panacea
Of all the many forms of so-called alternative medicine (SCAM), Reiki is perhaps the one that has the least plausibility. It assumes that a Reiki healer can send healing energy into the body of a patient which, in turn, stimulates the self-healing ability of the body and thus cures illness. Neither the source of the energy, its nature, or its effects have ever been convincingly demonstrated. These facts, however, do not stop enthusiasts to conduct clinical trials of Reiki.
The aim of this randomised clinical trial was to investigate the effect of the application of Reiki on fatigue and sleep quality in people with MS. A total of 60 people (control group = 30, intervention group = 30) participated in this study. Personal Information Form, Piper Fatigue Scale (PFS) and Pittsburg Sleep Quality Index (PSQI) were used as endpoints.
It was found that the PFS and PSQI total and subcomponent scores of the intervention group decreased after Reiki compared to the control group and this was statistically significant (p<0.05). The study showed that Reiki was significantly effective in improving fatigue and sleep quality in people with MS.
The authors concluded that, as Reiki is a simple, inexpensive and accessible method, it was suggested that its use in the management of MS should be encouraged and maintained in nursing practice.
In the introduction, the authors state this:
Reiki is a non-invasive, low-cost, easy-to-apply practice with no side effects and no negative effects on the existing treatment, and prevents acute and chronic conditions. It is frequently preferred in rehabilitation centres, emergency care units, nursing homes, elderly care centres, paediatrics, psychiatry, obstetrics and gynaecology clinics. Reiki can be applied by trained practitioners such as health professionals who have received first level reiki training in hospitals and clinics, caregivers or patients themselves. Reiki can be administered from with the patient or remotely when the patient and practitioner are in separate locations. Both types of Reiki are based on the premise of a universal source of healing energy that the Reiki practitioner can channel through intention.
For me, this begs the questions:
- If all of this were true, why do we need a study?
- If anyone believes such BS, are they the ideal people to conduct a study of Reiki?
Anyway, we should ask why this study generated a positive result. The most plausible explanation is that, as the study was not blind, the Reiki healers managed to maximise patient expectation. This, in turn, has generated a placebo respose which affected the subjective outcome measures. In other words, Reiki has no specific effect but patients tend to improve because of non-specific effects.
This study tested the efficacy and safety of individualized homeopathic medicines (IHMs) in treating hemorrhoids compared with placebo. The double-blind, randomized (1:1), two parallel arms, placebo-controlled trial was conducted at the surgery outpatient department of the State National Homoeopathic Medical College and Hospital, Lucknow, Uttar Pradesh, India.
Patients were 140 women and men, aged between 18 and 65 years, with a diagnosis of primary hemorrhoids grades I-III for at least 3 months. Excluded were the patients with grade IV hemorrhoids, anal fissure, and fistula, hypertrophic anal papillae, inflammatory bowel disease, coagulation disorders, rectal malignancies, obstructed portal circulation, patients requiring immediate surgical intervention, and vulnerable samples.
Patients were randomized to Group 1 (n = 70; IHMs plus concomitant care; verum) and Group 2 (n = 70; placebos plus concomitant care; control). Primary-the anorectal symptom severity and quality-of-life (ARSSQoL) questionnaire, and secondary-the EuroQol 5-dimensions 5-levels (EQ-5D-5L) questionnaire and EQ visual analogue scale (VAS); all of them were measured at baseline, and every month, up to 3 months.
Out of the 140 randomized patients, 122 were protocol compliant. Intention-to-treat sample (n = 140) was analyzed. The level of significance was set at p < 0.05 two tailed. Statistically significant between-group differences were elicited in the ARSSQoL total (Mann-Whitney U [MWU]: 1227.0, p < 0.001) and EQ-5D-5L VAS (MWU: 1228.0, p = 0.001) favoring homeopathy against placebos. Sulfur was the most frequently prescribed medicine. No harm or serious adverse events were reported from either of the groups.
The authors concluded that IHMs demonstrated superior results over placebo in the short-term treatment of hemorrhoids of grades I-III. The findings are promising, but need to be substantiated by further phase 3 trials.
Yes, I know: it is not easy to keep a straight face when reading such a paper. And the task is not made easier when considering the affiliations of its authors:
- 1East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre, Under Department of Health & Family Welfare, Government of West Bengal, India, South 24 Parganas, India.
- 2Department of Organon of Medicine and Homoeopathic Philosophy, State National Homoeopathic Medical College and Hospital, Lucknow, India.
- 3Department of AYUSH, Government of Uttar Pradesh, Lucknow, India.
- 4State National Homoeopathic Medical College and Hospital, Lucknow, India.
- 5Department of Materia Medica, State National Homoeopathic Medical College and Hospital, Lucknow, India.
- 6Department of Pathology & Microbiology, D. N. De Homoeopathic Medical College & Hospital, Government of West Bengal, Kolkata, India.
- 7Department of Pathology & Microbiology, Mahesh Bhattacharyya Homoeopathic Medical College & Hospital, Government of West Bengal, Howrah, India.
- 8Department of Repertory, D. N. De Homoeopathic Medical College and Hospital, Kolkata, India.
Let’s nevertheless ask three serious questions:
- According to classical homeopathy, for a cure, one needs a remedy that, when given to a healthy volunteer, causes the symptom one wants to treat. So, does sulfur etc.cause the symptoms of hemorrhoids?
- According to classical homeopathy, the remedy is supposed to cure the condition, not alleviate the symptoms. Is that what the results show?
- Is it plausible that homeopathy can have any effects on hemorrhoids?
I am confident that the answers are: no, no and no.
And this leads me to ask my final question: do we believe these findings?
I let you answer this one!
This review aimed to assess the therapeutic efficacy of Reiki therapy in alleviating anxiety.
In adherence to academic standards, a thorough search was conducted across esteemed databases such as PubMed, Web of Science, Science Direct, and the Cochrane Library. The primary objective of this search was to pinpoint peer-reviewed articles published in English that satisfied specific criteria: (1) employing an experimental or quasi-experimental study design, (2) incorporating Reiki therapy as the independent variable, (3) encompassing diverse patient populations along with healthy individuals, and (4) assessing anxiety as the measured outcome.
The study involved 824 participants, all of whom were aged 18 years or older. Reiki therapy was found to have a significant effect on anxiety intervention(SMD=-0.82, 95CI -1.29∼-0.36, P = 0.001). Subgroup analysis indicated that the types of subjects (chronically ill individuals and the general adult population) and the dosage/frequency of the intervention (≤ 3 sessions and 6–8 sessions) were significant factors influencing the variability in anxiety reduction.
The authors concluded that short-term Reiki therapy interventions of ≤ 3 sessions and 6–8 sessions have demonstrated effectiveness in reducing health and procedural anxiety in patients with chronic conditions such as gastrointestinal endoscopy inflammation, fibromyalgia, and depression, as well as in the general population. It is important to note that the efficacy of Reiki therapy in decreasing preoperative anxiety and death-related anxiety in preoperative patients and cancer patients is somewhat less consistent. These discrepancies may be attributed to individual pathophysiological states, psychological conditions, and treatment expectations.
_______________________
This is a truly stunning finding considering that few treatments are less plausible that Reiki. I strongly suspect that these conclusions are not tenable. To see whether this is true, we must look at the primary studies (tedious, I know, but can’t be helped). Here are the abstracts of the 13 studies included in this review:
Purpose: The purpose of the study was to investigate changes in the anxiety levels of patients receiving preoperative Reiki.
Material and methods: This study used a quasi-experimental model with a pretest-posttest control group.
Methods: Subjects (n = 210) were recruited from a hospital in Turkey, from June 2013 to July 2014. Subjects were then assigned to experimental (n = 105) and control (n = 105) groups.
Results: The level of anxiety of experimental group patients did not change according to their state anxiety scores (p > 0.10); however, the anxiety level of control group patients increased (p < 0.001).
Conclusion: The results of this study imply that the administration of Reiki is effective in controlling preoperative anxiety levels and in preventing them from increasing.
I am not sure what is meant by “a quasi-experimental model with pretest- posttest control group”. Yet, I suspect this was not a properly randomised trial and should thus have been exclused from the review. There was no control of placebo effects.
Fatigue is an extremely common side effect experienced during cancer treatment and recovery. Limited research has investigated strategies stemming from complementary and alternative medicine to reduce cancer-related fatigue. This research examined the effects of Reiki, a type of energy touch therapy, on fatigue, pain, anxiety, and overall quality of life. This study was a counterbalanced crossover trial of 2 conditions: (1) in the Reiki condition, participants received Reiki for 5 consecutive daily sessions, followed by a 1-week washout monitoring period of no treatments, then 2 additional Reiki sessions, and finally 2 weeks of no treatments, and (2) in the rest condition, participants rested for approximately 1 hour each day for 5 consecutive days, followed by a 1-week washout monitoring period of no scheduled resting and an additional week of no treatments. In both conditions, participants completed questionnaires investigating cancer-related fatigue (Functional Assessment of Cancer Therapy Fatigue subscale [FACT-F]) and overall quality of life (Functional Assessment of Cancer Therapy, General Version [FACT-G]) before and after all Reiki or resting sessions. They also completed a visual analog scale (Edmonton Symptom Assessment System [ESAS]) assessing daily tiredness, pain, and anxiety before and after each session of Reiki or rest. Sixteen patients (13 women) participated in the trial: 8 were randomized to each order of conditions (Reiki then rest; rest then Reiki). They were screened for fatigue on the ESAS tiredness item, and those scoring greater than 3 on the 0 to 10 scale were eligible for the study. They were diagnosed with a variety of cancers, most commonly colorectal (62.5%) cancer, and had a median age of 59 years. Fatigue on the FACT-F decreased within the Reiki condition (P=.05) over the course of all 7 treatments. In addition, participants in the Reiki condition experienced significant improvements in quality of life (FACT-G) compared to those in the resting condition (P <.05). On daily assessments (ESAS) in the Reiki condition, presession 1 versus postsession 5 scores indicated significant decreases in tiredness (P <.001), pain (P <.005), and anxiety (P<.01), which were not seen in the resting condition. Future research should further investigate the impact of Reiki using more highly controlled designs that include a sham Reiki condition and larger sample sizes.
This was a pilot study which should not report efficacy outcomes merely test the feasibility of a definitive trial. There was no control of placebo effects.
Purpose: This study’s aim is to determine the effect of Reiki when applied before upper gastrointestinal endoscopy on levels of anxiety, stress, and comfort.
Design: This single-blind, a pretest and post-test design, randomized, sham-controlled study was held between February and July 2021.
Methods: Patients who met the inclusion criteria were separated by randomization into three groups: Reiki, sham Reiki, and control. A total of 159 patients participated in the study. In the intervention groups (Reiki and sham Reiki), Reiki and sham Reiki were applied once for approximately 20 to 25 minutes before gastrointestinal endoscopy.
Findings: When the Reiki group was compared to the sham Reiki and control groups following the intervention, the decrease in the levels of patient stress (P < .001) and anxiety (P < .001) and the increase in patient comfort (P < .001) were found to be statistically significant.
Conclusions: Reiki applied to patients before upper gastrointestinal endoscopy was effective in reducing stress and anxiety and in increasing comfort.
Here an attempt was made to control for placebo effects and to blind patients. Whether the latter was successful was not tested. Thus a placebo effects cannot be excluded.
The purpose of this study was to evaluate the effect of Reiki as an alternative and complementary approach to treating community-dwelling older adults who experience pain, depression, and/or anxiety. Participants (N = 20) were randomly assigned to either an experimental or wait list control group. The pre- and posttest measures included the Hamilton Anxiety Scale, Geriatric Depression Scale-Short Form, Faces Pain Scale, and heart rate and blood pressure. The research design included an experimental component to examine changes in these measures and a descriptive component (semi-structured interview) to elicit information about the experience of having Reiki treatments. Significant differences were observed between the experimental and treatment groups on measures of pain, depression, and anxiety; no changes in heart rate and blood pressure were noted. Content analysis of treatment notes and interviews revealed five broad categories of responses: Relaxation; Improved Physical Symptoms, Mood, and Well-Being; Curiosity and a Desire to Learn More; Enhanced Self-Care; and Sensory and Cognitive Responses to Reiki.
No attempt to control for placebo effects.
Purpose: The purpose of this randomized pilot was to determine feasibility of testing Reiki, a complementary therapy intervention, for women undergoing breast biopsy (BB).
Background: Increasingly women face the possibility of BB, the definitive test for breast cancer. Psychological distress associated with BB includes anxiety and depression. Reiki was proposed as an intervention to decrease anxiety and promote relaxation.
Method: Thirty-two women scheduled for BB were randomized to Reiki intervention versus conventional care control. Anxiety and depression were evaluated using self-report questionnaires.
Findings: Analysis found no significant mean differences between groups over time. Comparably low baseline anxiety levels (possible selection bias) decreased naturally with time allowing little room for observing treatment effect.
Conclusions: Reiki, when administered in the naturalistic setting of a complementary therapy office, did not suggest evidence of efficacy. An intervention offered within the bounds of the conventional care setting may be more feasible for addressing BB distress.
The study failed to produce a positive finding.
The aim of this study was to investigate the effect of Reiki on pain, anxiety, and hemodynamic parameters on postoperative days 1 and 2 in patients who had undergone cesarean delivery. The design of this study was a randomized, controlled clinical trial. The study took place between February and July 2011 in the Obstetrical Unit at Odemis Public Hospital in Izmir, Turkey. Ninety patients equalized by age and number of births were randomly assigned to either a Reiki group or a control group (a rest without treatment). Treatment applied to both groups in the first 24 and 48 hours after delivery for a total of 30 minutes to 10 identified regions of the body for 3 minutes each. Reiki was applied for 2 days once a day (in the first 24 and 48 hours) within 4-8 hours of the administration of standard analgesic, which was administered intravenously by a nurse. A visual analog scale and the State Anxiety Inventory were used to measure pain and anxiety. Hemodynamic parameters, including blood pressure (systolic and diastolic), pulse and breathing rates, and analgesic requirements also were recorded. Statistically significant differences in pain intensity (p = .000), anxiety value (p = .000), and breathing rate (p = .000) measured over time were found between the two groups. There was a statistically significant difference between the two groups in the time (p = .000) and number (p = .000) of analgesics needed after Reiki application and a rest without treatment. Results showed that Reiki application reduced the intensity of pain, the value of anxiety, and the breathing rate, as well as the need for and number of analgesics. However, it did not affect blood pressure or pulse rate. Reiki application as a nursing intervention is recommended as a pain and anxiety-relieving method in women after cesarean delivery.
No control for placebo effects.
Objective: to evaluate the effectiveness of massage and reiki in the reduction of stress and anxiety in clients at the Institute for Integrated and Oriental Therapy in Sao Paulo (Brazil).
Method: clinical tests randomly done in parallel with an initial sample of 122 people divided into three groups: Massage + Rest (G1), Massage + Reiki (G2) and a Control group without intervention (G3). The Stress Systems list and the Trace State Anxiety Inventory were used to evaluate the groups at the start and after 8 sessions (1 month), during 2015.
Results: there were statistical differences (p = 0.000) according to the ANOVA (Analysis of Variance) for the stress amongst the groups 2 and 3 (p = 0.014) with a 33% reductions and a Cohen of 0.78. In relation to anxiety-state, there was a reduction in the intervention groups compared with the control group (p < 0.01) with a 21% reduction in group 2 (Cohen of 1.18) and a 16% reduction for group 1 (Cohen of 1.14).
Conclusion: Massage + Reiki produced better results amongst the groups and the conclusion is for further studies to be done with the use of a placebo group to evaluate the impact of the technique separate from other techniques.
No control for placebo effects.
This randomized controlled study aimed to determine the effect of Reiki and aromatherapy on vital signs, oxygen saturation, and anxiety level in patients undergoing upper gastrointestinal endoscopy. The sample consisted of 100 patients divided into Reiki (n = 34), aromatherapy (n = 33), and control (n = 33) groups. Data were collected 3 times (before, during, and after the procedure) using a descriptive characteristics questionnaire, a follow-up form, and the State Anxiety Subscale. The Reiki group had a mean State Anxiety Subscale score of 53.59 ± 2.98 and 43.94 ± 4.31 before and after the procedure, respectively. The aromatherapy group had a mean State Anxiety Subscale score of 54.03 ± 4.03 and 43.85 ± 3.91 before and after the procedure, respectively. The control group had a mean State Anxiety Subscale score of 38.79 ± 4.68 and 53.30 ± 7.26 before and after the procedure, respectively (P < .05). The results showed that the Reiki and aromatherapy groups had significantly lower State Anxiety Subscale scores than the control group after the procedure, indicating that Reiki and aromatherapy help reduce anxiety levels. There was a significant difference in the mean respiratory rates and oxygen saturation levels between the groups (P < .05). In conclusion, patients who do Reiki or undergo aromatherapy are less likely to experience anxiety before upper gastrointestinal endoscopy.
No control for placebo effects.
The aim of this study is to investigate the effects of Reiki application on pain, anxiety, and quality of life in patients with fibromyalgia. The study was completed with a total of 50 patients: 25 in the experimental group and 25 in the control group. Reiki was applied to the experimental group and sham Reiki to the control group once a week for 4 weeks. Data were collected from the participants using the Information Form, Visual Analog Scale, McGill-Melzack Pain Questionnaire, State-Trait Anxiety Inventory, and Short Form-36. There was a significant difference between the mean Visual Analog Scale pain scores during and before the first week (P = .012), second week (P = .002), and fourth week (P = .020) measurements of the individuals in the experimental and control groups, after application. In addition, at the end of the 4-week period, the State Anxiety Inventory (P = .005) and the Trait Anxiety Inventory (P = .003) were significantly decreased in the Reiki group compared with the control group. Physical function (P = .000), energy (P = .009), mental health (P = .018), and pain (P = .029) subdimension scores of quality of life in the Reiki group increased significantly compared with the control group. Reiki application to patients with fibromyalgia may have positive effects on reducing pain, improving quality of life, and reducing state and trait anxiety levels.
Here an attempt was made to control for placebo effects and to blind patients. Whether the latter was successful was not tested. Thus a placebo effects cannot be excluded. The sample size was small.
Background: Reiki is a biofield therapy which is based on the explanatory model that the fields of energy and information of living systems can be influenced to promote relaxation and stimulate a healing response.
Objective: To conduct a pragmatic within-subject pilot trial of a remote Reiki program for frontline healthcare workers’ health-related symptoms during the COVID-19 pandemic.
Methods: Healthcare professionals in the UK (eg, physicians, nurses, and paramedics) were eligible to sign up for a distance Reiki program and were also invited to participate in the research study. Eight Reiki practitioners simultaneously gave each participant Reiki remotely for 20 minutes on 4 consecutive days. Feasibility of the research was assessed, including recruitment, data completeness, acceptability and intervention fidelity, and preliminary evaluation of changes in outcome measures. Participants’ stress, anxiety, pain, wellbeing, and sleep quality were evaluated with 7-point numerical rating scales. Measures were completed when signing up to receive Reiki (pre) and following the final Reiki session (post). Pre and post data were analyzed using Wilcoxon signed ranks tests.
Results: Seventy-nine healthcare professionals signed up to receive Reiki and took the baseline measures. Of those, 40 completed post-measures after the 4-day intervention and were therefore included in the pre-post analysis. Most participants were female (97.5%), and the mean age was 43.9 years old (standard deviations = 11.2). The study was feasible to conduct, with satisfactory recruitment, data completeness, acceptability, and fidelity. Wilcoxon signed ranks tests revealed statistically significant decreases in stress (M = -2.33; P < .001), anxiety (M = -2.79; P < .001) and pain (M = -.79; P < .001), and significant increases in wellbeing (M = -1.79; P < .001) and sleep quality (M = -1.33; P = .019).
Conclusions: The Reiki program was feasible and was associated with decreased stress, anxiety and pain, and increased wellbeing and sleep quality in frontline healthcare workers impacted by the COVID-19 pandemic.
Pilot study should not report efficacy findings and should be excluded.
Background: There is a scarcity of studies in the international literature regarding alternative treatment to the pharmacological and psychotherapeutic intervention in the face of depression symptoms. This study aimed to test a protocol based on natural therapy, alternatives to pharmacological and psychotherapeutic, through Mindfulness Meditation, Reiki, Acupuncture and Auriculotherapy, to treat the symptoms of depression for those who were with no pharmacological or psychotherapeutic treatment for these symptoms.
Methods: this is a randomized single-blind controlled pilot study. The final sample was 21 participants divided in two groups: experimental and control. Participants were evaluated by validated instruments during the screening process and after the intervention. The instruments were: Depression, Anxiety and Stress Scale and Beck Depression Inventory. Intervention was performed in eight sessions, during two months. All the techniques were used in the experimental group. Analysis of variance with repeated measures was used to compare pre-intervention to post-intervention moments.
Results: the result of analysis indicates a significant reduction in the symptoms of depression after the intervention among the experimental group.
Limitations: there is no way to determine which of the techniques used produced the most significant result.
Conclusions: The protocol proposed in this study was effective in reducing the symptoms of depression to whom are not eligible for traditional treatment.
This is a pilot study and should not report efficacy findings. It is also not a study of just Reiki. It should have been excluded.
This is a constructive replication of a previous trial conducted by Bowden et al. (2010), where students who had received Reiki demonstrated greater health and mood benefits than those who received no Reiki. The current study examined impact on anxiety/depression. 40 university students-half with high depression and/or anxiety and half with low depression and/or anxiety-were randomly assigned to receive Reiki or to a non-Reiki control group. Participants experienced six 30-minute sessions over a period of two to eight weeks, where they were blind to whether noncontact Reiki was administered as their attention was absorbed in a guided relaxation. The efficacy of the intervention was assessed pre-post intervention and at five-week follow-up by self-report measures of mood, illness symptoms, and sleep. The participants with high anxiety and/or depression who received Reiki showed a progressive improvement in overall mood, which was significantly better at five-week follow-up, while no change was seen in the controls. While the Reiki group did not demonstrate the comparatively greater reduction in symptoms of illness seen in our earlier study, the findings of both studies suggest that Reiki may benefit mood.
No control for placebo effects
This is a constructive replication of a previous trial conducted by Bowden et al. (2010), where students who had received Reiki demonstrated greater health and mood benefits than those who received no Reiki. The current study examined impact on anxiety/depression. 40 university students-half with high depression and/or anxiety and half with low depression and/or anxiety-were randomly assigned to receive Reiki or to a non-Reiki control group. Participants experienced six 30-minute sessions over a period of two to eight weeks, where they were blind to whether noncontact Reiki was administered as their attention was absorbed in a guided relaxation. The efficacy of the intervention was assessed pre-post intervention and at five-week follow-up by self-report measures of mood, illness symptoms, and sleep. The participants with high anxiety and/or depression who received Reiki showed a progressive improvement in overall mood, which was significantly better at five-week follow-up, while no change was seen in the controls. While the Reiki group did not demonstrate the comparatively greater reduction in symptoms of illness seen in our earlier study, the findings of both studies suggest that Reiki may benefit mood.
This is the only rigorous study included in the review. Its findings are not easy to interpret (“For the sample as a whole, as can be seen from the total group means, there was little change over the course of the study”)
__________________________
Even though I did not have access to the full text of all of these RCTs, this analysis tells me a few important things; here are some of the main points I discovered:
- the new review is fatally flawed;
- the authors’ statement that their “article presents a systematic review of randomized controlled trials (RCTs) that were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines” is nonsensical;
- PRISMA guidelines were certainly not adhered to;
- there is no truly critical assessment of the primary studies;
- the literature searches were incomplete;
- the risk of bias tool for evaluating the primary studies was employed incorrectly;
- the review did not include all RCTs of Reiki (our own 2008 review included several trials that are not included here, and this blog has a few more);
- the review includes several studies that should have been excluded;
- most Reiki studies are of poor quality;
- with both the review and most of the primary studies, one feels a strong bias towards trying to prove that Reiki works;
- Reiki research is firmly in the hands of nurses (almost all the studies were conducted by nurses);
- almost all of the RCTs test Reiki versus no treatment, and this means that most do not control for placebo (or other non-specific) effects. In other words, the conclusions stating that Reiki is effective are simply wrong.
I am dismayed to see that a decent journal (BMC Palliative Care) published such a fatally flawed review. The paper fails to discuss any of its obvious flaws. Specifically, it does not even specify what interventions were used in the various control groups. Do the journal editors, peer-reviewers and authors not appreciate that, without such information, the findings are uninterpretable? Or do they perhaps deliberately try to mislead us?
If you ask me, this paper should be best withdrawn.
Our own review of Reiki is no longer up-to-date. Yet, it’s conclusion is, in my view, far more accurate than the one offered by the authors of the fatally flawed new review:
the evidence is insufficient to suggest that reiki is an effective treatment for any condition. Therefore the value of reiki remains unproven.
I am glad to hear that the Vatican is issueing new guidelines on supernatural phenomena. The document, compiled by the Vatican’s Dicastery for the Doctrine of the Faith, will lay out rules to assess the truthfulness of supernatural claims. Reports of such phenomena are said to have soared in recent years in an era of social media – sometimes spread through disinformation and rumour. The guidelines are likely to tighten criteria for the screening, analysis, and possible rejection of cases.
Apparitions have been reported across the centuries. Those recognised by the Church have prompted pilgrims, and popes, to visit spots where they are said to have taken place. Millions flock to Lourdes in France, for example, or Fatima in Portugal, where the Virgin Mary is alleged to have appeared to children, promising a miracle – after which crowds are said to have witnessed the sun zig-zagging through the sky. The visitation was officially recognised by the Church in 1930.
But other reports are found by church officials to be baloney. In 2016, an Italian woman began claiming regular apparitions of Jesus and Mary in a small town north of Rome after she brought back a statue from Medjugorje in Bosnia, where the Virgin Mary is also said to have appeared. Crowds prayed before the statue and received messages including warnings against same-sex marriage and abortion. It took eight years for the local bishop to debunk the story.
_________________________
Perhaps the Vatican should also have a look at faith healing*, the attempt to bring about healing through divine intervention. The Bible and other religious texts provide numerous examples of divine healing, and believers see this as a proof that faith healing is possible. There are also numerous reports of people suffering from severe diseases, including cancer and AIDS, who were allegedly healed by divine intervention.
Faith healing has no basis in science, is biologically not plausible. Some methodologically flawed studies have suggested positive effects, however, this is not confirmed by sound clinical trials. Several plausible explanations exist for the cases that have allegedly been healed by divine intervention, for instance, spontaneous remission or placebo response. Another explanation is fraud. For instance, the famous German faith healer, Peter Popoff, was exposed in 1986 for using an earpiece to receive radio messages from his wife giving him the home addresses and ailments of audience members which he purported had come from God during his faith healing rallies.
Faith healing may per se be safe, but it can nevertheless do untold indirect harm, and even fatalities are on record: “Faith healing, when added as an adjuvant or alternative aid to medical science, will not necessarily be confined to mere arguments and debates but may also give rise to series of complications, medical emergencies and even result in death.”
Alternatively, the Vatican might look at the healing potential of pilgrimages*, journeys to places considered to be sacred. The pilgrims often do this in the hope to be cured of a disease. The purpose of Christian pilgrimage was summarized by Pope Benedict XVI as follows:
To go on pilgrimage is not simply to visit a place to admire its treasures of nature, art or history. To go on pilgrimage really means to step out of ourselves in order to encounter God where he has revealed himself, where his grace has shone with particular splendour and produced rich fruits of conversion and holiness among those who believe.
There are only few scientific studies of pilgrimages. The purpose of this qualitative research was to explore whether pilgrims visiting Lourdes, France had transcendent experiences. The authors concluded that visiting Lourdes can have a powerful effect on a pilgrim and may include an “out of the ordinary” transcendent experience, involving a sense of relationship with the divine, or experiences of something otherworldly and intangible. There is a growing focus on Lourdes as a place with therapeutic benefits rather that cures: our analysis suggests that transcendent experiences can be central to this therapeutic effect. Such experiences can result in powerful emotional responses, which themselves may contribute to long term well-being. Our participants described a range of transcendent experiences, from the prosaic and mildly pleasant, to intense experiences that affected pilgrims’ lives. The place itself is crucially important, above all the Grotto, as a space where pilgrims perceive that the divine can break through into normal life, enabling closer connections with the divine, with nature and with the self.
Other researchers tested the effects of tap water labelled as Lourdes water versus tap water labelled as tap water found that placebos in the context of religious beliefs and practices can change the experience of emotional salience and cognitive control which is accompanied by connectivity changes in the associated brain networks. They concluded that this type of placebo can enhance emotional-somatic well-being, and can lead to changes in cognitive control/emotional salience networks of the brain.
The risks involved in pilgrimages is their often considerable costs. It is true, as the text above points out that “millions flock to Lourdes in France”. In other words, pilgrimiges are an important source of income, not least for the catholoc church.
A more important risk can be that they are used as an alternative to effective treatments. This, as we all know, can be fatal. As there is no good evidence that pilgrimiges cure diseases, their risk/benefit balance as a treatment of disease cannot be positive.
So, will the new rules of the Vatican curtail the risks on supernatural healing practises? I would not hold my breath!
_________________
* for references see my book from where this text has been borrowed and modified.
Whenever a journalist wants to discuss the subject of acupuncture with me, he or she will inevitably ask one question:
DOES ACUPUNCTURE WORK?
It seems a legitimate, obvious and simple question, particularly during ‘Acupuncture Awareness Week‘, and I have heard it hundreds of times. Why then do I hesitate to answer it?
Journalists – like most of us – would like a straight answer, like YES or NO. But straight answers are in short supply, particularly when we are talking about acupuncture.
Let me explain.
Acupuncture is part of ‘Traditional Chinese Medicine’ (TCM). It is said to re-balance the life forces that determine our health. As such it is seen as a panacea, a treatment for all ills. Therefore, the question, does it work?, ought to be more specific: does it work for pain, obesity, fatigue, hair-loss, addiction, anxiety, ADHA, depression, asthma, old age, etc.etc. As we are dealing with virtually thousands of ills, the question, does it work?, quickly explodes into thousands of more specific questions.
But that’s not all!
The question, does acupuncture work?, assumes that we are talking about one therapy. Yet, there are dozens of different acupuncture traditions and sites:
- body acupuncture,
- ear acupuncture,
- tongue acupuncture,
- scalp acupuncture,
- etc., etc.
Then there are dozens of different ways to stimulate acupuncture points:
- needle acupuncture,
- electroacupuncture,
- acupressure,
- moxibustion,
- ultrasound acupuncture,
- laser acupuncture,
- etc., etc.
And then there are, of course, different acupuncture ‘philosophies’ or cultures:
- TCM,
- ‘Western’ acupuncture,
- Korean acupuncture,
- Japanese acupuncture,
- etc., etc.
If we multiply these different options, we surely arrive at thousands of different variations of acupuncture being used for thousands of different conditions.
But this is still not all!
To answer the question, does it work?, we today have easily around 10 000 clinical trials. One might therefore think that, despite the mentioned complexity, we might find several conclusive answers for the more specific questions. But there are very significant obstacles that are in our way:
- most acupuncture trials are of lousy quality;
- most were conducted by lousy researchers who merely aim at showing that acupuncture works rather that testing whether it is effective;
- most originate from China and are published in Chinese which means that most of us cannot access them;
- they get nevertheless included in many of the systematic reviews that are currently being published without non-Chinese speakers ever being able to scrutinise them;
- TCM is a hugely important export article for China which means that political influence is abundant;
- several investigators have noted that virtually 100% of Chinese acupuncture trials report positive results regardless of the condition that is being targeted;
- it has been reported that about 80% of studies emerging from China are fabricated.
Now, I think you understand why I hesitate every time a journalist asks me:
DOES ACUPUNCTURE WORK?
Most journalists do not have the patience to listen to all the complexity this question evokes. Many do not have the intellectual capacity to comprehend an exhaustive reply. But all want to hear a simple and conclusive answer.
So, what do I say in this situation?
Usually, I respond that the answer would depend on who one asks. An acupuncturist is likely to say: YES, OF COURSE, IT DOES! An less biased expert might reply:
IT’S COMPLEX, BUT THE MOST RELIABLE EVIDENCE IS FAR FROM CONVINCING.
Medical Acupuncture is the name of a quarterly journal published for the ‘American Academy of Medical Acupuncture’ that publishes around 60 pro-acupuncture articles every year. Its editor is Richard C. Niemtzow, M.D., Ph.D., M.P.H. Richard is a retired US Air Force colonel who was the first full-time physician acupuncturist in the US Armed Forces. He is probably best known for his invention called ‘BATTLE FIELD ACUPUNCTURE’, a form of ear-acupuncture allegedly reducing pain in emergency situations.
Medline lists 79 papers (mostly published in 3rd class journals such as ‘Medical Acupuncture’) in Niemtzow’s name. Only one of them – 21 years ago – was a clinical trial. Here it is:
Purpose: We performed a pilot trial to assess the response of lower urinary tract symptoms and prostate specific antigen (PSA) to acupuncture in a population of patients biopsy negative for prostate cancer.
Materials and methods: A total of 30 patients were randomly assigned to 1 of 3 study groups, including observation for 3 months with 6 blood samples for PSA at set intervals, 9 sessions of acupuncture in 3 months to points of the kidney-bladder distinct meridian expected to treat the prostate with 6 blood samples for PSA at set intervals and 9 sessions of acupuncture in 3 months to points not expected to treat the prostate with 6 blood samples for PSA at set intervals. The effect of acupuncture on lower urinary tract symptoms was assessed monthly using the International Prostate Symptom Score.
Results: Trend analysis (repeated measures ANOVA) revealed no significant changes in the 3-month period in the randomized arms. Statistical analysis showed p = 0.063 for the International Prostate Symptom Score, p = 0.945 for PSA and p = 0.37 for the free-to-total PSA ratio.
Conclusions: Acupuncture to the kidney-bladder distinct meridian neither relieves lower urinary tract symptoms nor impacts PSA.
Yes, an acupuncture study with a negative result!
Niemtzow has, as far as I can see, never himself conducted a study of ‘battle field acupuncture’. In fact, there only very few trials of ‘battle field acupuncture‘. The most recent (albeit lousy) study even suggest that it is less effective than electroacupuncture (EA): EA was more effective than ‘battle field auricular acupuncture’ at reducing pain severity, but both similarly improved physical and mental health scores.
This does not stop Niemtzow to continue praising acupuncture in dozens of papers, particularly his ‘battle field’ version and especially in his ‘own’ journal. The most recent example has just been published; allow me to present an excerpt to you:
In December of 2023, I had the opportunity to visit the Van Gogh Museum in Amsterdam. The only day I had for this visit was characterized by a pouring and chilling rain. This did not stop the crowds of people visiting this famous exhibition. I reminded myself that Van Gogh was a troubled spirit. He lived a short tumultuous life characterized by cutting off his left ear lobe and he spent a sojourn in an asylum. Yet, his art emerged in all its beauty and splendor to become famous in the world. Despite all his troubles, he contributed a precious collection of magnificent art. Many individuals would not have surfaced out of personal disorders to produce such a wonderful gift to society. However, history tells us that many sensational contributions originated from people embroiled in mental health illnesses.
Medical Acupuncture published more than 13 years ago the acupuncture ‘‘diagnosis’’ of Vincent Van Gogh. The article, which is worth rereading, discussed the Five-Element pattern associated with the artist’s hallucinations, alcoholism, severe depression, insomnia, anxiety, dizziness, headaches, nightmares, etc. The author, Vera Kaikobad, LAc, stated: ‘‘It is poignant to realize that a few needles in the hands of a skilled acupuncturist may have spared this great artist such torment and perhaps saved his life.’’ Feasibly, in 2024 we should not only examine our patients for their physical complaints; we should venture into their mental health status as well. A back or neck pain is important, but so is anxiety, insomnia, etc. In promoting mental health, we may assist many patients who are perhaps capable of contributing to the well-being of the world. It is our responsibility as acupuncturists not to think of our patients as a neck or back pain, etc.; instead, we must see them as whole persons having spiritual and physical needs that must be addressed.
I feel that, overall, this remarkable effort justifies Niemtzow’s admission to my ALTERNATIVE MEDICINE HALL OF FAME.
WELCOME, RICHARD!
And let me introduce you to the rest of the 24 laureates:
- Helmut Kiene (anthroposophical medicine)
- Helge Franke (osteopathy, Germany)
- Tery Oleson (acupressure , US)
- Jorge Vas (acupuncture, Spain)
- Wane Jonas (homeopathy, US)
- Harald Walach (various SCAMs, Germany)
- Andreas Michalsen ( various SCAMs, Germany)
- Jennifer Jacobs (homeopath, US)
- Jenise Pellow (homeopath, South Africa)
- Adrian White (acupuncturist, UK)
- Michael Frass (homeopath, Austria)
- Jens Behnke (research officer, Germany)
- John Weeks (editor of JCAM, US)
- Deepak Chopra (entrepreneur, US)
- Cheryl Hawk (chiropractor, US)
- David Peters (osteopathy, homeopathy, UK)
- Nicola Robinson (TCM, UK)
- Peter Fisher (homeopathy, UK)
- Simon Mills (herbal medicine, UK)
- Gustav Dobos (various SCAMs, Germany)
- Claudia Witt (homeopathy, Germany/Switzerland)
- George Lewith (acupuncture, UK)
- John Licciardone (osteopathy, US)
An alarming story of research fraud in the area of so-called alternative medicine (SCAM) is unfolding: Bharat B. Aggarwal, the Indian-American biochemist who worked at MD Anderson Cancer Center, focused his research on curcumin, a compound found in turmeric, and authored more than 125 Medline-listed articles about it. They reported that curcumin had therapeutic potential for a variety of diseases, including various cancers, Alzheimer’s disease and, more recently, COVID-19.
The last of these papers, entitled “Curcumin, inflammation, and neurological disorders: How are they linked?”, was publiched only a few months ago. Here is its abstract:
Background: Despite the extensive research in recent years, the current treatment modalities for neurological disorders are suboptimal. Curcumin, a polyphenol found in Curcuma genus, has been shown to mitigate the pathophysiology and clinical sequalae involved in neuroinflammation and neurodegenerative diseases.
Methods: We searched PubMed database for relevant publications on curcumin and its uses in treating neurological diseases. We also reviewed relevant clinical trials which appeared on searching PubMed database using ‘Curcumin and clinical trials’.
Results: This review details the pleiotropic immunomodulatory functions and neuroprotective properties of curcumin, its derivatives and formulations in various preclinical and clinical investigations. The effects of curcumin on neurodegenerative diseases such as Alzheimer’s disease (AD), amyotrophic lateral sclerosis (ALS), brain tumors, epilepsy, Huntington’s disorder (HD), ischemia, Parkinson’s disease (PD), multiple sclerosis (MS), and traumatic brain injury (TBI) with a major focus on associated signalling pathways have been thoroughly discussed.
Conclusion: This review demonstrates curcumin can suppress spinal neuroinflammation by modulating diverse astroglia mediated cascades, ensuring the treatment of neurological disorders.
The Anderson Cancer Center initially appeared to approve of Aggarwal’s work. However, in 2012, following concerns about image manipulation raised by pseudonymous sleuth Juuichi Jigen, MD Anderson Cancer Center launched a research fraud probe against Aggarwal which eventually led to 30 of Aggarwal’s articles being retracted. Moreover, PubPeer commenters have noted irregularities in many publications beyond the 30 that have already been retracted. Aggarwal thus retired from M.D. Anderson in 2015.
Curcumin doesn’t work well as a therapeutic agent for any disease – see, for instance, the summary from Nelson et al. 2017:
“[No] form of curcumin, or its closely related analogues, appears to possess the properties required for a good drug candidate (chemical stability, high water solubility, potent and selective target activity, high bioavailability, broad tissue distribution, stable metabolism, and low toxicity). The in vitro interference properties of curcumin do, however, offer many traps that can trick unprepared researchers into misinterpreting the results of their investigations.”
Despite curcumin’s apparent lack of therapeutic promise, the volume of research produced on curcumin grows each year. More than 2,000 studies involving the compound are now published annually. Many of these studies bear signs of fraud and involvement of paper mills. As of 2020, the United States National Institutes of Health (NIH) has spent more than 150 million USD funding projects related to curcumin.
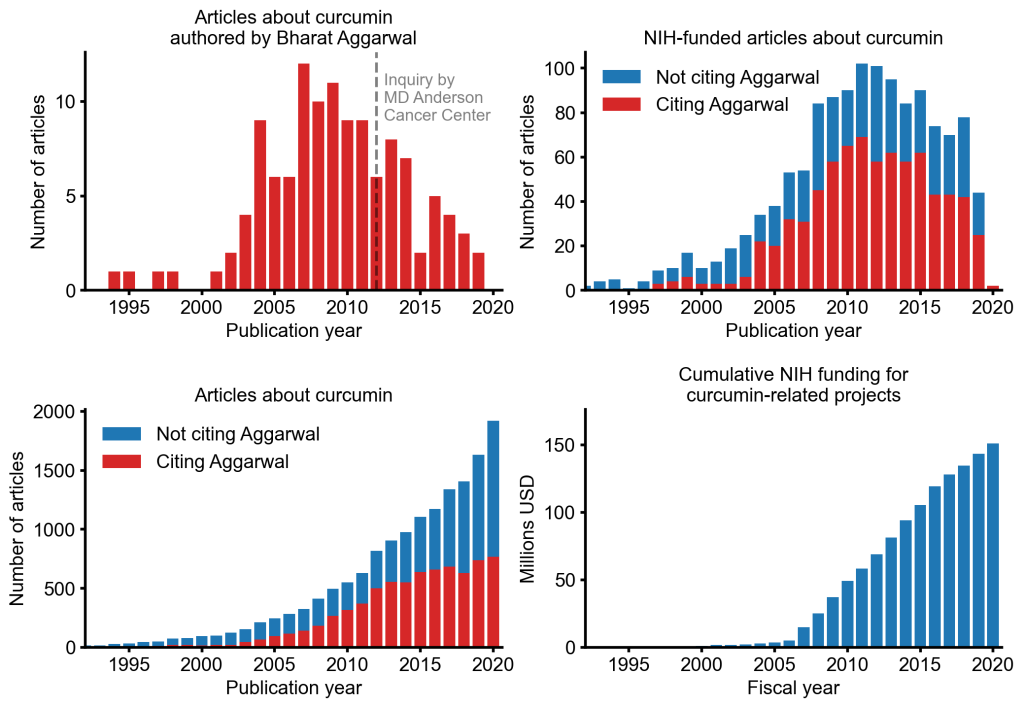
This proliferation of research has fueled curcumin’s popularity as a dietary supplement. It is estimated that the global market for curcumin as a supplement is around 30 million USD in 2020.
The damage done by this epic fraud is huge and far-reaching. Hundreds of millions of taxpayer dollars, countless hours spent toiling by junior scientists, thousands of laboratory animals sacrificed, thousands of cancer patients enrolled in clinical trials for ineffective treatments, and countless people who have eschewed effective cancer treatment in favor of curcumin, were encouraged by research steeped in lies.
I had the rare pleasure to give an interview for the ‘Frankfurter Allgemeine’. As it was, of course, in German, I took the liberty to translate it for my non-German speaking readers:
You have researched so-called alternative medicine over several decades, including homeopathy. What is your conclusion?
We are talking about far more than 400 methods – to draw one conclusion about all of them
is completely impossible. Except perhaps for this one: if something sounds too good to be true, it probably is.
Does this apply to homeopathy?
Highly diluted homeopathic remedies are popular because they have no side-effects. But there is also no effect. They are touted as a panacea. This is certainly not the case, on the contrary, they are
ineffective. And any therapy that is ineffective and promoted as a panacea is also dangerous.
How do you explain the fact that so many people swear by homeopathy?
There are several reasons for this. In Germany, homeopathy has an unbroken tradition, it was, for instance, promoted by the Nazis and later in the Federal Republic of Germany. It has a reputation for being gentle and effective. It might be gentle, but it is certainly not effective. It is also supported by lobby groups such as the manufacturers. And most people who use it don’t even understand what it actually is.
In any case, the placebo effect helps. What’s so bad about that??
Nothing at all, on the contrary: it is to be advocated. When we talk about placebo effects, we subsume many things under this umbrella that do not actually belong to it, such as the extensive, empathetic conversation that homeopaths often have with their patients. Besides, a common cold goes away whether you treat it or not. If you then use homeopathy, you can easily get the impression that it worked. Every good, empathetic doctor tries to maximize the placebo effect. To put it bluntly: you don’t need a placebo to generate a placebo effect. Patients also benefit from it when I give an effective remedy with empathy. In addition they benefit from the specific effect of my therapy, which should make up the lion’s share of the therapeutic response. If I withhold the most important thing I mistreat my patient.
But there are diseases for which there are no good remedies.
I often hear that argument. But there is practically always something we can do that at least
improves symptoms. Otherwise you should also say that instead of lying and recommending homeopathy – and thinking that, although there is nothing in it and it doesn’t work, but the patient, being an idiot, should take it nevertheless. It is unethical to use placebos as much as it is to use homeopathy.
Neurophysiologically, the placebo effect is becoming better and better understood.
The Italian neuroscientist Fabrizio Benedetti in particular has done very good work. But he also warns that this does not justify the use of homeopathy, for example.
Are there any studies on whether the placebo effect of homeopathy with its esoteric superstructure is greater than that giving just a piece of sugar?
There are analyses of what makes a particularly effective placebo. From this, we can learn that effective therapies in evidence-based medicine must be applied with empathy and sufficient time in order to maximize the ever-present placebo effect. So-called alternative medicine often does this quite well, and we can learn something from it. But the reason is that it often has nothing else. Homeopaths are a serious danger because they see homeopathy as a panacea. If someone has homeopathically treated their cold “successfully” for years and then gets cancer, they might think of turning to homeopathy for their cancer. It sounds crazy, but many homeopaths do offer cancer treatments on the internet, for instance. That sends shivers down my spine.
How should doctors and pharmacists react to the demand for homeopathic remedies?
Pharmacists are not primarily salespeople, they are a medical profession – they have to adhere to ethical guidelines. In this respect, evidence-based information of their clients/patients is very important.
Thomas Benkert, President of the German Federal Chamber of Pharmacists, has stated that he would not be able to stop giving advice if he always had to explain the lack of proof of efficacy.
He should perhaps read up on what his ethical duty to patients is.
What if doctors or pharmacists themselves believe in the effect?
Belief should not play a role, but evidence should.
Are you pleased with Lauterbach’s plan to no longer reimburse homeopathy?
I think it’s a shame that he justifies it by saying it’s ineffective. That is true. But the justification should be that it’s esoteric nonsense and therefore ineffective – and dangerous.
In the end, the Bundestag will decide.
I think Lauterbach has a good chance because things have started to move. Medical associations in Germany have spoken out against the additional designation of homeopathy, for example, and overall the wind has changed considerably.
What is it like in the UK, where you live?
The UK healthcare system, NHS, said goodbye to reimbursement of homeopathy about five years ago, even before France. The pharmacists’ association has distanced itself very clearly from homeopathy. However, most pharmacists still sell the remedies and many continue to support them.
You have also had disputes with the current head of state, King Charles. How did that come about?
A few years ago, he commissioned a paper claiming that so-called alternative medicine could save the British health service a lot of money. I protested against this – Charles accused me of leaking it to The Times before it was published. My university launched an investigation, which eventually found me innocent, but it led to the demise of my department. That caused me to retire two years early.
So Charles managed to close down the only research unit in the world that conducted critical and systematic research into so-called alternative medicine. Most researchers in this field only want to confirm their own prejudices and not disprove hypotheses. This is a serious misunderstanding of how science works. If someone reports only positive results for their favorite therapy in all conditions, something is wrong.
Some people say that homeopathy should not be researched because nothing positive can come out of it anyway.
There are certainly some SCAMs that are so nonsensical that they should not be researched, as is currently the case with homeopathy. I put it this way because I have researched homeopathy myself and, from my point of view, the situation was not so crystal clear 30 years ago.
Would you say that you have approached the matter with a sufficiently open mind?
No one can be completely unbiased. That’s why it’s important to do science properly, then you minimize bias as much as possible. When I took up my position at Exeter in 1993, I was perhaps somewhat biased towards homeopathy in a positive sense, because I had learned and used it myself, as well as other alternative medicine methods. The fact that the results then turned out to be negative in the vast majority of cases initially depressed me. But I have to live with that.
Every researcher prefers positive results, also because they are easier to publish. It was clear to me that, if I had succeeded in proving homeopathy right, I wouldn’t get one Nobel Prize, but two. Who wouldn’t want that?
(The interview was conducted by Hinnerk Feldwisch-Drentrup.)
Since the introduction of their new Education Standards in March 2023, the General Chiropractic Council (GCC) has been working with chiropractic education providers to support them in implementing the changes to their curricula. Recently, the GCC have stated this:
We expect students to be taught evidence-based practice: integrating individual clinical expertise, the best available evidence from current and credible clinical research, and the values and preferences of patients. Chiropractors are important members of a patient’s healthcare team, and interprofessional approaches enable the best outcomes. Programmes that meet these Standards will teach ethical, professional care and produce competent healthcare professionals who can serve the needs of patients.
These are indeed most encouraging words!
Basically, they are saying that chiropractic education will now have to be solidly based on the principles of evidence-based medicine (EBM) as well as sound medical ethics. Let me spell out what this really means. Chiropractic courses must teach that:
- The current and credible clinical evidence suggesting that spinal manipulations, the hallmark intervention of chiropractors, are effective is weak for back pain and negative or absent for all other conditions.
- The current and credible clinical evidence suggests that spinal manipulations, the hallmark intervention of chiropractors, can cause harm which in many instances is serious.
- The current and credible clinical evidence thus suggests that the risk/benefit balance for spinal manipulations, the hallmark intervention of chiropractors, is not positive.
- Medical ethics require that competent healthcare professionals inform their patients that spinal manipulations, the hallmark intervention of chiropractors, may not generate more good than harm which is the reason why they cannot employ these therapies.
So, the end of chiropractic in the UK is looming!
Unless, of course, the GCC’s words are not really meant to be translated into action. They could be just window dressing and politically correct bullshit. But that’ s really far too far fetched – after all they come from the GENERAL CHIROPRACTIC COUNCIL, known for its excellent track record, e.g.:
- The GCC “seems to be a little self-regulatory chiropractic bubble where chiropractors regulate chiropractors.”
- A 5-year strategy for UK chiropractors: not fit for purpose
- Chiro behaving badly… is the GCC fit for purpose?
- The UK General Chiropractic Council: fit for purpose?
- Farcical Chiropractic Council: Chiropractic Patient Satisfaction and Experience
- The General Chiropractic Council “regulates chiropractors to ensure the safety of patients” … well, you could have fooled me!
- Death of a chiropractic patient prompts a reaction by the UK General Chiropractic Council
According to chiropractic belief, vertebral subluxation (VS) is a clinical entity defined as a misalignment of the spine affecting biomechanical and neurological function. The identification and correction of VS is the primary focus of the chiropractic profession. The purpose of this study was to estimate VS prevalence using a sample of individuals presenting for chiropractic care and explore the preventative public health implications of VS through the promotion of overall health and function.
A brief review of the literature was conducted to support an operational definition for VS that incorporated neurologic and kinesiologic exam components. A retrospective, quantitative analysis of a multi-clinic dataset was then performed using this operational definition.
The operational definition used in this study included:
- (1) inflammation of the C2 (second cervical vertebra) DRG,
- (2) leg length inequality,
- (3) tautness of the erector spinae muscles,
- (4) upper extremity muscle weakness,
- (5) Fakuda Step test,
- radiographic analysis based on the (6) frontal atlas cranium line and (7) horizontal atlas cranium line.
Descriptive statistics on patient demographic data included age, gender, and past health history characteristics. In addition to calculating estimates of the overall prevalence of VS, age- and gender-stratified estimates in the different clinics were calculated to allow for potential variations.
A total of 1,851 patient records from seven chiropractic clinics in four states were obtained. The mean age of patients was 43.48 (SD = 16.8, range = 18-91 years). There were more females (n = 927, 64.6%) than males who presented for chiropractic care. Patients reported various reasons for seeking chiropractic care, including, spinal or extremity pain, numbness, or tingling; headaches; ear, nose, and throat-related issues; or visceral issues. Mental health concerns, neurocognitive issues, and concerns about general health were also noted as reasons for care. The overall prevalence of VS was 78.55% (95% CI = 76.68-80.42). Female and male prevalence of VS was 77.17% and 80.15%, respectively; notably, all per-clinic, age, or gender-stratified prevalences were ≥50%.
The authors concluded that the results of this study suggest a high rate of prevalence of VS in a sample of individuals who sought chiropractic care. Concerns about general health and wellness were represented in the sample and suggest chiropractic may serve a primary prevention function in the absence of disease or injury. Further investigation into the epidemiology of VS and its role in health promotion and prevention is recommended.
This is one of the most hilarious pieces of ‘research’ that I have recently encountered. The strategy is siarmingly simple:
- invent a ficticious pathology (VS) that will earn you plently of money;
- develop criteria that allow you to diagnose this pathology in the maximum amount of consumers;
- show gullible consumers that they are afflicted by this pathology;
- use scare mongering tactics to convince consumers that the pathology needs treating;
- offer a treatment that, after a series of expensive sessions, will address the pathology;
- cash in regularly while this goes on;
- when the consumer has paid enough, declare that your fabulous treatment has done the trick and the consumer is again healthy.
The strategy is well known amongst practitioners of so-called alternative medicine (SCAM), e.g.:
- Traditional acupuncturists diagnose a ficticious imbalance of yin and yang only to normalise it with numerous acupuncture sessions.
- Naturopaths diagnose ficticious intoxications and treat it with various detox measures.
- Iridologists diagnose ficticious abnormalities of the iris that allegedly indicate organ disstress and treat it with whatever SCAM they can offer.
As they say:
No disease can be more surely, effectively, and profitably treated than a condition that the unsuspecting customer did not have in the first place!
PS
Sadly, such behavior exists in convertional medicine occasionally too, but SCAM relies almost entirely on it.
