depression
- mind-body medicine (32.0%),
- massage (16.1%),
- chiropractic (14.4%),
- acupuncture (3.4%),
- naturopathy (2.2%),
- art and/or music therapy (2.1%).
Reporting post-COVID-19 was associated with an increased likelihood of using any SCAM in the last 12 months (AOR = 1.18, 95% CI [1.03, 1.34], p = 0.014) and specifically to visit an art and/or music therapist (AOR = 2.56, 95% CI [1.58, 4.41], p < 0.001). The overall use of any SCAM was more likely among post-COVID-19 respondents under 65 years old, females, those with an ethnical background other than Hispanic, African-American, Asian or Non-Hispanic Whites, having a higher educational level, living in large metropolitan areas and having a private health insurance.
The American Society of Clinical Oncology (ASCO) and the Society for Integrative Oncology have collaborated to develop guidelines for the application of integrative approaches in the management of:
- anxiety,
- depression,
- fatigue,
- use of cannabinoids and cannabis in patients with cancer.
These guidelines provide evidence-based recommendations to improve outcomes and quality of life by enhancing conventional cancer treatment with integrative modalities.
All studies that informed the guideline recommendations were reviewed by an Expert Panel which was made up of a patient advocate, an ASCO methodologist, oncology providers, and integrative medicine experts. Panel members reviewed each trial for quality of evidence, determined a grade quality assessment label, and concluded strength of recommendations.
The findings show:
- Strong recommendations for management of cancer fatigue during treatment were given to both in-person or web-based mindfulness-based stress reduction, mindfulness-based cognitive therapy, and tai chi or qigong.
- Strong recommendations for management of cancer fatigue after cancer treatment were given to mindfulness-based programs.
- Clinicians should recommend against using cannabis or cannabinoids as a cancer-directed treatment unless within the context of a clinical trial.
- The recommended modalities for managing anxiety included Mindfulness-Based Interventions (MBIs), yoga, hypnosis, relaxation therapies, music therapy, reflexology, acupuncture, tai chi, and lavender essential oils.
- The strongest recommendation in the guideline is that MBIs should be offered to people with cancer, both during active treatment and post-treatment, to address depression.
The authors concluded that the evidence for integrative interventions in cancer care is growing, with research now supporting benefits of integrative interventions across the cancer care continuum.
I am sorry, but I find these guidelines of poor quality and totally inadequate for the purpose of providing responsible guidance to cancer patients and carers. Here are some of my reasons:
- I know that this is a petty point, particularly for me as a non-native English speaker, but what on earth is an INTEGRATIVE THERAPY? I know integrative care or integrative medicine, but what could possibly be integrative with a therapy?
- I can vouch for the fact that the assertion “all studies that informed the guideline recommendations were reviewed” is NOT true. The authors seem to have selected the studies they wanted. Crucially, they do not reveal their selection criteria. I have the impression that they selected positive studies and omitted those that were negative.
- The panel of experts conducting the research should be mentioned; one can put together a panel to show just about anything simply by choosing the right individuals.
- The authors claim that they assessed the quality of the evidence, yet they fail to tell us what it was. I know that many of the trials are of low quality and their results therefore less than reliable. And guidance based on poor-quality studies is misguidance.
- The guidelines say nothing about the risks of the various treatments. In my view, this would be essential for any decent guideline. I know that some of the mentioned therapies are not free of adverse effects.
- They also say nothing about the absolute and relative effect sizes of the treatments they recommend. Such information would ne necessary for making informed decisions about the optimal therapeutic choices.
- The entire guideline is bar any critical thinking.
Overall, these guidelines provide more an exercise in promotion of dubious therapies than a reliable guide for cancer patients and their carers. The ASCO and the Society for Integrative Oncology should be ashamed to have given their names to such a poor-quality document.
The aim of this study was to assess the effectiveness of different forms of walking in reducing symptoms of depression and anxiety. A systematic review and meta-analysis of randomized controlled trials (RCTs) was conducted assessing the effects of walking on depressive and anxiety symptoms. MEDLINE, Cochrane Central Register of Controlled Trials (CENTRAL), Embase, PsycINFO, Allied and Complementary Medicine Database (AMED), CINAHL, and Web of Science were searched on April 5, 2022. Two authors independently screened the studies and extracted the data. Random-effects meta-analysis was used to synthesize the data. Results were summarized as standardized mean differences (SMDs) with 95% CIs in forest plots. The risk of bias was assessed by using the Cochrane Risk of Bias tool.
This review included 75 RCTs with 8636 participants; 68 studies reported depressive symptoms, 39 reported anxiety symptoms, and 32 reported both as the outcomes. One study reported the results for adolescents and was not included in the meta-analysis. The pooled results for adults indicated that walking could significantly reduce depressive symptoms (RCTs: n=44; SMD −0.591, 95% CI −0.778 to −0.403; I2=84.8%; τ2=0.3008; P<.001) and anxiety symptoms (RCTs: n=26; SMD −0.446, 95% CI −0.628 to −0.265; I2=81.1%; τ2=0.1530; P<.001) when compared with the inactive controls. Walking could significantly reduce depressive or anxiety symptoms in most subgroups, including different walking frequency, duration, location (indoor or outdoor), and format (group or individual) subgroups (all P values were <.05). Adult participants who were depressed (RCTs: n=5; SMD −1.863, 95% CI −2.764 to −0.962; I2=86.4%; τ2=0.8929) and those who were not depressed (RCTs: n=39; SMD −0.442, 95% CI −0.604 to −0.280; I2=77.5%; τ2=0.1742) could benefit from walking effects on their depressive symptoms, and participants who were depressed could benefit more (P=.002). In addition, there was no significant difference between walking and active controls in reducing depressive symptoms (RCTs: n=17; SMD −0.126, 95% CI −0.343 to 0.092; I2=58%; τ2=0.1058; P=.26) and anxiety symptoms (14 RCTs, SMD −0.053, 95% CI −0.311 to 0.206, I2=67.7%, τ2=0.1421; P=.69).
The authors concluded that various forms of walking can be effective in reducing symptoms of depression and anxiety, and the effects of walking are comparable to active controls. Walking can be adopted as an evidence-based intervention for reducing depression and anxiety. More evidence on the effect of low-intensity walking is needed in the future.
Clinical trials of walking are encounter considerable methodological difficulties: there is no adequate placebo, for instance. Thus, such studies are often conducted against no treatment or against ‘active control’ which means that the control group receives a therapy of known effectiveness.
The former comparison is not very meaningful because it does not allow us to tell whether the effects are truly caused by walking or by some non-specific effect. The latter comparison is more rigorous but also not perfect because the patients cannot be blinded.
This means we have to accept a degree of uncertainty in estimating the benefit of walking. As walking is not expensive, not hazardous, and has many other health benefits, this caveat seems truly minor. In other words, the findings reported here are encouraging and should be accepted in clinical practice.
Yet, there is still one ‘hair in the soup’: depressed people find it often very hard to motivate themselves to do activities such as walking. Thus, compliance with this treatment might often be less than satisfactory. It might be worth researching how this obstacle can be best overcome.
This study evaluated and compared the effectiveness of Reiki and Qi-gong therapy techniques in improving diabetic patients’ negative emotional states. This quas-experimental research design was carried out at the National Institute of Diabetes and Endocrinology’s Hospital in Cairo, Egypt. It included 200 Type 2 diabetes patients randomized into two equal groups, one for Qigong and one for Reiki techniques. A self-administered questionnaire with a standardized tool (Depression Anxiety Stress Scales [DASS[) was used in data collection. The intervention programs were administered in the form of instructional guidelines through eight sessions for each group.
The results showed that the two study groups had similar socio-demographic characteristics. After implementation of the intervention, most patients in the two groups were having no anxiety, no depression, and no stress. Statistically significant improvements were seen in all three parameters in both groups (p<0.001). The multivariate analysis identified the study intervention as the main statistically significant independent negative predictor of the patients’ scores of anxiety, depression, and stress. Reiki technique was also a statistically significant independent negative predictor of these scores.
The authors conclused that both Reiki and Qi-gong therapy techniques were effective in improving diabetic patients’ negative emotional states of anxiety, depression, and stress, with slight superiority of the Reiki technique. The inclusion of these techniques in the management plans of Type-2 diabetic patients is recommended.
This is an excellent example of how NOT to design a clinical trial!
- If your aim is to test the efficacy of Reiki, conduct a trial of Reiki versus sham-Reiki.
- If your aim is to test the efficacy of Qi-gong, conduct a trial of Qi-gong versus sham-Qi-gong.
- If you compare two therapies in one trial, one has to be of proven and undoubted efficacy.
- Comparing two treatments of unproven efficacy cannot normally lead to a meaningful result.
- It is like trying to solve a mathematical equasion with two unknowns.
- A study that cannot produce a meaningful result is a waste of resorces.
- It arguably also is a neglect of research ethics.
- Even if we disregarded all these flaws and problems, recommending therapies for routine use on the basis of one single study is irresponsible nonsense.
All this is truly elementary and should be known by any researcher (not to mention research supervisor). Yet, in the realm of so-called alternative medicine (SCAM), it needs to be stressed over and over again. The ‘National Institute of Diabetes and Endocrinology’s Hospital in Cairo’ (and all other institutions that produce such shameful pseudoscience) urgently need to get their act together:
you are doing nobody a favour!
The aim of this systematic review and network meta-analysis was to identify the optimal dose and modality of exercise for treating major depressive disorder, compared with psychotherapy, antidepressants, and control conditions.
The screening, data extraction, coding, and risk of bias assessment were performed independently and in duplicate. Bayesian arm based, multilevel network meta-analyses were performed for the primary analyses. Quality of the evidence for each arm was graded using the confidence in network meta-analysis (CINeMA) online tool. All randomised trials with exercise arms for participants meeting clinical cut-offs for major depression were included.
A total of 218 unique studies with a total of 495 arms and 14 170 participants were included. Compared with active controls (eg, usual care, placebo tablet), moderate reductions in depression were found for
- walking or jogging,
- strength training,
- mixed aerobic exercises,
- and tai chi or qigong.
The effects of exercise were proportional to the intensity prescribed. Strength training and yoga appeared to be the most acceptable modalities. Results appeared robust to publication bias, but only one study met the Cochrane criteria for low risk of bias. As a result, confidence in accordance with CINeMA was low for walking or jogging and very low for other treatments.
The authors concluded that exercise is an effective treatment for depression, with walking or jogging, yoga, and strength training more effective than other exercises, particularly when intense. Yoga and strength training were well tolerated compared with other treatments. Exercise appeared equally effective for people with and without comorbidities and with different baseline levels of depression. To mitigate expectancy effects, future studies could aim to blind participants and staff. These forms of exercise could be considered alongside psychotherapy and antidepressants as core treatments for depression.
As far as I can see, there are two main problems with these findings:
- Because too many of the studies are less than rigorous, the results are not quite as certain as the conclusions would seem to imply.
- Patients suffering from a major depressive disorder are often unable (too fatigued, demotivated, etc.) to do and/or keep up vigorous excerise over any length of time.
What I find furthermore puzzling is that, on the one hand, the results show that – as one might expect – the effects are proportional to the intensity of the excercise but, on the other hand tai chi and qugong which are both distinctly low-intensity turn out to be effective.
Nonetheless, this excellent paper is undoubtedly good news and offers hope for patients who are in desperate need of effective, safe and economical treatments.
This study was aimed at evaluating the effectiveness of osteopathic visceral manipulation (OVM) combined with physical therapy in pain, depression, and functional impairment in patients with chronic mechanical low back pain (LBP).
A total of 118 patients with chronic mechanical LBP were assessed, and 86 who met the inclusion criteria were included in the randomized clinical trial (RCT). The patients were randomized to either:
- Group 1 (n=43), who underwent physical therapy (5 days/week, for a total of 15 sessions) combined with OVM (2 days/week with three-day intervals),
- or Group 2 (n=43), which underwent physical therapy (5 days/week, for a total of 15 sessions) combined with sham OVM (2 days/week with three-day intervals).
Both groups were assessed before and after treatment and at the fourth week post-treatment.
Seven patients were lost to follow-up, and the study was completed with 79 patients. Pain, depression, and functional impairment scores were all improved in both groups (p=0.001 for all). This improvement was sustained at week four after the end of treatment. However, improvement in the pain, depression, and functional impairment scores was significantly higher in Group 1 than in Group 2 (p=0.001 for all).
The authors concluded that the results suggest that OVM combined with physical therapy is useful to improve pain, depression, and functional impairment in patients with chronic mechanical low back pain. We believe that OVM techniques should be combined with other physical therapy modalities in this patient population.
OVM was invented by the French osteopath, Jean-Piere Barral. In the 1980s, he stated that through his clinical work with thousands of patients, he discovered that many health issues were caused by our inner organs being entrapped and immobile. According to its proponents, OVM is based on the specific placement of soft manual forces that encourage the normal mobility, tone and function of our inner organs and their surrounding tissues. In this way, the structural integrity of the entire body is allegedly restored.
I am not aware of good evidence to show that OVM is effective – and this, sadly, includes the study above.
In my view, the most plausible explanation for its findings have little to do with OVM itself: sham OVM was applied “by performing light pressure and touches with the palm of the hand on the selected points for OVM without the intention of treating the patient”. This means that most likely patients were able to tell OVM from sham OVM and thus de-blinded. In other words, their expectation of receiving an effective therapy (and not the OVM per se) determined the outcome.
The BBC has a popular program entitled JUST ONE THING presented by Dr, Michael Mosely. In each of these short broadcasts, Mosely presents JUST ONE THING that will make your life more healthy. Whenever I listen to them, I get slightly irritated. Mosely is clearly a very skilled presenter and makes complicated things easy to understand; but for my taste his approach is totally devoid of critical thinking. This is obviously the point of the series and probably one reason for its success. So, maybe it needs to be tolerated – perhaps, but surely not if it seriously misleads the public on important health issues.
The most recent broadcast was entitled EMBRACE THE RAIN and, in my view, it did cross this crucial line. Mosely explained that after it has rained, the air is full of negative ions and these ions are effective against depression. The center piece was his interview with Prof Michael Terman who explained some of his research on the subject, in particular a clinical trial which showed that intensely ionized air was effective against depression. Terman explained that this was more than a placebo effect, that it worked even for serious chronic depressed patients, and that the effect was better than standard treatments.
At no stage was there an even mildly critical question from Mosely. Consequently many depressed patients might now abandon their standard treatments and opt for air ionizers in their homes or walks in the rain which was deemed to be just as effective. In view of the fact that chronic depression, through its suicide risk, can be a life-threatening condition, I find this rather concerning.
My concerns were not exactly alleviated when I did a quick search for the evidence. The most recent review on the subject states that there has been considerable interest in the potential effects of negative air ions (NAIs) on human health and well-being, but the conclusions have been inconsistent and the mechanisms remain unclear. So, why does Terman promote NAIs as though they are the best thing since sliced bread? It took me less than a minute to find a possible answer: he holds a patent for a NEGATIVE ION GENERATOR!
It is laudable of the BBC and Michael Mosely to present aspects of healthcare in a simple, understandable way. Yet, it would be even more laudable, if they did their homework a bit better and, crucially, tried to also educate the public in critical thinking. After all ’embracing the rain’ will not change lives but critical thinking most certainly does!
Acupuncture is questionable.
Acupressure is highly questionable.
Auricular acupressure is extremely questionable.
This study investigated the effect of auricular acupressure on the severity of postpartum blues. A randomized sham-controlled trial was conducted from February to November 2021, with 74 participants who were randomly allocated into two groups of either routine care + auricular acupressure (n = 37), or routine care + sham control (n = 37). Vacaria seeds with special non-latex adhesives were used to perform auricular acupressure on seven ear acupoints. There were two intervention sessions with an interval of five days. In the sham group, special non-latex adhesives without vacaria seeds were attached in the same acupoints as the intervention group. The severity of postpartum blues, fatigue, maternal-infant attachment, and postpartum depression was assessed. 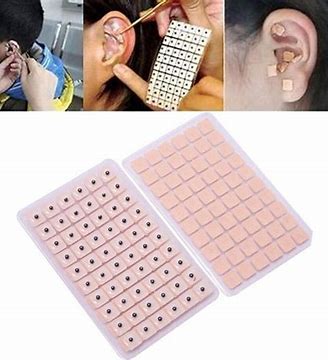
Auricular acupressure was associated with a significant effect in the reduction of postpartum blues on the 10th and 15th days after childbirth (SMD = −2.77 and −2.15 respectively), postpartum depression on the 21st day after childbirth (SMD = −0.74), and maternal fatigue on 10th, 15th and 21st days after childbirth (SMD = −2.07, −1.30 and −1.32, respectively). Also, the maternal-infant attachment was increased significantly on the 21st day after childbirth (SMD = 1.95).
The authors concluded that auricular acupressure was effective in reducing postpartum blues and depression, reducing maternal fatigue, and increasing maternal-infant attachment in the short-term after childbirth.
Let me put my doubts about these conclusions in the form of a few questions:
- If you had sticky tape on your ear, would you sometimes touch it?
- If you touched it, would you feel whether a vacaria seed was contained in it or not?
- Would you, therefore, say that such a trial could be properly blinded (not to forget the therapists who were, of course, in the know)?
- If the trial was thus de-blinded, would you claim that patient expectation did not influence the outcomes?
If you answered all of these questions with NO, you are – like I – of the opinion that the results of this trial could have easily been brought about, not by the alleged effects of acupressure, but by placebo and other non-specific effects.
It has been reported that King Charles refused to pay Prince Andrew’s £ 32,000-a-year bill for his personal healing guru. The Duke of York has allegedly submitted the claim to the Privy Purse as a royal expense having sought the help of a yoga teacher.
However, the claim has reportedly been denied by the King, who is said to have told Andrew the bill will need to be covered using his own money. It comes after sources claimed Andrew has been using the Indian yogi for a number of years for chanting, massages, and holistic therapy in the privacy of his mansion. The healer has reportedly enjoyed month-long stays at a time at the £30 million Royal Lodge in Windsor.
Previously, the Queen seems to have passed the claims. But now Charles is in control. A source said: “While the Queen was always happy to indulge her son over the years, Charles is far less inclined to fund such indulgences, particularly in an era of a cost-of-living crisis. “Families are struggling and would rightly baulk at the idea of tens of thousands paid to an Indian guru to provide holistic treatment to a non-working royal living in his grace and favour mansion. This time the King saw the bill for the healer submitted by Andrew to the Privy Purse and thought his brother was having a laugh.”
________________________
Poor Andrew!
How is he going to cope without his guru?
Will he be able to recover from the mysterious condition that prevents him to sweat?
Will his ego take another blow?
How will he be able to afford even the most basic holistic wellness?
How can Charles – who knows only too well about its benefits – be so cruel to his own brother?
Should I start a collection so that Andrew can pay for his most basic needs?
____________________________
Yes, these are the nagging questions and deep concerns that keep me awake at night!
PS
I have just been asked if, by any chance, the yoga teacher is a 16-year-old female. I have to admit that I cannot answer this question.
During the last few days, several journalists have asked me about ayahuasca. Apparently, Harry Windsor said in an interview that it changed his life! However, the family of a young woman who took her own life after using ayahuasca has joined campaigners condemning his comments. Others – including myself – claim that Harry is sending a worrying message talking about his ‘positive’ experience with ayahuasca, saying it ‘brought me a sense of relaxation, release, comfort, a lightness that I managed to hold on to for a period of time’.
So, what is ayahuasca?
This paper explains it quite well:
Ayahuasca is a hallucinogen brew traditionally used for ritual and therapeutic purposes in Northwestern Amazon. It is rich in the tryptamine hallucinogens dimethyltryptamine (DMT), which acts as a serotonin 5-HT2A agonist. This mechanism of action is similar to other compounds such as lysergic acid diethylamide (LSD) and psilocybin. The controlled use of LSD and psilocybin in experimental settings is associated with a low incidence of psychotic episodes, and population studies corroborate these findings. Both the controlled use of DMT in experimental settings and the use of ayahuasca in experimental and ritual settings are not usually associated with psychotic episodes, but little is known regarding ayahuasca or DMT use outside these controlled contexts. Thus, we performed a systematic review of the published case reports describing psychotic episodes associated with ayahuasca and DMT intake. We found three case series and two case reports describing psychotic episodes associated with ayahuasca intake, and three case reports describing psychotic episodes associated with DMT. Several reports describe subjects with a personal and possibly a family history of psychosis (including schizophrenia, schizophreniform disorders, psychotic mania, psychotic depression), nonpsychotic mania, or concomitant use of other drugs. However, some cases also described psychotic episodes in subjects without these previous characteristics. Overall, the incidence of such episodes appears to be rare in both the ritual and the recreational/noncontrolled settings. Performance of a psychiatric screening before administration of these drugs, and other hallucinogens, in controlled settings seems to significantly reduce the possibility of adverse reactions with psychotic symptomatology. Individuals with a personal or family history of any psychotic illness or nonpsychotic mania should avoid hallucinogen intake.
In other words, ayahuasca can lead to serious side effects. They include vomiting, diarrhea, paranoia, and panic. Ayahuasca can also interact with many medications, including antidepressants, psychiatric medications, drugs used to control Parkinson’s disease, cough medicines, weight loss medications, and more. Those with a history of psychiatric disorders, such as schizophrenia, should avoid ayahuasca because this could worsen their psychiatric symptoms. Additionally, taking ayahuasca can increase your heart rate and blood pressure, which may result in dangerous consequences for those who have a heart condition.
Thus ayahuasca is an interesting albeit dangerous herb (in most countries it is illegal to possess or consume it). Currently, it is clearly under-researched, which means we know very little about its potential benefits and even less about the harm it can do.
Considering this, one would think that any half-intelligent person with loads of influence would not promote or encourage its use – but, sadly, it seems that one would be mistaken.
