eczema
Atopic dermatitis (AD) is a common condition that often frustrates all attempts of treatment. This is an ideal situation for homeopaths who claim to have the solution. Yet the evidence fails to support their optimism. The two systematic reviews on the subject are not encouraging:
- There was insufficient evidence to make recommendations on maternal allergen avoidance for disease prevention, oral antihistamines, Chinese herbs, dietary restriction in established atopic eczema, homeopathy, house dust mite reduction, massage therapy, hypnotherapy, evening primrose oil, emollients, topical coal tar and topical doxepin.
- The evidence from controlled clinical trials therefore fails to show that homeopathy is an efficacious treatment for eczema.
But now, a new study has emerged and it seems to contradict the previous conclusions. This study compared the efficacy of individualized homeopathic medicines (IHMs) against placebos in the treatment of AD.
In this double-blind, randomized, placebo-controlled trial of 6 months duration (n = 60), adult patients were randomized to receive either IHMs (n = 30) or identical-looking placebos (n = 30). All participants received concomitant conventional care, which included the application of olive oil and maintaining local hygiene. The primary outcome measure was disease severity using the Patient-Oriented Scoring of Atopic Dermatitis (PO-SCORAD) scale; secondary outcomes were the Atopic Dermatitis Burden Scale for Adults (ADBSA) and Dermatological Life Quality Index (DLQI) – all were measured at baseline and every month, up to 6 months. Group differences were calculated on the intention-to-treat sample.
After 6 months of intervention, inter-group differences became statistically significant on PO-SCORAD, the primary outcome (−18.1; 95% confidence interval, −24.0 to −12.2), favoring IHMs against placebos (F 1, 52 = 14.735; p <0.001; two-way repeated measures analysis of variance). Inter-group differences for the secondary outcomes favored homeopathy, but were overall statistically non-significant (ADBSA: F 1, 52 = 0.019; p = 0.891; DLQI: F 1, 52 = 0.692; p = 0.409).
The authors concluded that IHMs performed significantly better than placebos in reducing the severity of AD in adults, though the medicines had no overall significant impact on AD burden or DLQI.
I was unable to access the full paper, or more precisely unwilling to pay for it (in case someone has access, please post the link in the comments section below). From what can be gleaned from the abstract, this study is rigorous and clearly reported.
So, why is the outcome positive?
Pehaps one clue lies in the origin of the study. Here are the affiliations of the authors:
- 1Department of Materia Medica, Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, Howrah, West Bengal, India.
- 2Department of Pathology and Microbiology, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 3Department of Pathology and Microbiology, Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, Govt. of West Bengal, Howrah, West Bengal, India.
- 4Department of Repertory, JIMS Homoeopathic Medical College and Hospital, Shamshabad, Telangana, India.
- 5Department of Repertory, Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, Govt. of West Bengal, Howrah, West Bengal, India.
- 6Department of Health and Family Welfare, Homoeopathic Medical Officer, Rajganj State Homoeopathic Dispensary, Rajganj Government Medical College and Hospital, Uttar Dinajpur, West Bengal, India.
- 7Department of Pathology and Microbiology, National Tuberculosis Elimination Program Wing, Imambara Sadar Hospital, Hooghly, Govt. of West Bengal, India.
- 8Department of Organon of Medicine and Homoeopathic Philosophy, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 9Department of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 10Department of Health and Family Welfare, East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre, Govt. of West Bengal, India.
- 11Department of Repertory, D. N. De Homoeopathic Medical College and Hospital, Kolkata, West Bengal, India.
I have previously noted that Indian studies of homeopathy (almost) never report a negative result. Why? Are the Indian homeopaths better than those elsewhere, or are they just less honest?
I recently looked at the list of best-sellers in homeopathy on Amazon. To my surprise, there were several books that were specifically focused on the homeopathic treatment of children. Since we had, several years ago, published a systematic review of this subject, these books interested me. Here is what Amazon tells us about them:
Homeopathic remedies are increasingly being used to treat common childhood ailments. They are safe, have no side effects or allergic reactions, are inexpensive and, above all, effective. In this guide, Dana Ullman explains what homeopathy is, how it works and how you can use it correctly to enhance your child’s health. He recommends remedies for more than 75 physical and emotional conditions, including: allergies, grief, anxiety, headaches, asthma, measles, bedwetting, nappy rash, bites and stings, shock, burns, sunburn, colic, teething, coughs and colds and travel sickness
Without doubt, this is the most comprehensive book on homeopathic pediatrics. Included is a complete guide to the correct use of homeopathy, recommended remedies for the treatment of more than seventy-five common physical, emotional, and behavioral conditions, and valuable information on the essential medicines that all parents should have in their home medicine kits
Tricia Allen, a qualified homeopath, offers a host of practical advice on how to treat illness using natural, homeopathic remedies. Homeopathy differs from conventional medicine in that it does not only alleviate the individual symptoms of an illness, but treats the underlying state to ensure that the disease does not return, something which rarely occurs when using traditional remedies. This guide gives you advice on; what homeopathy is and how to use it; each stage of childhood and how to deal with the complaints that occur at that time of a child’s development; the most common childhood illnesses, how to take your own steps to treating them, which homeopathic remedies to use and when to seek medical help and first aid.
The Homeopathic Treatment of Children is indispensible at giving both a clear overall impression of the various major constitutional types, and also a detailed outline for reference at the end of each chapter. Not only does Paul Herscu draw from various sources (repertories and materia medica), he also adds indispensable original information from his successful practice.
______________________________
The fact that such books exist is perhaps not all that surprising. Yet, I do find the fact that they are among the best-selling books on homeopathy surprising – or to be more precise, I find it concerning.
Why?
Simple: children cannot give informed consent to the treatments they receive. Thus, consent is given for them by their parents or (I suspect often) not at all. This renders homeopathic treatment of children more problematic than that of fully competent adults.
Homeopathy has not been shown to be effective for any pediatric condition. I know Dana Ullman disagrees and claims it works for children’s allergies, grief, anxiety, headaches, asthma, measles, bedwetting, nappy rash, bites and stings, shock, burns, sunburn, colic, teething, coughs and colds, and travel sickness. Yet, these claims are not based on anything faintly resembling sound evidence! Our above-mentioned systematic review reached the following conclusion: “The evidence from rigorous clinical trials of any type of therapeutic or preventive intervention testing homeopathy for childhood and adolescence ailments is not convincing enough for recommendations in any condition.”
And what follows from this state of affairs?
I am afraid it is this:
Treating sick children with homeopathy amounts to child abuse.
Holistic medicine is based on several core values:
- good health is a combination of physical, emotional, mental, spiritual, and social wellness
- prevention first, treatment second
- disease is caused by a problem with the whole body, rather than a single event or body part
- the goal of treatment is to fix the underlying cause of disease, instead of just improving the symptoms
- treatment involves a wide range of options, including education, self-care, CAM, and traditional medicine
- a person is not defined by their condition
- the relationship between a doctor and the person being treated determines the treatment outcome
Generally, traditional doctors treat symptoms. They provide medical solutions to alleviate a disease.
A holistic doctor treats the body as one. They aim to find the cause behind the disease, instead of just fixing the symptoms. This could require multiple therapies.
For example, if you have eczema, a medical doctor may give you a prescription cream. But a holistic doctor may suggest dietary and lifestyle changes. The holistic doctor might also recommend using the cream, plus natural home remedies like oatmeal baths.
So, now we know!
This could, of course, be just laughable if it were not perpetuating such common misconceptions. And as this sort of BS is so common, I feel obliged to carry on exposing it. Let me, therefore, correct the main errors in the short paragraph:
- ‘Traditional doctors’ are just doctors, proper doctors; holistic healers often give themselves the title ‘doctor’ but, unless they have been to medical school, they are not doctors.
- ‘Doctors treat symptoms’; yes, they do. But whenever possible, they treat the cause too. Therefore they do what is possible to identify the cause. And during the last 150 years or so, they have become reasonably good at this task.
- ‘A holistic doctor treats the body as one.’ That’s what they claim. But in reality, they are often not trained to do so. The body is mighty complex, and many holistic practitioners are simply not trained for coping with this complexity.
- ‘They aim to find the cause behind the disease’. They might well aim at that, but if they are not fully trained doctors, this is an impossible aim, and they merely end up finding what they have been taught about the cause of disease. An imbalance of Yin and Yang is the imagined cause of disease in TCM, and for many chiropractors, a subluxation is the cause of disease. But such assumptions are not facts; it is merely wishful thinking which get in the way of finding true causes of disease.
- Eczema happens to be a superb example (thank you ‘helpline’). The oatmeal bath of the holistic practitioner is at best a symptomatic treatment. This is why a proper doctor aims to find the cause of eczema which could be an allergy, for instance. Having identified it, the doctor would then advise how to avoid the allergen. If that is possible, further treatment might not be even necessary.
When practitioners are elaborating on their concept of holism, one often only needs to read on to find that those who pride themselves on holism are, in fact, the victims of multiple errors (or perhaps they use the holism gimmick only as a sales strategy, because consumers fall easily for this ‘bait and switch’). And those doctors who are accused of lacking holism are, in fact, more likely to be holistic than the so-called holists.
Evening primrose oil (EPO) is amongst the best-selling herbal remedies of all times. It is marketed in most countries as a dietary supplement. It is being promoted for eczema, rheumatoid arthritis, premenstrual syndrome, breast pain, menopause symptoms, and many other conditions. EPO seems to be a prime example for the fact that, in alternative medicine, the commercial success of a remedy is not necessarily determined by the strength of the evidence but by the intensity and cleverness of the marketing activities.
Evening primrose oil has been extensively tested in clinical trials for a wide range of conditions, including eczema (atopic dermatitis), postmenopausal symptoms, asthma, psoriasis, cellulite, hyperactivity, multiple sclerosis, schizophrenia, obesity, chronic fatigue syndrome, rheumatoid arthritis, and mastalgia. As I have reported previously, these data were burdened with mischief and scientific misconduct, and it is therefore not easy to differentiate between science, pseudoscience and fraud. The results of the more reliable investigations fail to show that it is effective for any condition. A Cochrane review of 2013, for instance, concluded that supplements of evening primrose oil lack effect on eczema; improvement was similar to respective placebos used in trials.
But now, a new study has emerged that casts doubt on this conclusion. The aim of this double-blinded, placebo-controlled RCT is to evaluate the efficacy and safety of EPO in Korean patients with atopic dermatitis (AD).
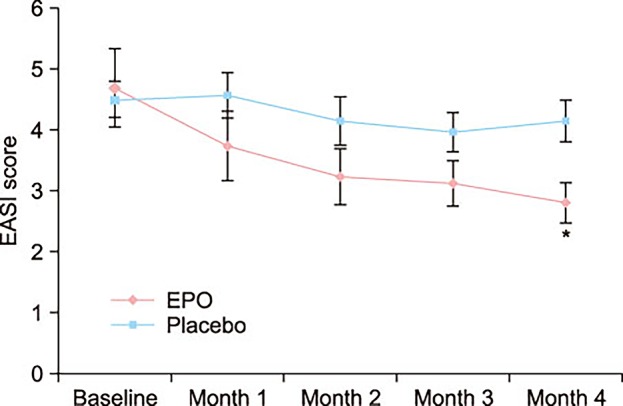
Fifty mild AD patients with an Eczema Area Severity Index (EASI) score of 10 or less were randomly divided into two groups. The first group received an oval unmarked capsule containing 450 mg of EPO (40 mg of GLA) per capsule, while placebo capsules identical in appearance and containing 450 mg of soybean oil were given to the other group. Treatment continued for a period of 4 months. EASI scores, transepidermal water loss (TEWL), and skin hydration were evaluated in all the AD patients at the baseline, and in months 1, 2, 3, and 4 of the study.
At the end of month 4, the patients of the EPO group showed a significant improvement in the EASI score, whereas the patients of the placebo group did not. There was a significant difference in the EASI score between the EPO and placebo groups. Although not statistically significant, the TEWL and skin hydration also slightly improved in the EPO patients group. Adverse effect were not found in neither the experimental group nor the control group during the study period.
The authors concluded by suggesting that EPO is a safe and effective medicine for Korean patients with mild AD.
I find this study odd for several reasons:
- One cannot possibly draw conclusions based on such a small sample.
- The authors state that a total of 69 mild AD patients were enrolled and randomized into either the control group (14 males and 17 females) or the EPO group (20 males and 18 females). Six patients in the control group and 13 patients in the EPO group dropped out due to follow up loss. No patient dropped out because the disease worsened. Should this not have necessitated an intention-to-treat analysis? And, if 19 patients were lost to follow-up, how do the authors know that their disease did not worsen?
- The graph shows impressively the lack of a placebo-response. I don’t understand why there was none.
- The authors state that there were no adverse effects at all. I find this implausible; we know that even taking placebos will prompt patients to report adverse effects.
So, what to make out of this?
I am not at all sure, but one thing is certain: this study does not alter my verdict on EPO; as far as I am concerned, the effectiveness of EPO for AD is unproven.
The ‘ALTERNATIVE MEDICINE SOCIETY’ claims to be a ‘a global network of medical practitioners and contributors who scour the best research and findings from around the world to provide the best advice on alternative, holistic, natural and integrative medicines and treatments for free.’
Sounds great!
They even give advice on ‘7 common diseases you can treat through natural medicine.’ This headline fascinated me, and I decided to have a closer look at what is being recommended there. The following is copied from the website which looks to me as though it was written by a naturopath. My comments appear dispersed in the original text and are in bold.
Despite an exponential research advancement in recent years, we’re finding more and more problems with conventional medicine – from reports of fraud, to terrible medicinal side effects, to bacterial tolerance to antibiotics. Thus, it’s no surprise that more and more people are looking towards more natural medicine for disease management. Many people are seeking solutions which are not only inexpensive, but are also less harmful. Did you know that a lot of the medical conditions suffered by patients today can be adequately treated with natural medicine? Here are seven diseases you can treat through natural medicine:
- High blood pressure/hypertension
High blood pressure, or hypertension, is a condition most of us are really familiar with. It’s a risk factor, not a ‘disease’. Defined as the elevation of blood pressure in systemic arteries, hypertension left untreated could lead to serious, possibly fatal complications such as strokes and heart attacks. Conventional treatments for hypertension usually include a cocktail of several drugs (no, good conventional doctors start with life-style advice, if that is not successful, one adds a diruretic, and only if that does not work, one adds a further drug) consisting of vasodilators, alpha/beta blockers, and enzyme inhibitors. However, hypertension can be managed, and altogether avoided with the use of natural medicine. Alternative treatments involve lifestyle changes (e.g. intentionally working out, alcohol intake moderation), dietary measures (e.g. lowering salt intake, choosing healthier food options), and natural medicine (e.g. garlic). As pointed out already, this is the conventional approach! Unfortunately, it often does not work because it is either not sufficiently effective or the patient is non-compliant. Altogether alternative treatments play only a very minor (many experts would say no) role in the management of hypertension.
- Arthritis
Arthritis literally translated from Greek, means joint (arthro-) inflammation (-itis). There are two main categories of arthritis: inflammatory and degenerative, and they need to be managed differently. This condition is common in old patients, due to prior dietary choices (diet is not important enough to be mentioned on 1st place), and the natural wearing out of joint structures. Doctors typically prescribe anti-inflammatory drugs (e.g. steroids) to reduce irritation, and pain relievers (e.g. analgesics) for managing the pain. On the other hand, natural medicine could do an equally effective job in treating arthritis, through the use of several herbs such as willow, turmeric, ginger, and capsicum. It is not true that these herbs have been shown to be of equal effectiveness. Research has also shown that lifestyle measures such as weight loss (that would be the advice of conventional doctors), and other natural treatments such as acupuncture (not very effective for degenerative arthritis and ineffective for inflammatory arthritis) and physical therapy (that is conventional medicine), also lessen pain and inflammation in patients. Altogether alternative treatments play only a very minor role in the management of arthritis.
- Bronchitis
Bronchitis may be defined as the irritation, or swelling of the bronchial tubes connecting our nasal cavity to our lungs commonly cause by infections or certain allergens (that would be asthma, not bronchitis). Patients with bronchitis typically deal with breathing difficulties, coughing spells, nasal congestion, and fever. There are usual prescriptions for bronchitis, but there are also very effective natural medicine available. Natural medicine include garlic, ginger, turmeric, eucalyptus, Echinacea, and honey. None of these have been shown by good evidence to be ‘very effective’! These herbs may be prepared at home as tonics, tea, or taken as is, acting as anti-microbial agents for fighting off the infections. Altogether alternative treatments play only a very minor role in the management of bronchitis.
- Boils
Boils are skin infections which occur as pus-filled pimples in various parts of the body. Despite being highly contagious and painful, boils can easily be treated with natural medicine. Some of the herbs proven to be effective in treating boils include Echinacea, turmeric, garlic, and tea tree oil, due to the presence of natural chemicals which have antibiotic capacities. There is no good evidence to support this claim. Repeated exposure to topical application of these natural medicine is guaranteed to cure your boils in no time. Altogether alternative treatments play only a very minor role in the management of boils.
- Eczema
Eczema is also a skin condition resulting from allergic reactions which are typically observed as persistent rashes. The rashes are usually incredibly itchy, showing up in the most awkward places such as the inside of the knees and thighs. Thankfully, eczema can be managed by lifestyle measures (such as avoiding certain foods which elicit allergies – these measures would be entirely conventional and require conventional allergy testing to be effective), and natural medicine. These includes herbal components such as sunflower seed oil, coconut oil, evening primrose oil and chamomile. There is no good evidence to show that these therapies are effective. These natural medicine contain different active ingredients which are not only able to moisturize the affected skin, but are also able to reduce inflammation and soothe itchiness. Altogether alternative treatments play only a very minor role in the management of eczema.
- Constipation
Constipation is a normal (??? why should it be normal???) medical condition in which patients are unable to empty bowels at ease. It may be caused by a wide variety of reasons such as bowel stricture, hyperparathyroidism, or simply a case of terrible (???) food choices. However, it can very easily be treated with natural medicine. Some common remedies are molasses, sesame seeds, fiber, ginger or mint tea, lemon water, prunes, castor oil (an old-fashioned and largely obsolete conventional treatment) and coffee (for none of the other treatments is there good evidence). The action of these natural medicine involves laxative effects which stimulate contractions along the colon which incidentally moves your bowels along. Conventional doctors would recommend life-style changes and would warn patients NOT to use laxatives long-term. Altogether alternative treatments play only a very minor role in the management of constipation.
- Hay Fever
Allergic rhinitis, as hay fever is also known, are allergic reactions to certain particles like dust or pollen which incite coughing sprees, sneezing spells, and congested sinuses. There are very good natural medicine options for treating hay fever, which contain ingredients which act the same way as your conventional anti-histamine drugs. If they act the same way, what would be their advantage? Some of the natural medicine used to treat hay fever include chamomile, ginger, green, and peppermint teas, as well as butterbur, calendula, and grapefruit. Butterbur is the only one in this list that is supported by some evidence. Altogether alternative treatments play only a very minor role in the management of hay fever.
In essence, none of the 7 ‘diseases’ can be treated effectively with any of the alternative treatments recommended here. ‘The best advice on alternative, holistic, natural and integrative medicines and treatments’, it seems to me, is therefore: AVOID CHARLATANS WHO TELL YOU THAT ALTERNATIVE TREATMENTS ARE MORE EFFECTIVE THAN CONVENTIONAL MEDICINE.
One of the best-selling supplements in the UK as well as several other countries is evening primrose oil (EPO). It is available via all sorts of outlets (even respectable pharmacies – or is that supposedly respectable?), and is being promoted for a wide range of conditions, including eczema. The NIH website is optimistic about its efficacy: “Evening primrose oil may have modest benefits for eczema.” Our brand-new Cochrane review was aimed at critically assessing the effects of oral EPO or borage oil (BO) on the symptoms of atopic eczema, and it casts considerable doubt on this somewhat uncritical view.
Here is what we did: We searched six databases as well as online trials registers and checked the bibliographies of included studies for further references to relevant trials. We corresponded with trial investigators and pharmaceutical companies to identify unpublished and ongoing trials. We also performed a separate search for adverse effects. All RCTs investigating oral intake of EPO or BO for eczema were included.
Two experts independently applied eligibility criteria, assessed risk of bias, and extracted data. We pooled dichotomous outcomes using risk ratios (RR), and continuous outcomes using the mean difference (MD). Where possible, we pooled study results using random-effects meta-analysis and tested statistical heterogeneity.
And here is what we found: 27 studies with a total of 1596 participants met our inclusion criteria: 19 studies tested EPO, and 8 studies assessed BO. A meta-analysis of results from 7 studies showed that EPO failed to improve global eczema symptoms as reported by participants and doctors. Treatment with BO also failed to improve global eczema symptoms. 67% of the studies had a low risk of bias for random sequence generation; 44%, for allocation concealment; 59%, for blinding; and 37%, for other biases.
Our conclusions were clear: Oral borage oil and evening primrose oil lack effect on eczema; improvement was similar to respective placebos used in trials. Oral BO and EPO are not effective treatments for eczema.
The very wide-spread notion that EPO is effective for eczema and a range of other conditions was originally promoted by the researcher turned entrepreneur, D F Horrobin, who claimed that several human diseases, including eczema, were due to a lack of fatty acid precursors and could thus be effectively treated with EPO. In the 1980s, Horrobin began to sell EPO supplements without having conclusively demonstrated their safety and efficacy; this led to confiscations and felony indictments in the US. As chief executive of Scotia Pharmaceuticals, Horrobin obtained licences for several EPO-preparations which later were withdrawn for lack of efficacy. Charges of mismanagement and fraud led to Horrobin being ousted as CEO by the board of the company. Later, Horrobin published a positive meta-analysis of EPO for eczema where he excluded the negative results of the largest published trial, but included results of 7 of his own unpublished studies. When scientists asked to examine the data, Horrobin’s legal team convinced the journal to refuse the request.
The evidence for EPO is negative not just for eczema. To the best of my knowledge, there is not a single disease or symptom for which it demonstrably works. Our own review of the data concluded ” EPO has not been established as an effective treatment for any condition”
Our new Cochrane review might help to put this long saga to rest. In my view, it is a fascinating tale of a scientist being blinded by creed and ambition. The results of such errors can be dramatic. Horrobin misled all of us: patients, health care professionals, scientists, regulators, decision makers, businessmen. This caused unnecessary expense and set back research efforts in a multitude of areas. I find the tale also fascinating from other perspectives; for instance, it begs the question why so many ‘respectable’ manufacturers and retailers are still allowed to make money on EPO. Is it not time to debunk the EPO-myth and say it as clearly as possible: EPO helps only those who financially profit from misleading the public?
During the last decade, Professor Claudia Witt and co-workers from the Charite in Berlin have published more studies of homeopathy than any other research group. Much of their conclusions are over-optimistic and worringly uncritical, in my view. Their latest article is on homeopathy as a treatment of eczema. As it happens, I have recently published a systematic review of this subject; it concluded that “the evidence from controlled clinical trials… fails to show that homeopathy is an efficacious treatment for eczema“. The question therefore arises whether the latest publication of the Berlin team changes my conclusion in any way.
Their new article describes a prospective multi-centre study which included 135 children with mild to moderate atopic eczema. The parents of the kids enrolled in this trial were able to choose either homeopathic or conventional doctors for their children who treated them as they saw fit. The article gives only scant details about the actual treatments administered. The main outcome of the study was a validated symptom score at 36 months. Further endpoints included quality of life, conventional medicine consumption, safety and disease related costs at six, 12 and 36 months.
The results showed no significant differences between the groups at 36 months. However, the children treated conventionally seemed to improve quicker than those in the homeopathy group. The total costs were about twice higher in the homoeopathic compared to the conventional group. The authors conclude as follows: “Taking patient preferences into account, while being unable to rule out residual confounding, in this long-term observational study, the effects of homoeopathic treatment were not superior to conventional treatment for children with mild to moderate atopic eczema, but involved higher costs“.
At least one previous report of this study has been available for some time and had thus been included in my systematic review. It is therefore unlikely that this new analysis might change my conclusion, particularly as the trial by Witt et al has many flaws. Here are just some of the most obvious ones:
Patients were selected according to parents’ preferences.
This means expectations could have played an important role.
It also means that the groups were not comparable in various, potentially important prognostic variables.
Even though much of the article reads as though the homeopaths exclusively employed homeopathic remedies, the truth is that both groups received similar amounts of conventional care and treatments. In other words, the study followed a ‘A+B versus B’ design (here is the sentence that best gives the game away “At 36 months the frequency of daily basic skin care was… comparable in both groups, as was the number of different medications (including corticosteroids and antihistamines)…”). I have previously stated that this type of study-design can never produce a negative result because A+B is always more than B.
Yet, at first glance, this new study seems to prove my thesis wrong: even though the parents chose their preferred options, and even though all patients were treated conventionally, the addition of homeopathy to conventional care failed to produce a better clinical outcome. On the contrary, the homeopathically treated kids had to wait longer for their symptoms to ease. The only significant difference was that the addition of homeopathy to conventional eczema treatments was much more expensive than conventional therapy alone (this finding is less than remarkable: even the most useless additional intervention costs money).
So, is my theory about ‘A+B versusB’ study-designs wrong? I don’t think so. If B equals zero, one would expect exactly the finding Witt et al produced: A+0=A. In turn, this is not a compliment for the homeopaths of this study: they seem to have been incapable of even generating a placebo-response. And this might indicate that homeopathy was not even usefull as a means to generate a placebo-response. Whatever interpretation one adopts, this study tells us very little of value (as children often grow out of eczema, we cannot even be sure whether the results are not simply a reflection of the natural history of the disease); in my view, it merely demonstrates that weak study designs can only create weak findings which, in this particular case, are next to useless.
The study was sponsored by the Robert Bosch Stiftung, an organisation which claims to be dedicated to excellence in research and which has, in the past, spent millions on researching homeopathy. It seems doubtful that trials of this caliber can live up to any claim of excellence. In any case, the new analysis is certainly no reason to change the conclusion of my systematic review.
To their credit, Witt et al are well aware of the many weaknesses of their study. Perhaps in an attempt to make them appear less glaring, they stress that “the aim of this study was to reflect the real world situation“.Usually I do not accept the argument that pragmatic trials cannot be rigorous – but I think Witt et al do have a point here: the real word tells us that homeopathic remedies are pure placebos!