politics
The BBC stands for reliable information, at least that’s what I used to believe. After reading a recent article published on the BBC website, I have my doubts, however. See for yourself; here are a few excerpts:
On a holiday to Kerala on India’s south-western Malabar Coast, Shilpa Iyer decided to visit Kotakkal, a town that became famous after the establishment of Arya Vaidya Sala, Kerala’s best-known centre for the practice of Ayurveda, in 1902. Seven days later, she left the historical treatment centre after completeing panchakarma, a cleansing and rejuvenating programme for the body, mind and consciousness.
“There was nothing really wrong, but I was always busy with the demands of modern life and plagued with continual aches and pains. So, I decided to focus on my own health,” Iyer says.
Panchakarma, a holistic Ayurvedic therapy, involves a series of detoxifying procedures. It integrates herbal medicines, cleansing therapies, personalised diet plans and wellness activities to eliminate the root cause of disease, revive and rejuvenate the body, and ensure health and longevity.
Iyer says she left “feeling lighter, healthier and better than ever before”. She isn’t the only one who signed up for an Ayurvedic treatment in Kerala; the holistic system of medicine is a way of life in this coastal paradise.
… Ayurveda translates to “knowledge of life” and originated in India more than 3,000 years ago. It is based on the ideology that health and wellness depend on a delicate balance between the mind, body, spirit and environment, and places great emphasis on preventive strategies rather than curative ones. The ancient system of medicine is centred on the idea of universal interconnectedness between prakriti (the body’s constitution) and doshas (life forces). Varied combinations of the five elements — aakash (sky), jal (water), prithvi (earth), agni (fire) and vayu (air) – create the three doshas.

Dr Gaurang Paneri, an Ayurveda practitioner, explains every person has the three doshas, vata, pitta and kapha, in varying strength and magnitude. “The predominant dosha determines their prakriti. Diseases arise when doshas are affected because of an external or internal stimulus (typically linked to eating habits, lifestyle or physical exercise). Ayurveda works to ensure harmony between the three,” he says…
The small state has more than 100 Ayurvedic government-run hospitals, 800 Ayurvedic pharmaceutical factories and 800 Ayurvedic medicine dispensaries. As many as 120 holiday resorts and private wellness centres offer specialised treatments such as kasti vvasti, an oil-based treatment for back pain and inflammation in the lumbosacral region; elakkizhi, a treatment with heated herbal poultices to tackles aches, pains and muskoskeletal trauma; njavara kizhi, a massage therapy for arthritis or chronic musculoskeletal discomfort; and shirodhara, a restorative therapy to ease stress and anxiety and that involves pouring warm, medicated oil over the forehead.
Most treatment centres offer therapies and treatments for a range of health issues, including immunity, mental health, anxiety, pain management, weight loss, skin and health care, sleep issues, psoriasis, eczema, eye care, arthritis, sciatica, gastric problems and paralysis. The treatments typically include dietary changes, herbal medicines, massage therapies, poultices, meditation and breath exercises…
___________________________
I find such advertisements disguised as journalism disturbing:
- No mention that the treatments in question lack conclusive evidence of effectiveness.
- Not a word about the fact that many can be outright dangerous.
- No mention of the often exorbitant fees visitors are asked to pay.
Please do better next time you report about health matters, BBC!
This review updated and extended a previous one on the economic impact of homeopathy. A systematic literature search of the terms ‘cost’ and ‘homeopathy’ from January 2012 to July 2022 was performed in electronic databases. Two independent reviewers checked records, extracted data, and assessed study quality using the Consensus on Health Economic Criteria (CHEC) list.
Six studies were added to 15 from the previous review. Synthesizing both health outcomes and costs showed homeopathic treatment being at least equally effective for less or similar costs than control in 14 of 21 studies. Three studies found improved outcomes at higher costs, two of which showed cost-effectiveness for homeopathy by incremental analysis. One found similar results and three similar outcomes at higher costs for homeopathy. CHEC values ranged between two and 16, with studies before 2009 having lower values (Mean ± SD: 6.7 ± 3.4) than newer studies (9.4 ± 4.3).
The authors concluded that, although results of the CHEC assessment show a positive chronological development, the favorable cost-effectiveness of homeopathic treatments seen in a small number of high-quality studies is undercut by too many examples of methodologically poor research.
I am always impressed by the fantastic and innovative phraseology that some authors are able to publish in order to avaid calling a spade a spade. The findings of the above analysis clearly fail to be positive. So why not say so? Why not honestly conclude something like this:
Our analysis failed to show conclusive evidence that homeopathy is cost effective.
To find an answer to this question, we need not look all that far. The authors’ affiliations give the game away:
- 1Department of Psychology and Psychotherapy, Witten/Herdecke University, Witten, Germany.
- 2Medical Scientific Services/Medical Affairs, Deutsche Homöopathie-Union DHU-Arzneimittel GmbH & Co. KG, Karlsruhe, Germany.
- 3Institute of Integrative Medicine, Witten/Herdecke University, Herdecke, Germany.
- 4Department of Pharmaceutical and Pharmacological Sciences, KU Leuven, Leuven, Belgium.
Another rather funny give-away is the title of the paper: the “…evaluation for…”comes form the authors’ original title (Overview and quality assessment of health economic evaluations for homeopathic therapy: an updated systematic review) and it implies an evaluation in favour of. The correct wording would be “evaluation of”, I think.
I rest my case.
An interesting and fully referenced (205 references) article caught my attention; it seems highly relevant to the discussions we are having on this blog. Let me show you the abstract:
Medical misinformation has always existed, but it has recently become more frequent due to the development of the internet and social media. Medical misinformation can cover a wide variety of topics, and studies show that some groups are more likely to be affected by medical misinformation than others, like those with less trust in health care, less health literacy, and a more positive attitude toward alternative medicines. Aspects of the internet, like echo chambers and algorithms, have contributed to the rise of medical misinformation, along with belief in anecdotal evidence and alternative remedies that are not backed by science. Some personal beliefs and a lack of media literacy skills are also contributing to medical misinformation. Medical misinformation causes higher rates of death and negative health outcomes, a lack of trust in medical professionals, and more racism and hate crimes. One possible way to combat the spread of misinformation is education surrounding media literacy. Still, there are gaps in this practice that must be addressed like a lack of high-quality research about different educational programs.
The author also offers the following key points:
- Medical misinformation is becoming an urgent issue for United States citizens—leading to increased deaths,
a lack of trust in health professionals, and hate crimes and racism. - Although this is a worldwide issue, the United States has the second highest rate of misinformation of any
country, behind India. - One piece of misinformation during the COVID-19 pandemic stated that highly concentrated alcohol could
disinfect the body and kill the virus. Studies show that 800 people died, 5,876 were hospitalized, and 60
became completely blind from drinking methanol, thinking it would cure coronavirus. - Studies estimate that only 14% of the United States population has proficient health literacy, which makes it difficult to recognize medical misinformation.
- Media literacy education is being pursued in order to combat the spread of misinformation, but more research is needed in order to understand the long-term effects of this education and what programs are best.
__________________
I would like to stress, as indeeed the author does as well, that medical misinformation is a phenomenon that is by no means confined to the US. Like most information, misinformation has become a global issue. Its dangers cannot be under-estimated. My blog offers an abundance of reports where misinformation in the realm of so-called alternative medicine (SCAM) has caused harm and even death. The author advocates media literacy as a remedy for the problem. I would argue that even more important would be to teach CRITICAL THINKING, a task that has to start at school and must continue well into adult life.
This conclusion is so very obvious that it begs an important question: WHY HAS IT NOT BEEN DONE YEARS AGO? The answer, I fear, is simple: for reasons that are self-evident, governments have little interst in the public being able to think critically. On the contrary, governments across the world foremost want to be re-elected, and critical thinking would be a major obstacle to this aim.
In spite of the safety and efficiency of the COVID-19 vaccines and the many promotion efforts of political and expert authorities, a fair portion of the population remained hesitant if not opposed to vaccination. Public debate and the available literature point to the possible role of people’s attitudes towards medical institutions as well as their preference for so-called alternative medicine (SCAM) on their motivations and intentions to be vaccinated. Other potential ideological factors are beliefs about environmental laissez-faire and divine providence insofar as they encourage people to let the pandemic unfold without human interference.
In three cross-sectional samples (total N = 8214), collected at successive moments during the Belgian vaccination campaign, the present research examines the distal role of these psychological and ideological factors on vaccination intentions via motivational processes.
- Study 1 gauges the relation between trust in medical institutions and preference for SCAM on intentions to get vaccinated via motivations.
- Study 2 examines the role of beliefs in the desirability of letting nature take its course (‘environmental laissez-faire beliefs’) on vaccination intention via motivations.
- Study 3 tests whether people’s adherence to environmental laissez-faire and beliefs about divine providence are linked to their motivations for vaccination via trust in the medical institutions and SCAM.
The results show that adherence to SCAM has a deleterious effect on vaccination intentions, whereas trust in medical institutions has a positive effect. Both ideological factors pertaining to external control are only moderately related, with environmental laissez-faire beliefs having stronger effects on SCAM, medical trust and vaccination motivations.
The evidence of an association between SCAM and willingness to get vaccinated is undeniable. On this blog, we have discussed it repeatedly, e.g.:
- Use of so-called alternative medicine (SCAM) and its association with SARS-CoV-2 vaccination status
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- Andrew Wakefield, Donald Trump, SCAM, and the anti-vaccination cult
- Measles are back – not least thanks to so-called alternative medicine (SCAM), I fear
- Reasons for parental hesitancy or refusal of childhood vaccination
- Endorsement of so-called alternative medicine (SCAM) and vaccine hesitancy among physicians
- Are people who oppose COVID-19 vaccinations intellectually challenged?
- So-called alternative medicine (SCAM) and vaccine hesitancy among physicians: findings from Germany, Finland, Portugal, and France
- Interest in so-called alternative medicine is linked to vaccination coverage
- Misinformation and conspiratorial thinking are at the heart of so-called alternative medicine(SCAM)
- Vaccination rates of Canadian healthcare professionals: those of chiropractors and naturopaths are at the lowest
- Echo chambers of vaccine hesitancy and so-called alternative medicine (SCAM)
- Preference of so-called alternative medicine predicts negative attitudes to vaccination
- What are the reasons for opposing COVID vaccinations?
- Anti-vax arguments used by proponents of SCAM are stupid, or wrong, or both
But what exactly is the nature of this association?
- Does SCAM-use predispose to vaccination hesitancy?
- Does Vaccination hesitancy predispose to SCAM use?
- Is both true?
After reading all this research that has emerged on the subject, I get the impression that we are mostly dealing here with a cross-correlation where a certain mind-set of being
- prone to conspiracy theories,
- anti-establishment,
- anti-science,
- irrational,
- of low intelligence,
- unable of critical thinking,
- etc., etc,
determines both the SCAM-use and the vaccination hesitancy.
Whenever a journalist wants to discuss the subject of acupuncture with me, he or she will inevitably ask one question:
DOES ACUPUNCTURE WORK?
It seems a legitimate, obvious and simple question, particularly during ‘Acupuncture Awareness Week‘, and I have heard it hundreds of times. Why then do I hesitate to answer it?
Journalists – like most of us – would like a straight answer, like YES or NO. But straight answers are in short supply, particularly when we are talking about acupuncture.
Let me explain.
Acupuncture is part of ‘Traditional Chinese Medicine’ (TCM). It is said to re-balance the life forces that determine our health. As such it is seen as a panacea, a treatment for all ills. Therefore, the question, does it work?, ought to be more specific: does it work for pain, obesity, fatigue, hair-loss, addiction, anxiety, ADHA, depression, asthma, old age, etc.etc. As we are dealing with virtually thousands of ills, the question, does it work?, quickly explodes into thousands of more specific questions.
But that’s not all!
The question, does acupuncture work?, assumes that we are talking about one therapy. Yet, there are dozens of different acupuncture traditions and sites:
- body acupuncture,
- ear acupuncture,
- tongue acupuncture,
- scalp acupuncture,
- etc., etc.
Then there are dozens of different ways to stimulate acupuncture points:
- needle acupuncture,
- electroacupuncture,
- acupressure,
- moxibustion,
- ultrasound acupuncture,
- laser acupuncture,
- etc., etc.
And then there are, of course, different acupuncture ‘philosophies’ or cultures:
- TCM,
- ‘Western’ acupuncture,
- Korean acupuncture,
- Japanese acupuncture,
- etc., etc.
If we multiply these different options, we surely arrive at thousands of different variations of acupuncture being used for thousands of different conditions.
But this is still not all!
To answer the question, does it work?, we today have easily around 10 000 clinical trials. One might therefore think that, despite the mentioned complexity, we might find several conclusive answers for the more specific questions. But there are very significant obstacles that are in our way:
- most acupuncture trials are of lousy quality;
- most were conducted by lousy researchers who merely aim at showing that acupuncture works rather that testing whether it is effective;
- most originate from China and are published in Chinese which means that most of us cannot access them;
- they get nevertheless included in many of the systematic reviews that are currently being published without non-Chinese speakers ever being able to scrutinise them;
- TCM is a hugely important export article for China which means that political influence is abundant;
- several investigators have noted that virtually 100% of Chinese acupuncture trials report positive results regardless of the condition that is being targeted;
- it has been reported that about 80% of studies emerging from China are fabricated.
Now, I think you understand why I hesitate every time a journalist asks me:
DOES ACUPUNCTURE WORK?
Most journalists do not have the patience to listen to all the complexity this question evokes. Many do not have the intellectual capacity to comprehend an exhaustive reply. But all want to hear a simple and conclusive answer.
So, what do I say in this situation?
Usually, I respond that the answer would depend on who one asks. An acupuncturist is likely to say: YES, OF COURSE, IT DOES! An less biased expert might reply:
IT’S COMPLEX, BUT THE MOST RELIABLE EVIDENCE IS FAR FROM CONVINCING.
In recent weeks and months, I have been thinking quite a lot about the various types of scientists. This is partly due to me finishing a book entitled:
1. SCIENTIST
Scientists gather information through observation and experimentation, formulate hypothesis, and then test them. They work in vastly different areas but have certain attitudes or qualities in common, e.g. critial thinking and an open mind. As scientists tend to publish their findings, a very simple (but not fool-proof) way to identify a scinetist is to look him/her up, for example by finding his/her H-Index. (The H-Index is defined as the maximum value of h such that the given author/journal has published at least h papers that have each been cited at least h times. For instance, if someone has 10 papers that were cited 10 times, his H-Index would be 10. If another scientist has 50 papers that were cited 50 times, his H-Index would be 50.)
2. PSEUDO-SCIENTIST
Pseudo-scientists are people who pretend to produce science but, in fact, they generate pseudoscience. The demarkation of pseudo-science from science is sometimes difficult, as we have seen several times on this blog, e.g.:
- Characteristics of pseudoscience
- Science or Pseudoscience?
- Is acupuncture pseudoscience?
- The techniques of pseudoscience
- Pseudoscience revisited
- Tolerance towards pseudo-science?
- How to become a charlatan
The pseudo-scientist does have no or just a few publications in the peer-reviewed literature and no H-Index to speak of.
3. WOULD-BE SCIENTIST
The term ‘would-be scientist’ is not one that is commonly used, nor is it one that has an accepted definition. The way I see it, would-be scientists are aspiring to become scientist. They are on the way to become a scientist but have not quite arrived yet. To the would-be scientist I say: good luck to you; I hope you make it and I look forward to reading about your scientific achievements. The would-be scientist is, however, not the topic of my post.
4. THE PREDEND-SCIENTIST
The predent-scientist (PS) is the one who I want to focus on here. He – yes, the PS is usually male – talks a lot about science; so much so that outsiders would get the impression that he actually is a scientist. Crucially, the PS himself has managed to delude himself to the point where believes to be a scientist.
While scientists tend to be media-shy, the PS enjoys the limelight to generate the impression of being a scientist. He talks eloquently and at length about science. Much of what he says or writes might even be correct. The PS is often quite well-versed and knows (most of) his stuff.
The crucial difference between the PS and the scientist is that the PS produces no or very little science; neither does he intend to. To identify the PS, an easy (but not fool-proof) method is to him look up. Typically, he has published several articles in the popoular press or books for the lay public, but – as he does not conduct scientific research – he does not generate papers in the peer-reviewed scientific literature. This void, however, has never stopped the PS from appearing in the media speaking about science, nor from occupying prominent positions in the world of science, nor from avidly rubbing shoulders with scientists. Few people see anything wrong with that, mainly because the PS has convinced them (most importantly himself) that he actually is a scientist. While the scientist is trained in doing science, the PS is trained in talking about science.
Don’t get me wrong, the PS can have his merits. He often presents science to the public more or less accurately and frequently is rhetorically superior to the scientist. I nevertheless have reservations about the PS (and the recent pandemic has shown us how dangerous PSs can beome). The questions to ask ourselves are the following:
- Does PS have a truly open mind?
- Can he set aside ideologies?
- Will he change his opinion vis a vis new evidence?
- Is he prepared to consider criticism?
- Does he avoid ‘black and white’ thinking?
- Is he sufficiently humble?
- Is he honest with himself and others?
These questions refer to important attitudes that scientists learn – often the hard way – while doing science. If someone lacks this experience, such attitudes are likely to be under-developed. Perhaps, it all boils down to honesty: if a man who has never done any amount of science to speak of has convinced himself to be a scientist, he arguably is dishonest with himself and the public.
In order to make my points as clearly as possible, I admittedly caricaturized the extremes of a wider spectrum; my appologies for that. In reality, the different types of scientists rarely exist as entirely pure forms. Frequently, people are mixtures of two types, either because they did different things during different periods of their lives, or because they simply are hybrids.
To provide a few examples, let me show you 14 H-Indices (according to ‘Google Scholar’) of people (in alphabetical order) who you might have heard of, for instance, because they have featured on my blog. I leave it up to you to decide how well they fit in any of my three categories and who might qualify to be a PS.
- Fabrizio Benedetti – H-Index = 83
- David Colquhoun – H-Index = 78
- Ian Chalmers – H-Index = 84
- Michael Dixon – H-Index = 0
- David Gorski – H-Index = 30
- Holm Hümmler – H-Index = 0
- Ted Kaptchuk – H-Index = 103
- Jos Kleinjen – H-Index = 104
- Andreas Michalsen – H-Index = 0
- Michael Mosely – H-Index = 0
- Dana Ullman – H-Index = 0
- Dale Thompson (alias DC) – H-Index = 0
- Chris van Tulleken – H-Index = 0
- Harald Walach – H-Index = 9
My conclusion: the PS, a person who presents himself as a scientist without having done any meaningful amount of science himself, is a man who is not entirely honest. The H-Index can be helpful for identifying PSs. An index of zero, for instance, seems to send out a fairly clear message. In the case low indices, it is advisable to go one step further and study the actual articles That mede up the index. However, the H-Index tells us nothing about whether someone presents himself as a scientist; this information must be gleaned from the person him(her)self.
The origin of coronavirus 2 (SARS-CoV-2) has been the subject of intense speculation and several conspiracy theories, not least amongst the enthusiasts of so-called alternative medicine. Now Australian scientists have attempted to identify the origin of the coronavirus 2 (SARS-CoV-2). As this is undoubtedly a most sensitive subject, let me show you the unadulterated abstract of their paper:
The origin of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is contentious. Most studies have focused on a zoonotic origin, but definitive evidence such as an intermediary animal host is lacking. We used an established risk analysis tool for differentiating natural and unnatural epidemics, the modified Grunow–Finke assessment tool (mGFT) to study the origin of SARS-COV-2. The mGFT scores 11 criteria to provide a likelihood of natural or unnatural origin. Using published literature and publicly available sources of information, we applied the mGFT to the origin of SARS-CoV-2. The mGFT scored 41/60 points (68%), with high inter-rater reliability (100%), indicating a greater likelihood of an unnatural than natural origin of SARS-CoV-2. This risk assessment cannot prove the origin of SARS-CoV-2 but shows that the possibility of a laboratory origin cannot be easily dismissed.
The somewhat clumsy wording harbours explosive potential. It is more likely that the pandemic was started by a laboratory accident than by a zoonosis. In this case, it would be man-made rather than natural. The authors of the paper do, however, caution that their analysis does not prove the origin of the coronavirus. They merely speak of likelihoods. Moreover, it seems important to stress that there is no scientific evidence that Sars-CoV-2 was deliberately developed as a biological warfare agent.
Will this paper put an end to speculation and conspiracy?
I doubt it!
The Amercian Medical Association (AMA) recently published a lengthy article on naturopathy in the US. Here are some excerpts:
There are three types of health professionals who offer naturopathic treatment:
- Naturopathic doctors. These nonphysicians graduate from a four-year, professional-level program at an accredited naturopathic medical school, earning either the doctor of naturopathy (ND) degree or the doctor of naturopathic medicine (NMD) degree.
- Traditional naturopaths, who have obtained education through some combination of a mentorship program with another professional or at an alternative clinic, distance-learning program or classroom schooling on natural health, or other holistic studies.
- Other health professionals such as chiropractors, massage therapists, dentists, nurses, nutritionists, or physicians who practice under a professional license but include some naturopathic methods in their practice and who may have studied on their own or taken courses on naturopathic methods.
At least 24 states and the District of Columbia regulate the practice of naturopathy. In order to be licensed, naturopaths in these states must earn an ND or NMD from an accredited naturopathic program and pass the Naturopathic Physicians Licensing Exam. Three states—Florida, South Carolina and Tennessee—prohibit the practice of naturopathy. In states that neither license nor prohibit the practice of naturopathy, traditional naturopaths and NDs alike may practice without being subject to state regulation.
Postgraduate training is neither common nor required of graduates of naturopathic schools, except in Utah … less than 10% of naturopaths participate in an approved residency, and such residencies last only a year and lack a high degree of standardization.
… naturopaths are required to get at least 1,200 hours of direct patient contact, physicians get 12,000–16,000 hours of clinical training…
ND programs emphasize naturopathic principes—for example, the healing power of nature—and naturopathic therapeutics such as botanical medicine, homeopoathy and hydrotherapy. Coursework in naturopathic therapeutics is combined with, and taught alongside, coursework in sciences. But there are no specifications around the number of hours required in each area … naturopathic students may lack exposure to key clinical scenarios in the course of their training … naturopathic students’ clinical experience is typically gained through outpatient health care clinics, as naturopathic medical schools typically do not have significant hospital affiliation. This means there is no guarantee that a naturopathic student completing a clinical rotation will see patients who are actually sick or hospitalized, and they may not be exposed to infants, children, adolescents or the elderly. It has been said that naturopaths tend to treat the “worried well.”
… Naturopaths claim they are trained as primary care providers and, as such, are educated and trained to diagnose, manage and treat many conditions, including bloodstream infections, heart disease and autoimmune disorders. Yet their education and training falls several years and thousands of hours short of what physicians get.
…The AMA believes it is the responsibility of policymakers to ensure that naturopaths’ claims that they can treat a broad range of conditions are backed by facts—facts that include the specific education and training necessary to ensure patient safety.
________________
The AMA is clearly cautious here. A less polite statement might simply stress that naturopaths are taught a lot of nonsense which they later tend to administer to their unsuspecting patients. On this blog, we have repeatedly discussed the danger naturopaths present to public health in the US and elsewhere, e.g.:
- How reliable are the claims made by naturopathic influencers?
- Naturopath jailed for selling fraudulent vaccination documents
- Naturopath fined for misdiagnosing and treating a rectal tumor for hemorrhoids
- Naturopaths are ‘not bound by science,’ lawyer argues
- Vaccination rates of Canadian healthcare professionals: those of chiropractors and naturopaths are at the lowest
- Is veterinary naturopathy animal abuse?
- Naturopathic ‘cancer specialist’ using coffee enemas found guilty
- Patients consulting chiropractors, homeopaths, or naturopaths are less likely to agree to the flu jab
- A naturopath responsible for the death of two cancer patients was sentenced to two years
- A naturopath in court after two of his cancer patients died
- Many naturopaths, homeopaths, and chiropractors are a risk to public health
- Naturopath treats autism with fecal transplants
- A naturopath promoting fake news about COVID vaccinations
- Naturopathy (according to the WNF) = quackery steeped in obsolete fantasies
- Canadian naturopaths may no longer call themselves ‘medically trained’
- Naturopaths’ counselling against vaccinations could be criminally negligent
- Naturopathy for cancer … claims that have the potential to be lethal
- Severe liver injury due to naturopaths’ prescription of Epsom salt
- Naturopaths should not treat children
- Some naturopaths are clearly a danger to public health
- Death of a child through naturopathy
Claims that naturopaths are a viable alternative to evidence-based medicine are wrong, irresponsible and dangerous. Regulators must be reminded that they have the duty to protect the public from charlatans and should therefore ensure that no false therapeutic or diagnostic claims can be made by naturopaths.
Please allow me to write a post today that has nothing at all to do with so-called alternative medicine, not even with medicine.
Yesterday, 13 March, was my mother’s birthday. She was born in 1911 and died in 1989. I often think of her and the remarkable life she had, particularly, of course, on 13 March.
Going through my X-feed yesterday, I saw this post from the Auschwitz Memorial:
Józef Kowalski was born in Siedliska on 13 March 1911 to Wojciech and Zofia Borowiec, the seventh of their nine children. He was ordained a priest on 29 May 1938 as member of the Salesian Religious Society. During the German occupation of Poland, the Salesians continued their educational work. The Gestapo arrested Kowalski on 23 May 1941, along with eleven other Salesians. They were taken to Montelupich Prison and tortured.
Kowalski was sent to Auschwitz on 26 June 1941. There, he ministered to his fellow prisoners usually in secret, but at least once in front of everyone at the moment of mass execution. He was ordered by Blockführer Gerhard Palitzsch to trample upon his rosary but refused. Palitzsch was one of the most brutal of all the SS officers of the camps (he later vanished from the records, possibly killed in action). As punishment, he was assigned to a penal company. In his last letter to his parents, Józef wrote:
Do not worry about me; I am in God’s hands. I want to assure you that I feel His help at every step. Despite the present situation, I am happy and completely at peace.
On 3 July 1942 he was mocked and severely beaten by the guards for being a priest. The same night, they pulled him out of his barracks, gravely beat him again and killed him. Kowalski’s body was found the next day and burned with others. He was 31 years of age.
Pope John Paul II who had known Kowalski personally beatified Kowalski on 13 June 1999.
____________________________
Please forgive me if you find this post irrelevant or inappropriate.
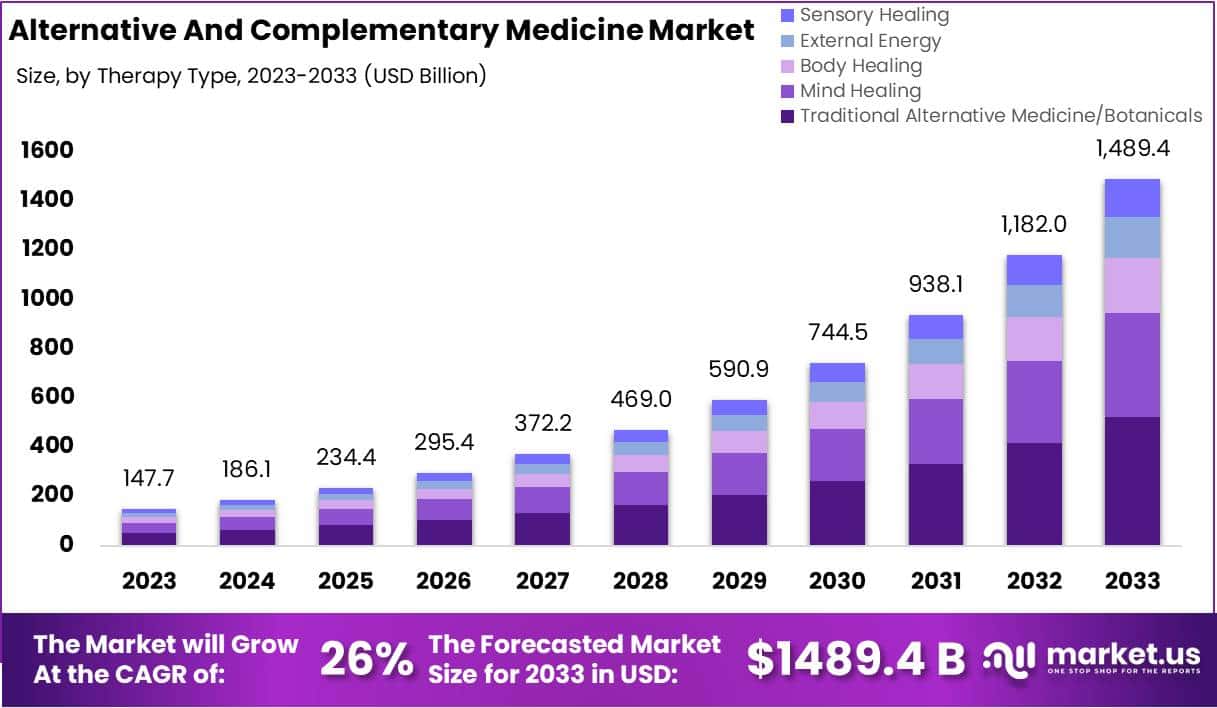
I usually take ‘market reports’ with a pinch of salt. Having said that, this document makes some rather interesting predictions:
The size of the market for so-called alternative medicine (SCAM) is projected to expand from USD 147.7 billion in 2023 to approximately USD 1489.4 billion by the year 2033. This projection indicates a remarkable Compound Annual Growth Rate (CAGR) of 26% over the forecast period.
The market for SCAM is experiencing significant growth, fueled by increasing consumer interest in natural and holistic health solutions. This trend reflects a broader shift in societal attitudes towards health and wellness, emphasizing preventive care and natural health practices.
The market’s dynamics are influenced by various factors, including consumer preferences, regulatory standards, and evolving perceptions of health and wellness. As the popularity of these alternative therapies grows, it is crucial for individuals to consult with healthcare professionals to ensure that these non-conventional approaches are safely and effectively incorporated into their overall health regimen. The increasing acceptance of SCAM underscores a collective move towards more personalized and holistic healthcare solutions, resonating with today’s health-conscious consumers.
In 2023, Traditional Alternative Medicine/Botanicals led the market, capturing a 35.2% share, which reflects a strong consumer inclination towards these treatments. Dietary Supplements were prominent in the market, securing a 25.1% share in 2023, which underscores the high consumer demand for nutritional aids. Direct Sales were the most favored distribution channel, accounting for 43.2% of the market share in 2023, which indicates their significant impact on guiding consumer purchases. Pain Management was the predominant application area, holding a 24.9% market share in 2023, propelled by the growing acknowledgment of non-pharmacological treatment options. Adults represented a substantial portion of the market, making up 62.33% in 2023, signifying a marked preference for SCAM therapies within this age group. Europe stood out as the market leader, claiming a 42.6% share in 2023, a position supported by widespread acceptance, governmental backing, and an increasing elderly population. The regions of North America and Asia-Pacific are highlighted as areas with potential, signaling opportunities for market expansion beyond the European stronghold in the upcoming years.
Leading Market Players Are:
- Columbia Nutritional
- Nordic Nutraceuticals
- Ramamani Iyengar Memorial Yoga Institute
- The Healing Company Ltd.
- John Schumacher Unity Woods Yoga Centre
- Sheng Chang Pharmaceutical Company
- Pure encapsulations LLC.
- Herb Pharm
- AYUSH Ayurvedic Pte Ltd.
Recent developments:
- In December 2023, Adoratherapy launched the Alkemie Chakra Healing Line, an aromatherapy range aimed at harmonizing the seven chakras.
- Coworth Park introduced the Hebridean Sound Treatment in October 2023, merging traditional Hebridean sounds with guided meditation to offer a novel, restorative wellness experience.
- The World Health Organization released draft guidelines in September 2023 for the safe, effective application of traditional medicines.
- Telehealth services, expanding significantly in August 2023, have broadened the reach of SCAM, enhancing patient access to these treatments.


