nurses
Of all the many forms of so-called alternative medicine (SCAM), Reiki is perhaps the one that has the least plausibility. It assumes that a Reiki healer can send healing energy into the body of a patient which, in turn, stimulates the self-healing ability of the body and thus cures illness. Neither the source of the energy, its nature, or its effects have ever been convincingly demonstrated. These facts, however, do not stop enthusiasts to conduct clinical trials of Reiki.
The aim of this randomised clinical trial was to investigate the effect of the application of Reiki on fatigue and sleep quality in people with MS. A total of 60 people (control group = 30, intervention group = 30) participated in this study. Personal Information Form, Piper Fatigue Scale (PFS) and Pittsburg Sleep Quality Index (PSQI) were used as endpoints.
It was found that the PFS and PSQI total and subcomponent scores of the intervention group decreased after Reiki compared to the control group and this was statistically significant (p<0.05). The study showed that Reiki was significantly effective in improving fatigue and sleep quality in people with MS.
The authors concluded that, as Reiki is a simple, inexpensive and accessible method, it was suggested that its use in the management of MS should be encouraged and maintained in nursing practice.
In the introduction, the authors state this:
Reiki is a non-invasive, low-cost, easy-to-apply practice with no side effects and no negative effects on the existing treatment, and prevents acute and chronic conditions. It is frequently preferred in rehabilitation centres, emergency care units, nursing homes, elderly care centres, paediatrics, psychiatry, obstetrics and gynaecology clinics. Reiki can be applied by trained practitioners such as health professionals who have received first level reiki training in hospitals and clinics, caregivers or patients themselves. Reiki can be administered from with the patient or remotely when the patient and practitioner are in separate locations. Both types of Reiki are based on the premise of a universal source of healing energy that the Reiki practitioner can channel through intention.
For me, this begs the questions:
- If all of this were true, why do we need a study?
- If anyone believes such BS, are they the ideal people to conduct a study of Reiki?
Anyway, we should ask why this study generated a positive result. The most plausible explanation is that, as the study was not blind, the Reiki healers managed to maximise patient expectation. This, in turn, has generated a placebo respose which affected the subjective outcome measures. In other words, Reiki has no specific effect but patients tend to improve because of non-specific effects.
This review aimed to assess the therapeutic efficacy of Reiki therapy in alleviating anxiety.
In adherence to academic standards, a thorough search was conducted across esteemed databases such as PubMed, Web of Science, Science Direct, and the Cochrane Library. The primary objective of this search was to pinpoint peer-reviewed articles published in English that satisfied specific criteria: (1) employing an experimental or quasi-experimental study design, (2) incorporating Reiki therapy as the independent variable, (3) encompassing diverse patient populations along with healthy individuals, and (4) assessing anxiety as the measured outcome.
The study involved 824 participants, all of whom were aged 18 years or older. Reiki therapy was found to have a significant effect on anxiety intervention(SMD=-0.82, 95CI -1.29∼-0.36, P = 0.001). Subgroup analysis indicated that the types of subjects (chronically ill individuals and the general adult population) and the dosage/frequency of the intervention (≤ 3 sessions and 6–8 sessions) were significant factors influencing the variability in anxiety reduction.
The authors concluded that short-term Reiki therapy interventions of ≤ 3 sessions and 6–8 sessions have demonstrated effectiveness in reducing health and procedural anxiety in patients with chronic conditions such as gastrointestinal endoscopy inflammation, fibromyalgia, and depression, as well as in the general population. It is important to note that the efficacy of Reiki therapy in decreasing preoperative anxiety and death-related anxiety in preoperative patients and cancer patients is somewhat less consistent. These discrepancies may be attributed to individual pathophysiological states, psychological conditions, and treatment expectations.
_______________________
This is a truly stunning finding considering that few treatments are less plausible that Reiki. I strongly suspect that these conclusions are not tenable. To see whether this is true, we must look at the primary studies (tedious, I know, but can’t be helped). Here are the abstracts of the 13 studies included in this review:
Purpose: The purpose of the study was to investigate changes in the anxiety levels of patients receiving preoperative Reiki.
Material and methods: This study used a quasi-experimental model with a pretest-posttest control group.
Methods: Subjects (n = 210) were recruited from a hospital in Turkey, from June 2013 to July 2014. Subjects were then assigned to experimental (n = 105) and control (n = 105) groups.
Results: The level of anxiety of experimental group patients did not change according to their state anxiety scores (p > 0.10); however, the anxiety level of control group patients increased (p < 0.001).
Conclusion: The results of this study imply that the administration of Reiki is effective in controlling preoperative anxiety levels and in preventing them from increasing.
I am not sure what is meant by “a quasi-experimental model with pretest- posttest control group”. Yet, I suspect this was not a properly randomised trial and should thus have been exclused from the review. There was no control of placebo effects.
Fatigue is an extremely common side effect experienced during cancer treatment and recovery. Limited research has investigated strategies stemming from complementary and alternative medicine to reduce cancer-related fatigue. This research examined the effects of Reiki, a type of energy touch therapy, on fatigue, pain, anxiety, and overall quality of life. This study was a counterbalanced crossover trial of 2 conditions: (1) in the Reiki condition, participants received Reiki for 5 consecutive daily sessions, followed by a 1-week washout monitoring period of no treatments, then 2 additional Reiki sessions, and finally 2 weeks of no treatments, and (2) in the rest condition, participants rested for approximately 1 hour each day for 5 consecutive days, followed by a 1-week washout monitoring period of no scheduled resting and an additional week of no treatments. In both conditions, participants completed questionnaires investigating cancer-related fatigue (Functional Assessment of Cancer Therapy Fatigue subscale [FACT-F]) and overall quality of life (Functional Assessment of Cancer Therapy, General Version [FACT-G]) before and after all Reiki or resting sessions. They also completed a visual analog scale (Edmonton Symptom Assessment System [ESAS]) assessing daily tiredness, pain, and anxiety before and after each session of Reiki or rest. Sixteen patients (13 women) participated in the trial: 8 were randomized to each order of conditions (Reiki then rest; rest then Reiki). They were screened for fatigue on the ESAS tiredness item, and those scoring greater than 3 on the 0 to 10 scale were eligible for the study. They were diagnosed with a variety of cancers, most commonly colorectal (62.5%) cancer, and had a median age of 59 years. Fatigue on the FACT-F decreased within the Reiki condition (P=.05) over the course of all 7 treatments. In addition, participants in the Reiki condition experienced significant improvements in quality of life (FACT-G) compared to those in the resting condition (P <.05). On daily assessments (ESAS) in the Reiki condition, presession 1 versus postsession 5 scores indicated significant decreases in tiredness (P <.001), pain (P <.005), and anxiety (P<.01), which were not seen in the resting condition. Future research should further investigate the impact of Reiki using more highly controlled designs that include a sham Reiki condition and larger sample sizes.
This was a pilot study which should not report efficacy outcomes merely test the feasibility of a definitive trial. There was no control of placebo effects.
Purpose: This study’s aim is to determine the effect of Reiki when applied before upper gastrointestinal endoscopy on levels of anxiety, stress, and comfort.
Design: This single-blind, a pretest and post-test design, randomized, sham-controlled study was held between February and July 2021.
Methods: Patients who met the inclusion criteria were separated by randomization into three groups: Reiki, sham Reiki, and control. A total of 159 patients participated in the study. In the intervention groups (Reiki and sham Reiki), Reiki and sham Reiki were applied once for approximately 20 to 25 minutes before gastrointestinal endoscopy.
Findings: When the Reiki group was compared to the sham Reiki and control groups following the intervention, the decrease in the levels of patient stress (P < .001) and anxiety (P < .001) and the increase in patient comfort (P < .001) were found to be statistically significant.
Conclusions: Reiki applied to patients before upper gastrointestinal endoscopy was effective in reducing stress and anxiety and in increasing comfort.
Here an attempt was made to control for placebo effects and to blind patients. Whether the latter was successful was not tested. Thus a placebo effects cannot be excluded.
The purpose of this study was to evaluate the effect of Reiki as an alternative and complementary approach to treating community-dwelling older adults who experience pain, depression, and/or anxiety. Participants (N = 20) were randomly assigned to either an experimental or wait list control group. The pre- and posttest measures included the Hamilton Anxiety Scale, Geriatric Depression Scale-Short Form, Faces Pain Scale, and heart rate and blood pressure. The research design included an experimental component to examine changes in these measures and a descriptive component (semi-structured interview) to elicit information about the experience of having Reiki treatments. Significant differences were observed between the experimental and treatment groups on measures of pain, depression, and anxiety; no changes in heart rate and blood pressure were noted. Content analysis of treatment notes and interviews revealed five broad categories of responses: Relaxation; Improved Physical Symptoms, Mood, and Well-Being; Curiosity and a Desire to Learn More; Enhanced Self-Care; and Sensory and Cognitive Responses to Reiki.
No attempt to control for placebo effects.
Purpose: The purpose of this randomized pilot was to determine feasibility of testing Reiki, a complementary therapy intervention, for women undergoing breast biopsy (BB).
Background: Increasingly women face the possibility of BB, the definitive test for breast cancer. Psychological distress associated with BB includes anxiety and depression. Reiki was proposed as an intervention to decrease anxiety and promote relaxation.
Method: Thirty-two women scheduled for BB were randomized to Reiki intervention versus conventional care control. Anxiety and depression were evaluated using self-report questionnaires.
Findings: Analysis found no significant mean differences between groups over time. Comparably low baseline anxiety levels (possible selection bias) decreased naturally with time allowing little room for observing treatment effect.
Conclusions: Reiki, when administered in the naturalistic setting of a complementary therapy office, did not suggest evidence of efficacy. An intervention offered within the bounds of the conventional care setting may be more feasible for addressing BB distress.
The study failed to produce a positive finding.
The aim of this study was to investigate the effect of Reiki on pain, anxiety, and hemodynamic parameters on postoperative days 1 and 2 in patients who had undergone cesarean delivery. The design of this study was a randomized, controlled clinical trial. The study took place between February and July 2011 in the Obstetrical Unit at Odemis Public Hospital in Izmir, Turkey. Ninety patients equalized by age and number of births were randomly assigned to either a Reiki group or a control group (a rest without treatment). Treatment applied to both groups in the first 24 and 48 hours after delivery for a total of 30 minutes to 10 identified regions of the body for 3 minutes each. Reiki was applied for 2 days once a day (in the first 24 and 48 hours) within 4-8 hours of the administration of standard analgesic, which was administered intravenously by a nurse. A visual analog scale and the State Anxiety Inventory were used to measure pain and anxiety. Hemodynamic parameters, including blood pressure (systolic and diastolic), pulse and breathing rates, and analgesic requirements also were recorded. Statistically significant differences in pain intensity (p = .000), anxiety value (p = .000), and breathing rate (p = .000) measured over time were found between the two groups. There was a statistically significant difference between the two groups in the time (p = .000) and number (p = .000) of analgesics needed after Reiki application and a rest without treatment. Results showed that Reiki application reduced the intensity of pain, the value of anxiety, and the breathing rate, as well as the need for and number of analgesics. However, it did not affect blood pressure or pulse rate. Reiki application as a nursing intervention is recommended as a pain and anxiety-relieving method in women after cesarean delivery.
No control for placebo effects.
Objective: to evaluate the effectiveness of massage and reiki in the reduction of stress and anxiety in clients at the Institute for Integrated and Oriental Therapy in Sao Paulo (Brazil).
Method: clinical tests randomly done in parallel with an initial sample of 122 people divided into three groups: Massage + Rest (G1), Massage + Reiki (G2) and a Control group without intervention (G3). The Stress Systems list and the Trace State Anxiety Inventory were used to evaluate the groups at the start and after 8 sessions (1 month), during 2015.
Results: there were statistical differences (p = 0.000) according to the ANOVA (Analysis of Variance) for the stress amongst the groups 2 and 3 (p = 0.014) with a 33% reductions and a Cohen of 0.78. In relation to anxiety-state, there was a reduction in the intervention groups compared with the control group (p < 0.01) with a 21% reduction in group 2 (Cohen of 1.18) and a 16% reduction for group 1 (Cohen of 1.14).
Conclusion: Massage + Reiki produced better results amongst the groups and the conclusion is for further studies to be done with the use of a placebo group to evaluate the impact of the technique separate from other techniques.
No control for placebo effects.
This randomized controlled study aimed to determine the effect of Reiki and aromatherapy on vital signs, oxygen saturation, and anxiety level in patients undergoing upper gastrointestinal endoscopy. The sample consisted of 100 patients divided into Reiki (n = 34), aromatherapy (n = 33), and control (n = 33) groups. Data were collected 3 times (before, during, and after the procedure) using a descriptive characteristics questionnaire, a follow-up form, and the State Anxiety Subscale. The Reiki group had a mean State Anxiety Subscale score of 53.59 ± 2.98 and 43.94 ± 4.31 before and after the procedure, respectively. The aromatherapy group had a mean State Anxiety Subscale score of 54.03 ± 4.03 and 43.85 ± 3.91 before and after the procedure, respectively. The control group had a mean State Anxiety Subscale score of 38.79 ± 4.68 and 53.30 ± 7.26 before and after the procedure, respectively (P < .05). The results showed that the Reiki and aromatherapy groups had significantly lower State Anxiety Subscale scores than the control group after the procedure, indicating that Reiki and aromatherapy help reduce anxiety levels. There was a significant difference in the mean respiratory rates and oxygen saturation levels between the groups (P < .05). In conclusion, patients who do Reiki or undergo aromatherapy are less likely to experience anxiety before upper gastrointestinal endoscopy.
No control for placebo effects.
The aim of this study is to investigate the effects of Reiki application on pain, anxiety, and quality of life in patients with fibromyalgia. The study was completed with a total of 50 patients: 25 in the experimental group and 25 in the control group. Reiki was applied to the experimental group and sham Reiki to the control group once a week for 4 weeks. Data were collected from the participants using the Information Form, Visual Analog Scale, McGill-Melzack Pain Questionnaire, State-Trait Anxiety Inventory, and Short Form-36. There was a significant difference between the mean Visual Analog Scale pain scores during and before the first week (P = .012), second week (P = .002), and fourth week (P = .020) measurements of the individuals in the experimental and control groups, after application. In addition, at the end of the 4-week period, the State Anxiety Inventory (P = .005) and the Trait Anxiety Inventory (P = .003) were significantly decreased in the Reiki group compared with the control group. Physical function (P = .000), energy (P = .009), mental health (P = .018), and pain (P = .029) subdimension scores of quality of life in the Reiki group increased significantly compared with the control group. Reiki application to patients with fibromyalgia may have positive effects on reducing pain, improving quality of life, and reducing state and trait anxiety levels.
Here an attempt was made to control for placebo effects and to blind patients. Whether the latter was successful was not tested. Thus a placebo effects cannot be excluded. The sample size was small.
Background: Reiki is a biofield therapy which is based on the explanatory model that the fields of energy and information of living systems can be influenced to promote relaxation and stimulate a healing response.
Objective: To conduct a pragmatic within-subject pilot trial of a remote Reiki program for frontline healthcare workers’ health-related symptoms during the COVID-19 pandemic.
Methods: Healthcare professionals in the UK (eg, physicians, nurses, and paramedics) were eligible to sign up for a distance Reiki program and were also invited to participate in the research study. Eight Reiki practitioners simultaneously gave each participant Reiki remotely for 20 minutes on 4 consecutive days. Feasibility of the research was assessed, including recruitment, data completeness, acceptability and intervention fidelity, and preliminary evaluation of changes in outcome measures. Participants’ stress, anxiety, pain, wellbeing, and sleep quality were evaluated with 7-point numerical rating scales. Measures were completed when signing up to receive Reiki (pre) and following the final Reiki session (post). Pre and post data were analyzed using Wilcoxon signed ranks tests.
Results: Seventy-nine healthcare professionals signed up to receive Reiki and took the baseline measures. Of those, 40 completed post-measures after the 4-day intervention and were therefore included in the pre-post analysis. Most participants were female (97.5%), and the mean age was 43.9 years old (standard deviations = 11.2). The study was feasible to conduct, with satisfactory recruitment, data completeness, acceptability, and fidelity. Wilcoxon signed ranks tests revealed statistically significant decreases in stress (M = -2.33; P < .001), anxiety (M = -2.79; P < .001) and pain (M = -.79; P < .001), and significant increases in wellbeing (M = -1.79; P < .001) and sleep quality (M = -1.33; P = .019).
Conclusions: The Reiki program was feasible and was associated with decreased stress, anxiety and pain, and increased wellbeing and sleep quality in frontline healthcare workers impacted by the COVID-19 pandemic.
Pilot study should not report efficacy findings and should be excluded.
Background: There is a scarcity of studies in the international literature regarding alternative treatment to the pharmacological and psychotherapeutic intervention in the face of depression symptoms. This study aimed to test a protocol based on natural therapy, alternatives to pharmacological and psychotherapeutic, through Mindfulness Meditation, Reiki, Acupuncture and Auriculotherapy, to treat the symptoms of depression for those who were with no pharmacological or psychotherapeutic treatment for these symptoms.
Methods: this is a randomized single-blind controlled pilot study. The final sample was 21 participants divided in two groups: experimental and control. Participants were evaluated by validated instruments during the screening process and after the intervention. The instruments were: Depression, Anxiety and Stress Scale and Beck Depression Inventory. Intervention was performed in eight sessions, during two months. All the techniques were used in the experimental group. Analysis of variance with repeated measures was used to compare pre-intervention to post-intervention moments.
Results: the result of analysis indicates a significant reduction in the symptoms of depression after the intervention among the experimental group.
Limitations: there is no way to determine which of the techniques used produced the most significant result.
Conclusions: The protocol proposed in this study was effective in reducing the symptoms of depression to whom are not eligible for traditional treatment.
This is a pilot study and should not report efficacy findings. It is also not a study of just Reiki. It should have been excluded.
This is a constructive replication of a previous trial conducted by Bowden et al. (2010), where students who had received Reiki demonstrated greater health and mood benefits than those who received no Reiki. The current study examined impact on anxiety/depression. 40 university students-half with high depression and/or anxiety and half with low depression and/or anxiety-were randomly assigned to receive Reiki or to a non-Reiki control group. Participants experienced six 30-minute sessions over a period of two to eight weeks, where they were blind to whether noncontact Reiki was administered as their attention was absorbed in a guided relaxation. The efficacy of the intervention was assessed pre-post intervention and at five-week follow-up by self-report measures of mood, illness symptoms, and sleep. The participants with high anxiety and/or depression who received Reiki showed a progressive improvement in overall mood, which was significantly better at five-week follow-up, while no change was seen in the controls. While the Reiki group did not demonstrate the comparatively greater reduction in symptoms of illness seen in our earlier study, the findings of both studies suggest that Reiki may benefit mood.
No control for placebo effects
This is a constructive replication of a previous trial conducted by Bowden et al. (2010), where students who had received Reiki demonstrated greater health and mood benefits than those who received no Reiki. The current study examined impact on anxiety/depression. 40 university students-half with high depression and/or anxiety and half with low depression and/or anxiety-were randomly assigned to receive Reiki or to a non-Reiki control group. Participants experienced six 30-minute sessions over a period of two to eight weeks, where they were blind to whether noncontact Reiki was administered as their attention was absorbed in a guided relaxation. The efficacy of the intervention was assessed pre-post intervention and at five-week follow-up by self-report measures of mood, illness symptoms, and sleep. The participants with high anxiety and/or depression who received Reiki showed a progressive improvement in overall mood, which was significantly better at five-week follow-up, while no change was seen in the controls. While the Reiki group did not demonstrate the comparatively greater reduction in symptoms of illness seen in our earlier study, the findings of both studies suggest that Reiki may benefit mood.
This is the only rigorous study included in the review. Its findings are not easy to interpret (“For the sample as a whole, as can be seen from the total group means, there was little change over the course of the study”)
__________________________
Even though I did not have access to the full text of all of these RCTs, this analysis tells me a few important things; here are some of the main points I discovered:
- the new review is fatally flawed;
- the authors’ statement that their “article presents a systematic review of randomized controlled trials (RCTs) that were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines” is nonsensical;
- PRISMA guidelines were certainly not adhered to;
- there is no truly critical assessment of the primary studies;
- the literature searches were incomplete;
- the risk of bias tool for evaluating the primary studies was employed incorrectly;
- the review did not include all RCTs of Reiki (our own 2008 review included several trials that are not included here, and this blog has a few more);
- the review includes several studies that should have been excluded;
- most Reiki studies are of poor quality;
- with both the review and most of the primary studies, one feels a strong bias towards trying to prove that Reiki works;
- Reiki research is firmly in the hands of nurses (almost all the studies were conducted by nurses);
- almost all of the RCTs test Reiki versus no treatment, and this means that most do not control for placebo (or other non-specific) effects. In other words, the conclusions stating that Reiki is effective are simply wrong.
I am dismayed to see that a decent journal (BMC Palliative Care) published such a fatally flawed review. The paper fails to discuss any of its obvious flaws. Specifically, it does not even specify what interventions were used in the various control groups. Do the journal editors, peer-reviewers and authors not appreciate that, without such information, the findings are uninterpretable? Or do they perhaps deliberately try to mislead us?
If you ask me, this paper should be best withdrawn.
Our own review of Reiki is no longer up-to-date. Yet, it’s conclusion is, in my view, far more accurate than the one offered by the authors of the fatally flawed new review:
the evidence is insufficient to suggest that reiki is an effective treatment for any condition. Therefore the value of reiki remains unproven.
- the intervention group participants received reiki remotely for 20 minutes for 4 consecutive days,
- the control group participants received no intervention.
A controlled clinical trial has the purpose of comparing outcomes of two or more treatments. Therefore, intra-group changes are utterly irrelevant. The only thing of interest is the comparison between the intervention and control groups. In the present study, this did not show a significant difference. In other words, distant Reiki had no effect.
This means that the bit in the conclusion telling us that Reiki helps students cope with test anxiety is quite simply not true.
This leaves us with the first part of the conclusion: Reiki is a safe and easy-to-practice method. This may well be true – yet it is meaningless. Apart from the fact that the study was not aimed at assessing safety or ease of practice, the statement is true for far too many things to be meaningful, e.g.:
- Not having Reiki (the control group) is a safe and easy-to-practice method.
- Going for a walk is a safe and easy-to-practice method.
- Cooking a plate of spagetti is a safe and easy-to-practice method.
- Having a nap is a safe and easy-to-practice method.
- Reading a book is a safe and easy-to-practice method.
(I think you get my gist)
To make the irony complete, let me tell you that this trial was published in Journal of Nursing Education. On the website, the journal states: The Journal of Nursing Education is a monthly, peer-reviewed journal publishing original articles and new ideas for nurse educators in various types and levels of nursing programs for over 60 years. The Journal enhances the teaching-learning process, promotes curriculum development, and stimulates creative innovation and research in nursing education.
I suggest that the journal urgently embarks on a program of educating its editors, reviewers, contributors and readers about science, pseudoscience, minimal standards, scientific rigor, and medical ethics.
Supportive care is often assumed to be beneficial in managing the anxiety symptoms common in patients in sterile hematology unit. The authors of this study hypothesize that personal massage can help the patient, particularly in this isolated setting where physical contact is extremely limited.
The main objective of this study therefore was to show that anxiety could be reduced after a touch-massage performed by a nurse trained in this therapy.
A single-center, randomized, unblinded controlled study in the sterile hematology unit of a French university hospital, validated by an ethics committee. The patients, aged between 18 and 65 years old, and suffering from a serious and progressive hematological pathology, were hospitalized in sterile hematology unit for a minimum of three weeks. They were randomized into either a group receiving 15-minute touch-massage sessions or a control group receiving an equivalent amount of quiet time once a week for three weeks.
In the treated group, anxiety was assessed before and after each touch-massage session, using the State-Trait Anxiety Inventory questionnaire with subscale state (STAI-State). In the control group, anxiety was assessed before and after a 15-minute quiet period. For each patient, the difference in the STAI-State score before and after each session (or period) was calculated, the primary endpoint was based on the average of these three differences. Each patient completed the Rosenberg Self-Esteem Questionnaire before the first session and after the last session.
Sixty-two patients were randomized. Touch-massage significantly decreased patient anxiety: a mean decrease in STAI-State scale score of 10.6 [7.65-13.54] was obtained for the massage group (p ≤ 0.001) compared with the control group. The improvement in self-esteem score was not significant.
The authors concluded that this study provides convincing evidence for integrating touch-massage in the treatment of patients in sterile hematology unit.
I find this conclusion almost touching (pun intended). The wishful thinking of the amateur researchers is almost palpable.
Yes, I mean AMATEUR, despite the fact that, embarrassingly, the authors are affiliated with prestigeous institutions:
- 1Nantes Université, CHU Nantes, Service Interdisciplinaire Douleur, Soins Palliatifs et de Support, Médecine intégrative, UIC 22, Nantes, F-44000, France.
- 2Université Paris Est, EA4391 Therapeutic and Nervous Excitability, Creteil, F-93000, France.
- 3Nantes Université, CHU Nantes, Hematology Department, Nantes, F-44000, France.
- 4Nantes Université, CHU Nantes, CRCI2NA – INSERM UMR1307, CNRS UMR 6075, Equipe 12, Nantes, F-44000, France.
- 5Institut Curie, Paris, France.
- 6Université Paris Versailles Saint-Quentin, Versailles, France.
- 7Nantes Université, CHU Nantes, Direction de la Recherche et l’Innovation, Coordination Générale des Soins, Nantes, F-44000, France.
- 8Methodology and Biostatistics Unit, DRCI CHU Nantes CHD Vendée, La Roche Sur Yon, F-85000, France.
- 9Nantes Université, CHU Nantes, Service Interdisciplinaire Douleur, Soins Palliatifs et de Support, Médecine intégrative, UIC 22, Nantes, F-44000, France. [email protected].
So, why do I feel that they must be amateurs?
- Because, if they were not amateurs, they would know that a clinical trial should not aim to show something, but to test something.
- Also, if they were not amateurs, they would know that perhaps the touch-massage itself had nothing to do with the outcome, but that the attention, sympathy and empathy of a therapist or a placebo effect can generate the observed effect.
- Lastly, if they were not amateurs, they would not speak of convincing evidence based on a single, small, and flawed study.
A ‘pragmatic, superiority, open-label, randomised controlled trial’ of sleep restriction therapy versus sleep hygiene has just been published in THE LANCET. Adults with insomnia disorder were recruited from 35 general practices across England and randomly assigned (1:1) using a web-based randomisation programme to either four sessions of nurse-delivered sleep restriction therapy plus a sleep hygiene booklet or a sleep hygiene booklet only. There was no restriction on usual care for either group. Outcomes were assessed at 3 months, 6 months, and 12 months. The primary endpoint was self-reported insomnia severity at 6 months measured with the insomnia severity index (ISI). The primary analysis included participants according to their allocated group and who contributed at least one outcome measurement. Cost-effectiveness was evaluated from the UK National Health Service and personal social services perspective and expressed in terms of incremental cost per quality-adjusted life year (QALY) gained. The trial was prospectively registered (ISRCTN42499563).
Between Aug 29, 2018, and March 23, 2020 the researchers randomly assigned 642 participants to sleep restriction therapy (n=321) or sleep hygiene (n=321). Mean age was 55·4 years (range 19–88), with 489 (76·2%) participants being female and 153 (23·8%) being male. 580 (90·3%) participants provided data for at least one outcome measurement. At 6 months, mean ISI score was 10·9 (SD 5·5) for sleep restriction therapy and 13·9 (5·2) for sleep hygiene (adjusted mean difference –3·05, 95% CI –3·83 to –2·28; p<0·0001; Cohen’s d –0·74), indicating that participants in the sleep restriction therapy group reported lower insomnia severity than the sleep hygiene group. The incremental cost per QALY gained was £2076, giving a 95·3% probability that treatment was cost-effective at a cost-effectiveness threshold of £20 000. Eight participants in each group had serious adverse events, none of which were judged to be related to intervention.
The authors concluded that brief nurse-delivered sleep restriction therapy in primary care reduces insomnia symptoms, is likely to be cost-effective, and has the potential to be widely implemented as a first-line treatment for insomnia disorder.
I am frankly amazed that this paper was published in a top journal, like THE LANCET. Let me explain why:
The verum treatment was delivered over four consecutive weeks, involving one brief session per week (two in-person sessions and two sessions over the phone). Session 1 introduced the rationale for sleep restriction therapy alongside a review of sleep diaries, helped participants to select bed and rise times, advised on management of daytime sleepiness (including implications for driving), and discussed barriers to and facilitators of implementation. Session 2, session 3, and session 4 involved reviewing progress, discussion of difficulties with implementation, and titration of the sleep schedule according to a sleep efficiency algorithm.
This means that the verum group received fairly extensive attention, while the control group did not. In other words, a host of non-specific effects are likely to have significantly influenced or even entirely determined the outcome. Despite this rather obvious limitation, the authors fail to discuss any of it. On the contrary, that claim that “we did a definitive test of whether brief sleep restriction therapy delivered in primary care is clinically effective and cost-effective.” This is, in my view, highly misleading and unworthy of THE LANCET. I suggest the conclusions of this trial should be re-formulated as follows:
The brief nurse-delivered sleep restriction, or the additional attention provided exclusively to the patients in the verum group, or a placebo-effect or some other non-specific effect reduced insomnia symptoms.
Alternatively, one could just conclude from this study that poor science can make it even into the best medical journals – a problem only too well known in the realm of so-called alternative medicine (SCAM).
“We are hugely concerned about the welfare of doctors and healthcare workers with long COVID”. These are the first words of a comprehensive survey of UK doctors with post-acute COVID health complications. It reveals that these doctors experience symptoms such as:
- fatigue,
- headaches,
- muscular pain,
- nerve damage,
- joint pain,
- respiratory problems.
Around 60% of doctors said that post-acute COVID ill health has affected their ability to carry out day-to-day activities on a regular basis. 18% reported that they were now unable to work due to their post-acute COVID ill-health, and only 31% said they were working full-time, compared with more than half before the onset of their illness.
The report demands financial support for doctors and healthcare staff with post-acute COVID, post-acute COVID to be recognized as an occupational disease in healthcare workers, with a definition that covers all of the debilitating disease’s symptoms and for improved access to physical and mental health services to aid comprehensive assessment, appropriate investigations and treatment. The report also calls for greater workplace protection for healthcare staff risking their lives for others and better support for post-acute COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
In November 2021, an online survey investigating the emotional states of depression, anxiety, stress, compassion satisfaction, and compassion fatigue was administered to 78 Italian healthcare workers (HCWs). Between 5 and 20% of the cohort showed the effects of the adverse psychological impact of the pandemic and more than half of them experienced medium levels of compassion fatigue as well as a medium level of compassion satisfaction. The results also show that those with fewer years of clinical practice might be at greater risk of burnout, anxiety, and stress symptoms and might develop a lower level of compassion satisfaction. Moreover, the factors that potentially contribute to poor mental health, compassion fatigue, and compassion satisfaction seem to differ between residents and specialist physicians.
A cross-sectional study was conducted from September 2021 to April 2022 and targeted all physicians working at King Fahd Hospital of the University, Al Khobar, Saudi Arabia. Patient Health Questionnaire-9 and General Anxiety Disorder-7 were used to elicit self-reported data regarding depression and anxiety, respectively. In addition, sociodemographic and job-related data were collected. A total of 438 physicians responded, of which 200 (45.7%) reported symptoms of depression and 190 (43.4%) of anxiety. Being aged 25-30 years, female, resident, and reporting a reduction in work quality were factors significantly associated with both anxiety and depression. Female gender (AOR = 3.570; 95% CI = 2.283-5.582; P < 0.001), working an average 9-11 hours/day (AOR = 2.130; 95% CI = 1.009-4.495; P < 0.047), and self-perceived reduction in work quality (AOR = 3.139; 95% CI = 2.047-4.813; P < 0.001) were significant independent predictors of anxiety. Female gender (AOR = 2.929; 95% CI = 1.845-4.649; P < 0.001) and self-perceived reduction in work quality (AOR = 3.141; 95% CI = 2.053-4.804; P < 0.001) were significant independent predictors of depression.
An observational, multicenter cross-sectional study was conducted at eight tertiary care centers in India. The consenting participants were HCWs between 12 and 52 weeks post-discharge after COVID-19 infection. The mean age of the 679 eligible participants was 31.49 ± 9.54 years. The overall prevalence of COVID sequelae was 30.34%, with fatigue (11.5%) being the most common followed by insomnia (8.5%), difficulty in breathing during activity (6%), and pain in joints (5%). The odds of having any sequelae were significantly higher among participants who had moderate to severe COVID-19 (OR 6.51; 95% CI 3.46-12.23) and lower among males (OR 0.55; 95% CI 0.39-0.76). Besides these, other predictors for having sequelae were age (≥45 years), presence of any comorbidity (especially hypertension and asthma), category of HCW (non-doctors vs doctors), and hospitalization due to COVID-19.
Such data are scary. Not only will we have a tsunami of long-Covid patients from the general public, and not only do we currently lack effective causal treatments for the condition, but also is the number of HCWs who are supposed to deal with all this drastically reduced.
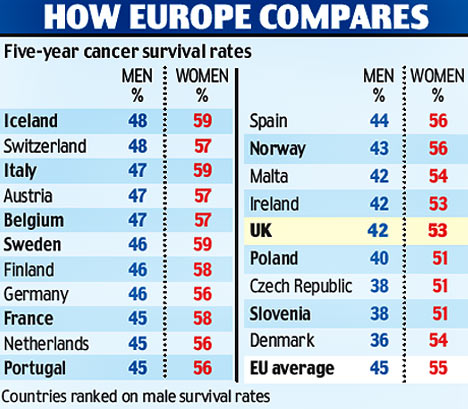
Most if not all countries are going to be affected by these issues. But the UK public might suffer the most, I fear. The reasons are obvious if you read a previous post of mine: in the UK, we have significantly fewer doctors, nurses, hospital beds, and funding (as well as politicians who care and would be able to do something about the problem) than in other comparable countries. To me, this looks like the emergence of a perfect storm.
Yesterday, the NHS turned 75, and virtually all the newspapers have joined in the chorus singing its praise.
RIGHTLY SO!
The idea of nationalized healthcare free for all at the point of delivery is undoubtedly a good one. I’d even say that, for a civilized country, it is an essential concept. The notion that an individual who had the misfortune to fall ill might have to ruin his/her livelihood to get treated is absurd and obscene to me.
The NHS was created the same year that I was born. Even though I did not grow up in the UK, I cannot imagine a healthcare system where people have to pay to get or stay healthy. To me, ‘free’ – it is, of course not free at all but merely free at the point of delivery – is a human right just as freedom of speech or the right to a good education.
 While reading some of what has been written about the NHS’s 75th birthday, I came across more platitudes than I care to remember. Yes, we are all ever so proud of the NHS but we would be even more proud if our NHS did work adequately. I find it somewhat hypocritical to sing the praise of a system that is clearly not functioning nearly as well as that of comparable European countries (where patients also don’t have to pay out of their own pocket for healthcare). I also find it sickening to listen to politicians paying lip service, while doing little to fundamentally change things. And I find it enraging to see how the conservatives have systematically under-funded the NHS, while pretending to support it adequately.
While reading some of what has been written about the NHS’s 75th birthday, I came across more platitudes than I care to remember. Yes, we are all ever so proud of the NHS but we would be even more proud if our NHS did work adequately. I find it somewhat hypocritical to sing the praise of a system that is clearly not functioning nearly as well as that of comparable European countries (where patients also don’t have to pay out of their own pocket for healthcare). I also find it sickening to listen to politicians paying lip service, while doing little to fundamentally change things. And I find it enraging to see how the conservatives have systematically under-funded the NHS, while pretending to support it adequately.
How can we be truly proud of the NHS when it seems to be dying a slow and agonizing death due to political neglect? In the UK, politicians like to be ‘world beating’ with everything, and I am sure some Tories want you to believe that, under their leadership, a world-beating healthcare system has been established in the UK.
Let me tell you: it’s not true. I have personal experience with the healthcare systems of 5 different nations and worked as a doctor in 3 of them. In Austria, France, and Germany for instance, the system is significantly better and no patient’s finances are ruined through illness.
Now there is talk about reform – yet again! Let us please not look towards the US when thinking of reforming the NHS. I have lived for a while in America and can tell you one thing: when it comes to healthcare, the US is not a civilized country. If reform of the NHS is again on the cards, let us please look towards the more civilized parts of the world!
It has been reported that the PLASTIC SURGERY INSTITUTE OF ·UTAH, INC.; MICHAEL KIRK MOORE JR.; KARI DEE BURGOYNE; KRISTIN JACKSON ANDERSEN; AND SANDRA FLORES, stand accused of running a scheme out of the Plastic Surgery Institute of Utah, Inc. to defraud the United States and the Centers for Disease Control and Prevention.
Dr. Michael Kirk Moore, Jr. and his co-defendants at the Plastic Surgery Institute of Utah have allegedly given falsified vaccine cards to people in exchange for their donating $50 to an unnamed organization, one which exists to “liberate the medical profession from government and industry conflicts of interest.” As part of the scheme, Moore and his co-defendants are accused of giving children saline injections so that they would believe they were really being vaccinated.
The co-defendants are Kari Dee Burgoyne, an office manager at the Plastic Surgery Institute of Utah; Sandra Flores, the office’s receptionist; and, strangest of all, a woman named Kristin Jackson Andersen, who according to the indictment is Moore’s neighbor. Andersen has posted copious and increasingly conspiratorial anti-vaccine content on Facebook and Instagram; Dr. Moore himself was a signatory on a letter expressing support for a group of COVID-skeptical doctors whose certification was under review by their respective medical boards. The letter expresses support for ivermectin, a bogus treatment for COVID.
According to the indictment, the Plastic Surgery Center of Utah was certified as a real vaccine provider and signed a standard agreement with the CDC, which among other things requires doctor’s offices not to “sell or seek reimbursement” for vaccines.
Prosecutors allege that, when people seeking falsified vaccine cards contacted the office, Burgoyne, the office manager, referred them to Andersen, Dr. Moore’s neighbor. Andersen, according to the indictment, would ask for the name of someone who’d referred them—it had to be someone who’d previously received a fraudulent vaccine card, per the indictment—then direct people to make a $50 donation to a charitable organization, referred to in the indictment only as “Organization 1.” Each vaccine card seeker was required to put an orange emoji in the memo line of their donation.
After making a donation to the unnamed charitable organization, prosecutors allege, Andersen would send a link to vaccine card seekers to enable them to make an appointment at the Plastic Surgery Institute. With adult patients, Moore would allegedly use a real COVID vaccine dose in a syringe, but squirt it down the drain. Flores, the office’s receptionist, gave an undercover agent a note, reading “with 18 & younger, we do a saline shot,” meaning that kids were injected with saline instead of a vaccine. Prosecutors allege the team thus disposed of at least 1,937 doses of COVID vaccines.
All four people are charged with conspiracy to defraud the United States; conspiracy to convert, sell, convey, and dispose of government property; and conversion, sale, conveyance, and disposal of government property and aiding and abetting.
Throughout the scheme, the group reported the names of all the vaccine seekers to the Utah Statewide Immunization Information System, indicating that the practice had administered 1,937 doses of COVID-19 vaccines, which included 391 pediatric doses. The value of all the doses totaled roughly $28,000. With the money from the $50 vaccination cards totaling nearly $97,000, the scheme was valued at nearly $125,000, federal prosecutors calculated.
“By allegedly falsifying vaccine cards and administering saline shots to children instead of COVID-19 vaccines, not only did this provider endanger the health and well-being of a vulnerable population, but also undermined public trust and the integrity of federal health care programs,” Curt Muller, special agent in charge with the Department of Health and Human Services for the Office of the Inspector General, said in a statement.
_________________________________
I am already baffled by anti-vax attitudes when they originate from practitioners of so-called alternative medicine (SCAM). When they come from real physicians and are followed by real actions, I am just speechless. As I stated many times before: studying medicine does unfortunately not protect you from recklessness, greed, or stupidity.
Drip IV is “Australia’s first and leading mobile healthcare company specialising in assisting with nutritional deficiencies”. They claim to provide a mobile IV service that is prescribed and tailored individually to your nutritional needs. Treatment plans and customised infusions are determined by a medical team to suit individual requirements. They deliver vitamins, minerals and amino acids directly to the body via the bloodstream, a method they state allows for optimal bioavailability.
These claims are a little puzzling to me, not least because vitamins, minerals and amino acids tailored individually to the nutritional needs of the vast majority of people would mean administering nothing at all. But I guess that virtually every person who consults the service will get an infusion [and pay dearly for it].
The Australian Therapeutic Goods Administration (TGA) seems to have a similarly dim view on Drip IV. The TGA has just issued 20 infringement notices totalling $159,840 to the company and to one of its executive officers. The reason: unlawful advertising of intravenous infusion products to Australian consumers on a company website and social media. Ten notices totalling $133,200 were issued to the company and ten notices totalling $26,640 were issued to an executive officer. The TGA considers the intravenous infusion products to be therapeutic goods because of the claims made about them, and the advertising to be unlawful because the advertisements allegedly:
- contained prohibited representations, such as claims regarding cancer.
- contained restricted representations such as that the products would alleviate fatigue caused by COVID-19, assist in the treatment of Graves’ Disease and Alzheimer’s Disease, and support the treatment of autoimmune diseases such as Multiple Sclerosis. No TGA approval had been given to make such claims.
- referred to ingredients that are prescription only, such as glutathione. Prescription medicines cannot be advertised directly to the public in Australia.
- contained a statement or picture suggesting or implying the products were ‘TGA Approved’. Advertising of therapeutic goods cannot include a government endorsement.
- contained a statement or picture expressing that the goods were ‘miraculous’.
Vitamin infusions have become very popular around the globe. There are now thousands of clinics offering this service, and many of them advertise aggressively with claims that are questionable. Here is just one example from the UK:
Modern life is hectic. If you are looking to boost your wellbeing, increase your energy levels, lift your mood and hydrate your body, Vitamin IV Infusions are ideal. Favoured by celebrities such as Madonna, Simon Cowell and Rihanna, Vitamin IV Infusions are an easy, effective way of delivering vitamins, minerals and amino acids directly into your bloodstream via an IV (intravenous) drip. Vitamins are essential for normal growth and staying healthy – but our bodies can’t produce all of the nutrients we need to function and thrive. That’s why more than one in three people take daily vitamin supplements – often without realising that only 15% of the active nutrients consumed orally actually find their way into their bloodstream. With Vitamin IV Infusions, the nutrients enter your bloodstream directly and immediately, and are delivered straight to your cells. We offer four different Vitamin IV Infusions, so you can choose the best combination for your personal needs, while boosting your general health, energy and wellbeing.
My advice to consumers is a little different and considerably less costly:
- to ensure you get enough vitamins, minerals, and amino acids, eat a balanced diet;
- to boost your well-being, sit down and calculate the savings you made by NOT using such a service;
- to increase your energy levels, take a nap;
- to lift your mood, recount the money you saved and think of what nice things you might buy with it;
- to hydrate your body drink a glass of water.
Perhaps it is time the authorities in all countries had a look at what these clinics are offering and what health claims they are making. Perhaps it is time they act as the TGA just did.
All healthcare professionals have an ethical obligation to be truthful and act in the best interest of the patient by adhering to the best available evidence. Providing false or misleading information to patients or consumers is thus a breach of medical ethics. In Canada, the authorities have started taking action against nurses that violate these ethical principles.
- A nurse has been suspended for asking a co-worker to create fake vaccine records.
Now it has been reported that a former registered nurse in West Kelowna has been suspended for four weeks after giving a vulnerable client anti-vaccine information and recommending “alternative pseudoscience” treatments.
According to the terms of a consent agreement posted on the B.C. College of Nurses and Midwives site, Carole Garfield was under investigation for actions that happened in September 2021. The college claims that Garfield contacted the client when she was off duty, using her personal mobile phone and email to give information against the COVID-19 vaccine and recommending so-called alternative medicine (SCAM). The exact nature of the “pseudoscience modalities” Garfield recommended to the client was not listed in the college’s notice.
Garfield’s nursing licence was cancelled back in April, according to the college’s registry. It’s unclear how exactly the four-week suspension will be applied. In addition to her month-long suspension and a public reprimand, Garfield is not allowed to be the sole nurse on duty for six months. She will also be given education about ethics, boundaries, and client confidentiality, as well as the province’s professional nursing standards. “The inquiry committee is satisfied that the terms will protect the public,” read a statement from the college.
In my view, it is high time for professional bodies to act against healthcare professionals who issue misleading information to their patients. In the realm of so-called alternative medicine (SCAM), issuing false or misleading information is extremely common and causes untold harm. Such harm would be largely preventable if the professional bodies in charge would start acting responsibly in the best interest of patients. It is high time that they follow the Canadian example!

