Monthly Archives: January 2021
Yesterday, someone posted a disparaging comment about Indian research into homeopathy; he claimed that it was unreliable. I agreed, but later I thought ‘HOW ARROGANT OF ME!’. So, I decided to do a little research – actually, it turned out to be a little more than just ‘a little’.
I searched Medline for ‘homeopathy, study, India’. This resulted in 101 hits. Of these 101 articles, 31 contained data published by Indian authors providing evidence at least vaguely related to the effectiveness of homeopathy. I decided to include these in my analysis. Below I quote first the title of each paper followed by (in brackets) the sentence from the 31 abstracts that best describes the direction of the results.
- Multimorbidity After Surgical Menopause Treated with Individualized Classical Homeopathy: A Case Report (She was treated with individualized classical homeopathy and followed up for 31 months. She was relieved of the vasomotor symptoms and psychological disturbances of climacteric syndrome, her weight reduced, the ultrasound scan showed absence of lipomatosis/gall bladder disease/hepatic steatosis. Blood tests showed reduction of thyroid stimulating hormone and a balance in the lipid status. Individualized classical homeopathy may have a role in the climacteric syndrome and comorbidities after surgical menopause.)
- Therapeutic evaluation of homeopathic treatment for canine oral papillomatosis (The current study proves that the combination of homeopathy drugs aids in fastening the regression of canine oral papilloma and proved to be safe and cost-effective.)
- Deep vein thrombosis cured by homeopathy: A case report (The present case report intends to record yet another case of DVT in an old patient totally cured exclusively by the non-invasive method of treatment with micro doses of potentized homeopathic drugs selected on the basis of the totality of symptoms and individualization of the case.)
- Diabetic retinopathy screening uptake after health education with or without retinal imaging within the facility in two AYUSH hospitals in Hyderabad, India: A nonrandomized pilot study (AYUSH hospitals could provide a feasible and acceptable location for providing DR screening services.)
- Individualised Homeopathic Therapy in ANCA Negative Rapidly Progressive Necrotising Crescentic Glomerulonephritis with Severe Renal Insufficiency – A Case Report (A 60-year-old Indian woman was treated with classical homeopathy for ANCA-negative RPGN, and after one year of treatment, serum creatinine and other parameters indicating renal injury dropped steadily despite the withdrawal of immunosuppressive drugs; renal dialysis, which was conducted twice a week initially, was made rarer and stopped after one year. Classical homeopathy may be considered a potential therapeutic modality in severe pathologies.)
- Improvements in long standing cardiac pathologies by individualized homeopathic remedies: A case series (… individualized homeopathic therapy was instituted along with the conventional medicines and the results were encouraging. The changes in the laboratory diagnostic parameters (single-photon emission computed tomography, electrocardiograph, echocardiography and ejection fraction as the case may be) are demonstrated over time. The key result seen in all three cases was the preservation of general well-being while the haemodynamic states also improved.)
- Could Homeopathy Become An Alternative Therapy In Dengue Fever? An example Of 10 Case Studies (We present a retrospective case series of 10 Indian patients who were diagnosed with dengue fever and treated exclusively with homeopathic remedies at Bangalore, India. This case series demonstrates with evidence of laboratory reports that even when the platelets dropped considerably there was good result without resorting to any other means.)
- Homeopathic Treatment of Vitiligo: A Report of Fourteen Cases (In 14 patients with vitiligo treated with individualized homeopathy, the best results were achieved in the patients who were treated in the early stages of the disease. We believe that homeopathy may be effective in the early stages of vitiligo, but large controlled clinical studies are needed in this area.)
- An Exploratory Study of Autonomic Function Investigations in Hemophiliacs on Homoeopathy Medications Using Impedance Plethysmography (Homoeopathic medicines used as an adjunct was associated with decrease in parasympathetic modulations.)
- Embryonic Zebrafish Model – A Well-Established Method for Rapidly Assessing the Toxicity of Homeopathic Drugs: – Toxicity Evaluation of Homeopathic Drugs Using Zebrafish Embryo Model (Our findings clearly demonstrate that no toxic effects were observed for these three homeopathic drugs at the potencies and exposure times used in this study. The embryonic zebrafish model is recommended as a well-established method for rapidly assessing the toxicity of homeopathic drugs.)
- Treatment of hemorrhoids with individualized homeopathy: An open observational pilot study (Under classical homeopathic treatment, hemorrhoids patients improved considerably in symptoms severity and anoscopic scores. However, being observational trial, our study cannot provide efficacy data. Controlled studies are required.)
- Patients’ preference for integrating homeopathy (PPIH) within the standard therapy settings in West Bengal, India: The part 1 (PPIH-1) study (A favorable attitude toward integrating homeopathy into conventional healthcare settings was obtained among the patients attending the homeopathic hospitals in West Bengal, India.)
- Patients’ Preference for Integrating Homoeopathy Services within the Secondary Health Care Settings in India: The Part 3 (PPIH-3) Study (A total of 82.40% (95% confidence interval = 79.23, 85.19) of the participants were in favor of integrating homoeopathy services.)
- Obstetrics and gynecology outpatient scenario of an Indian homeopathic hospital: A prospective, research-targeted study (The most frequently treated conditions were leucorrhea (20.5%), irregular menses (13.3%), dysmenorrhea (10%), menorrhagia (7.5%), and hypomenorrhea (6.3%). Strongly positive outcomes (+3/+2) were mostly recorded in oligomenorrhea (41.7%), leucorrhea (34.1%), polycystic ovary (33.3%), dysmenorrhea (28%), and irregular menses (22.2%). Individualized prescriptions predominated (95.6%).)
- Relative Apoptosis-inducing Potential of Homeopa-thic Condurango 6C and 30C in H460 Lung Cancer Cells In vitro: -Apoptosis-induction by homeopathic Condurango in H460 cells (Condurango 30C had greater apoptotic effect than Condurango 6C as claimed in the homeopathic doctrine.)
- Beliefs, attitudes and self-use of Ayurveda, Yoga and Naturopathy, Unani, Siddha, and Homeopathy medicines among senior pharmacy students: An exploratory insight from Andhra Pradesh, India (Pharmacy students held favorable attitude and beliefs about AYUSH use.)
- Integrative nanomedicine: treating cancer with nanoscale natural products (Taken together, the nanoparticulate research data and the Banerji Protocols for homeopathic remedies in cancer suggest a way forward for generating advances in cancer treatment with natural product-derived nanomedicines.)
- Evidence of an Epigenetic Modification in Cell-cycle Arrest Caused by the Use of Ultra-highly-diluted Gonolobus Condurango Extract (Condurango 30C appeared to trigger key epigenetic events of gene modulation in effectively combating cancer cells, which the placebo was unable to do.)
- Calcarea carbonica induces apoptosis in cancer cells in p53-dependent manner via an immuno-modulatory circuit (Our results indicated a “two-step” mechanism of the induction of apoptosis in tumor cells by calcarea carbonica)
- Post-cancer Treatment with Condurango 30C Shows Amelioration of Benzo[a]pyrene-induced Lung Cancer in Rats Through the Molecular Pathway of Caspa- se-3-mediated Apoptosis Induction: -Anti-lung cancer potential of Condurango 30C in rats (The overall result validated a positive effect of Condurango 30C in ameliorating lung cancer through caspase-3-mediated apoptosis induction and EGFR down-regulation.)
- The potentized homeopathic drug, Lycopodium clavatum (5C and 15C) has anti-cancer effect on hela cells in vitro (Thus, the highly-diluted, dynamized homeopathic remedies LC-5C and LC-15C demonstrated their capabilities to induce apoptosis in cancer cells, signifying their possible use as supportive medicines in cancer therapy.)
- Ameliorating effect of mother tincture of Syzygium jambolanum on carbohydrate and lipid metabolic disorders in streptozotocin-induced diabetic rat: Homeopathic remedy (The result of the present study indicated that the homeopathic drug S jambolanum (mother tincture) has a protective effect on diabetic induced carbohydrate and lipid metabolic disorders in STZ-induced diabetic animal.)
- SEM studies on blood cells of Plasmodium berghei infected Balb/c mice treated with artesunate and homeopathic medicine China (The combination of artesunate and China was found to be very effective and did not cause any alteration on the surface of blood cells as observed in SEM.)
- Induction of apoptosis of tumor cells by some potentiated homeopathic drugs: implications on mechanism of action (These data indicate that apoptosis is one of the mechanisms of tumor reduction of homeopathic drugs.)
- TDZ-induced high frequency shoot regeneration in Cassia sophera Linn. via cotyledonary node explants (Regenerated plantlets were successfully acclimatized and hardened off inside the culture room and then transferred to green house with 100 % survival rate.)
- Modulation of Signal Proteins: A Plausible Mechanism to Explain How a Potentized Drug Secale Cor 30C Diluted beyond Avogadro’s Limit Combats Skin Papilloma in Mice (We tested the hypothesis if suitable modulations of signal proteins could be one of the possible pathways of action of a highly diluted homeopathic drug, Secale cornutum 30C (diluted 10(60) times; Sec cor 30). It could successfully combat DMBA + croton oil-induced skin papilloma in mice as evidenced by histological, cytogenetical, immunofluorescence, ELISA and immunoblot findings.)
- Can homeopathy bring additional benefits to thalassemic patients on hydroxyurea therapy? Encouraging results of a preliminary study (The homeopathic remedies being inexpensive and without any known side-effects seem to have great potentials in bringing additional benefits to thalassemic patients; particularly in the developing world where blood transfusions suffer from inadequate screening and fall short of the stringent safety standards followed in the developed countries.)
- Effect of homeopathic medicines on transplanted tumors in mice (These findings support that homeopathic preparations of Ruta and Hydrastis have significant antitumour activity. The mechanism of action of these medicines is not known at present.)
- Inhibition of chemically induced carcinogenesis by drugs used in homeopathic medicine (These studies demonstrate that homeopathic drugs, at ultra low doses, may be able to decrease tumor induction by carcinogen administration.)
- Can homeopathic treatment slow prostate cancer growth? (The findings indicate that selected homeopathic remedies for the present study have no direct cellular anticancer effects but appear to significantly slow the progression of cancer and reduce cancer incidence and mortality in Copenhagen rats injected with MAT-LyLu prostate cancer cells.)
- Ameliorating effect of microdoses of a potentized homeopathic drug, Arsenicum Album, on arsenic-induced toxicity in mice (The results lend further support to our earlier views that microdoses of potentized Arsenicum Album are capable of combating arsenic intoxication in mice, and thus are strong candidates for possible use in human subjects in arsenic contaminated areas under medical supervision.)
So, 31 of 31 yield positive results and conclusions – 100%!
When I suggested that Indian research into homeopathy is suspect, I was merely speculating on the basis of reading such papers for many years. I had not seen a systematic analysis to justify my harsh judgment; in fact, I don’t think that such a review is currently available (which would make this post the first of its kind). I had no idea how true my seemingly disrespectful remark would turn out to be. There is not one paper from India that does not suggest positive findings for homeopathy. I find this truly remarkable!
You can, of course, interpret my findings in two very different ways:
- Either you assume that homeopathy is hugely effective and works always and for everything under every experimental condition.
- Or you conclude that Indian research into homeopathy is suspect and far from trustworthy.
If you believe the first option to be true, I fear that you must be as deluded as homeopathic remedies are diluted.
The aim of the paper (published in ‘HOMEOPATHY’) was to perform a systematic review of basic research of homeopathic high dilutions in cancer.
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline, we conducted a literature search in the database PubMed for original publications, from 2000 to 2018 and in English, on in vitro and in vivo experimental cancer models testing homeopathic high dilutions.
Twenty-three articles met the inclusion criteria-14 in vitro, eight in vivo, and one in vitro plus in vivo experimental models. Most studies were from India. Research prominently focused on cytotoxic effects involving apoptotic mechanisms. Intrinsic aspects of homeopathy should be considered in experimental designs to emphasize the specificity of such effects.
The authors concluded that fundamental research of homeopathy in cancer is still at an early stage and has mainly been performed by a few groups of investigators. The results point to an interference of well-selected homeopathic medicines with cell cycle and apoptotic mechanisms in cancer cells. However, these findings still need independent reproduction.
I happen to be a co-author of the PRISMA guideline and can assure you that this systematic review is very far from adhering to it. It borders on fraud to state otherwise; at the very minimum, the authors, the editor of ‘HOMEOPATHY‘, as well as the reviewers of this article are guilty of seriously misleading the public. Any reputable journal would have insisted that the abstract of this paper makes the following points very clear so that misunderstandings are avoided:
- There is no valid hypothesis to suggest that homeopathic high dilutions affect cancer.
- The included studies are mostly of poor or very poor quality.
- The results of such pre-clinical in vitro and in vivo experiments have little bearing on the treatment of human cancers.
- The fact that independent replications are missing suggests that these studies are irreproducible.
- The fact that most studies originate from the same research groups implies that homeopathy is not considered to be a viable avenue by rational thinkers.
- In the interest of cancer patients, the idea that homeopathy might be of any use in cancer needs to be discouraged.
In one of my last posts, I stated that research into so-called alternative medicine (SCAM) is fast becoming the laughing stock of serious scientists. This paper is an excellent example of this phenomenon.
The objective of this survey was to determine
- which patients’ characteristics are associated with the use of so-called alternative medicine (SCAM) during cancer treatment,
- their pattern of use,
- and if it has any association with its safety profile.
A total of 316 patients undergoing chemotherapy treatment in cancer centers in Poland between 2017 and 2019 were asked about their use of SCAM.
Patients’ opinion regarding the safety of unconventional methods is related to the use of SCAM. Moreover, patients’ thinking that SCAM can replace conventional therapy was correlated with his/her education. Moreover, the researchers performed analyses to determine factors associated with SCAM use including sociodemographic and clinical characteristics.
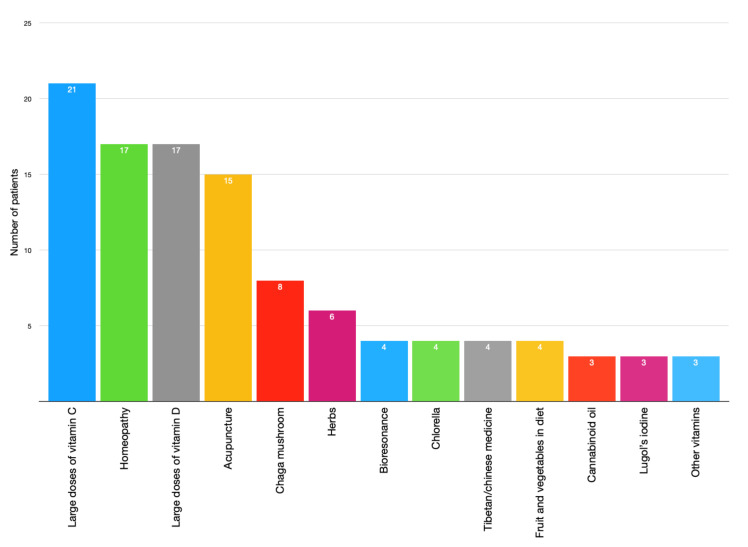
Crucially, they also conducted a survival analysis of patients undergoing chemotherapy with 42 months of follow-up. Using Kaplan-Meier curves and log-rank analysis, they found no statistical difference in overall survival between the groups that used and did not use any form of SCAM.

The authors concluded that SCAM use is common among patients undergoing chemotherapy treatment and should be considered by medical teams as some agents may interact with chemotherapy drugs and affect their efficacy or cause adverse effects.
As I have stated before, I find most surveys of SCAM use meaningless. This article is no exception – except for the survival analysis. It would have merited a separate, more detailed paper, yet the authors hardly comment on it. The analysis shows that SCAM users do not live longer than non-users. Previously, we have discussed several studies that suggested they live less long than non-users.
While this aspect of the new study is interesting, it proves very little. There are, of course, multiple factors involved in the survival of cancer patients, and even if SCAM use were a determinant, it is surely less important than many other factors. To get a better impression of the role SCAM plays, we need studies that carefully match patients according to the most obvious prognostic variables (RCTs would be problematic, difficult to do and unethical). Such studies do exist and they too fail to show that SCAM use prolongs survival, some even suggest it might shorten survival.
Unintended consequences are outcomes of a purposeful action that are not intended or foreseen. They exist almost everywhere and often have effects that are the opposite of what was intended.
Just look at our current misery, the pandemic, for instance. Practically all epidemiologists advocated stricter and earlier preventative measures than the ‘anti-lockdown’ brigade in politics and elsewhere wanted and implemented. Had we listened to the epidemiologists, we would almost certainly have had fewer lockdowns and less economic downturn. The unintended consequences of the political decisions to be slow and less than strict with lockdowns are what we can currently observe in many countries:
- repeated, longer, and less and less effective lockdowns,
- huge economic damage,
- more deaths,
- more long-term illness;
- financial hardship for many,
- more psychological problems and frustration.
But I am not here to moan about politicians not listening enough to scientists. I want to vent my anger and concern about much of the research that is currently being published in the realm of so-called alternative medicine (SCAM).
What is happening here – slightly simplified and exaggerated to make my point – is (as often discussed previously) roughly this:
- more and more enthusiasts of SCAM feel that they should conduct and publish some research;
- they are largely ignorant of or willfully ignore the accepted standards of science;
- they have little interest in cause and effect or critical thinking;
- they aim to promote and not to test SCAM;
- several SCAM journals have realized that there is good money to be earned from publishing utter rubbish;
- more and more papers are being published that are flawed to the point of being meaningless;
- the few relevant SCAM papers with sound science get drowned out and become all but invisible;
- outsiders glancing at the literature get the impression that SCAM is swamped with rubbish and thus an area that is best avoided;
- consequently, SCAM research is fast losing all credibility and is becoming the laughing stock of proper scientists;
- eventually, the notion that ‘ALL SCAM IS RUBBISH’ must filter through into public life;
- in the end, the pseudo-researchers of SCAM will have provided the nail in SCAM’s coffin.
The INTENDED consequence was to promote SCAM.
The UNINTENDED consequence will be to destroy SCAM.
This self-destructive course of SCAM might be applauded by some skeptics. However, if you believe (as I do) that there are a few good things to be found in SCAM, this development can only be regrettable.
What can be done to avert such a negative outcome?
I wish I knew!
But four productive steps might be the following:
- make sure researchers are adequately trained and supervised to do sound science;
- motivate funding agencies to stop supporting pseudo-science;
- ensure that journal editors and reviewers realize they have the responsibility to avoid publishing nonsense
- motivate Medline to de-list a few of the worst SCAM journals.
“Today, scientists note that the glycyrrhizic acid contained in this plant prevents the development of a new coronavirus, which the whole world is fighting against. Moreover, even a small concentration of an aqueous extract of licorice root has a neutralizing effect.”

These are the words of President Gurbanguly Berdymukhamedov of Turkmenistan. The plant he referred to is licorice. With is the promotion of a herbal solution for the pandemic, he is in good company:
- Thailand’s health ministry approved the use of Andrographis Paniculata, commonly known as green chiretta, to treat patients who are in the early stages of a Covid-19 infection.
- The health authorities of Tamil Nadu distributed herbal medicine to the general public as a preventive measure against Coronavirus disease.
- Madagascar claims to have a cure for Covid-19, the herbal tea named Covid-Organics has the plant artemisia as an ingredient.
- China has been using TCM alongside conventional treatment methods to treat Covid-19 patients. Some of the herbal formulations used in the treatment are:
- Jinhua Qinggan Granule
- Sheganmahuang decoction
- Lianhuaqingwen capsule
- Maxingshigan decoction
- Xuebijing Injection
- Indonesia is testing two herbal medicines: Cordyceps militaris, a fungus common in the Himalayas, and a herbal formulation comprising Ginger, gripeweed, Ngai camphor, and Andrographis paniculata.
And what about some evidence? In 2020, Medline listed 302 articles on herbal medicine for COVID-19. Here I selected just 10 of them to give you a flavor:
COVID-19 is the most recently discovered coronavirus infectious disease and leads to pandemic all over the world. The clinical continuum of COVID-19 varies from mild illness with non-specific signs and symptoms of acute respiratory disease to extreme respiratory pneumonia and septic shock. It can transmit from animal to human in the form of touch, through the air, water, utensils, fomite and feco-oral route blood. The pathogenesis and clinical features of COVID-19 be the same as the clinical manifestation associated epidemic Fever. In Unani medicine, various herbal drugs are described under the caption of epidemic disease. Great Unani scholar also Avicenna (980-1037 AD) recommended that during epidemic condition movement should be restricted, self-isolation, fumigation around the habitant with perfumed herbs (Ood, Kafoor, Sumbuluttib, Saad Kofi, Loban, etc.), and use of appropriate antidotes (Tiryaqe Wabai) and vinegar (Sirka) as prophylaxis. Herbal approach is based on single (Unnab-Ziziphus jujuba, Sapistan-Cordia myxa, Bahidana-Cydonia oblonga, Khatmi-Althea officinalis, Khubazi-Malva sylvestris, Zafran-Crocus sativus, Sibr-Aloe barbedensis, Murmuki-Commiphora myrrha, Darchini-Cinnamomum zeylanicum, Qaranfal-Syzygium aromaticum, Rihan-Oscimum sanctum, Habtus Sauda-Nigella sativa, Aslus Sus-Glycyrrhiza glabra, Maghze Amaltas-Cassia fistula and Adusa-Adhatoda vasica) and compound drugs (Habbe Bukhar, Sharbat Khaksi, Sharbat Zanjabeel, Naqu Nazla, Majoon Chobchini, Jawrish Jalinus and Khamira Marvareed) most of them are claimed for anti-viral, anti-pyretic, blood purifier, cardioprotective and expectorant activities. Traditionally most of the herbal practitioners are using it.
According to the World Health Organization (WHO), viral diseases continue to rise, and pose a significant public health problem. Novel coronavirus disease (COVID-19) is an infectious disease caused by SARS-CoV-2. The pathogenesis and clinical manifestations of COVID-19 is close to Amraz-e-Wabai (epidemic diseases) which was described by Hippocrates, Galen, Aristotle, Razes, Haly Abbas, Avicenna, Jurjani etc. Presently, there is no specific or challenging treatment available for COVID-19. Renowned Unani Scholars recommended during epidemic situation to stay at home, and fumigate the shelters with aromatics herbs like Ood kham (Aquilaria agallocha Roxb.), Kundur (Boswellia serrata Roxb), Kafoor (Cinnamomum camphora L.), Sandal (Santalum album L), Hing (Ferula foetida L.) etc. Use of specific Unani formulations are claimed effective for the management of such epidemic or pandemic situation like antidotes (Tiryaqe Wabai, Tiryaqe Arba, Tiryaqe Azam, Gile Armani), Herbal Decoction (Joshandah), along with Sharbate Khaksi, Habbe Bukhar, Sharbate Zanjabeel, Khamira Marwareed, Jawarish Jalinus, and Sirka (vinegar). Such drugs are claimed for use as antioxidant, immunomodulatory, cardiotonic, and general tonic actions. The study enumerates the literature regarding management of epidemics in Unani medicine and attempts to look the same in the perspective of COVID-19 prevention and management.
Unani system of medicine is based on the humoral theory postulated by Hippocrates, according to him the state of body health and disease are regulated by qualitative and quantitative equilibrium of four humours. Amraz-e-Waba is an umbrella term which is used in Unani medicine for all types of epidemics (smallpox, measles, plague, Hameer Saifi, influenza, Nipaha, Ebola, Zika, and 2019 novel coronavirus, etc.) mostly fatal in nature. The coronavirus disease 2019 (COVID-19) is a severe acute respiratory infection, and the pathogenesis and clinical features resemble with those of Nazla-e-Wabaiya (influenza) and Zatul Riya (pneumonia) which were well described many years ago in Unani text such as high-grade fever, headache, nausea and vomiting, running nose, dry cough, respiratory distress, alternate and small pulse, asthenia, foul smell from breath, insomnia, frothy stool, syncope, coldness in both upper and lower extremities, etc. The World Health Organization declared COVID-19 as a global emergency pandemic. Unani scholars like Hippocrates (370-460 BC), Galen (130-200 AD), Rhazes (865-925 AD), and Avicenna (980-1037 AD) had described four etiological factors for Amraz-e-Waba viz., change in quality of air, water, Earth, and celestial bodies, accordingly mentioned various preventive measures to be adopted during epidemics such as restriction of movement, isolation or “quarantena”, and fumigation with loban (Styrax benzoin W. G. Craib ex Hartwich.), sandalwood (Santalum album L.), Zafran (Crocus sativus L.), myrtle (Myrtus communis L.), and roses (Rosa damascena Mill.) and use of vinegar (sirka) and antidotes (Tiryaq) as prophylaxis, and avoiding consumption of milk, oil, sweet, meat, and alcohol. This review focuses and elaborates on the concept, prevention, and probable management of COVID-19 in the light of Amraz-e-Waba.
Background: Current recommendations for the self-management of SARS-Cov-2 disease (COVID-19) include self-isolation, rest, hydration, and the use of NSAID in case of high fever only. It is expected that many patients will add other symptomatic/adjuvant treatments, such as herbal medicines.
Aims: To provide a benefits/risks assessment of selected herbal medicines traditionally indicated for “respiratory diseases” within the current frame of the COVID-19 pandemic as an adjuvant treatment.
Method: The plant selection was primarily based on species listed by the WHO and EMA, but some other herbal remedies were considered due to their widespread use in respiratory conditions. Preclinical and clinical data on their efficacy and safety were collected from authoritative sources. The target population were adults with early and mild flu symptoms without underlying conditions. These were evaluated according to a modified PrOACT-URL method with paracetamol, ibuprofen, and codeine as reference drugs. The benefits/risks balance of the treatments was classified as positive, promising, negative, and unknown.
Results: A total of 39 herbal medicines were identified as very likely to appeal to the COVID-19 patient. According to our method, the benefits/risks assessment of the herbal medicines was found to be positive in 5 cases (Althaea officinalis, Commiphora molmol, Glycyrrhiza glabra, Hedera helix, and Sambucus nigra), promising in 12 cases (Allium sativum, Andrographis paniculata, Echinacea angustifolia, Echinacea purpurea, Eucalyptus globulus essential oil, Justicia pectoralis, Magnolia officinalis, Mikania glomerata, Pelargonium sidoides, Pimpinella anisum, Salix sp, Zingiber officinale), and unknown for the rest. On the same grounds, only ibuprofen resulted promising, but we could not find compelling evidence to endorse the use of paracetamol and/or codeine.
Conclusions: Our work suggests that several herbal medicines have safety margins superior to those of reference drugs and enough levels of evidence to start a clinical discussion about their potential use as adjuvants in the treatment of early/mild common flu in otherwise healthy adults within the context of COVID-19. While these herbal medicines will not cure or prevent the flu, they may both improve general patient well-being and offer them an opportunity to personalize the therapeutic approaches.
Recently, the novel life-threatening coronavirus infection (COVID-19) was reported at the end of 2019 in Wuhan, China, and spread throughout the world in little time. The effective antiviral activities of natural products have been proved in different studies. In this review, regarding the effective herbal treatments on other coronavirus infections, promising natural products for COVID-19 treatment are suggested. An extensive search in Google Scholar, Science Direct, PubMed, ISI, and Scopus was done with search words include coronavirus, COVID-19, SARS, MERS, natural product, herb, plant, and extract. The consumption of herbal medicine such as Allium sativum, Camellia sinensis, Zingiber officinale, Nigella sativa, Echinacea spp. Hypericum perforatum, and Glycyrrhiza glabra, Scutellaria baicalensis can improve the immune response. It seems that different types of terpenoids have promising effects in viral replication inhibition and could be introduced for future studies. Additionally, some alkaloid structures such as homoharringtonine, lycorine, and emetine have strong anti-coronavirus effects. Natural products can inhibit different coronavirus targets such as S protein (emodin, baicalin) and viral enzymes replication such as 3CLpro (Iguesterin), PLpro (Cryptotanshinone), helicase (Silvestrol), and RdRp (Sotetsuflavone). Based on previous studies, natural products can be introduced as preventive and therapeutic agents in the fight against coronavirus.
Background: The aim of the present review is to provide basic knowledge about the treatment of Coronavirus via medicinal plants. Coronavirus (COVID-19, SARS-CoV, and MERS-CoV) as a viral pneumonia causative agent, infects thousands of people in China and worldwide. There is currently no specific medicine or vaccine available and it is considered a threat to develop effective novel drug or anti-coronavirus vaccine treatment. However, natural compounds to treat coronaviruses are the most alternative and complementary therapies due to their diverse range of biological and therapeutic properties.
Methods: We performed an open-ended, English restricted search of Scopus database, Web of Science, and Pubmed for all available literature from Jan-March, 2020, using terms related to phytochemical compounds, medicinal plants and coronavirus.
Results: The view on anti-coronavirus (anti-CoV) activity in the plant derived phytochemicals and medicinal plants give the strong base to develop a novel treatment of corona virus activity. Various phytochemicals and medicinal plant extracts have been revised and considered to be the potential anti-CoV agents for effective control and future drug development. We discuss some important plants (Scutellaria baicalensis, Psorothamnus arborescens, Glycyrrhiza radix, Glycyrrhiza uralensis , Lycoris radiate, Phyllanthus emblica, Camellia sinensis, Hyptis atrorubens Poit, Fraxinus sieboldiana, Erigeron breviscapus, Citri Reticulatae Pericarpium, Amaranthus tricolor, Phaseolus vulgaris, Rheum palmatum, Curcuma longa and Myrica cerifera) emerged to have broad spectrum antiviral activity.
Conclusion: Nigella sativa has potent anti-SARS-CoV activity and it might be useful souce for developing novel antiviral therapies for coronaviruses.
COVID-19 has been declared a pandemic by WHO on March 11, 2020. No specific treatment and vaccine with documented safety and efficacy for the disease have been established. Hence it is of utmost importance to identify more therapeutics such as Chinese medicine formulae to meet the urgent need. Qing Fei Pai Du Tang (QFPDT), a Chinese medicine formula consisting of 21 herbs from five classical formulae has been reported to be efficacious on COVID-19 in 10 provinces in mainland China. QFPDT could prevent the progression from mild cases and shorten the average duration of symptoms and hospital stay. It has been recommended in the 6th and 7th versions of Clinical Practice Guideline on COVID-19 in China. The basic scientific studies, supported by network pharmacology, on the possible therapeutic targets of QFPDT and its constituent herbs including Ephedra sinica, Bupleurum chinense, Pogostemon cablin, Cinnamomum cassia, Scutellaria baicalensis were reviewed. The anti-oxidation, immuno-modulation and antiviral mechanisms through different pathways were collated. Two clusters of actions identified were cytokine storm prevention and angiotensin converting enzyme 2 (ACE2) receptor binding regulation. The multi-target mechanisms of QFPDT for treating viral infection in general and COVID-19 in particular were validated. While large scale clinical studies on QFPDT are being conducted in China, one should use real world data for exploration of integrative treatment with inclusion of pharmacokinetic, pharmacodynamic and herb-drug interaction studies.
In December 2019, a novel coronavirus SARS-CoV-2, causing the disease COVID-19, spread from Wuhan throughout China and has infected people over 200 countries. Thus far, more than 3,400,000 cases and 240,000 deaths have occurred worldwide, and the coronavirus pandemic continues to grip the globe. While numbers of cases in China have been steadying, the number of infections outside China is increasing at a worrying pace. We face an urgent need to control the spread of the COVID-19 epidemic, which is currently expanding to a global pandemic. Efforts have focused on testing antiviral drugs and vaccines, but there is currently no treatment specifically approved. Traditional Chinese medicine (TCM) is grounded in empirical observations and the Chinese people use TCM to overcome these sorts of plagues many times in thousands of years of history. Currently, the Chinese National Health Commission recommended a TCM prescription of Qing-Fei-Pai-Du-Tang (QFPDT) in the latest version of the “Diagnosis and Treatment guidelines of COVID-19” which has been reported to provide reliable effects for COVID-19. While doubts about TCM still exist today, this review paper will describe the rationalities that QFPDT is likely to bring a safe and effective treatment of COVID-19.
The fight against the novel coronavirus pneumonia (namely COVID-19) that seriously harms human health is a common task for all mankind. Currently, development of drugs against the novel coronavirus (namely SARS-CoV-2) is quite urgent. Chinese medical workers and scientific researchers have found some drugs to play potential therapeutic effects on COVID-19 at the cellular level or in preliminary clinical trials. However, more fundamental studies and large sample clinical trials need to be done to ensure the efficacy and safety of these drugs. The adoption of these drugs without further testing must be careful. The relevant articles, news, and government reports published on the official and Preprint websites, PubMed and China National Knowledge Infrastructure (CNKI) databases from December 2019 to April 2020 were searched and manually filtered. The general pharmacological characteristics, indications, adverse reactions, general usage, and especially current status of the treatment of COVID-19 of those potentially effective drugs, including chemical drugs, traditional Chinese medicines (TCMs), and biological products in China were summarized in this review to guide reasonable medication and the development of specific drugs for the treatment of COVID-19.
Objective: To analysis the medication characteristics of the prescriptions issued via open channel by the National and Provincial Health Committee and the State Administration of Traditional Chinese Medicine in treating coronavirus disease 2019 (COVID-19).
Methods: We collected the data of traditional Chinese medicine related to treatment plans published by the National and Provincial Health Committee and the State Administration of Traditional Chinese Medicine from the start of COVID-19 outbreak to February 19, 2020. The frequency analysis, cluster analysis and association analysis were performed.
Results: The study collected 4 national and 34 regional prevention and treatment plans, 578 items, 84 traditional Chinese formulations, 60 Chinese patent medicines, and 230 Chinese herbs. The high frequently used herbs were Liquorice, Scutellariabaicalensis, Semen armeniacaeamarae, and Gypsum. The commonly used traditional formulations included Maxing Shigan decoction, Yin Qiao powder, and Xuanbai Chengqi decoction. The Chinese patent drugs included Angong Niuhuang pill, Xuebijing injection, and Lianhua Qingwen capsule. The most common paired medications were Ephedra and Semen armeniacaeamarae, Fructusforsythiae and Liquorice. Two core combinations and one novel formula were discovered in the study.
Conclusions: Yin Qiao powder and Huopo Xialing decoction are the basic formulations for Weifen syndrome of COVID-19. In addition, Maxing Shigan decoction, Liang Ge powder, Qingwen Baidu decoction and Da Yuan decoction are the basic formulations for Qifen syndrome of COVID-19. The main medication characteristics are clearing heat, entilating lung, removing toxicity and removing turbidity. It shows that removing toxicity and eliminating evil are the prescription thought in treating epidemic disease of traditional Chinese medicine.
Confused?
Me too!
What seems to emerge is this:
- ‘Herbalists and Co’ did not wait long to jump on the corona bandwagon.
- They managed to confuse not just you and me, but even politicians, presidents, and their advisers.
- They produced a plethora of articles implying that an endless array of herbs might be effective.
- In doing so, no clear consensus emerged as to which herbs are the most promising.
- Sound evidence seems to be not available.
- Clinical trials are slow to start or not even planned.
- Everything is based on more or less wild extrapolation.
- Much of what is being published is borderline irresponsible.
- YET, IT MUST BE GOOD FOR BUSINESS!
THE TELEGRAPH is not my favourite paper, but occasionally it does publish something worth reading – like, for instance, yesterday when it carried this article:
The head of NHS England warned homeopaths had “crossed the line” after a Sunday Telegraph investigation revealed some were peddling myths that taking duck extract was as effective as the coronavirus vaccines.
Sir Simon Stephens warned people taking their advice from homeopaths were putting themselves at greater risk, and warned they would slow down the nation’s vaccine efforts. His calls were echoed by Professor Stephen Powis, the NHS medical director, who said the findings were the “latest in a long line of disturbing and potentially dangerous online myths”…
Sir Simon told the Sunday Telegraph: “It’s one thing for homeopaths to peddle useless but harmless potions, but they cross a dangerous line when making ridiculous assertions about protecting people from Covid infection. “Anyone who took those seriously would be putting themselves at higher risk of coming to harm from Covid infection.” Prof Powis added: “Spouting claims on social media about Covid cures that are not backed by scientific evidence and accurate public health advice is the latest in a long line of disturbing and potentially dangerous online myths. We urge everyone to ignore misleading claims and get vital protection against Covid when they are invited for their vaccine.” …
Helen Earner, operations director at the Charity Commission, said the findings were being examined as “a matter of urgency”. She added: “Any claims that a charity may be providing misinformation during this time of national emergency is a matter of serious concern to the Commission.” She added that a regulatory compliance case had been opened into the matter and that the commission will be liaising with other agencies as part of the investigation…
These days, I read such articles with mixed feelings. On the one hand, I applaud the fact that UK officials do take note of dangerous quackery and promise to take action. On the other hand, I cannot help feeling a bit frustrated and ask myself: WHY HAS IT TAKEN THEM SO LONG?
I know, for instance, that the Charity Commission has long been dragging its feet to do something about charities that promote overtly dangerous quackery. I have discussed such charities three years ago, and others have done so even before me. As to the UK homeopaths’ (and other practitioners of so-called alternative medicine, SCAM) dangerously bizarre attitude towards vaccinations, I started providing evidence and warning the public as early as 1995.
Perhaps they did not know about it?
Yes, perhaps – I only published these warnings in the
BRITISH JOURNAL OF GENERAL PRACTICE
and in the
This gets even more frustrating when I consider that the anti-vaccination attitude in SCAM is merely one facet of a much bigger and much more important subject. Starting also in 1995, I published dozens of papers, gave hundreds of lectures on it, and often called it the ‘indirect risks‘ of SCAM. They can be summarised in one single sentence:
EVEN IF A SCAM IS TOTALLY HARMLESS, THE SCAM PRACTITIONER OFTEN ISN’T.
It is therefore tempting to shout:
I TOLD YOU SO!
But that would hardly be helpful. Instead, I let me beg Sir Simon Stephens, Prof Powis, Helen Earner, and anyone else in a position of power to take a minute and consider the wider implications of tolerating SCAM practitioners impose their overtly dangerous health-related views on the unsuspecting public.
Guest post by Ken McLeod
On 31 March 2020, the Chiropractic Board of Australia issued a statement1 to all Australian chiropractors that they:
“should not make advertising claims on preventing or protecting patients and health consumers from contracting COVID-19 or accelerating recovery from COVID-19. To do so involves risk to public safety and may be unlawful advertising. For example, we are seeing some advertising claims that spinal adjustment/manipulation, acupuncture and some products confer or boost immunity or enhance recovery from COVID-19 when there is no acceptable evidence in support.
“Advertisers must be able to provide acceptable evidence of any claims made about treatments that benefit patients/health consumers. We will consider taking action against anyone found to be making false or misleading claims about COVID-19 in advertising. If the advertiser is a registered health practitioner, breaching advertising obligations is also a professional conduct matter which may result in disciplinary action, especially where advertising is clearly false, misleading or exploitative.”
What could be clearer than that?
So what was published by a registered chiropractor on 16 March 2020, two weeks before the Board’s warning, and is still on his website 10 months later? You guessed it, a video on the website of chiropractor Morgan Weber, a video ‘Coronavirus – Balancing the hysteria…’, 2 in which he says:
– the COVID-19 19 pandemic is all ‘hysteria’ and ‘what have we got to worry about’, because ‘Our body, (has) 51 trillion cells’ vs ‘A one single-cell virus,’ (sic.) ‘51 trillion cells that orchestrate our immune system, every function. Yet we seem to have more faith and trust in ‘medicine’ than we do in this amazing body we call home. Crazy, right? Crazy.’
Weber further downplays the crisis by saying ‘Enough of this nonsense about the big bad bug and all the worry about washing your hands.’
Weber, after denigrating evidence-based medicine, recommends instead:
– ‘Keep up with your chiropractic adjustments….’
Weber is a registered chiropractor practicing at Wave Chiropractic, Maroochydore, Queensland, Australia. His AHPRA registration is CHI0001601286. Weber’s webpage home site is at https://www.wavechiropractic.com.au/index.php
WEBER’S VIDEO:
Since 16 March 2020 Weber has posted a video on his website a video ‘Coronavirus – Balancing the hysteria…’. 3
Weber says:
BEGINS TRANSCRIPT
00:00. Hi everyone. Hasn’t it been fascinating lately? The news, the hysteria. Everything has gone almost upside-down. Crazy. I found it so fascinating.
00:12. So today we thought we would have a bit of a chat and sort of balance the scales and the story getting told out there in the mass media. I hope you’ve got your toilet paper stockpiled and sorted ha ha ha ha. It’s hilarious to see people coming and going with huge amounts under their arms as they come out of the grocery store. Crazy isn’t it, crazy times.
00:42. So let’s think about if for a second, and if we bypass all that hysteria and noise and just think a little bit about this. Our body, 51 trillion cells. A one single-cell virus. My gosh. What have we got to worry about? We have this amazing system. 51 trillion cells that orchestrate our immune system, every function. Yet we seem to have more faith and trust in ‘medicine’ than we do in this amazing body we call home. Crazy, right? Crazy.
01:20 ‘The other story, the other sort of facts behind what we do, and I (unintelligible) told a fair few of you of this already, how the immune system works. So, across the road from Waves, we have a really kind of bare patch of grass, just before you go onto the beach. Now if I took a handful of seeds. Now this is an analogy for how our system works, and how amazing our body’s immune system is. If I took a bunch of seeds and dropped them onto the ground, some grass seeds, not all of those seeds would take. There needs to be a hospitable environment, a moist warm sunlit area for those seeds to take, then root and grow into a fully mature grass and perpetuate on and on and on. However that area across the road is barren rocky sandy and yuck. You drop those seeds, most of those are going to blow off and away because that area is a no-go, it’s got a strong resistance, a barrier, a non-hospitable environment.
02:18. Now that is how our immune system works. Now the story I feel that should be out there, is what are you doing to nurture your body to do the best it can be, to have the strongest barrier it can be.
02: 30. Enough of this nonsense about the big bad bug and all the worry about washing your hands. ‘Cause I tell you what, if you are neglecting to nurture your body and the 51 trillion cells to be the best they can be, watch out, that may not be enough, washing your hands.
02:47. So let’s talk about that. How do we orchestrate a healthy system that has a strong immune barrier to anything that’s out there? And really guys, this should be a day-to-day forte (?) for everyone who just wants to be their best.
03:00. So let’s go through it. Boosting your barriers. You need to trust your body. First and foremost, the 51 trillion cells are remarkable. Trust in that.
03: 12. You’ve gotta eat well. Eat well with nutrient-dense, mineral-dense foods. Stay well hydrated. Move. You’ve gotta move well. Exercise your body regularly, moving all parts in all directions. Enjoy healthy sunlight exposure. You’ve gotta think well. Follow your passions and purpose. Think positively. Perhaps switch off the TV.
03:41. Keep up with your chiropractic adjustments. An optimal brain and body communication via the nervous system is vital so ensuring your body is in a surviving state. Do all these things guys. Up the ante of them. Go in harder with your (unintelligible) exercises, your hydration etcetera, and trust in your body. It’s amazing. It’s built with this in-built protective mechanism. Foster it. Help to balance that story out there, and help people to take on a more useful interpretation of this current crisis out there.
04:19. I hope this was of value and you guys enjoy.
END TRANSCRIPT
The regulator has been informed. As the world’s death toll rockets past 2 million, we wait to see if they really meant what they said about disciplinary action.
On 10/1/2021 THE GUARDIAN reported about some bizarre anthroposophic treatments in Germany. About a month before, we had discussed the issue here on this blog. The GUARDIAN article prompted the following press release, dated 12/1/2021, by the ‘International Federation of Anthroposophic Medical Associations’ (oddly abbreviated IVAA):
IVAA welcomes the reporting by The Observer, a sister paper of The Guardian, on the care of Covid-19 patients in German anthroposophic hospitals, including critically ill patients in the intensive care ward. The article rightly highlights how these treatments are provided in addition to state-of-the-art conventional treatments, how anthroposophic medicine is fully integrated into the German health care system and how anthroposophy “enjoys a high level of social acceptance and institutional support in German-speaking countries”. The World Health Organization’s Traditional Medicine Strategy has indeed set integration of traditional and complementary medicine into health care systems as one of its strategic goals.
While the article is generally biased against anthroposophic medicine and only quotes two known opponents of anthroposophy, it nevertheless provides welcome reporting on integrative medicine that is highly popular with patients in Europe.
There are many peer-reviewed studies on anthroposophic medicine and anthroposophic medications have been in use for decades, showing an excellent safety profile. The Observer’s critique that patients should provide consent for such treatments does not hold because the treatments are not experimental, are provided in addition to standard care, based on long clinical experience and in hospitals openly publicizing their integrative medicine approach. As the article reports, German insurance companies pay flat-rate payments for hospital treatment of coronavirus patients; the additional anthroposophic treatments are thus financed out of hospital budgets and are cost-neutral for insurance companies.
Unfortunately, and as correctly reported by The Observer, individual supporters of anthroposophic medicine have sided with demonstrations against corona measures; this does in no way reflect the official position of anthroposophic medicine and IVAA member organizations have clearly distanced themselves.
END OF PRESS RELEASE
One does not need to be a champion in critical thinking to realize that this press release deserves a few comments.
- The claim that anthroposophic medicine (AM) is ‘fully integrated into the German healthcare system‘ is misleading. In Germany, AM belongs to the special therapeutic measures (‘besondere Therapierichtungen’) which indicates almost the opposite of ‘fully integrated’.
- Similarly, AM is not ‘highly accepted’ but belongs to the fringe of so-called alternative medicine (SCAM). There are only very few anthroposophic hospitals in Germany, and most Germans would not even know what AM is.
- The press release claims that ‘there are many peer-reviewed studies on anthroposophic medicine‘. The link it provides leads to an AM organization’s list of references. For infections, this list references the following 9 papers: (1) Martin DD. Fever: Views in Anthroposophic Medicine and their Scientific Validity. Evid Based Complement Alternat Med. 2016;2016(1):13 pages.(2) Soldner G, Stellman HM. Individual Paediatrics: Physical, Emotional and Spiritual Aspects of Diagnosis and Counseling – Anthroposophic-homeopathic Therapy, Fourth edition. 4 edition. CRC Press; 2014. 984 S. (3) Glöckler M, Goebel W. A Guide to Child Health: A Holistic Approach to Raising Healthy Children. Floris Books; 2013. (4) Goebel MW, Michael MK, Glöckler MM. Kindersprechstunde: ein medizinisch-pädagogischer Ratgeber. Verlag Urachhaus; 2016. (5) Szoeke H, Marodi M, Sallay Z, Székely B, Sterner M-G, Hegyi G. Integrative versus Conventional Therapy of Chronic Otitis Media with Effusion and Adenoid Hypertrophy in Children: A Prospective Observational Study. Forsch KomplementärmedizinResearch Complement Med. 2016;23(4):231–239. (6) Hamre HJ, Glockmann A, Schwarz R, Riley DS, Baars EW, Kiene H, u. a. Antibiotic use in children with acute respiratory or ear infections: prospective observational comparison of anthroposophic and conventional treatment under routine primary care conditions. Evid Based Complement Alternat Med. 2014;2014(Article ID 243801). (7) Hamre HJ, Fischer M, Heger M, Riley D, Haidvogl M, Baars E, u. a. Anthroposophic vs. conventional therapy of acute respiratory and ear infections. Wien Klin Wochenschr. 2005;117(7–8):256–268. (8) Hamre HJ, Glockmann A, Fischer M, Riley DS, Baars E, Kiene H. Use and Safety of Anthroposophic Medications for Acute Respiratory and Ear Infections: A Prospective Cohort Study. Drug Target Insights. 14. September 2007;2:209–19. (9) Jeschke E, Lüke C, Ostermann T, Tabali M, Huebner J, Matthes H. Verordnungsverhalten anthroposophisch orientierter Ärzte bei akuten Infektionen der oberen Atemwege. Forsch KomplementärmedizinResearch Complement Med. 2007;14(4):207–215. These are mostly NOT peer-reviewed papers, and none yields anything close to conclusive findings about the alleged efficacy of AM treatments. The truth is that there is no good evidence to support AM.
- The mention that AM remedies have been used for decades is a fallacy (appeal to tradition).
- Yes, AM remedies are safe – mainly because they, like homeopathic remedies, usually contain no active ingredients.
- Patients should provide consent for such treatments to ALL treatments, experimental or not.
- Clinicians practicing AM have long been known to hold an anti-vax attitude which has also caused problems in the past.
My conclusion: this press release was written in true anthroposophic style and spirit: ill-informed, in disregard of medical ethics, based on wishful thinking and aimed at misleading the public.
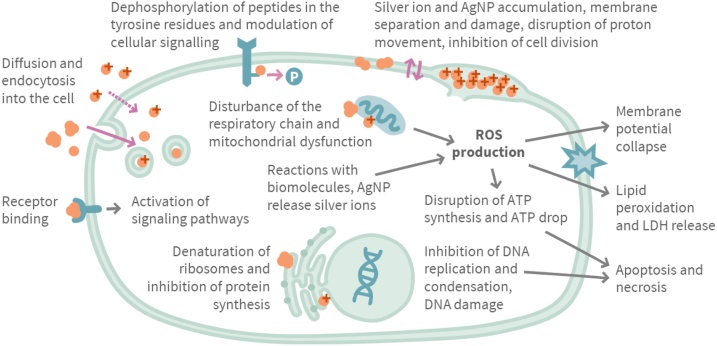
The aim of this investigation was to evaluate the marketing practices, beliefs and health claims regarding the use of colloidal silver in Finland. Contents of three company websites selling colloidal silver were reviewed, and the claims used in the marketing of colloidal silver were compared to the scientific information about silver. In Facebook posts and discussion about colloidal silver were analyzed.
In Finland, the marketing of colloidal silver products on websites selling the products did not follow the regulations of authorities; several scientifically unfounded claims about the efficacy and medical use of colloidal silver were found. After the Finnish Broadcasting Company (Yle) documentary and an intervention by authorities, contents of the websites were changed, but still questionable information and misleading claims could be found. In the analyzed Facebook groups attitudes towards medical use of colloidal silver were uncritically positive, internal use was highly promoted and the restrictions of use were considered unjustified.
The authors concluded that the use of quackery products such as colloidal silver can be dangerous, and their use and marketing should be controlled and restricted.
The authors stress that silver nanoparticles (AgNPs) are potentially toxic due to their small size and Ag+-release capabilities, and the use of colloidal silver products containing AgNPs can cause a wide variety of adverse effects such as argyria.
WebMD cautions that despite promoters’ claims, silver has no known function in the body and is not an essential mineral supplement. Colloidal silver products were once available as over-the-counter drug products. In 1999 the U.S. Food and Drug Administration (FDA) ruled that these colloidal silver products were not considered safe or effective. Colloidal silver products marketed for medical purposes or promoted for unproven uses are now considered “misbranded” under the law without appropriate FDA approval as a new drug. There are currently no FDA-approved over-the-counter or prescription drugs containing silver that are taken by mouth. However, there are still colloidal silver products being sold as homeopathic remedies and dietary supplements.
On this blog, we have discussed that colloidal silver is nevertheless marketed aggressively by crooks (see here and here). The message that emerges from all this seems clear: do not fall for the plethora of false claims made by irresponsible entrepreneurs who want your money and risk your health. Keep your money and health by staying away from colloidal silver and similar SCAMs.
It’s sad but true: not everyone likes THE ALTERNATIVE MEDICINE HALL OF FAME. Take this recent comment, for instance:
It is pathetic to see that Edzard only engages in the systematic harassment of his former colleagues or people who in most cases ignore him. Perhaps because he knows that his battle against homeopathy was totally lost in Germany, Switzerland and Brazil, as could be seen in the imminent failure of the “Questao Da Ciencia Institute”… Edzard acts as a real bully against Dr. Jacobs by including her in a “hall of fame” to humiliate her before the hoolingans who applaud her, who are always the four guardian trolls who never contribute or benefit to the discussion…
But then there are others who do appreciate it and recognize that it serves an important purpose: to alert the public to the fact that there is something deeply wrong with much of the published research in so-called alternative medicine (SCAM). Incidentally, this was also the theme of my last post on acupuncture and is the topic of many of my recent articles. Thus the aim of my HALL OF FAME is not to humiliate anyone; it is merely one of many of my attempts to protect the public from misleading information that has the potential to do much harm.
And therefore, I am not likely to close the HALL OF FAME any time soon.
Someone who has been waiting for ages to get admitted is the prolific psychologist Professor Harald Walach. He has in the past changed employment frequently. After building up a research group in SCAM at the University Hospital in Freiburg he held a research professorship with the University of Northampton, UK from 2005-2009 where he directed the MSc Program of Transpersonal Psychology and Consciousness Studies. From 2010 to 2016, he worked at the European University Viadrina in Frankfurt (Oder), where he headed a postgraduate Master program training doctors in SCAM and cultural sciences. Currently, Walach is affiliated with three institutions:
- Department of Pediatric Gastroenterology, Medical University Poznan, Poznan, Poland.
- Department of Psychology, University Witten-Herdecke, Witten, Germany.
- Change Health Science Institute, Berlin, Germany
In 2012, Walach was elected pseudoscientist of the year, a fact that should almost automatically unlock the HALL’s door for him. But let’s not be hasty; let’s have a look at his publications. My Medline search for ‘Walach H, clinical trial’ generated 40 hits of which 19 related to clinical studies of so-called alternative medicine (SCAM). Here are their conclusions:
- Both physiotherapy and PPT improve subacute low back pain significantly. PPT is likely more effective and should be studied further.
- One treatment session of enhanced MMT physiotherapy or RegentK can lead to nearly full function and thus recovery of a ruptured ACL after 1 year.
- MBSR did not produce cardiac autonomic benefits or changes in daily activity in FM. Furthermore, the lack of an association between patient-experienced clinical improvement and objective physiological measures suggests that subjective changes in the wellbeing of FM patients over time are not related to alterations in the cardiorespiratory autonomic function or activity levels.
- Mindfulness therapy may prevent disability pension and it may have a potential to significantly reduce societal costs and increase the effectiveness of care. Accumulated weeks of unemployment and sickness benefit are possible risk factors for BDS.
- Mindfulness therapy is a feasible and acceptable treatment. The study showed that mindfulness therapy was comparable to enhanced treatment as usual in improving quality of life and symptoms.
- In conclusion, primary outcome analyses did not support the efficacy of MBSR in fibromyalgia, although patients in the MBSR arm appeared to benefit most.
- Homeopathic remedies produce different symptoms than placebo.
- We, therefore, conclude that homeopathic remedies produce more symptoms typical for a remedy than non-typical symptoms. The results furthermore suggest a somewhat non-classical pattern because symptoms of one remedy appear to be mimicked in the other trial arm. This might be indicative of entanglement in homeopathic systems.
- In patients with CFS, distant healing appears to have no statistically significant effect on mental and physical health but the expectation of improvement did improve outcome.
- Treatments with QUANTEC may be accompanied by beneficial health effects.
- The results showed that both remedies ‘produced’ significantly more symptoms than placebo. With regard to the specificity, the Calendula officinalis group displayed more remedy-specific symptoms than placebo. However, in the Ferrum muriaticum group more Calendula symptoms than placebo were also recorded.
- Homeopathic proving symptoms appear to be specific to the medicine and do not seem to be due to a local process.
- We conclude that in an unselected sample of headache patients some may indeed be susceptible to the low intensity type of electromagnetic radiation exemplified by sferics pulses.
- We conclude that Bach-flower remedies are an effective placebo for test anxiety and do not have a specific effect.
- Approximately 30% of patients in homeopathic treatment will benefit after 1 y of treatment. There is no indication of a specific, or of a delayed effect of homeopathy.
- There is no indication that belladonna 30CH produces symptoms different from placebo or from no intervention. Symptoms of a homeopathic pathogenetic trial (HPT) are most likely chance fluctuations.
- Chronically ill patients who want to be treated by distant healing and know that they are treated improve in quality of life.
- Mind machines do not have a specific effect on general well-being and physiological relaxation, although they may produce unusual psychological experiences; people with psychiatric illnesses should not use such devices.
- Group evaluation showed no clearcut differences. The claim that homoeopathic potencies can produce symptoms other than placebo in healthy subjects should be put to further scrutiny.
So, as we see, Prof Walach has published many clinical trials on numerous SCAMs . Their majority arrived at positive conclusions. His TI is therefore sky-high. But he has also published studies that were dramatically negative, even some of homeopathy!
The main criterion for admission to THE ALTERNATIVE MEDICINE HALL OF FAME is to have published SCAM research that hardly ever concludes negatively. Does Walach fulfill it? Should he be allowed to join this illustrious group of people?
- Andreas Michalsen ( various SCAMs, Germany)
- Jennifer Jacobs (homeopath, US)
- Jenise Pellow (homeopath, South Africa)
- Adrian White (acupuncturist, UK)
- Michael Frass (homeopath, Austria)
- Jens Behnke (research officer, Germany)
- John Weeks (editor of JCAM, US)
- Deepak Chopra (entrepreneur, US)
- Cheryl Hawk (US chiropractor)
- David Peters (osteopathy, homeopathy, UK)
- Nicola Robinson (TCM, UK)
- Peter Fisher (homeopathy, UK)
- Simon Mills (herbal medicine, UK)
- Gustav Dobos (various SCAMs, Germany)
- Claudia Witt (homeopathy, Germany/Switzerland)
- George Lewith (acupuncture, UK)
- John Licciardone (osteopathy, US)
I have to admit, the decision was not easy in this case. However, after considering all the evidence, I have decided in favour of admission.
WELCOME PROF WALACH!