patient choice
The BBC stands for reliable information, at least that’s what I used to believe. After reading a recent article published on the BBC website, I have my doubts, however. See for yourself; here are a few excerpts:
On a holiday to Kerala on India’s south-western Malabar Coast, Shilpa Iyer decided to visit Kotakkal, a town that became famous after the establishment of Arya Vaidya Sala, Kerala’s best-known centre for the practice of Ayurveda, in 1902. Seven days later, she left the historical treatment centre after completeing panchakarma, a cleansing and rejuvenating programme for the body, mind and consciousness.
“There was nothing really wrong, but I was always busy with the demands of modern life and plagued with continual aches and pains. So, I decided to focus on my own health,” Iyer says.
Panchakarma, a holistic Ayurvedic therapy, involves a series of detoxifying procedures. It integrates herbal medicines, cleansing therapies, personalised diet plans and wellness activities to eliminate the root cause of disease, revive and rejuvenate the body, and ensure health and longevity.
Iyer says she left “feeling lighter, healthier and better than ever before”. She isn’t the only one who signed up for an Ayurvedic treatment in Kerala; the holistic system of medicine is a way of life in this coastal paradise.
… Ayurveda translates to “knowledge of life” and originated in India more than 3,000 years ago. It is based on the ideology that health and wellness depend on a delicate balance between the mind, body, spirit and environment, and places great emphasis on preventive strategies rather than curative ones. The ancient system of medicine is centred on the idea of universal interconnectedness between prakriti (the body’s constitution) and doshas (life forces). Varied combinations of the five elements — aakash (sky), jal (water), prithvi (earth), agni (fire) and vayu (air) – create the three doshas.

Dr Gaurang Paneri, an Ayurveda practitioner, explains every person has the three doshas, vata, pitta and kapha, in varying strength and magnitude. “The predominant dosha determines their prakriti. Diseases arise when doshas are affected because of an external or internal stimulus (typically linked to eating habits, lifestyle or physical exercise). Ayurveda works to ensure harmony between the three,” he says…
The small state has more than 100 Ayurvedic government-run hospitals, 800 Ayurvedic pharmaceutical factories and 800 Ayurvedic medicine dispensaries. As many as 120 holiday resorts and private wellness centres offer specialised treatments such as kasti vvasti, an oil-based treatment for back pain and inflammation in the lumbosacral region; elakkizhi, a treatment with heated herbal poultices to tackles aches, pains and muskoskeletal trauma; njavara kizhi, a massage therapy for arthritis or chronic musculoskeletal discomfort; and shirodhara, a restorative therapy to ease stress and anxiety and that involves pouring warm, medicated oil over the forehead.
Most treatment centres offer therapies and treatments for a range of health issues, including immunity, mental health, anxiety, pain management, weight loss, skin and health care, sleep issues, psoriasis, eczema, eye care, arthritis, sciatica, gastric problems and paralysis. The treatments typically include dietary changes, herbal medicines, massage therapies, poultices, meditation and breath exercises…
___________________________
I find such advertisements disguised as journalism disturbing:
- No mention that the treatments in question lack conclusive evidence of effectiveness.
- Not a word about the fact that many can be outright dangerous.
- No mention of the often exorbitant fees visitors are asked to pay.
Please do better next time you report about health matters, BBC!
We all have heard of so-called alternative therapies but few of us are aware of the fact that there are also alternative diagnoses. These are diagnoses used regularly by practitioners of so-called alternative medicine (SCAM) that have no basis on science, or – to put it simply – that do not exist. They are nonetheless popular with SCAM practitioners and allegedly cause a wide range of non-specific symptoms such as:
- anxiety,
- brain fog,
- constipation,
- depression,
- dizziness,
- fatigue,
- headaches,
- heart palpitations,
- insomnia,
- irritability,
- muscle and joint pain,
- loss of appetite,
- loss of libido,
- weight gain.
In this series of posts, I will briefly discuss some of these diagnoses and list the treatments that SCAM practitioners might recommend for them.
Adrenal Fatigue
Adrenal fatigue is not the same as adrenal insufficiency or Addison’s disease; it is a term coined by a chiropractor who claimed that the stresses of modern life tire out the adrenal glands. In turn, this phenomenon allegedly leads to generalised weariness.
There is not evidence that this is true, nor that adrenal fatigue even exists. A systematic review of the evidence concluded that “there is no substantiation that adrenal fatigue is an actual medical condition.”
Yet, SCAM practitioners advise to cure adrenal fatigue with a range of dietary supplements (e.g. fish oil, ashwagandha, rhodiola rosea, schisandra and holy basil, licorice, magnesium, various vitamins), special diets, lifestyle adjustments, stress management and many other SCAMs. They all have in common that their effectiveness is not supported by convincing evidence from rigorous clinical trials.
Candidiasis hypersensitivity
Most of us are infected by the fungus Candida albicans without being affected by it in any way. Yet, many SCAM practitioners claim that candidiasis hypersensitivity is a condition that causes symptoms like fatigue, premenstrual tension, gastrointestinal symptoms, and depression and therefore needs treating.
But, candidiasis hypersensitivity does not exist. An RCT concluded that, “in women with presumed candidiasis hypersensitivity syndrome, nystatin does not reduce systemic or psychological symptoms significantly more than placebo.”
This, however, does not stop SCAM practitioners to recommend numerous forms of SCAM to treat the condition, e.g.: dietary supplements containing probiotics, milk thistle, red thyme, barberry, garlic, or external applications of coconut oil, essential oils of peppermint oil, lavender oil, oregano oil, and tea tree. No sound evidence exists to show that ant of these SCAMs can successfully treat the condition.
Chronic intoxications
Chronic intoxications do ecist, of course. But in the realm of SCAM, they are diagosed for the sole putpose of selling their various ‘detox’ treatments. The alleged rationale is that our bodies are overloaded with all sorts ot harmful substances, for instance, from the environment, from our food, from modern drugs, or from our own metabolism.
To eliminate them, we need to ‘detox’. For that purpose, SCAM practitioners recommend a very wide range of SCAMs; in fact, it is hardly possible to identify a single form of SCAM that is not said to detoxify our bodies. Yet, for none of them is there compelling evidence that it eliminates toxins from our body. Some of the most popular detox regimen include:
- acupuncture;
- CEASE therapy;
- chelation therapy;
- crystal healing;
- cupping;
- detox diets;
- detox supplements;
- gua sha;
- homeopathy;
- homotoxicology;
- Kombucha;
- oil pulling;
- vaginal steaming.
Interim conclusion: non-existing diagnoses are perfect opportunities for SCAM practitioners to rip off gullible patients.
Prof Michael Frass is the undisputed star amongst researchers of homeopathy. Here are the awards and achievements that he mentions on his website:
- 1994 until 2019Head, Special Outpatient Clinic “Homeopathy in Malignant Diseases”, Department of Internal Medicine I, General Hospital of the City of Vienna
- 1992 until Feb. 2004Director, Intensivstation 13.i2, Klinik für Innere Medizin I
- 1994 until 1998 Medical Director Maimonides Center
- since May 1994Vice President of the “Medical Society for Classical Homeopathy” (ÄKH)
- since Oct. 1995Head of the Working Group for Homeopathy of the ÄKH in Vienna
- since Jan. 1998 Speaker of the ÄKH at training courses
- 1999 – 2012Training Officer of the Austrian Society for Internal and General Intensive Care Medicine (ÖGIAIM)
- 2001 until 2019 Coordinator of the lecture series “Selected chapters and scientific discussion of complementary medicine methods”, Med. Univ. Vienna, VO 560480
- May 2002 – Dec. 2005Director of the Ludwig Boltzmann Institute for Homeopathy
- since June 2003Member of the Scientific Advisory Board of the Vienna International Academy of Holistic Medicine
- 2004 until 2019Expert in Airway Management and Homeopathy in Intensive Care Medicine at the Center of Excellence in Internal Critical Care Medicine (CEMIC).
- 2005 until 2019Coordinator of the free elective “Homeopathy”, Med. Univ. Vienna, VO 562 923
- since June 2005Director, Institute for Homeopathy Research
- 2006 until 2019Member of the planning area + lecturer for the line element “Interdisciplinary Patient Management” (compulsory lecture for medical students)
- since June 2006President of the Austrian Umbrella Association for Medical Holistic Medicine.
- since Nov. 2010Chairman of the Scientific Society for Homeopathy (WissHom)
Many of my readers will remember the case of the Prof. Frass et al study of homeopathy for cancer. On this blog, we have seen several articles about it:
- Michael Frass’ research into homeopathy for cancer: “numerous breaches of scientific integrity”
- An update on the dubious cancer study by Prof Michael Frass et al
- A thorough analysis of Prof M. Frass’ recent homeopathy trial casts serious doubts on its reliability
- Homeopathy prolongs survival of lung cancer patients … Can it be true?
The study and the suspicion of scientific misconduct it raised eventually resulted in an official complaint by the Viennese Medical School to the authority that deals with suspicions of publication fraud, the ‘Austrian Agency for Scientific Integrity’. It took a very long time, but recently they have published their final on-line summary of their assessment of the case; here is my translation:
Enquiry A 2021/10:
After an Austrian university was informed externally and by name of possible scientific misconduct in a study and the resulting publication, the institution concerned submitted the already publicised suspected case in the field of applied natural sciences to the OeAWI with a request for examination by the Commission.
After establishing sufficient suspicion of various violations of good scientific practice, the Commission declared itself responsible and initiated proceedings. In the course of this, the principal investigator was given the opportunity to submit a written statement and to provide the Commission for Research Integrity Annual Report 2022 material that would help to clarify the facts of the case, which the accused submitted in large quantities.
In a very complex, comprehensive investigation, which required, among other things, the on-site inspection of original documents, the Commission was able to substantiate the suspicion of data falsification, fabrication and manipulation. In a final statement, the study director, who no longer works for the university in question, and the numerous co-authors were informed in detail about the course and results of the commission’s investigation and informed of the recommendations to the university and journal. The Commission recommended that the university concerned should consider investigating its own responsibilities and act accordingly, and that the publication should be withdrawn as a matter of urgency. The journal responsible for the publication was asked to withdraw the publication on the basis of the findings of the investigation.
Nobody who has studied the Frass paper in some detail can be surprised by the verdict. I do applaud the ‘Austrian Agency for Scientific Integrity’ for their work. Yet, I do also have some criticism: health fraud on the scale of Frass can easily costs lives. I find it therefore unacceptable that the verdict took so long to get published.
Even worse is, in my view, the fact that the journal, ‘Oncologist’, is still offering this paper today, albeit with this ‘expression of concern’:
This is an Expression of Concern regarding: Michael Frass, Peter Lechleitner, Christa Gründling, Claudia Pirker, Erwin Grasmuk-Siegl, Julian Domayer, Maximilian Hochmair, Katharina Gaertner, Cornelia Duscheck, Ilse Muchitsch, Christine Marosi, Michael Schumacher, Sabine Zöchbauer-Müller, Raj K. Manchanda, Andrea Schrott, Otto Burghuber, Homeopathic Treatment as an Add-On Therapy May Improve Quality of Life and Prolong Survival in Patients with Non-Small Cell Lung Cancer: A Prospective, Randomized, Placebo-Controlled, Double-Blind, Three-Arm, Multicenter Study, The Oncologist, Volume 25, Issue 12, December 2020, Pages e1930–e1955, https://doi.org/10.1002/onco.13548
In August 2022, the journal editors received credible information from the Austrian Agency for Research Integrity about potential data falsification and data manipulation in this article.*** While The Oncologist editorial team investigates and communicates with the corresponding author, the editors are publishing this Expression of Concern to alert readers that, pending the outcome and review of a full investigation, the research results presented may not be reliable.
Cancer patients will thus still read the dangerously misleading conclusions of the Frass fabrication: “Quality of life (QoL) improved significantly in the homeopathy group compared with placebo. In addition, survival was significantly longer in the homeopathy group versus placebo and control. A higher QoL might have contributed to the prolonged survival. The study suggests that homeopathy positively influences not only QoL but also survival. Further studies including other tumor entities are warranted.” And lives of cancer patients remain needlessly at risk. In my view, this is seriously unethical.
***As far as I know, they received credible information from others long before that!
Spinal manipulation is usually performed by a therapist (chiropractor, osteopath, physiotherpist, doctor, etc.). But many people do it themselves. Self-manipulation is by no means safer than the treatment by a therapist, it seems. We have previously seen cases where the results were dramatic:
- Spinal epidural haematoma after neck manipulation (edzardernst.com)
- A ‘Self-Chiropractic Spinal Manipulation’ that resulted in death (edzardernst.com)
Now, a further case has been reported. In this paper, American pathologists present a tragic case of fatal vertebral artery dissection that occurred as the result of self-manipulation of the cervical spine.
The decedent was a 40-year-old man with no significant past medical history. He was observed to “crack his neck” while at work. Soon after, he began experiencing neck pain, then developed stroke-like symptoms and became unresponsive. He was transported to a local medical center, where imaging showed bilateral vertebral artery dissection. His neurological status continued to decline, and brain death was pronounced several days later.
An autopsy examination showed evidence of cerebellar and brainstem infarcts, herniation, and diffuse hypoxic-ischemic injury. A posterior neck dissection was performed to expose the vertebral arteries, which showed grossly visible hemorrhage and dilation. There was no evidence of traumatic injury to the bone or soft tissue of the head or neck. Bilateral dissection tracts were readily appreciated on microscopic examination. Death was attributed to self-manipulation of the neck, which in turn led to bilateral vertebral artery dissection, cerebellar and brainstem infarcts, herniation, hypoxic-ischemic injury, and ultimately brain death.
It seems clear to me that only few and spectacular cases of this nature are being published. In other words, the under-reporting of adverse effects of self-manipulation must be close to 100%. It follows that the risk of sel-manipulation is impossible to quantify. I suspect it is substancial. In any case, the precautionary principle compells me to re-issue my warning:
do not allow anybody to manipulate your neck, not even yourself!
In spite of the safety and efficiency of the COVID-19 vaccines and the many promotion efforts of political and expert authorities, a fair portion of the population remained hesitant if not opposed to vaccination. Public debate and the available literature point to the possible role of people’s attitudes towards medical institutions as well as their preference for so-called alternative medicine (SCAM) on their motivations and intentions to be vaccinated. Other potential ideological factors are beliefs about environmental laissez-faire and divine providence insofar as they encourage people to let the pandemic unfold without human interference.
In three cross-sectional samples (total N = 8214), collected at successive moments during the Belgian vaccination campaign, the present research examines the distal role of these psychological and ideological factors on vaccination intentions via motivational processes.
- Study 1 gauges the relation between trust in medical institutions and preference for SCAM on intentions to get vaccinated via motivations.
- Study 2 examines the role of beliefs in the desirability of letting nature take its course (‘environmental laissez-faire beliefs’) on vaccination intention via motivations.
- Study 3 tests whether people’s adherence to environmental laissez-faire and beliefs about divine providence are linked to their motivations for vaccination via trust in the medical institutions and SCAM.
The results show that adherence to SCAM has a deleterious effect on vaccination intentions, whereas trust in medical institutions has a positive effect. Both ideological factors pertaining to external control are only moderately related, with environmental laissez-faire beliefs having stronger effects on SCAM, medical trust and vaccination motivations.
The evidence of an association between SCAM and willingness to get vaccinated is undeniable. On this blog, we have discussed it repeatedly, e.g.:
- Use of so-called alternative medicine (SCAM) and its association with SARS-CoV-2 vaccination status
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- Andrew Wakefield, Donald Trump, SCAM, and the anti-vaccination cult
- Measles are back – not least thanks to so-called alternative medicine (SCAM), I fear
- Reasons for parental hesitancy or refusal of childhood vaccination
- Endorsement of so-called alternative medicine (SCAM) and vaccine hesitancy among physicians
- Are people who oppose COVID-19 vaccinations intellectually challenged?
- So-called alternative medicine (SCAM) and vaccine hesitancy among physicians: findings from Germany, Finland, Portugal, and France
- Interest in so-called alternative medicine is linked to vaccination coverage
- Misinformation and conspiratorial thinking are at the heart of so-called alternative medicine(SCAM)
- Vaccination rates of Canadian healthcare professionals: those of chiropractors and naturopaths are at the lowest
- Echo chambers of vaccine hesitancy and so-called alternative medicine (SCAM)
- Preference of so-called alternative medicine predicts negative attitudes to vaccination
- What are the reasons for opposing COVID vaccinations?
- Anti-vax arguments used by proponents of SCAM are stupid, or wrong, or both
But what exactly is the nature of this association?
- Does SCAM-use predispose to vaccination hesitancy?
- Does Vaccination hesitancy predispose to SCAM use?
- Is both true?
After reading all this research that has emerged on the subject, I get the impression that we are mostly dealing here with a cross-correlation where a certain mind-set of being
- prone to conspiracy theories,
- anti-establishment,
- anti-science,
- irrational,
- of low intelligence,
- unable of critical thinking,
- etc., etc,
determines both the SCAM-use and the vaccination hesitancy.
Lumbar stabilization exercises (LSEs) are said to be beneficial for chronic mechanical low back pain (CMLBP). However, further research focusing on intervention combinations is recommended. This study examined the effect of kinesio tape (KT) with LSEs on CMLBP adult patients.
A randomized blinded clinical trial was conducted. Fifty CMLBP patients of both genders were assigned into one of two groups and received 8 weeks of treatment:
- group A (control): LSEs only,
- group B (experimental): KT with LSEs.
The primary outcome was back disability, measured by the Oswestry disability index. Secondary outcomes included pain intensity, trunk extensor endurance, and sagittal spinal alignment, as indicated by the visual analog scale, Sorensen-test, and C7–S1 sagittal vertical axis, respectively. The reported data was analyzed by a two-way MANOVA using an intention-to-treat procedure.
Multivariate tests indicate statistically significant effects for group (F = 4.42, p = 0.005, partial η2 = 0.148), time (F = 219.55, p < 0.001, partial η2 = 0.904), and group-by-time interaction (F = 3.21, p = 0.01, partial η2 = 0.149). Univariate comparisons between groups revealed significant reductions in the experimental group regarding disability (p = 0.029, partial η2 = 0.049) and pain (p = 0.001, partial η2 = 0.102) without a significant difference in the Sorensen test (p = 0.281) or C7–S1 SVA (p = 0.491) results. All within-group comparisons were statistically significant (p < 0.001).
The authors concluded that the combination of KT and LSEs is an effective CMLBP treatment option. Although patients in both groups displayed significant changes in all outcomes, the combined interventions induced more significant reductions in back disability and pain intensity.
One of the main reason for conducting a controlled clinical trial is to determine whether the intervention, rather than some other factor, was the cause of the observed outcome. Yet, these trials can be designed in such a way that they mislead us on precisely this point. The present study is an example for such a case.
The authors leave us in no doubt that the KT was the cause of the positive outcome. However, they might be entirely wrong. Here are some other possibilities:
- the extra attention might have done the trick;
- the ritual of applying KT must have an effect;
- the expectation of the patient could have influenced the outcome;
- verbal or non-verbal communication between the patient and the therapist would have had an effect.
I know, it is often difficult to control for such influences in clinical trials. But, if it proves to be impossible [and in the case of KT it probably is possible], one should at the very least be cautious when drawing conclusions from the results. I suggest something like this:
The combination of KT and LSEs generated better outcomes than LSE alone. Whether this is due to specific effects of KT or non-specific context effects remains unclear.
I had never heard of him – but after getting insulted by ‘Dr. Nick Campos’ I became interested and looked him up. What I found was interesting. Here is how he describes himself.
Dr. Nick Campos is a teacher of universal principles and truths as they pertain to the health, wellness and evolution of body, mind and spirit, particularly as they relate to human growth and potential.
As a healer trained in the art of chiropractic, and as a prominent chiropractic sports physician, he has helped thousands of people overcome physical injury and trauma, allowing them to regain their functional lives.
Dr. Campos believes that wellness encompasses more than just the physical body, so a balanced mental and spiritual life is also necessary for full expression of being. Therefore, Dr. Campos assists people with mental and spiritual challenges and misperceptions, while teaching them tools to empower themselves in all areas of life.
Dr. Campos teaches universal principles of health, wellness, growth and evolution as they pertain to body, mind and spirit. His work is carried out through several media including books, articles and a widely-read, syndicated blog (Optimal Health). His book The Six Keys to Optimal Health is the quintessential guide to achieving and maintaining optimal wellness in the twenty-first century. Dr. Campos’ mission is to inspire people to adopt a new way of thinking and living.
In 2010 Dr. Campos launched his evolutionary personal growth and development consulting business dedicated to helping people tune-into and manifest their most inspired dreams. As the Dream Designer™, Dr. Campos shows people how to uncover their life’s purpose, and how to implement powerful strategies designed to create the life of their dreams.
Dr. Nick Campos has a planetary vision of impacting billions of people for years to come. His inspired mission is to help people tap into their incredible self-healing, self-regulating powers. With certainty and gratitude, he aims to teach the world the power inherent in the human mind, and prepare humankind for the next phase of planetary evolution. As the world changes rapidly, those that adapt steadily and most-balanced will have the greatest advantage to navigating new horizons.
Many people limp through their lives following other people’s standards, and striving for achievement in areas not really inspiring to them. As a result, they end up suffering from frustration, lack of fulfillment and potentially depression. Does this sound like you?
By not following your innermost drives, or by repressing your true heart’s desires, you run the greatest risk of succumbing to physical and mental pressures, strain and ultimately illness. Life can be stressful enough without the added anxiety of not knowing who you are or where you are going.
Chronic fatigue syndrome and fibromyalgia are modern manifestations of this lack of purpose, but that doesn’t have to be your destiny.
Dream Design consulting services starts by helping you tune-in to your most authentic self—who you are, what you value, and how your body and mind work to direct you down your most inspired path. You will uncover the fears, resentments and infatuations that have been acting as barriers to your personal growth, and learn effective ways to overcome them.
And Dr Campos gives courses. On his website, we currently find Upcoming dates:
January 14, 2023 Burbank, CA
January 26, 2023 Palm Desert, CA
February 11, 2023 Thousand Oaks, CA
February 23, 2023 Palm Desert, CA
March 11, 2023 Burbank, CA
March 25, 2023 Palm Desert, CA
______________________________
Either this line of his business is not doing all that well or he offers time travel as part of the package.
On X 9formally Twitter), ,Dr’ Campos called me a LOSER – perhaps I should return the compliment?
An article about chiropractic caught my attention. Let me show you its final section which, I think, is relevant to what we often discuss on this blog:
If chiropractic treatment is unscientific, then why do I feel better? Because lots of things alleviate pain. Massage, analgesia and heat – but also a provider who listens, empathises and bothers to examine a patient. Then there is the placebo effect. For centuries, doctors have recognised that different interventions with unclear pathways result in clinical improvement. Among the benefits patients attributed to placebo 100 years ago: “I sleep better; my appetite is improved; my breathing is better; I can walk further without pain in my chest; my nerves are steadier.” Nothing has changed. Pain is a universal assignment; no one has a monopoly on its relief.
The chiropractic industry owes its existence to a ghost. Its founder, David Palmer, wrote in his memoir The Chiropractor that the principles of spinal manipulation were passed on to him during a séance by a doctor who had been dead for half a century. Before this, Palmer was a “magnetic healer”.
Today, chiropractors preside over a multibillion-dollar regulated industry that draws patients for various reasons. Some can’t find or afford a doctor, feel dismissed, or worse, mistreated. Others mistrust the medical establishment and big pharma. Still others want natural healing. But none of these reasons justifies conflating a chiropractor with a doctor. The conflation feels especially hazardous in an environment of health illiteracy, where the mere title of doctor confers upon its bearer strong legitimacy.
Chiropractors don’t have the same training as doctors. They cannot issue prescriptions or order advanced imaging. They do not undergo lifelong peer review or open themselves to monthly morbidity audits.
I know that doctors could do with a dose of humility, but I can’t find any evidence (or the need) for the assertion on one website that chiropractors are “academic overachievers”. Or the ambit claim that most health professionals have no idea how complicated the brain is, but chiropractors do.
Forget doctors, patients deserve more respect.
My friend’s back feels better for now. When it flares, I wonder if she will seek my advice – and I am prepared to hear no. Everyone is entitled to see a chiropractor. But no patient should visit a chiropractor thinking that they are seeing a doctor.
______________________
I would put it more bluntly:
- chiropractors are poorly trained; in particular, they do not learn to question their own, often ridiculous beliefs;
- they are poorly regulated; in the UK, the GCC seems to protect the chiros rather than the public;
- chiropractors regularly disregard essential rules of medical ethics, e.g. informed consent;
- many try to mislead us by pretending they are physicians;
- their hallmark intervention, spinal manipulation, can cause considerable harm;
- it generates hardly any demonstrable benefit for any condition;
- chiropractors also cause considerable harm, e.g. by interfering with real medicine, e.g. vaccinations;
- thus, in general, chiropractors do more harm than good;
- yes, everyone is entitled to see a chiropractor, but before they do, reliable information should be mandatory.
The Amercian Medical Association (AMA) recently published a lengthy article on naturopathy in the US. Here are some excerpts:
There are three types of health professionals who offer naturopathic treatment:
- Naturopathic doctors. These nonphysicians graduate from a four-year, professional-level program at an accredited naturopathic medical school, earning either the doctor of naturopathy (ND) degree or the doctor of naturopathic medicine (NMD) degree.
- Traditional naturopaths, who have obtained education through some combination of a mentorship program with another professional or at an alternative clinic, distance-learning program or classroom schooling on natural health, or other holistic studies.
- Other health professionals such as chiropractors, massage therapists, dentists, nurses, nutritionists, or physicians who practice under a professional license but include some naturopathic methods in their practice and who may have studied on their own or taken courses on naturopathic methods.
At least 24 states and the District of Columbia regulate the practice of naturopathy. In order to be licensed, naturopaths in these states must earn an ND or NMD from an accredited naturopathic program and pass the Naturopathic Physicians Licensing Exam. Three states—Florida, South Carolina and Tennessee—prohibit the practice of naturopathy. In states that neither license nor prohibit the practice of naturopathy, traditional naturopaths and NDs alike may practice without being subject to state regulation.
Postgraduate training is neither common nor required of graduates of naturopathic schools, except in Utah … less than 10% of naturopaths participate in an approved residency, and such residencies last only a year and lack a high degree of standardization.
… naturopaths are required to get at least 1,200 hours of direct patient contact, physicians get 12,000–16,000 hours of clinical training…
ND programs emphasize naturopathic principes—for example, the healing power of nature—and naturopathic therapeutics such as botanical medicine, homeopoathy and hydrotherapy. Coursework in naturopathic therapeutics is combined with, and taught alongside, coursework in sciences. But there are no specifications around the number of hours required in each area … naturopathic students may lack exposure to key clinical scenarios in the course of their training … naturopathic students’ clinical experience is typically gained through outpatient health care clinics, as naturopathic medical schools typically do not have significant hospital affiliation. This means there is no guarantee that a naturopathic student completing a clinical rotation will see patients who are actually sick or hospitalized, and they may not be exposed to infants, children, adolescents or the elderly. It has been said that naturopaths tend to treat the “worried well.”
… Naturopaths claim they are trained as primary care providers and, as such, are educated and trained to diagnose, manage and treat many conditions, including bloodstream infections, heart disease and autoimmune disorders. Yet their education and training falls several years and thousands of hours short of what physicians get.
…The AMA believes it is the responsibility of policymakers to ensure that naturopaths’ claims that they can treat a broad range of conditions are backed by facts—facts that include the specific education and training necessary to ensure patient safety.
________________
The AMA is clearly cautious here. A less polite statement might simply stress that naturopaths are taught a lot of nonsense which they later tend to administer to their unsuspecting patients. On this blog, we have repeatedly discussed the danger naturopaths present to public health in the US and elsewhere, e.g.:
- How reliable are the claims made by naturopathic influencers?
- Naturopath jailed for selling fraudulent vaccination documents
- Naturopath fined for misdiagnosing and treating a rectal tumor for hemorrhoids
- Naturopaths are ‘not bound by science,’ lawyer argues
- Vaccination rates of Canadian healthcare professionals: those of chiropractors and naturopaths are at the lowest
- Is veterinary naturopathy animal abuse?
- Naturopathic ‘cancer specialist’ using coffee enemas found guilty
- Patients consulting chiropractors, homeopaths, or naturopaths are less likely to agree to the flu jab
- A naturopath responsible for the death of two cancer patients was sentenced to two years
- A naturopath in court after two of his cancer patients died
- Many naturopaths, homeopaths, and chiropractors are a risk to public health
- Naturopath treats autism with fecal transplants
- A naturopath promoting fake news about COVID vaccinations
- Naturopathy (according to the WNF) = quackery steeped in obsolete fantasies
- Canadian naturopaths may no longer call themselves ‘medically trained’
- Naturopaths’ counselling against vaccinations could be criminally negligent
- Naturopathy for cancer … claims that have the potential to be lethal
- Severe liver injury due to naturopaths’ prescription of Epsom salt
- Naturopaths should not treat children
- Some naturopaths are clearly a danger to public health
- Death of a child through naturopathy
Claims that naturopaths are a viable alternative to evidence-based medicine are wrong, irresponsible and dangerous. Regulators must be reminded that they have the duty to protect the public from charlatans and should therefore ensure that no false therapeutic or diagnostic claims can be made by naturopaths.
I usually take ‘market reports’ with a pinch of salt. Having said that, this document makes some rather interesting predictions:
The size of the market for so-called alternative medicine (SCAM) is projected to expand from USD 147.7 billion in 2023 to approximately USD 1489.4 billion by the year 2033. This projection indicates a remarkable Compound Annual Growth Rate (CAGR) of 26% over the forecast period.
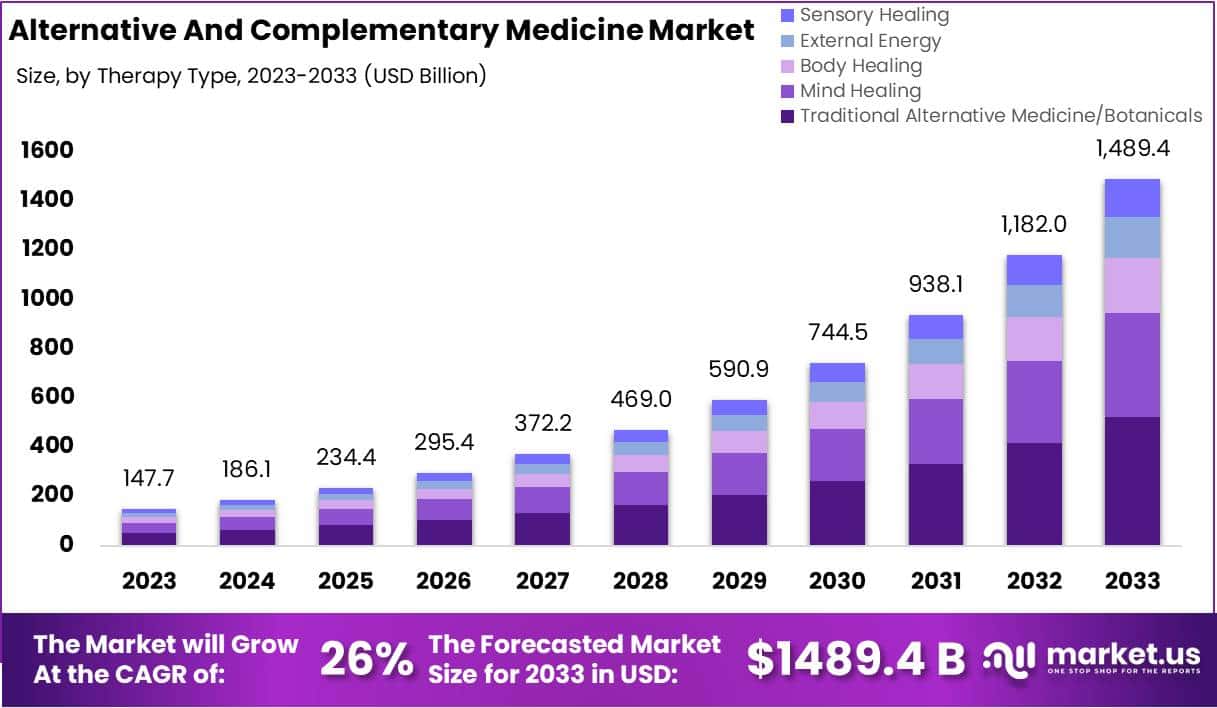
The market for SCAM is experiencing significant growth, fueled by increasing consumer interest in natural and holistic health solutions. This trend reflects a broader shift in societal attitudes towards health and wellness, emphasizing preventive care and natural health practices.
The market’s dynamics are influenced by various factors, including consumer preferences, regulatory standards, and evolving perceptions of health and wellness. As the popularity of these alternative therapies grows, it is crucial for individuals to consult with healthcare professionals to ensure that these non-conventional approaches are safely and effectively incorporated into their overall health regimen. The increasing acceptance of SCAM underscores a collective move towards more personalized and holistic healthcare solutions, resonating with today’s health-conscious consumers.
In 2023, Traditional Alternative Medicine/Botanicals led the market, capturing a 35.2% share, which reflects a strong consumer inclination towards these treatments. Dietary Supplements were prominent in the market, securing a 25.1% share in 2023, which underscores the high consumer demand for nutritional aids. Direct Sales were the most favored distribution channel, accounting for 43.2% of the market share in 2023, which indicates their significant impact on guiding consumer purchases. Pain Management was the predominant application area, holding a 24.9% market share in 2023, propelled by the growing acknowledgment of non-pharmacological treatment options. Adults represented a substantial portion of the market, making up 62.33% in 2023, signifying a marked preference for SCAM therapies within this age group. Europe stood out as the market leader, claiming a 42.6% share in 2023, a position supported by widespread acceptance, governmental backing, and an increasing elderly population. The regions of North America and Asia-Pacific are highlighted as areas with potential, signaling opportunities for market expansion beyond the European stronghold in the upcoming years.
Leading Market Players Are:
- Columbia Nutritional
- Nordic Nutraceuticals
- Ramamani Iyengar Memorial Yoga Institute
- The Healing Company Ltd.
- John Schumacher Unity Woods Yoga Centre
- Sheng Chang Pharmaceutical Company
- Pure encapsulations LLC.
- Herb Pharm
- AYUSH Ayurvedic Pte Ltd.
Recent developments:
- In December 2023, Adoratherapy launched the Alkemie Chakra Healing Line, an aromatherapy range aimed at harmonizing the seven chakras.
- Coworth Park introduced the Hebridean Sound Treatment in October 2023, merging traditional Hebridean sounds with guided meditation to offer a novel, restorative wellness experience.
- The World Health Organization released draft guidelines in September 2023 for the safe, effective application of traditional medicines.
- Telehealth services, expanding significantly in August 2023, have broadened the reach of SCAM, enhancing patient access to these treatments.
