Monthly Archives: April 2021
Thread embedding acupuncture therapy (TEAT) involves the insertion of thread at specific points on the body surface. The claim is that TEAT provides a sustained stimulation of acupoints and is therefore superior to needle acupuncture. Initially, TEAT was used in China to treat obesity, today it is employed to treat many conditions, including musculoskeletal conditions such as ankle sprain, shoulder pain, lumbar intervertebral disc herniation, and plantar fasciitis. Its effectiveness is, however, doubtful and so is its safety.
This review evaluated the safety of thread embedding acupuncture therapy (TEAT) and discuss the prevention and treatment of some adverse events (AEs).
Databases, including China National Knowledge Infrastructure (CNKI), CBMdisc, Wanfang, VIP databases and PubMed, MEDLINE, EMBASE, and Web of Science, were searched from their inception to January 2020. Included were randomized controlled trials (RCTs) and case reports in which AEs with TEAT were reported. Cochrane Collaboration’s tool and RevMan V.5.3.3 software were used to evaluate the quality of the studies.
A total of 61 articles (45 RCTs and 16 case reports) with a total of 620 cases of AEs were included in this review. These studies were published in two countries: China and South Korea. Twenty-eight kinds of AEs were noted. The most common AEs were induration, bleeding and ecchymosis, redness and swelling, fever, and pain. They accounted for 75.35% of all AEs. Most AEs were mild.; The rarest AEs were epilepsy, irregular menstruation, skin ulcer, thread malabsorption, and fat liquefaction, with 1 case each. Not all of them had a clear causal relationship with TEAT. Most of the AEs were local reactions and systemic reactions accounted for only 1.27%. Although the included studies showed that AEs were very commonly encountered (11.09%), only 5 cases of severe AEs reported from 2013 to 2017 (0.1%) by using catgut thread, which is rarely employed nowadays with new absorbable surgical suture being more popular. All of the patients with severe AEs were recovered after symptomatic treatment with no sequelae.
The authors concluded that the evidence showed that TEAT is a relatively safe and convenient therapy especially since application of new absorbable surgical suture. Improving practitioner skills, regulating operations, and paying attention to the patients’ conditions may reduce the incidence of AEs and improve safety of TEAT.
TEAT was initially used in China only but recently it has become popular elsewhere as well. Therefore the question about its risks has become relevant. The present paper is interesting in that it demonstrates that AEs do occur with some regularity. The authors’ conclusion that TEAT is “relatively safe” is, however, not justified because:
- the total sample size was not large enough for a generalizable conclusion;
- only RCTs and case reports were included, whereas case series and case-control studies (which would provide more relevant data) were excluded or might not even exist;
- RCTs of acupuncture often fail to mention or under-report AEs;
- acupuncture papers from China are notoriously unreliable.
So, all we can conclude from the evidence presented here is that AEs after TEAT do occur and do not seem to be all that rare. As the efficacy of TEAT has not been shown beyond doubt, this must inevitably lead to the conclusion that the risk-benefit balance of TEAT is not positive. In turn, that means that TEAT cannot be recommended as a treatment for any condition.
If I search on Amazon for books on ALTERNATIVE MEDICINE, I get between 50 000 and 60 000 volumes, depending on what country I am in. As a very rough guess, I estimate that about 95% of them are rubbish – not just useless, but dangerous. Because of this lamentable situation, I am delighted each time I come across one that belongs to the other 5%. And in recent years, there have been quite a few.
No, I am not about to advertise another book of mine; I am about to commend to you
Brad McKay’s FAKE MEDICINE
(I don’t often publish book reviews here, but I feel that might change.)
The new book is advertised with the following words: “Dr Brad McKay, Australian GP and science communicator, has seen the rise of misinformation permeate our lives and watched as many of us have turned away from health experts. Too often, we place our trust in online influencers, celebrities and Dr Google when it comes to making important health decisions. Fake Medicine explores the potential dangers of wellness warriors, anti-vaxxers, fad diets, dodgy supplements, alternative practitioners and conspiracy theories. This book is an essential tool for debunking pseudoscience and protecting you and your loved ones from the health scams that surround us. Protect your mind, body and wallet by fighting fake medicine.”
They describe the book fairly accurately. McKay covers all of these subjects with considerable skill. His book is well-suited for people who are newcomers to the critical assessment of so-called alternative medicine (SCAM); the text is free of jargon or long-winded technical explanations. Instead, the author mostly tells stories of events that actually happened to him. Several happened to him in a most personal fashion, as his experience as a young gay Australian with a form of conversion therapy administered by religious zealots, or the story where he took some highly dodgy Chinese medicine to boost his energy levels.
Lots of people have done similarly foolish things, I know, but not many are doctors and can thus put their experience in a medical perspective. And crucially, not many can write as entertaining as Brad. I had thought I knew most of what there is to know about SCAM, but I did learn something new from Brad: did you know what GISH GALLOP is? Well, I didn’t!
One of the most useful parts of the book is chapter 16 where Brad tells everyone what they can and should do to stop fake medicine in its tracks. And he does mean EVERYONE! – not just skeptics or sceptics or activists or scientists. This book is truly written for laypeople. If you don’t belong to this group, buy it anyway and give it to someone from your circle of friends who needs it. I am sure there are a few.
Many chiropractors seem to view the present pandemic as a business opportunity and make no end of false claims to attract customers. This has now been outlawed in the US. Medscape reported that a US district court will decide whether a chiropractor who is charged with 10 counts of making false marketing claims related to COVID-19 will be the first person convicted under a new federal law.
On his website, chiropractor ‘Dr.’ Eric Neptune advertises his services as follows:
Have you ever been told by your medical doctor that you or a member of your family had a specific disease, syndrome, or sickness? Did your doctor then recommend a drug or surgery to fix the issue, or tell you that you would have to live with it for the rest of your life? If so, you are not alone!
Nepute Wellness Center is unlike any medical clinic you may have been to. The clinic team is focused on finding and fixing the CAUSE of your problem vs. seeking out and treating only the SYMPTOMS. Nepute Wellness Center is equipped with state-of-the-art diagnostic equipment and testing, as well as medical doctors, nurses, and chiropractors who have been uniquely trained to treat your whole body, regardless of age, and return your body to a healthy balance so that it can heal itself the way God intended.
If you are tired of trying to treat your symptoms using prescription and over-the-counter pills, or even considering surgery, then Nepute Wellness Center may be right for you! Or like many, you want to be proactive with your health and prevent sickness and disease before you begin to suffer any symptoms, allowing you to live the full life you deserve, then make Nepute Wellness Center your partner in health!
Already over a year ago, Eric Nepute, the owner of Quickwork, based in St. Louis, Missouri, managed to make headlines. He had recorded a video that racked up more than 21 million views and suggested that drinking tonic water would prevent COVID-19 infections. Now, Mr. Neptune is the first person charged by the Federal Trade Commission (FTC) under the new COVID- 19 Consumer Protection Act. His company which has several locations in St. Louis County advertised its vitamin D and zinc products on social media and the internet as drugs that could treat or prevent COVID-19 claiming that their products are “more effective than the available COVID-19 vaccines”.
The FTC warned Nepute’s company in May 2020 about making unsubstantiated claims for other products regarding efficacy against COVID-19 and advised him to immediately stop making claims that were not supported by scientific evidence. However, Nepute seemed undeterred.
The FTC is seeking to fine Nepute and Quickwork up to US$43,792 for each violation of the COVID-19 Consumer Protection Act. In addition, the FTC seeks to bar the company from making health claims unless they are true and can be substantiated by scientific evidence.
Through his attorney, Neptune told the local NBC TV news affiliate, “I feel that I have not done anything wrong. I encourage everyone to live a healthy lifestyle during this unprecedented time. My attorneys are reviewing the complaint and I have no further comments at this time.”
Of all the many forms of so-called alternative medicine (SCAM), essential oils (EOs) are perhaps the most popular and least harmful – at least this is what we are supposed to believe. The truth is, as so often in SCAM, a little different.
Some EOs are claimed to have anticonvulsant activity and might benefit people with epilepsy. Lemongrass, lavender, clove, dill, and other EOs containing constituents such as asarone, carvone, citral, eugenol, or linalool are good candidates for evaluation as antiepileptic drugs. Conversely, other EOs are suspected to have pro-convulsant properties. These EOs are present in many balms and oils available freely over the counter. The effect of exposure to these EOs and occurrence of seizure has not been studied systematically. The aim of this study was therefore to evaluate the relationship between essential oils and the first episode of seizure and breakthrough seizures in known epileptic patients.
This multi-center prospective study was conducted in four hospitals in India over four years. Every person presenting with the first episode of seizure or breakthrough seizure was asked about exposure to EOs, mode of exposure, time to onset of a seizure in relation to exposure, duration of seizure, type of seizure, and antiepileptic drug therapy.
During the four-year period, there were 55 patients with essential oil-related seizures (EORS). 22 (40 %) had essential oil-induced seizures (EOIS) and 33 (60 %) had essential oil-provoked seizures (EOPS). The female: male ratio was 1:1.1, the age of the patients ranged from 8 months to 77 years. In the EOIS group, 95 % had generalized tonic-clonic seizures and 5% had focal impaired awareness seizures. In the EOPS group, 42.4 % had focal impaired awareness seizures, 27.3 % generalized tonic-clonic seizures, 15 % focal to bilateral tonic-clonic seizures, and 15 % focal aware motor seizures. EOs implicated were preparations containing eucalyptus and camphor.
The authors concluded that exposure to essential oils of eucalyptus and camphor is an under-recognized cause of the first and breakthrough seizure. Identifying the true causative factor will prevent unnecessary antiepileptic drug therapy and future recurrence.
These results are, of course, far from conclusive. However, they seem important enough to bear in mind and to stimulate further research. Meanwhile, patients with epilepsy might be well advised to be cautious with essential oils, particularly those from eucalyptus and camphor.
In 2008, the British Chiropractic Association sued Simon Singh because he disclosed that they were promoting chiropractic for infant colic. The BCA lost the case, plenty of money, and all its reputation. Ever since the issue is a very sore point for chiropractic pride. The data show that Simon was quite correct in stating that they are happily promoting bogus treatments without a jot of evidence. Here for instance is my systematic review:
Some chiropractors claim that spinal manipulation is an effective treatment for infant colic. This systematic review was aimed at evaluating the evidence for this claim. Four databases were searched and three randomised clinical trials met all the inclusion criteria. The totality of this evidence fails to demonstrate the effectiveness of this treatment. It is concluded that the above claim is not based on convincing data from rigorous clinical trials.
But chiropractors steadfastly refuse to accept defeat and keep on trying to find positive results. Now Danish chiropractors have made another attempt.
The purpose of this study is to evaluate the effect of chiropractic care on infantile colic. This multicenter, single-blind randomized controlled trial was conducted in four Danish chiropractic clinics, 2015–2019. Information was distributed in the maternity wards and by maternal and child health nurses. Children aged 2–14 weeks with unexplained excessive crying were recruited through home visits and randomized (1:1) to either chiropractic care or control group. Both groups attended the chiropractic clinic twice a week for 2 weeks. The intervention group received chiropractic care, while the control group was not treated. The parents were not present in the treatment room and unaware of their child’s allocation.
The primary outcome was change in daily hours of crying before and after treatment. Secondary outcomes were changes in hours of sleep, hours being awake and content, gastrointestinal symptoms, colic status and satisfaction. All outcomes were based on parental diaries and a final questionnaire.
Of 200 recruited children, 185 completed the trial (treatment group n = 96; control group n = 89). Duration of crying in the treatment group was reduced by 1.5 h compared with 1 h in the control group (mean difference − 0.6, 95% CI − 1.1 to − 0.1; P = 0.026), but when adjusted for baseline hours of crying, age, and chiropractic clinic, the difference was not significant (P = 0.066). The proportion obtaining a clinically important reduction of 1 h of crying was 63% in the treatment group and 47% in the control group (p = 0.037), and NNT was 6.5. We found no effect on any of the secondary outcomes.

The authors concluded that excessive crying was reduced by half an hour in favor of the group receiving chiropractic care compared with the control group, but not at a statistically significant level after adjustments. From a clinical perspective, the mean difference between the groups was small, but there were large individual differences, which emphasizes the need to investigate if subgroups of children, e.g. those with musculoskeletal problems, benefit more than others from chiropractic care.
This seems to be a rigorous trial. However, I don’t quite understand why the authors even mention that, before adjusting, the results seemed to favor chiropractic. This only makes a squarely negative study look positive! Why would anyone want to do that? Could this perhaps hint at a reason for this odd behavior? “The study was primarily funded by the Foundation for Chiropractic Research and Postgraduate Education.”
On 17/2/2020 I posted this article:
The drop in cases and deaths due to COVID-19 infections in India has been attributed to India’s national policy of using homeopathy. Early in the epidemic, the national “Ministry of AYUSH, recommended the use of Arsenic album 30 as preventive medicine against COVID-19. Its prophylactic use has been advised in states like Karnataka, Tamil Nadu, Kerala, and Maharashtra. The ‘OFFICIAL HOMEOPATHY RESOURCE’ is now claiming that homeopathy is the cause of the observed outcome…
If you click on the link, you will find that the OFFICIAL HOMEOPATHY RESOURCE has now removed the original. No problem! Thanks to Alan Henness, we can still access it; he announced in a tweet that he has archived a copy. So, here is the full article again:
India’s National Policy of Using Homeopathic Medicine To Prevent COVID is Dramatically Working
A dramatic plunge in cases and deaths of COVID in India can be attributed to India’s national policy of using homeopathy.
Early in the epidemic, the national “Ministry of AYUSH, (medical alternatives), in its guidelines, issued an advisory to states across India recommending the use of a traditional homeopathic drug, Arsenic album 30 as a form of preventive medicine against COVID-19. Its prophylactic use has been advised in states like Karnataka, Tamil Nadu, Kerala and Maharashtra and in some places, it has been used in high-risk areas. In places like Bhopal, claims were raised when doctors said that mild COVID cases were successfully treated with homeopathy.” [Times of India]
And now the results of that policy and use are clear, even though scientists in the conventional paradigm are mystified as to why the drop is so dramatic. They know nothing about homeopathy and its history of successfully treating epidemics.
India has a population of 1 billion, 300 million people. Relative to this massive population the number of cases per day and especially the number of deaths per day are now exceptionally low. According to the Daily Mail:
“Scientists are trying to work out why coronavirus cases in India are falling when at one point it looked like the country might overtake the US as the worst-hit nation.
In September the country was reporting some 100,00 new cases per day, but that went into decline in October and is now sitting at around 10,000 per day – leaving experts struggling to explain why.”


But why?
Why did the original disappear?
The reason seems obvious:
Saturday’s official toll recorded another 2,600 deaths and 340,000 new infections in India, bringing the total number of cases to 16.5 million, second only to the US. There have been 190,000 deaths attributed to Covid in India since the start of the pandemic. These figures are dramatic but most likely they are gross underestimates of the truth.
The egg on the face of homeopathy gets bigger if we consider things like the COVID-19 advice from ‘HOMEOPATHY INTERNATIONAL’, or the fact that UK’s biggest provider of homeopathy training encouraged the use of homeopathic potions made with phlegm to protect against and treat Covid-19. The egg finally turns into a veritable omelette, once we learn that the leading academic journal in homeopathy, HOMEOPATHY, promoted the idea that homeopathic have a place in the fight against the pandemic – not just once but repeatedly – and that the leading UK homeopath, Elizabeth Thompson, recommended homeopathy for COVID-19 infections after herself falling ill with the virus.
No, I do not feel the slightest tinge of Schadenfreude, about all this. I am writing about it because I still hope that it will prevent some people from risking their health with useless therapies and perhaps even stop some charlatans to make ridiculously irresponsible claims about them. So, please do me a favor and heed my message:
The promotion of homeopathy and other ineffective therapies costs many lives!
French researchers aimed to assess the efficacy of osteopathic manipulation for fibromyalgia (FM) in a randomized clinical trial. Patients were randomized to osteopathic or sham treatment. Treatment was administered by experienced physical medicine physicians, and consisted of six sessions per patient, over 6weeks. Treatment credibility and expectancy were repeatedly evaluated.
For the osteopathic treatment, the patient was first placed in a prone position. Each vertebra from C7 to L5 was mobilized in a dorsoventral direction by progressive pressure on the spinous process (SP), and in rotation by applying pressure on the lateral surface of the SP (bilaterally). The sacral bone was repeatedly mobilized in nutation–counternutation (5–10 times). The piriformis muscles were progressively stretched. The hip joint was then progressively mobilized in extension combined with abduction and adduction to stretch the adductor, abductor, and flexor muscles (10 times). The shoulders were progressively mobilized, one by one, with a repeated circumduction movement of the glenohumeral joint (10 times). The patient was then placed in a supine position, for the following maneuvers. At the neck, bimanual traction was performed, followed by repeated mobilization in lateral flexion and in rotation (both sides, five times, 3–5 times each). At the shoulders, we first performed cranial traction of both arms and then repeated caudal traction of one arm and then the other, by blocking the clavicle, thereby opening the acromioclavicular and glenohumeral joints (three times). At the hips, repeated tractions were performed on the legs (three times) and the hip joint was mobilized by circumduction movements. Finally, the patient was placed in the lateral decubitus position for mobilization of the lumbar and thoracolumbar spine. Thrust manipulations were allowed at any level, according to the patient’s complaint.
The sham treatment followed the same order, but the maneuvers were stopped halfway through to prevent joint mobilization at the spine. At the hips and shoulders, the stretching techniques were also stopped halfway. The joint techniques were simulated, with no significant mobilization. Thrust manipulation was forbidden.
Patients completed standardized questionnaires at baseline, during treatment, and at 6, 12, 24, and 52 weeks after randomization. The primary outcome was pain intensity (100-mm visual analog scale) during the treatment period. Secondary outcomes included fatigue, functioning, and health-related quality of life. Primarily intention-to-treat analyses were adjusted for credibility, using multiple imputations for missing data.
In total, 101 patients (94% women) were included. Osteopathic treatment did not significantly decrease pain relative to sham treatment (mean difference during treatment: −2.2mm; 95% confidence interval, −9.1 to 4.6mm). No significant differences were observed for secondary outcomes. No serious adverse events were observed, despite a likely rebound in pain and altered functioning at week 12 in patients treated by osteopathy. Patient expectancy
was predictive of pain during treatment, with a decrease of 12.9mm (4.4–21.5mm) per 10 points on the 0–30 scale. Treatment credibility and expectancy were also predictive of several secondary outcomes.
The authors concluded that osteopathy conferred no benefit over sham treatment for pain, fatigue, functioning, and quality of life in patients with FM. These findings do not support the use of osteopathy to treat these patients. More attention should be paid to the expectancy of patients in FM management.
The French team should be congratulated on this excellent piece of research. This is a very well conducted and reported study. It should serve as a blueprint to researchers of manual therapies for future trials. The results are clear and not unexpected: osteopathy is little more than a theatrical placebo.
Indian homeopaths aimed at evaluating the efficacy of individualized homeopathy (IH) for atopic dermatitis (AD). They conducted a double-blind, randomized, placebo-controlled, short-term, preliminary trial in an Indian homeopathy hospital. Patients were randomized to either IH (n = 30) or identical-looking placebo (n = 30) using computerized randomization and allocation. Outcomes were patient-oriented scoring of AD (PO-SCORAD; primary endpoint), Dermatological Life Quality Index (DLQI) score, and AD burden score for adults (ADBSA; secondary endpoints), measured monthly for 3 months. An intention-to-treat sample was analyzed after adjusting baseline differences.
On PO-SCORAD, improvement was higher in IH against placebo, but nonsignificant statistically (pmonth 1 = 0.433, pmonth 2 = 0.442, pmonth 3 = 0.229). Secondary outcomes were also nonsignificant – both DLQI and ADBSA (p > 0.05). Four adverse events (diarrhea, injury, common cold) were recorded.
The authors concluded that there was a small, but nonsignificant direction of effect towards homeopathy, which renders the trial inconclusive. A properly powered robust trial is indicated.
Thee questions:
- Why use statistics only to ignore its results?
- Why discredit research into so-called alternative medicine (SCAM) in this way?
- Who on earth would publish such misleading conclusions?
This article was published in Complementary Medicine Research which claims to be an international peer-reviewed journal that aims to bridge the gap between conventional and complementary/alternative medicine on a sound scientific basis, promoting their mutual integration. It boasts that “experts of both conventional medicine and complementary/alternative medicine cooperate on the journal’s editorial board, ensuring a high standard of scientific quality”. Its editor is Harald Walach who we have met several times before.
I had a look at the long list of members of the editorial board and was unable to see many ‘experts in conventional medicine’. If that is so, the journal’s peer review process is bound to turn into a farcical procedure where any rubbish will pass.
The journal reminds authors that “published research must comply with internationally-accepted standards for research practice and reporting.” I believe that the internationally accepted standards of research reporting include something about not misleading the public by claiming that the absence of an effect is a small effect in favor of homeopathy. By revealing that there was no significant effect, the authors of this study demonstrate that IH was not effective as a treatment of AD. It is in my mind unethical to try to disguise this result by making it look like a small positive effect or claiming the result was inconclusive.
High standard of scientific quality?
No, quite the opposite!
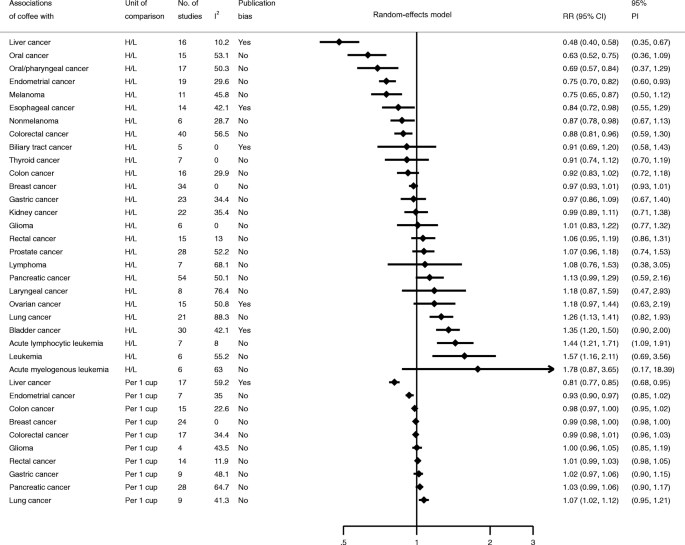
Epidemiological studies on the association between coffee intake, arguably a herbal remedy, and cancer risk have yielded inconsistent results. To summarize and appraise the quality of the current evidence, researchers conducted an umbrella review of existing findings from meta-analyses of observational studies.
They searched PubMed, Embase, Web of Science and the Cochrane database to obtain systematic reviews and meta-analyses of associations between coffee intake and cancer incidence. For each association, they estimated the summary effect size using the fixed- and random-effects model, the 95% confidence interval, and the 95% prediction interval. We also assessed heterogeneity, evidence of small-study effects, and excess significance bias.
Twenty-eight individual meta-analyses including 36 summary associations for 26 cancer sites were retrieved for this umbrella review. A total of 17 meta-analyses were significant at P ≤ 0.05 in the random-effects model. For the highest versus lowest categories, 4 of 26 associations had a more stringent P value (P ≤ 10− 6). Associations for five cancers were significant in dose-response analyses. Most studies (69%) showed low heterogeneity (I2 ≤ 50%). Three and six associations had evidence of excessive significance bias and publication bias, respectively. Coffee intake was inversely related to the risk of liver cancer and endometrial cancer and was characterized by dose-response relationships. There were no substantial changes when the researchers restricted analyses to a meta-analysis of cohort studies.
The authors concluded that there is highly suggestive evidence for an inverse association between coffee intake and risk of liver and endometrial cancer. Further research is needed to provide more robust evidence for cancer at other sites.
This is an interesting analysis that begs many questions. Let me just make four brief points:
- Correlation is not causation! Epidemiological studies throw up all sorts of associations that are too often mistaken as causal relationships. The question of whether coffee causes a decrease in the risk of certain cancers is as yet unanswered. The authors mention dose relationships which would, of course, increase the likelihood of a causal effect. Yet, they do not prove it.
- Another argument that would strengthen the possibility of a causal effect would be a plausible mechanism of action. However, the biological mechanism of how coffee might affect the risk remains unclear. Coffee contains a range of biologically active chemicals, including caffeine and phenolic compounds. In so-called alternative medicine (SCAM), coffee is also claimed to be a ‘detox‘ remedy. Yet it is unclear how exactly they might reduce the risk.
- The studies were all about the oral consumption of coffee. None considered anal application, like in Gerson therapy.
- The only way to find out whether coffee does, in fact, reduce the risk of certain cancers is to conduct prospective controlled clinical trials. Such studies are, however, not easy to conduct, particularly if designed such that their findings are truly reliable.
So, the answer to the question DOES COFFEE CONSUMPTION PREVENT CANCER? will remain unanswered for some time, I am afraid. Meanwhile, I suggest we enjoy our coffee per oral (and avoid it per anal).
Some time ago, I published ‘The 10 commandments of quackery’. Since then, I discovered that there are several errors that occur with such regularity in the comment section of this blog as well as in most other discussions about so-called alternative medicine (SCAM), that – in the hope to improve the logical reasoning of my readers (and often times my own) – it seems timely to publish the
10 ‘commandments’ of rational thought
- Thou shalt not confuse popularity of a therapy with its efficacy or safety (appeal to popularity).
- Thou shalt not assume that the test of time is a valid substitute for evidence (appeal to tradition).
- Thou shalt not believe that natural therapies are necessarily harmless (appeal to nature).
- Thou shalt not think that those who question your claim need to prove that you are wrong (reversal of the burden of proof).
- Thou shalt not assume that a therapy administered before a symptomatic improvement was necessarily the cause of that outcome (post hoc ergo propter hoc).
- Thou shalt not suppose that, because you do not know or understand an issue, it cannot be true (appeal to ignorance).
- Thou shalt not misrepresent your opponent’s position in order to make it easier for you to defeat it (straw man fallacy).
- Thou shalt not argue that, because others do wrong, you are permitted to do the same (tu quoque fallacy).
- Thou shalt not assume that your argument is correct because some authority agrees with you (appeal to authority).
- Thou shalt not attack your opponents instead of their arguments (ad hominem).
Yes, I know, one could add a lot more. But these 10 ‘commandments’ relate to the errors in rational thought that I feel would, if taken on board, be most useful in our discussions about SCAM.