cranial osteopathy
This blog is now almost 13 years old. In well over 3 000 (!) posts, I have been trying to alert consumers to the things that are wrong with much of so-called alternative medicine (SCAM). In this new series of posts entitled ‘WHAT HAPPENED NEXT? …’ I intend to re-visit some of my early posts and ask: WHAT HAPPENED NEXT?
This might show us
- what has changed,
- what has remained the same
- and what needs to change.
Here we go:
In my blog post of 17/12/2012 about Craniosacral Therapy (CST) I concluded that:
1) ineffective therapies, such as CST, may seem harmless but, through their ineffectiveness, they constitute a serious threat to our health;
2) bogus treatments become bogus through the false claims which are being made for them;
3) seriously flawed studies can be worse than none at all: they generate false positive results and send us straight up the garden path.
Almost 13 years after writing this, I fear that the notion ‘SCAM MAY BE INEFFECTIVE BUT IT CANNOT DO ANY HARM!’ is still as popular as it was before. Equally, the dismal quality of research into SCAM is still a problem. And, of course, CST is still around with unsupported, often dangerous claims.
So, has anything changed at all?
I am not sure.
If nothing much has changed, what does that mean for me, my motivation and this blog?
When I started my blog I already had ~20 years experience in full-time SCAM research. If that experience had taught me anything at all, it was not to expect too much. SCAM is a most resistant phenomenon. I don’t see my blog as an instrument for abolishing SCAM (an outright impossibility, in my view). I prefer to think of it as a means of damage limitation.
Having said all this, I must admit that the often dismal quality of research and the tolerance of pseudoscience by journal editors and consumers do disappoint me. But my conclusion is not to give up and resign but to work a bit harder trying my best to prevent harm!
The ‘Healy’ has featured on this blog before and is thus known to my regulars: The ‘Healy’: deep cellular healing with quantum bollocks. Now the ‘Healy’ has won an award … albeit a negative one: the Austrian Skeptiks necative prize ‘GOLDENES BRETT VORM KOPF’ (Golden Plank before the Head)
Other nomineed for the award were:
- The broadcaster AUF1 TV, which has been categorised as right-wing extremist.
- The Austrian Veterinary Association known to support homeopathy for animals.
At yesterday’s gala in the Vienna City Hall, it was announced that the ‘Healy’ is the proud winner.
A total of 160 nominations were received by the Vienna Sceptics (Gesellschaft für kritisches Denken, GkD), which awards the prize on behalf of the Gesellschaft zur Wissenschaftlichen Untersuchung von Parawissenschaften (GWUP). On the basis of all these nominations, a ‘shortlist’ of three was subsequently agreed upon by the jury.
The organisers explained in their press release that the ‘Healy’ is advertised as a medical device for the treatment of pain, including chronic pain and migraines, as well as for the supportive treatment of mental illnesses such as depression and anxiety with a lot of pseudo-scientific phraseology.
A ‘quantum sensor’ allegedly measures the ideal ‘frequency’ of the user and causes a ‘bioenergetic field harmonisation’. However, the ‘quantum sensor’ turns out to be nothing more than a simple infrared diode, available for 20 cents. By contrast, consumers are asked to pay up to 4,500 Euros for the ‘Healy’!
Several research platforms, medical information portals and consumer centres have come to damning conclusions about the device. There is talk of ‘bioresonance scams’, ‘dubious frequency therapy’ for which there is a lack of scientific evidence and an ‘esoteric scam’. In addition to the considerable commercial interest and widespread use, the jury said that the manufacturer’s way of dealing with critics was also decisive for the win.
Having recently favoured the Austrian Veterinary Association (AVA) to win the award, I am in two minds. On the one hand, I am disappointed that the AVA did not make it. On the other hand, having reported about the ‘Healy’s extraordinary quantum bollocks some time ago, I am delighted that a worthy winner has been found and crowned.
Whenever I report a case of arterial dissection after spinal manipulation, a defender of the indefensible comments that the case does not prove anything.
Let’s try again, shall we?
It has been reported that Nerissa E. Weeks has filed a negligence complaint against Dr. Jack J. Cacic and his business, Lake Worth Chiropractic & Wellness (LWCW). Weeks, a resident of Lake Worth, alleges that she suffered permanent neurological injuries due to the negligence of Dr. Cacic during chiropractic treatments at LWCW. Weeks initially sought treatment from Cacic on January 12, 2023, for low back pain related to a herniated disc in her lumbar spine. Following this initial visit, she returned to Cacic’s office several months later on June 26, 2023, complaining of neck pain and headaches.
During subsequent visits on June 26 and June 28, Cacic performed cervical manipulations and other treatments without obtaining appropriate informed consent from Weeks regarding the risks involved. On June 30, following another session of cervical manipulations by Cacic, Weeks experienced severe dizziness and vertigo shortly after the procedure. She was subsequently hospitalized and diagnosed with an acute right vertebral artery dissection and an ischemic stroke.
Weeks contends that Cacic failed to recognize symptoms indicative of a vertebral artery dissection and did not provide adequate care consistent with professional standards. The complaint states: “As a direct and proximate result of the negligence of the Defendants, WEEKS suffered permanent neurologic injuries due to an acute thromboembolic cerebrovascular accident.”
The plaintiff is seeking damages exceeding $50,000 for medical expenses, loss of earnings, pain and suffering, mental anguish, disability, impairment, and other related costs incurred due to the alleged negligence. Represented by attorney Hector Buigas from Morgan & Morgan P.A., Weeks demands compensatory damages along with interest, taxable costs, attorneys’ fees, prejudgment interest on medical bills as well as any other relief deemed proper by the court.
____________________
How many more such cases do we need before chiropractors admit that cervical manipulations do more harm than good?
How long until all chiropractors explain to their patients that cervical manipulations do more harm than good?
How long until cervical manipulations become obsolete?
Craniosacral therapy (CST) is a widely taught component of osteopathic medical education. It is included in the standard curriculum of osteopathic medical schools, despite controversy surrounding its use. This paper seeks to systematically review randomized clinical trials (RCTs) assessing the clinical effectiveness of CST compared to standard care, sham treatment, or no treatment in adults and children.
A search of Embase, PubMed, and Scopus was conducted on 10/29/2023 with no restriction placed on the date of publication. Additionally, a Google Scholar search was conducted to capture grey literature. Backward citation searching was also implemented. All RCTs employing CST for any clinical outcome were included. Studies not available in English as well as any studies that did not report adequate data for inclusion in a meta-analysis were excluded. Multiple reviewers were used to assess for inclusions, disagreements were settled by consensus. PRISMA guidelines were followed in the reporting of this meta-analysis. Cochrane’s Risk of Bias 2 tool was used to assess for risk of bias. All data were extracted by multiple independent observers. Effect sizes were calculated using a Hedge’s G value (standardized mean difference) and aggregated using random effects models.
The primary study outcome was the effectiveness of CST for selected outcomes as applied to non-healthy adults or children and measured by standardized mean difference effect size. Twenty-four RCTs were included in the final meta-analysis with a total of 1,613 participants. When results were analyzed by primary outcome, no significant effects were found. When secondary outcomes were included, results showed that only Neonate health, structure (g = 0.66, 95% CI [0.30; 1.02], Prediction Interval [-0.73; 2.05]) and Pain, chronic somatic (g = 0.34, 95% CI [0.18; 0.50], Prediction Interval [-0.41; 1.09]) showed statistically significant effects. However, wide prediction intervals and high bias limit the real-world implications of this finding.
The authors concluded that CST did not demonstrate broad significance in this meta-analysis, suggesting limited usefulness in patient care for a wide range of indications.
To this, one should perhaps add that CST is one of those forms of so-called alternative medicine (SCAM) that is utterly implausible; there is not conceivable mechanism by which CST might work other than a placebo effects. Therefore, the finding that it is ineffective (positive effects on secondary outcomes are most likely due to residual bias and possibly fraud) is hardly surprising. The most sensible conclusion, in my view, is that CST too ridiculous to merit further research because that would, in effect, be an unethical waste of resources.
The ‘University College of Osteopathy’ announced a proposal to merge with the AECC University College (AECC UC). Both institutions will seek to bring together the two specialist providers to offer a “unique inter-disciplinary environment for education, clinical practice and research in osteopathy, chiropractic, and across a wide range of allied health and related disciplines”.
The partnership is allegedly set to unlock significant opportunities for growth and development by bringing together the two specialist institutions’ expertise and resources across two locations – in Dorset and central London.
As a joint statement, Chair of the Board of Governors at AECC UC, Jeni Bremner and Chair of the Board of Governors at UCO, Professor Jo Price commented:
“We believe the proposed merger would further the institutional ambitions for both of our organisations and the related professional groups, by allowing us to expand our educational offering, grow student numbers and provide a unique inter-disciplinary training environment, providing students the opportunity to be immersed in multi-professional practice and research, with exposure to and participation in multi-disciplinary teams.
“There is also an exciting and compelling opportunity to expedite the development of a nationally unique, and internationally-leading MSK Centre of Excellence for Education and Research, developed and delivered across our two sites.”
The announcement is accompanied by further uncritical and promotional language:
Established as the first chiropractic training provider in Europe, AECC UC has been at the forefront of evidence-based chiropractic education, practice and research for more than 50 years. The institution is on an exciting journey of growth and development, having expanded and diversified its academic portfolio and activity beyond its traditional core offering of chiropractic across a broad range of allied health courses and apprenticeships, working closely with NHS, local authority and other system partners across Dorset and the south-west. The proposed merger with UCO would allow AECC UC to enhance the breadth and depth of its offer to support the expansion and development of the health and care workforce across a wider range of partners.
Now in its 106th year, UCO is one of the UK’s leading providers of osteopathic education and research with an established reputation for creating highly-skilled, evidence-informed graduates. UCO research is recognised as world-leading, delivering value to the osteopathic and wider health care community.
Sharon Potter, Acting Vice-Chancellor of UCO, said:
“As an institution that has long been at the forefront of osteopathic education and research, we are committed to ensuring further growth and development of the osteopathic profession.
“UCO has been proactively considering options to future-proof the institution. Following a review of strategic options, UCO is delighted by the proposed merger, working closely with AECC UC to ensure that UCO and osteopathy thrives as part of the inter-professional health sciences landscape, both academically and clinically. There is significant congruence between UCO and AECC UC in our strong aligned values, commitment to and delivery of excellent osteopathic education, clinical care and research, and opinion leadership.
“AECC UC has a strong track record of respecting the differences in professions, evidenced by the autonomy across the 10 different professional groups supported by the institution. The merger will not only mean we are protecting UCO through preserving its osteopathic heritage and creating a sustainable future, but that our staff and students can collaborate with other professional groups such as physiotherapy, chiropractic, sport rehabilitation, podiatry and diagnostic imaging, in a multidisciplinary MSK and rehabilitation environment unlike anywhere else in the UK.”
Professor Lesley Haig, Vice-Chancellor of AECC UC, commented:
“Preserving the heritage of UCO and safeguarding its future status as the flagship osteopathy training provider in the UK will be critical, just as it has been to protect the chiropractic heritage of the AECC brand. UCO is seen as synonymous with, and reflective of, the success of the osteopathy profession and we fully recognise and respect the important role that UCO plays not only as a sector-leading provider of osteopathic education, research and clinical care, but as the UK’s flagship osteopathy educational provider.
“Overall it is clear that UCO and AECC UC already have a common values base, similar understanding of approaches to academic and clinical delivery, and positive relationships upon which a future organisational structure and opportunities can be developed. It’s an exciting time for both institutions as we move forward in partnership to create something unique and become recognised nationally and internationally as a centre of excellence.”
The proposed merger would continue the already founded positive relations between the institutions, where regular visits, sharing of good practice, and collaborative research work are already taking place. Heads of terms for the potential merger have now been agreed and both institutions are entering into the next phase of discussions, which will include wide consultation with staff, students and other stakeholders to produce a comprehensive implementation plan.
__________________________________
In case this bonanza of platitudes and half-truths has not yet overwhelmed you, I might be so bold as to ask 10 critical questions:
- What is an “evidence-based chiropractic education”? Does it include the messages that 1) subluxation is nonsense, 2) chiropractic manipulations can cause harm, 3) there is little evidence that they do more good than harm?
- How an an “expansion and development of the health and care workforce” be anticipated on the basis of the 3 points I just made?
- What does the term “evidence-informed graduates” mean? Does it mean they are informed that you teach them nonsense but instruct them to practice this nonsense anyway?
- Do “options to future-proof the institution” include the continuation of misleading the public about the value of chiropractic/osteopathy?
- Does the”delivery of excellent osteopathic education, clinical care and research, and opinion leadership” account for the fact that the evidence for osteopathy is weak at best and for most conditions negative?
- By “preserving its osteopathic heritage”, do you intend to preserve also the reputation of your founding father, Andrew Taylor Still, who did many dubious things. In 1874, for instance, he was excommunicated by the Methodist Church because of his “laying on of hands”; specifically, he was accused of trying to emulate Jesus Christ, labelled an agent of the Devil, and condemned as practicing voodoo. Or do you prefer to white-wash the osteopathic heritage?
- You also want “to protect the chiropractic heritage”; does that mean you aim at white-washing the juicy biography of the charlatan who created chiropractic, DD Palmer, as well?
- “UCO and AECC UC already have a common values base” – what are they? As far as I can see, they mainly consist in hiding the truth about the uselessness of your activities from the public.
- How do you want to “recognised nationally and internationally as a centre of excellence”? Might it be a good idea to begin by critically assessing your interventions and ask whether they do more good than harm?
- Crucially, what is really behing the merger that you are trying to sell us with such concentrated BS?
This case report aims to describe the effects of craniosacral therapy and acupuncture in a patient with chronic migraine.
A 33-year-old man with chronic migraine was treated with 20 sessions of craniosacral therapy and acupuncture for 8 weeks. The number of migraine and headache days were monitored every month. The pain intensity of headache was measured on the visual analog scale (VAS). Korean Headache Impact Test-6 (HIT-6) and Migraine Specific Quality of Life (MSQoL) were also used.
The number of headache days per month reduced from 28 to 7 after 8 weeks of treatment and to 3 after 3 months of treatment. The pain intensity of headache based on VAS reduced from 7.5 to 3 after 8 weeks and further to < 1 after 3 months of treatment. Furthermore, the patient’s HIT-6 and MSQoL scores improved during the treatment period, which was maintained or further improved at the 3 month follow-up. No side effects were observed during or after the treatment.
The authors concluded that this case indicates that craniosacral therapy and acupuncture could be effective treatments for chronic
migraine. Further studies are required to validate the efficacy of craniosacral therapy for chronic migraine.
So, was the treatment period 8 weeks long or was it 3 months?
No, I am not discussing this article merely for making a fairly petty point. The reason I mention it is diffteren. I think it is time to discuss the relevance of case reports.
What is the purpose of a case report in medicine/healthcare. Here is the abstract of an article entitled “The Importance of Writing and Publishing Case Reports During Medical Training“:
Case reports are valuable resources of unusual information that may lead to new research and advances in clinical practice. Many journals and medical databases recognize the time-honored importance of case reports as a valuable source of new ideas and information in clinical medicine. There are published editorials available on the continued importance of open-access case reports in our modern information-flowing world. Writing case reports is an academic duty with an artistic element.
An article in the BMJ is, I think, more informative:
It is common practice in medicine that when we come across an interesting case with an unusual presentation or a surprise twist, we must tell the rest of the medical world. This is how we continue our lifelong learning and aid faster diagnosis and treatment for patients.
It usually falls to the junior to write up the case, so here are a few simple tips to get you started.
First steps
Begin by sitting down with your medical team to discuss the interesting aspects of the case and the learning points to highlight. Ideally, a registrar or middle grade will mentor you and give you guidance. Another junior doctor or medical student may also be keen to be involved. Allocate jobs to split the workload, set a deadline and work timeframe, and discuss the order in which the authors will be listed. All listed authors should contribute substantially, with the person doing most of the work put first and the guarantor (usually the most senior team member) at the end.
Getting consent
Gain permission and written consent to write up the case from the patient or parents, if your patient is a child, and keep a copy because you will need it later for submission to journals.
Information gathering
Gather all the information from the medical notes and the hospital’s electronic systems, including copies of blood results and imaging, as medical notes often disappear when the patient is discharged and are notoriously difficult to find again. Remember to anonymise the data according to your local hospital policy.
Writing up
Write up the case emphasising the interesting points of the presentation, investigations leading to diagnosis, and management of the disease/pathology. Get input on the case from all members of the team, highlighting their involvement. Also include the prognosis of the patient, if known, as the reader will want to know the outcome.
Coming up with a title
Discuss a title with your supervisor and other members of the team, as this provides the focus for your article. The title should be concise and interesting but should also enable people to find it in medical literature search engines. Also think about how you will present your case study—for example, a poster presentation or scientific paper—and consider potential journals or conferences, as you may need to write in a particular style or format.
Background research
Research the disease/pathology that is the focus of your article and write a background paragraph or two, highlighting the relevance of your case report in relation to this. If you are struggling, seek the opinion of a specialist who may know of relevant articles or texts. Another good resource is your hospital library, where staff are often more than happy to help with literature searches.
How your case is different
Move on to explore how the case presented differently to the admitting team. Alternatively, if your report is focused on management, explore the difficulties the team came across and alternative options for treatment.
Conclusion
Finish by explaining why your case report adds to the medical literature and highlight any learning points.
Writing an abstract
The abstract should be no longer than 100-200 words and should highlight all your key points concisely. This can be harder than writing the full article and needs special care as it will be used to judge whether your case is accepted for presentation or publication.
What next
Discuss with your supervisor or team about options for presenting or publishing your case report. At the very least, you should present your article locally within a departmental or team meeting or at a hospital grand round. Well done!
Both papers agree that case reports can be important. They may provide valuable resources of unusual information that may lead to new research and advances in clinical practice and should offer an interesting case with an unusual presentation or a surprise twist.
I agree!
But perhaps it is more constructive to consider what a case report cannot do.
It cannot provide evidence about the effectiveness of a therapy. To publish something like:
- I had a patient with the common condition xy;
- I treated her with therapy yz;
- this was followed by patient feeling better;
is totally bonkers – even more so if the outcome was subjective and the therapy consisted of more than one intervention, as in the article above. We have no means of telling whether it was treatment A, or treatment B, or a placebo effect, or the regression towards the mean, or the natural history of the condition that caused the outcome. The authors might just as well just have reported:
WE RECENTLY TREATED A PATIENT WHO GOT BETTER
full stop.
Sadly – and this is the reason why I spend some time on this subject – this sort of thing happens very often in the realm of SCAM.
Case reports are particularly valuable if they enable and stimulate others to do more research on a defined and under-researched issue (e.g. an adverse effect of a therapy). Case reports like the one above do not do this. They are a waste of space and tend to be abused as some sort of indication that the treatments in question might be valuable.
This systematic review and meta-analysis was aimed at analyzing the effectiveness of craniosacral therapy in improving pain and disability among patients with headache disorders.
PubMed, Physiotherapy Evidence Database, Scopus, Cochrane Library, Web of Science, and Osteopathic Medicine Digital Library databases were searched in March 2023. Two independent reviewers searched the databases and extracted data from randomized clinical trials comparing craniosacral therapy with control or sham interventions. The same reviewers assessed the methodological quality and the risk of bias using the PEDro scale and the Cochrane Collaboration tool, respectively. Grading of recommendations, assessment, development, and evaluations was used to rate the certainty of the evidence. Meta-analyses were conducted using random effects models using RevMan 5.4 software.
The searches retrieved 735 papers, and 4 studies were finally included. The craniosacral therapy provided statistically significant but clinically unimportant change on pain intensity (Mean difference = –1.10; 95% CI: –1.85, –0.35; I2: 44%), and no change on disability or headache effect (Standardized Mean Difference = –0.34; 95% CI –0.70, 0.01; I2: 26%). The certainty of the evidence was downgraded to very low.
The authors concluded that very low certainty of evidence suggests that craniosacral therapy produces clinically unimportant effects on pain intensity, whereas no significant effects were observed in disability or headache effect.
I find it strange that researchers seem so frequently unable to formulate their conclusions clearly. Is it political correctness? Or are they somehow favorably inclined (i.e. biased) towards the treatment that they pretend to critically evaluate?
Let’s look at the facts related to this review:
- Craniosacral therapy (CST) is utterly implausible.
- Only 4 RCTs were found.
- They were of poor quality.
- They were published mostly by people who want to promote CST.
- Therefore the overall statistically significant effect is most likely a false-positive result.
- This means that the conclusion should be much more straight forward.
I suggest something along the following lines:
A critical evaluation of the existing RCTs failed to find convincing evidence that CST is an effective treatment for headache disorders.
I have seen some daft meta-analyses in my time – this one, however, takes the biscuit. Here is its unaltered abstract:
Although mindfulness-based mind-body therapy (MBMBT) is an effective non-surgical treatment for patients with non-specific low back pain (NLBP), the best MBMBT mode of treatment for NLBP patients has not been identified. Therefore, a network meta-analysis (NMA) was conducted to compare the effects of different MBMBTs in the treatment of NLBP patients.
Methods: PubMed, EMBASE, Cochrane Central Register of Controlled Trials, and Web of Science databases were searched for randomized controlled trials (RCTs) applying MBMBT for the treatment of NLBP patients, with all of the searches ranging from the time of database creation to January 2023. After 2 researchers independently screened the literature, extracted information, and evaluated the risks of biases in the included studies, the data were analyzed by using Stata 16.0 software.
Results: A total of 46 RCTs were included, including 3,886 NLBP patients and 9 MBMBT (Yoga, Ayurvedic Massage, Pilates, Craniosacral Therapy, Meditation, Meditation + Yoga, Qigong, Tai Chi, and Dance). The results of the NMA showed that Craniosacral Therapy [surface under the cumulative ranking (SUCRA): 99.2 and 99.5%] ranked the highest in terms of improving pain and disability, followed by Other Manipulations (SUCRA: 80.6 and 90.8%) and Pilates (SUCRA: 54.5 and 71.2%). In terms of improving physical health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Pilates (SUCRA: 72.3%) and Meditation (SUCRA: 55.9%). In terms of improving mental health, Craniosacral Therapy (SUCRA: 100%) ranked the highest, followed by Meditation (SUCRA: 70.7%) and Pilates (SUCRA: 63.2%). However, in terms of improving pain, physical health, and mental health, Usual Care (SUCRA: 7.0, 14.2, and 11.8%, respectively) ranked lowest. Moreover, in terms of improving disability, Dance (SUCRA: 11.3%) ranked lowest.
Conclusion: This NMA shows that Craniosacral Therapy may be the most effective MBMBT in treating NLBP patients and deserves to be promoted for clinical use.
___________________________
This meta-analysis has too many serious flaws to mention. Let me therefore just focus on the main two:
- Craniosacral Therapy is not an MBMBT.
- Craniosacral Therapy is not effective for NLBP. The false positive result was generated on the basis of 4 studies. All of them have serious methodological problems that prevent an overall positive conclusion about the effectiveness of this treatment. In case you don’t believe me, here are the 4 abstracts:
1) Background and objectives: The study aimed to compare the effectiveness of craniosacral therapy (CST), muscle energy technique (MET), and sensorimotor training (SMT) on pain, disability, depression, and quality of life of patients with non-specific chronic low back pain (NCLBP).
Methodology: In this randomized clinical trial study 45 patients with NCLBP were randomly divided in three groups including CST, SMT, and MET. All groups received 10 sessions CST, SMT, and MET training in 5 weeks. Visual analogue scale (VAS), Oswestry functional disability questionnaire (ODQ), Beck depression inventory-II (BDI-II), and 36-item short form health survey (SF-36) were used to evaluate the pain, disability, depression, and quality of life, respectively, in three times, before treatment, after the last session of treatment, and after 2 months follow up.
Results: The Results showed that VAS, ODI, BDI, and SF-36 changes were significant in the groups SMT, CST and MET (p < 0.001, p < 0.001, p < 0.001). The VAS, ODI, BDI, and SF-36 changes in post-treatment and follow-up times in the CST group were significantly different in comparison to SMT group, and the changes in VAS, ODI, BDI, and SF-36 at after treatment and follow-up times in the MET group compared with the CST group had a significant difference (p < 0.001).
Conclusion: Craniosacral therapy, muscle energy technique, and sensorimotor training were all effective in improvement of pain, depression, functional disability, and quality of life of patients with non-specific chronic low back pain. Craniosacral therapy is more effective than muscle energy technique, and sensorimotor training in post-treatment and follow up. The effect of craniosacral therapy was continuous after two months follow up.
2) Background: Craniosacral therapy (CST) and sensorimotor training (SMT) are two recommended interventions for nonspecific chronic low back pain (NCLBP). This study compares the effects of CST and SMT on pain, functional disability, depression and quality of life in patients with NCLBP.
Methodology: A total of 31 patients with NCLBP were randomly assigned to the CST group (n=16) and SMT (n=15). The study patients received 10 sessions of interventions during 5 weeks. Visual analogue scale (VAS), Oswestry disability index (ODI), Beck depression inventory-II (BDI-II), and Short Form-36 (SF-36) questionnaires were used at baseline (before the treatment), after the treatment, and 2 months after the last intervention session. Results were compared and analyzed statistically.
Results: Both groups showed significant improvement from baseline to after treatment (p < 0.05). In the CST group, this improvement continued during the follow-up period in all outcomes (p < 0.05), except role emotional domain of SF-36. In the SMT group, VAS, ODI and BDI-II increased during follow-up. Also, all domains of SF-36 decreased over this period. Results of group analysis indicate a significant difference between groups at the end of treatment phase (p < 0.05), except social functioning.
Conclusions: Results of our research confirm that 10 sessions of craniosacral therapy (CST) or sensorimotor training (SMT) can significantly control pain, disability, depression, and quality of life in patients with NCLBP; but the efficacy of CST is significantly better than SMT.
3) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
4) Background: Non-specific low back pain is an increasingly common musculoskeletal ailment. The aim of this study was to examine the utility of craniosacral therapy techniques in the treatment of patients with lumbosacral spine overload and to compare its effectiveness to that of trigger point therapy, which is a recognised therapeutic approach.
Material and methods: The study enrolled 55 randomly selected patients (aged 24-47 years) with low back pain due to overload. Other causes of this condition in the patients were ruled out. The participants were again randomly assigned to two groups: patients treated with craniosacral therapy (G-CST) and patients treated with trigger point therapy (G-TPT). Multiple aspects of the effectiveness of both therapies were evaluated with the use of: an analogue scale for pain (VAS) and a modified Laitinen questionnaire, the Schober test and surface electromyography of the multifidus muscle. The statistical analysis of the outcomes was based on the basic statistics, the Mann-Whitney U test and Wilcoxon’s signed rank test. The statistical significance level was set at p≤0.05.
Results: Both groups demonstrated a significant reduction of pain measured with the VAS scale and the Laitinen questionnaire. Moreover, the resting bioelectric activity of the multifidus muscle decreased significantly in the G-CST group. The groups did not differ significantly with regard to the study parameters.
Conclusions: 1. Craniosacral therapy and trigger point therapy may effectively reduce the intensity and frequency of pain in patients with non-specific low back pain. 2. Craniosacral therapy, unlike trigger point therapy, reduces the resting tension of the multifidus muscle in patients with non-specific lumbosacral pain. The mechanism of these changes requires further research. 3. Craniosacral therapy and trigger point therapy may be clinically effective in the treatment of patients with non-specific lumbosacral spine pain. 4. The present findings represent a basis for conducting further and prospective studies of larger and randomized samples.
_______________________________
I REST MY CASE
Infant colic is a sensitive subject for chiropractors in the UK. In case you forgot, here is why. Consequently, the subject has featured regularly on this blog – and now there is new evidence:
A systematic review and meta-analysis were conducted on infantile colic studies that used SO-CALLED alternative medicine (SCAM) techniques as interventions. The outcome measures were hours spent crying and/or sleeping. The authors used the PubMed, Physiotherapy Evidence Database, Cochrane Library, Embase, Web of Science, Scopus, Osteopathic Medicine Digital Database, and Google Scholar databases from inception to 11 November 2022.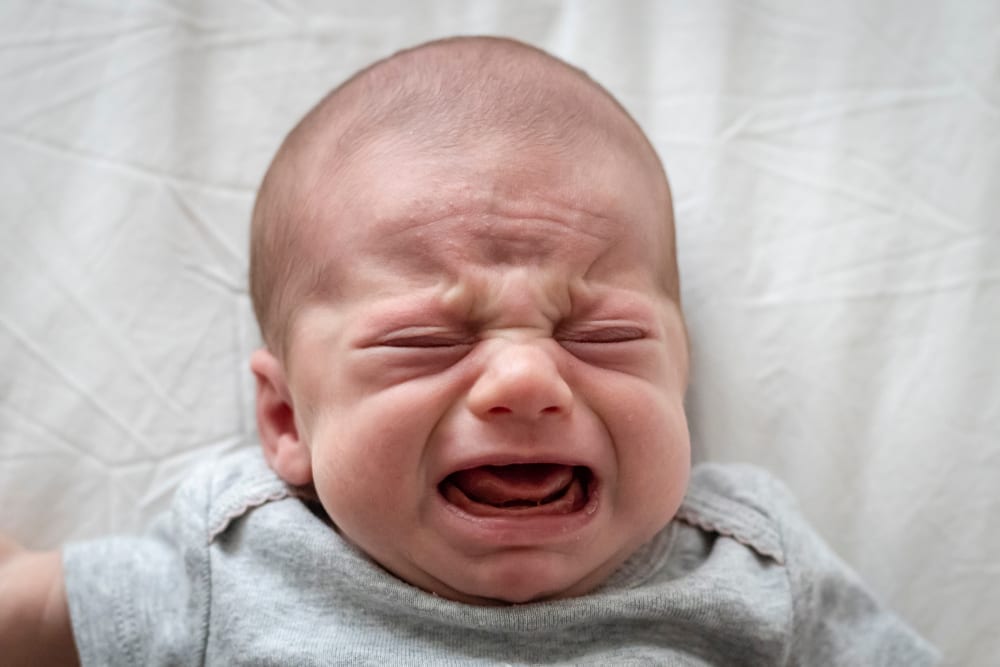
The methodological quality of the randomized control trials ranged from fair to high. The authors focused on five studies with 422 babies using the following interventions: cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization. These treatments failed to decrease the crying time (mean difference -1.08, 95% CI -2.17 to 0.01, I2 = 92%) and to increase the sleeping time (mean difference 1.11, 95% CI -0.20 to 2.41; I2: 91%), compared with no intervention. The quality of the evidence was rated as very low for both outcome measures.The authors concluded that osteopathy and chiropractic treatment failed to reduce the crying time and increase sleeping time in babies with infantile colic, compared to no additional intervention.The 5 included studies were the following:
- Miller JE, Newell D, Bolton JE. Efficacy of chiropractic manual therapy on infant colic: A pragmatic single-blind, randomized controlled trial. J Manipulative Physiol Ther. 2012;35(8):600–7.
- Castejón-Castejón M, Murcia-González MA, Todri J, Lena O, Chillón-Martínez R. Treatment of infant colic with craniosacral therapy. A randomized controlled trial. Complement Ther Med. 2022;71(February 2021).
- Olafsdottir E, Forshei S, Fluge G, Markestad T. Randomised controlled trial of infantile colic treated with chiropractic spinal manipulation. Arch Dis Child. 2001;84(2):138–41.
- Holm LV, Jarbøl DE, Christensen HW, Søndergaard J, Hestbæk L. The effect of chiropractic care on infantile colic: results from a single-blind randomised controlled trial. Chiropr Man Ther. 2021;29(1):1–11.
- Hayden C, Mullinger B. A preliminary assessment of the impact of cranial osteopathy for the relief of infantile colic. Complement Ther Clin Pract. 2006;12(2):83–90.
This means that, in recent years, several new studies have emerged. I find this surprising: there is no plausible mechanism of action and the previous reviews were negative.
Why flog a dead horse?
But – come to think of it – this is a question one might ask about most of the research into cranial, visceral, or structural osteopathy or chiropractic manipulation or mobilization.
This study described osteopathic practise activity, scope of practice and the osteopathic patient profile in order to understand the role osteopathy plays within the United Kingdom’s (UK) health system a decade after the authors’ previous survey.
The researchers used a retrospective questionnaire survey design to ask about osteopathic practice and audit patient case notes. All UK-registered osteopaths were invited to participate in the survey. The survey was conducted using a web-based system. Each participating osteopath was asked about themselves, and their practice and asked to randomly select and extract data from up to 8 random new patient health records during 2018. All patient-related data were anonymized.
The survey response rate was 500 osteopaths (9.4% of the profession) who provided information about 395 patients and 2,215 consultations. Most osteopaths were:
- self-employed (81.1%; 344/424 responses),
- working alone either exclusively or often (63.9%; 237/371),
- able to offer 48.6% of patients an appointment within 3 days (184/379).
Patient ages ranged from 1 month to 96 years (mean 44.7 years, Std Dev. 21.5), of these 58.4% (227/389) were female. Infants <1 years old represented 4.8% (18/379) of patients. The majority of patients presented with musculoskeletal complaints (81.0%; 306/378) followed by pediatric conditions (5%). Persistent complaints (present for more than 12 weeks before the appointment) were the most common (67.9%; 256/377) and 41.7% (156/374) of patients had co-existing medical conditions.
The most common treatment approaches used at the first appointment were:
- soft-tissue techniques (73.9%; 292/395),
- articulatory techniques (69.4%; 274/395),
- high-velocity low-amplitude thrust (34.4%; 136/395),
- cranial techniques (23%).
The mean number of treatments per patient was 7 (mode 4). Osteopaths’ referral to other healthcare practitioners amounted to:
- GPs 29%
- Other complementary therapists 21%
- Other osteopaths 18%
The authors concluded that osteopaths predominantly provide care of musculoskeletal conditions, typically in private practice. To better understand the role of osteopathy in UK health service delivery, the profession needs to do more research with patients in order to understand their needs and their expected outcomes of care, and for this to inform osteopathic practice and education.
What can we conclude from a survey that has a 9% response rate?
Nothing!
If I ignore this fact, do I find anything of interest here?
Not a lot!
Perhaps just three points:
- Osteopaths use high-velocity low-amplitude thrusts, the type of manipulation that has most frequently been associated with serious complications, too frequently.
- They also employ cranial osteopathy, which is probably the least plausible technique in their repertoire, too often.
- They refer patients too frequently to other SCAM practitioners and too rarely to GPs.
To come back to the question asked in the title of this post: What do UK osteopaths do? My answer is
ALMOST NOTHING THAT MIGHT BE USEFUL.
