similarly ineffective therapies would therefore save funds that can be used more efficiently elsewhere.
6. It might save lives
Because they usually are free of active molecules, homeopathic remedies are often seen as a safe treatments. However, homeopathy can nevertheless harm and even kill patients, if they use it as an alternative medicines in cases of severe illness. It follows that telling the truth about homeopathy’s ineffectiveness can save lives.
7. It could counter-balance the multiple lies that are being told.
We all have seen the multitude of untruths that are being told about the value of homeopathy (if you haven’t, you ought to read SCAM). The multitude of falsehoods seriously misleads many consumers into believing that homeopathy is a valuable therapeutic option for many conditions. I feel strongly that it is my moral duty as an independent expert to counter-balance this plethora of lies in order to minimise the harm it is doing.
I have just been in Sao Paulo to give a lecture at the opening of a new university institute, ‘Question of Science‘. Under the leadership of Natalia Pasternak, the institute will promote scepticism in Brazil, particularly in the area of alternative medicine. Brazil currently has no less than 29 types of alternative medicine paid for with public money, and even homeopathy is officially being recognised and taught at all Brazilian medical schools.
But the most peculiar case of Brazilian quackery must surely be phosphoethanolamine. Gilberto Chierice, a Chemistry Professor at the University of São Paulo, used resources from a campus laboratory to unofficially manufacture, distribute, and promote the chemical to cancer patients claiming that it was a cheap cure for all cancers without side-effects. Remarkably, this was in the total absence of through clinical testing. In September 2015, university administrators therefore began preventing him from continuing with this practice. However, in October 2015, several courts in Brazil ruled in favour of plaintiffs who wanted the compound to remain available. In an unusual move of defence of common sense, a state court overturned the lower courts’ decision a month later, and the secretary for Brazil’s science and technology ministry promised to fund further research on the compound. In 2016, a law was passed in Brazil allowing the sale of synthetic phosphorylethanolamine for cancer treatment. Due to opposition from the Brazilian Medical Association, the Brazilian Society of Clinical Oncology, and the regulatory agency ANVISA, the country’s Supreme Court then suspended the law. I was told that a stepwise plan of clinical testing had been implemented. As the drug even failed to pass the most preliminary tests, the program had to be aborted.
This story seems like a re-play of many similar tales of bogus cancer cures of the past. They all seem to follow a similar pattern:
- Someone dreams up a ‘cure’ for all cancers that is cheap and free of side-effects.
- This appeals to many desperate cancer patients who are fighting for their lives.
- It also attracts several entrepreneurs who are hoping to make a fast buck.
- The story is picked up by the press and consequently a sizable grass-roots movement of support emerges.
- Populist politicians jump on the vote-winning band-waggon.
- The experts caution that the bogus cancer ‘cure’ is devoid of evidence and might put patients’ lives at risk.
- The legislators get involved.
- Law suits start left, right and centre.
- Eventually, the cancer ‘cure’ is scientifically tested and confirmed to be bogus.
- Eventually, the law rules against the bogus ‘cure’.
- A conspiracy theory emerges stating that the cancer ‘cure’ was unjustly suppressed to protect the interests of Big Pharma.
- A few years later, the subject re-surfaces and the whole cycle starts from the beginning.
Such stories remind us that fighting bogus claims is hugely important, even if it does not always succeed or turns out to be merely an exercise of damage limitation. Every life saved by the struggle against quackery makes it worthwhile.
I wish the new Institute ‘Question of Science‘ all the luck it richly deserves and desperately needs.
Professor Frass is well known to most people interested in homeopathy. He has also featured several times on this blog (see here, here and here). Frass has achieved what few homeopaths have: he has integrated homeopathy into a major medical school, the Medical School of the University of Vienna (my former faculty). In 2002, he started teaching homeopathy to medical students, and in 2004, he opened an out-patient clinic ‘Homeopathy for malignant diseases’ at the medical school.
This achievement was widely used for boosting the reputation of homeopathy; the often heard argument was that ‘homeopathy must be good and evidence-based, because a major medical school has adopted it’. This argument is now obsolete: Frass’ lectures have recently been axed!
How come?
Apparently, several students*** filed complaints with their dean about Frass’ lectures. This prompted the dean, Prof Mueller, to look into the matter and take drastic action. He is quoted stating that “the medical faculty rejects unscientific methods and quackery”.
Frass had repeatedly been seen on television claiming that homeopathy could be an effective adjuvant therapy for cancer, and that he had studies to prove it. Such statements had irritated Mueller who then instructed Frass in writing to abstain from such claims and to close his homeopathic out-patient clinic at the University. The matter was also brought to the attention of the University’s ethics committee which decided that Frass’ studies were not suited to provide a scientific proof.
Frass commented saying that he is not surprised about criticism because homeopathy is difficult to understand. He will retire next year from the University and will probably continue his homeopathic practice in a private setting.
(If you can read German, this article in the Austrian paper DER STANDARD has more details)
***as they had invited me to give a lecture on homeopathy some time ago, I like to think that I might have something to do with all this.
The primary objective of this paper was to assess the efficacy of homeopathy by systematically reviewing existing systematic reviews and meta-analyses and to systematically review trials on open-label placebo (OLP) treatments. A secondary objective was to understand whether homoeopathy as a whole may be considered as a placebo treatment. Electronic databases and previously published papers were systematically searched for systematic reviews and meta-analyses on homoeopathy efficacy. In total, 61 systematic reviews of homeopathy were included.
The same databases plus the Journal of Interdisciplinary Placebo Studies (JIPS) were also systematically searched for randomised controlled trials (RCTs) on OLP treatments, and 10 studies were included.
Qualitative syntheses showed that homoeopathy efficacy can be considered comparable to placebo. Twenty‐five reviews demonstrated that homoeopathy efficacy is comparable to placebo, 20 reviews did not come to a definite conclusion, and 16 reviews concluded that homoeopathy has some effect beyond placebo (in some cases of the latter category, authors drew cautious conclusions, due to low methodological quality of included trials, high risk of bias and sparse data).
Qualitative syntheses also showed that OLP treatments may be effective in some health conditions.
The authors concluded that, if homoeopathy efficacy is comparable to placebo, and if placebo treatments can be effective in some conditions, then homoeopathy as a whole may be considered as a placebo treatment. Reinterpreting homoeopathy as a placebo treatment would define limits and possibilities of this practice. This perspective shift suggests a strategy to manage patients who seek homoeopathic care and to reconcile them with mainstream medicine in a sustainable way.
The authors also mention in their discussion section that one of the most important work which concluded that homoeopathy has some effect beyond placebo is the meta‐analysis performed by Linde et al. (1997), which included 119 trials with 2,588 participants and aimed to assess the efficacy of homoeopathy for many conditions. Among these ones, there were conditions with various degrees of placebo responsiveness. This work was thoroughly re‐analysed by Linde himself and other authors (Ernst, 1998; Ernst & Pittler, 2000; Linde et al., 1999; Morrison et al., 2000; Sterne et al., 2001), who, selecting high‐quality extractable data and taking into consideration some methodological issues and biases of included trials (like publication bias and biases within studies), underscored that it cannot be demonstrated that homoeopathy has effects beyond placebo.
I agree with much of what the authors state. However, I fail to see that homeopathy should be used as an OLP treatment. I have several reasons for this, for instance:
- Placebo effects are unreliable and do occur only in some but not all patients.
- Placebo effects are usually of short duration.
- Placebo effects are rarely of a clinically relevant magnitude.
- The use of placebo, even when given as OLP, usually involves deception which is unethical.
- Placebos might replace effective treatments which would amount to neglect.
- One does not need a placebo for generating a placebo effect.
The idea that homeopathic remedies could be used in clinical practice as placebos to generate positive health outcomes is by no means new. I know that many doctors have used it that way. The idea that homeopathy could be employed as OLP, might be new, but it is neither practical, nor ethical, nor progressive.
Regardless of this particular debate, this new review confirms yet again:
HOMEOPATHY = PLACEBO THERAPY
This systematic review was aimed at evaluating the effects of acupuncture on the quality of life of migraineurs. Only randomized controlled trials that were published in Chinese and English were included. In total, 62 trials were included for the final analysis; 50 trials were from China, 3 from Brazil, 3 from Germany, 2 from Italy and the rest came from Iran, Israel, Australia and Sweden.
Acupuncture resulted in lower Visual Analog Scale scores than medication at 1 month after treatment and 1-3 months after treatment. Compared with sham acupuncture, acupuncture resulted in lower Visual Analog Scale scores at 1 month after treatment.
The authors concluded that acupuncture exhibits certain efficacy both in the treatment and prevention of migraines, which is superior to no treatment, sham acupuncture and medication. Further, acupuncture enhanced the quality of life more than did medication.
The authors comment in the discussion section that the overall quality of the evidence for most outcomes was of low to moderate quality. Reasons for diminished quality consist of the following: no mentioned or inadequate allocation concealment, great probability of reporting bias, study heterogeneity, sub-standard sample size, and dropout without analysis.
Further worrisome deficits are that only 14 of the 62 studies reported adverse effects (this means that 48 RCTs violated research ethics!) and that there was a high level of publication bias indicating that negative studies had remained unpublished. However, the most serious concern is the fact that 50 of the 62 trials originated from China, in my view. As I have often pointed out, such studies have to be categorised as highly unreliable.
In view of this multitude of serious problems, I feel that the conclusions of this review must be re-formulated:
Despite the fact that many RCTs have been published, the effect of acupuncture on the quality of life of migraineurs remains unproven.
The American Dance Therapy Association defines Dance Movement Therapy as the psychotherapeutic use of movement to promote emotional, social, cognitive, and physical integration of the participant.
Dance/movement therapy is:
- Focused on movement behavior as it emerges in the therapeutic relationship. Expressive, communicative, and adaptive behaviors are all considered for group and individual treatment. Body movement, as the core component of dance, simultaneously provides the means of assessment and the mode of intervention for dance/movement therapy.
- Practiced in mental health, rehabilitation, medical, educational and forensic settings, and in nursing homes, day care centers, disease prevention, health promotion programs and in private practice.
- Effective for individuals with developmental, medical, social, physical and psychological impairments.
- Used with people of all ages, races and ethnic backgrounds in individual, couples, family and group therapy formats.
This sounds interesting, but does dance therapy work?
The aim of this paper was to perform a systematic review on the effectiveness of dance-based programs in patients with fibromyalgia, as well as calculate the overall effect size of the improvements, through a meta-analysis.
A total of 7 RCTs fulfilled all inclusion criteria. Their methodological quality was low. Duration of dance programs ranged from 12 to 24 weeks. Sessions lasted between 60 and 120 minutes and were performed 1-2 times per week. The overall effect size for pain was -1.64 with a 95% CI from -2.69 to -0.59 which can be interpreted as large. In addition, significant improvements were observed in quality of life, depression, impact of the disease, anxiety, and physical function.
The authors concluded that dance-based intervention programs can be an effective intervention for people suffering from fibromyalgia, leading to a significant reduction of the level of pain with an effect size that can be considered as large. However, findings and conclusions from this meta-analysis must be taken with caution due to the small number of articles and the large heterogeneity.
I don’t doubt that physical activity can ease pain, particularly, if combined with the often positive social interactions of dance. What is unclear to me is whether dance therapy generates results that are better than other forms of physical activity.
And then again, is that question really all that important? Perhaps the best advice to patients is to engage in the type of physical exercise the like best. At the very least, this would minimise the often poor compliance with such programs and might thus maximise their potential benefits.
I only recently came across this review; it was published a few years ago but is still highly relevant. It summarizes the evidence of controlled clinical studies of TCM for cancer.
The authors searched all the controlled clinical studies of TCM therapies for all kinds of cancers published in Chinese in four main Chinese electronic databases from their inception to November 2011. They found a total of 2964 reports (involving 253,434 cancer patients) including 2385 randomized controlled trials and 579 non-randomized controlled studies.
The top seven cancer types treated were lung cancer, liver cancer, stomach cancer, breast cancer, esophagus cancer, colorectal cancer and nasopharyngeal cancer by both study numbers and case numbers. The majority of studies (72%) applied TCM therapy combined with conventional treatment, whilst fewer (28%) applied only TCM therapy in the experimental groups. Herbal medicine was the most frequently applied TCM therapy (2677 studies, 90.32%). The most frequently reported outcome was clinical symptom improvement (1667 studies, 56.24%) followed by biomarker indices (1270 studies, 42.85%), quality of life (1129 studies, 38.09%), chemo/radiotherapy induced side effects (1094 studies, 36.91%), tumour size (869 studies, 29.32%) and safety (547 studies, 18.45%).
The authors concluded that data from controlled clinical studies of TCM therapies in cancer treatment is substantial, and different therapies are applied either as monotherapy or in combination with conventional medicine. Reporting of controlled clinical studies should be improved based on the CONSORT and TREND Statements in future. Further studies should address the most frequently used TCM therapy for common cancers and outcome measures should address survival, relapse/metastasis and quality of life.
This paper is important, in my view, predominantly because it exemplifies the problem with TCM research from China and with uncritical reviews on this subject. If a cancer patient, who does not know the background, reads this paper, (s)he might think that TCM is worth trying. This conclusion could easily shorten his/her life.
The often-shown fact is that TCM studies from China are not reliable. They are almost invariably positive, their methodological quality is low, and they are frequently based on fabricated data. In my view, it is irresponsible to publish a review that omits discussing these facts in detail and issuing a stark warning.
TCM FOR CANCER IS A VERY BAD CHOICE!
The inventor of homeopathy, Samuel Hahnemann, was a German physician. It is therefore not surprising that homeopathy quickly took hold in Germany. After its initial success, homeopathy’s history turned out to be a bit of a roller coaster. But only recently, a vocal and effective opposition has come to the fore (see my previous post).
Despite the increasing opposition, the advent of EBM, and the much-publicised fact that the best evidence fails to show homeopathy’s effectiveness, there are many doctors who still practice it. According to one website, there are 4330 doctor homeopaths in Germany (plus, of course, almost the same number of Heilpraktiker who also use homeopathy). This figure is, however, out-dated. The German Medical Association told a friend that, at the end of 2017, there were 5612 doctors practising in Germany who hold the additional qualification (‘Zusatz-Weiterbildung’) homeopathy.
That’s a lot, I find.
Why so many?
Whenever I give lectures on the subject, this is the question that comes up with unfailing regularity. Many people who ask would also imply that, if so many doctors use it, homeopathy must be fine, because doctors have studied and know what they are doing.
My answer usually is that the phenomenon is due to many factors:
- history,
- regulation,
- misinformation,
- powerful lobby groups,
- patient demand,
- homeopathy’s image of being gentle, safe and holistic,
- patients’ need to believe in something more than ‘just science’,
- the fact that most German health insurances reimburse it,
- political support,
- etc.
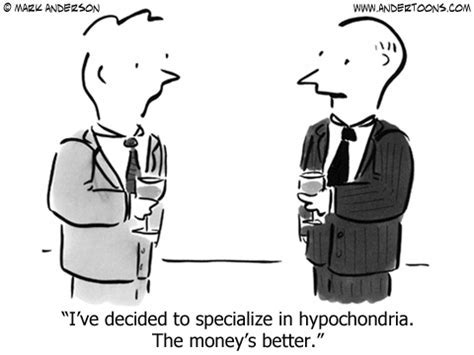
But, in fact, the true explanation, as I have learnt recently, might be much simpler and more profane: MONEY!
A German GP gets 4.36 Euros for taking a conventional history.
If he is a homeopath taking an initial homeopathic history, (s)he gets 130 € according to the ‘Selektivvertrag’.
So, yes, doctors have studied and know that the difference between the two amounts is significant.
In the latest issue of ‘Simile’ (the Faculty of Homeopathy‘s newsletter), the following short article with the above title has been published. I took the liberty of copying it for you:
Members of the Faculty of Homeopathy practising in the UK have the opportunity to take part in a trial of a new homeopathic remedy for treating infant colic. An American manufacturer of homeopathic remedies has made a registration application for the new remedy to the MHRA (Medicines and Healthcare products Regulatory Agency) under the UK “National Rules” scheme. As part of its application the manufacturer is seeking at least two homeopathic doctors who would be willing to trial the product for about a year, then write a short report about using the remedy and its clinical results. If you would like to take part in the trial, further details can be obtained from …
END OF QUOTE
A homeopathic remedy for infant colic?
Yes, indeed!
The British Homeopathic Association and many similar ‘professional’ organisations recommend homeopathy for infant colic: Infantile colic is a common problem in babies, especially up to around sixteen weeks of age. It is characterised by incessant crying, often inconsolable, usually in the evenings and often through the night. Having excluded underlying pathology, the standard advice given by GPs and health visitors is winding technique, Infacol or Gripe Water. These measures are often ineffective but fortunately there are a number of homeopathic medicines that may be effective. In my experience Colocynth is the most successful; alternatives are Carbo Veg, Chamomilla and Nux vomica.
SO, IT MUST BE GOOD!
But hold on, I cannot find a single clinical trial to suggest that homeopathy is effective for infant colic.
Ahhhhhhhhhhhhhhhhhhh, I see, that’s why they now want to conduct a trial!
They want to do the right thing and do some science to see whether their claims are supported by evidence.
How very laudable!
After all, the members of the Faculty of Homeopathy are doctors; they have certain ethical standards!
After all, the Faculty of Homeopathy aims to provide a high level of service to members and members of the public at all times.
Judging from the short text about the ‘homeopathy for infant colic trial’, it will involve a few (at least two) homeopaths prescribing the homeopathic remedy to patients and then writing a report. These reports will unanimously state that, after the remedy had been administered, the symptoms improved considerably. (I know this because they always do improve – with or without treatment.)
These reports will then be put together – perhaps we should call this a meta-analysis? – and the overall finding will be nice, positive and helpful for the American company.
And now, we all understand what homeopaths, more precisely the Faculty of Homeopathy, consider to be evidence.