Monthly Archives: November 2018
The UK media have often disappointed me when reporting about matters related to alternative medicine. Yet, this is ‘small fry’ compared to their coverage of the EU during the last decades. Here I have selected 50 (there are plenty more) headlines from a long list of ‘alternative truths’ and Euromyths of their invented or misleading healthcare-related stories:
- New EU sulphur rules will cause problems with oil-fired Aga’s, Dec 2009
- EU ‘bans boozing’, Feb 2005
- UK diners will face £200m for EU allergen rules, Nov 2014
- False alarm over 999 calls, Dec 2006
- Ambulances turn yellow for Europe, Mar 2002
- EU to force St Johns Ambulances to replace its entire fleet, Apr 2002
- Human medicines to be forbidden for use on animals, Feb/Mar 1995
- Taxpayers money used to rehabilitate Peruvian drug addicts, Jul 2014
- EU bans children from blowing up balloons, Oct 2011
- EU health directive to prevent barmaids from showing cleavage, Nov 2005
- “EU red tape” is denying cancer patients access to new treatments, Jun 2016
- EC rules on levels of listeria threaten British cheeses, Feb 1995
- Sales of cigars to fall due to be sold individually with a health warning, Jan 1994
- Circus performers required to wear hard hats, Jul 2003
- EU responsible for your hay fever, May 2015
- Condom dimensions to be harmonised, Mar 2000
- Fishing boats obliged to carry condoms, Nov 1992
- EU to push for standard condom size, Oct 1994
- EU plans to liquify corpses and pour them down the drain, July 2010
- Traditional cricket teas will be subjected to random hygiene checks, Apr 1993
- EC to ban prawn cocktail crisps, Jan 1993
- Smoky bacon crisps to be banned, May 2003
- EU outlaws teeth whitening products, Feb 2003
- EU blocking vital checks on doctors’ qualifications, Apr 2016
- EU doctors in UK a threat to patients, Sep 2016
- UK hospital have to employ people who do not speak English, Apr 2012
- Hundreds of GPs to be forced to acquire additional qualifications, Sep 1994
- 58 hour working week will ground hospitals to a halt, Aug 2004
- UK doctors unable to treat off shore patients at night, Feb 1999
- HGV drivers not permitted to wear glasses, Feb 1996
- Regulators to set maximum heat of electric blankets, leaving pensioners cold, Oct 1993
- Organic farmers ordered by EU to use homeopathic medicine, Apr 2015
- Small inshore fishing boats to be forced to carry extensive medical kits, Dec 1994
- Rare meat to be banned due to “too much bacteria”, Sep 1993
- Street vendors face closure due to an EC food hygiene Directive, Nov 1992
- EC to stop UK citizens taking extra strong multi-vitamin pills, Feb 1993
- EU rights to reside in another member state, EU benefit claimants and NHS treatment entitlement, Feb 2013
- Brussels to ban herbal cures, Mar 1999
- License to be required to sell herbal medicines, Oct 1994
- Update on whether license to be required to sell herbal medicines, Nov 1994
- Horses to no longer receive medicine that would make them unsafe for consumption, Jan 1994
- Hysteria about listeria, Feb 1995
- European Commission approve unsafe high-risk medical devices, Jul 2016
- Medicines to receive Latin labelling, May 1999
- Soya milk indistinguishable from cow milk and thus to be banned, April 1995
- Scotch whisky must be handled as a dangerous chemical, Nov 1995
- EC hygiene rules force closure of abattoirs, Nov 1992
- EU ban on ciggie breaks? Just hot air, Jun 2007
- Brussels to reinstate tobacco subsidies, Feb 2013
- EU to ban vitamin supplements, Mar 2002
_________________________________________________________
Yes, some of this is so nonsensically idiotic that it could be quite funny.
But sadly, it is also very annoying, even infuriating. I am sure these relentless lies are partly the cause why Brexit is currently dividing the UK and threatening to become a monumental exercise in self-destruction.
On this blog and elsewhere, I have repeatedly criticised the concepts of ‘integrative medicine’ (IM). But criticising is easy, improving would be better. Today, I want to re-visit and revise the idea of IM and propose the concept of a ‘reformed integrated medicine’ (RIM).
Proponents of IM suggest that we should use ‘the best of both worlds’ for the benefit of our patients. This seems to be a progressive and ethical approach to improving healthcare. Therefore, I fully accept this idea. However, I suggest to not stop here; if we are serious about wanting the best for our patients, we must not just integrate, we should also disintegrate! We also need to think about disintegrating (discarding) modalities that are not fit for purpose. This, in a nutshell, is the concept of RIM.
In order to make real progress, we need to have a critical look at all the diagnostic, preventive, therapeutic and rehabilitative practices available to date and:
- integrate those into routine care that demonstrably generate more good than harm,
- disintegrate those that do not meet this criterion.
THE BEST, AND ONLY THE BEST OF BOTH WORLDS!!!
This means, we use must throw overboard those that are not best. In healthcare ‘best’ can, of course, only mean effective and safe.
I am aware that this is only a very rough sketch of what RIM stands for. But even in this preliminary form, it is easy to see that, although IM and RIM seem to differ only marginally, their effects on healthcare would differ dramatically. Let me demonstrate this by providing 5 examples from my area of expertise:
| Iridology | embraced by IM | discarded by RIM |
| Homeopathy | embraced by IM | discarded by RIM |
| Chiropractic | embraced by IM | discarded by RIM |
| Reiki | embraced by IM | discarded by RIM |
| Reflexology | embraced by IM | discarded by RIM |
I am sure, you get the gist of it. In RIM, we no longer employ things that don’t work. They are of no real use to patients and possibly even cause harm. RIM not only is the only ethical approach, it also generates progress.
So, RIM – just a tiny adaptation of IM – is the solution.
Gosh, I am proud of my splendid innovation.
Progress at last!
__________________________________________________________________
Ooops … I just realised, RIM has one little flaw: it already exists.
It’s called evidence-based medicine.
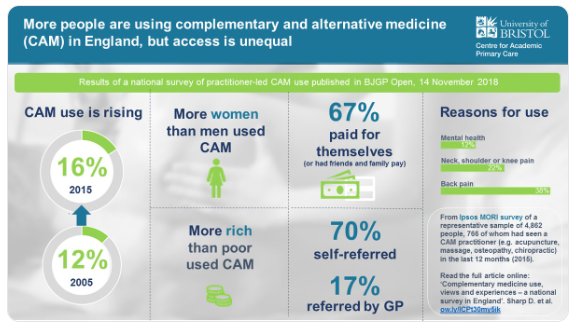
A survey was commissioned in 2015 to obtain general population figures for practitioner-led CAM use in England, and to discover people’s views and experiences regarding access.
Of 4862 adults surveyed, 766 (16%) had seen a CAM practitioner. People most commonly visited CAM practitioners for manual therapies (massage, osteopathy, chiropractic) and acupuncture, as well as yoga, pilates, reflexology, and mindfulness or meditation. Women, people with higher socioeconomic status (SES) and those in south England were more likely to access CAM. Musculoskeletal conditions (mainly back pain) accounted for 68% of use, and mental health 12%. Most was through self-referral (70%) and self-financing. GPs (17%) or NHS professionals (4%) referred and/or recommended CAM to users. These CAM users were more often unemployed, with lower income and social grade, and receiving NHS-funded CAM. Responders were willing to pay varying amounts for CAM; 22% would not pay anything. Almost two in five responders felt NHS funding and GP referral and/or endorsement would increase their CAM use.
The authors concluded that CAM use in England is common for musculoskeletal and mental health problems, but varies by sex, geography, and SES. It is mainly self-referred and self-financed; some is GP-endorsed and/or referred, especially for individuals of lower SES. Researchers, patients, and commissioners should collaborate to research the effectiveness and cost-effectiveness of CAM and consider its availability on the NHS.
The table below shows the percentage figures for specific CAMs (right column).
| Type of CAM practitioner | n | % |
| Massage practitioner | 143 | 19 |
| Osteopath | 91 | 12 |
| Acupuncturist | 88 | 11 |
| Chiropractor | 87 | 11 |
| Yoga teacher | 52 | 7 |
| Physiotherapist-delivered CAM | 41 | 5 |
| Pilates teacher | 28 | 4 |
| Reflexologist | 22 | 3 |
| Meditation and/or mindfulness teacher | 20 | 3 |
| Homeopath | 20 | 3 |
| Reiki practitioner | 17 | 2 |
| Hypnotherapist | 15 | 2 |
| Herbalist | 14 | 2 |
| Chinese herbal medical practitioner | 12 | 2 |
| Other | 74 | 10 |
Our own survey suggested that, in 2005, the 1-year prevalence of CAM-use in England was 26.3 % and the practitioner-led CAM-use was 12.1 %. The two surveys are, however, not comparable because they did use different methodologies; for instance, they included different types of CAM. I therefore think that any conclusion of an increase in practitioner-led CAM-use between 2005 and 2015 is not warranted. It also follows that the graphic below is misleading.
In the discussion, the authors of the new survey make the following point: Ability to pay may be a factor in accessing CAM (indicated by the association of CAM use with higher SES; lower SES responders being more likely to be GP-referred to CAM; and responders stating that they may use more CAM if the NHS provided services, and GPs endorsed and/or referred them). Integration of CAM into the NHS through primary care could promote continuity of care, safety, and balance of power. An integrative medicine approach includes many of the values recently included in UK health policy documents; for example, Five Year Forward View. It is patient-centred, as discussed in 2010, focuses on prevention, and emphasises patient self-management and person- and community-centred approaches to health and wellbeing. Many of these values underpin social prescribing, which is an increasingly popular model of health care. There seems to be significant patient demand for CAM and more holistic approaches, and a view that CAM may improve patient satisfaction.
I have in a previous post commented on prevalence surveys: the argument that is all too often spun around such survey data goes roughly as follows: a large percentage of the population uses alternative medicine; people pay out of their own pocket for these treatments; they are satisfied with them (if not, they would not pay for them). BUT THIS IS GROSSLY UNFAIR! Why should only those individuals who are rich enough to afford alternative medicine benefit from it? ALTERNATIVE MEDICINE SHOULD BE MADE AVAILABLE FOR ALL.
To me, it is obvious that this line of argument is dangerously wrong. It lends itself to the promotion of unproven therapies to the detriment of good healthcare and progress. Sadly, I fear that the new survey is going to be misused in this way.
The DAILY MAIL is by no means my favourite paper (see, for instance, here, here and here). This week, the Mail published another article which, I thought, is worth mentioning. The Mail apparently asked several UK doctors which dietary supplements they use for their own health (no mention of the number they had to approach to find any fitting into this category). The results remind me of a statement by the Permanent Secretary, Sir Humphrey Appleby in the famous TV series YES MINISTER: “if nobody knows anything then nobody can accuse anybody else of knowing nothing, and so the one thing we do know is that nobody knows anything, and that’s better than us knowing nothing”.
Below, I present the relevant quotes by the doctors who volunteered to be interviewed and add the most up-to date evidence on each subject.
Professor Christopher Eden, 57, is a consultant urological surgeon at the Royal Surrey County Hospital in Guildford.
“I take a 1g supplement of vitamin C daily. (The recommended daily amount, or RDA, is 40mg, which is equivalent to a large orange.) This amount of vitamin C makes the urine mildly acidic and increases the levels of an antimicrobial protein called siderocalin, found naturally in urine, which makes the environment less favourable to bad bacteria and reduces the risk of infection.”
Ascorbic acid (vitamin C) cannot be recommended for the prevention of urinary tract infections.
Louise Newson, 48, is a GP and menopause specialist based in Stratford-upon-Avon.
“Women going through the menopause or perimenopause may get bowel symptoms such as bloating which are due to hormone imbalances affecting the balance of gut bacteria. Probiotic (good bacteria) supplements correct this imbalance and are also linked to levels of the brain chemical serotonin, which can improve mood. This is important during the menopause. I make sure I take a probiotic daily, specifically one with a high bacteria count including Lactobacillus acidophilus. I look for one that has to be kept in the fridge, as this is a sign of a quality product.”
Professor Tony Kochhar, 45, is a consultant orthopaedic surgeon at London Bridge Hospital.
“Having taken statins for a couple of years, I developed tendonitis, inflammation in the foot, which caused pain around the outside of it. My GP told me to stop taking the statins, which helped, and I now control my condition with diet. I also take a supplement of collagen (a natural protein found in the tendons) to build up tendon structure and reduce pain. I take two 1,200mg collagen supplements daily and it has really helped. Within two weeks of starting them, my pain had gone.”
Dr Anne Rigg, 51, is a consultant oncologist at London Bridge Hospital.
“One theory is that vitamin D may help control normal breast cell growth and may even stop breast cancer cells from growing. The body creates vitamin D from sunlight on the skin when we are outdoors, but because of the British weather and the rightful use of sunscreen, it’s easy to become deficient. I take the recommended daily dose of 10mcg. [Fatty fish such as salmon and mackerel are good sources, too, but you’d have to eat them in large amounts to get the recommended daily dosage.] It’s vital not to overdose, as it can increase the risk of kidney stones: the vitamin helps absorb calcium from the diet, which can build up into stones.”
Supplementation with vitamin D did not result in a lower incidence of invasive cancer…
Dr Rob Hogan, 62, is an optometrist at iCare Consulting.
“I’m aware, too, of the increased risk of age-related macular degeneration (AMD), a leading cause of sight loss in people over 60. This is where the small central portion of the retina (the macula) at the back of the eye deteriorates. So I take MacuShield, a supplement which, studies have found, can help improve vision and keep the back of the eye healthy. It contains a mixture of natural compounds — lutein, zeaxanthin and meso-zeaxanthin — which are antioxidants that have been found in studies to improve vision and eye health. I take one a day, usually with a meal.”
Dr Milad Shadrooh, 37, is a dentist in Basingstoke, Hampshire.
“I take a varied supplement daily to maintain good health and, specifically, healthy teeth. It contains calcium (an adult’s RDA is 700mg, which is equivalent to three 200ml cups of milk) as most people, including me, don’t get enough in their diet.”
Dr Joanna Gach, 49, is a consultant dermatologist at University Hospitals Coventry and Warwickshire NHS Trust.
“Every so often, I take a multivitamin capsule containing zinc, selenium and biotin. These are all helpful for sorting out my brittle nails and maintaining healthy hair.”
Luke Cascarini, 47, is a consultant maxillofacial surgeon at Guy’s and St Thomas’ Hospital in London.
“I take a daily vitamin drink containing a high-dose vitamin B complex, which is necessary for good oral health.”
Dr Jenni Byrom, 44, is a consultant gynaecologist at Birmingham’s Women’s and Children’s Hospital.
“I take evening primrose oil for premenstrual symptoms such as breast pain. I take 1g of evening primrose oil daily and have found it really makes a difference.”
Dr Sarah Myhill, 60, is a GP based in Wales.
“I take 10g of vitamin C dissolved in a glass of water every day before I start my shift — and I never get colds. I believe that high doses of vitamin C can kill bad microbes on contact — or, at least, help reduce the severity of infections such as colds and sore throats.”
Jonathan Dearing, 49, is a consultant orthopaedic surgeon specialising in sports injuries at BMI Carrick Glen Hospital in Ayrshire.
“I carry a vitamin D oral spray and use it after exercise, as it helps improve muscle recovery by regulating various processes that help them repair and grow.”
Dr Glyn Thomas, 46, is a cardiologist and cardiac electrophysiologist at the Bristol Heart Institute.
“I take a magnesium supplement as it can help address an extra heartbeat — something I suffered with for 20 years.”
_____________________________________________________
Firstly, let me congratulate those colleagues who actually might have got it right:
- Dr Hogan
- Dr Shadrooh
- Mr Cascarini
- Mr Dearing
I say ‘MIGHT HAVE GOT IT RIGHT’ because, even in their cases, the evidence is far from strong and certainly not convincing.
Secondly, let me commiserate those who spend their money on unproven supplements. I find it sad that this group amounts to two thirds of all the ‘experts’ asked.
Thirdly, let me remind THE DAILY MAIL of what I posted recently: journalists to be conscious of their responsibility not to mislead the public and do more rigorous research before reporting on matters of health. Surely, the Mail did us no favour in publishing this article. It will undoubtedly motivate lots of gullible consumers to buy useless or even harmful supplements.
And lastly, let me remind all healthcare professionals that promoting unproven treatments to the unsuspecting public is not ethical.
Today is Charles’ 70th birthday! On previous occasions, I have published a detailed review of Charles’ outstanding achievements in the realm of alternative medicine. For his 70th, I feel that something else is required. How about a personal birthday card?
HAPPY BIRTHDAY YOUR ROYAL HIGHNESS!
I know, it is not easy to become 70, but you must look on the bright side: you are reasonably healthy, you are not exactly a poor man, and you even managed to change the rules and marry the woman you have always loved. What else could you wish for?
Yes, I know, your big idea of ‘Integrated Medicine’ is not doing all that brilliantly. Your book ‘Harmony‘ was viciously ridiculed, and the ‘best of both worlds’ turns out to be a bit of a strange idea. The thing is that, in healthcare, there is only one real world: the world of reality, facts and evidence. The other is the unreal world of fantasy, wishful thinking and mysticism.
We all know you love homeopathy. After listening to Laurence van der Post in your younger days, it would have been lovely for you, had the notion of a remedy based on a mystical vital force been true. It would have avoided all the complexities of reality. But now, at the age of 70, you must have realised that make belief is a poor substitute for fact.
It has become all but impossible to ignore the truth about homeopathy. Only last year, the European Academies Science Advisory Council concluded that “the claims for homeopathy are implausible and inconsistent with established scientific concepts” and that “there are no known diseases for which there is robust, reproducible evidence that homeopathy is effective beyond the placebo effect”. Such brutal realism must be painful. And now the NHS decided to ditch homeopathy completely. All your homeopathic spider memos for nothing!
Yes, it is tough to grow old. But perhaps it is not too late. You could try to forget about van der Post and all your other ill-advised ‘advisers’. Instead, you could gather a few young, energetic, bright scientists and let them inspire you with the beauty and excitement of reality and science. You could still become a force for real progress in healthcare.
Think about it and keep looking on the bright side.
Many happy returns
Edzard Ernst
The public is often impressed by scenes shown on TV where surgeons in China operate patients apparently with no other anaesthesia than acupuncture. Such films have undoubtedly contributed significantly to the common belief that acupuncture cannot possibly be a placebo (every single time I give a public talk about acupuncture, the issue comes up, and someone asks me: how can you doubt the efficacy of acupuncture when, in China, they use it for major operations?).
Some years ago, I have myself been involved is such a BBC broadcast and had to learn the hard way that such scenes are more than just a bit misleading.
Unfortunately, the experts rarely object to any of this. They seem to have become used to the false claims and overt propaganda that is rife in the promotion of acupuncture, and have resigned to the might of poor journalism.
The laudable exception is a team of French authors of a recent and excellent paper.
This unusual article analysed a clip from the program “Acupuncture, osteopathy, hypnosis: do complementary medicines have superpowers?” about acupuncture as an anaesthetic for surgical procedures in China. Their aim was to propose a rational explanation for the phenomena observed and to describe the processes leading a public service broadcasting channel to offer this type of content at prime time and the potential consequences in terms of public health. For this purpose, they used critical thinking attitudes and skills, along with a bibliographical search of Medline, Google Scholar and Cochrane Library databases.
Their results reveal that the information delivered in the television clip is ambiguous. It did not allow the viewer to form an informed opinion on the relevance of acupuncture as an anaesthetic for surgical procedures. It is reasonable to assume that the clip shows surgery performed with undisclosed epidural anaesthesia coupled with mild intravenous anaesthesia, sometimes performed in other countries.
What needs to be highlighted, the authors of this critique state, is the overestimation of acupuncture added to the protocol. The media tend to exaggerate the risks and expected effects of the treatments they report on, which can lead patients to turn to unproven therapies.
The authors concluded that broadcasting such a clip at prime time underlines the urgent need for the public and all health professionals to be trained in sorting and critically analysing health information.
In my view, broadcasting such misleading films also underlines the urgent need for journalists to be conscious of their responsibility not to mislead the public and do more rigorous research before reporting on matters of health.
Back pain is a huge problem: it affects many people, causes much suffering and leads to extraordinary high cost for all of us. Considering these facts, it would be excellent to identify a treatment that truly works. However, at present, we do not have found the ideal therapy; instead we have dozens of different approaches that are similarly effective/ineffective. Two of these therapies are massage and acupuncture.
Is one better than the other?
This study compared the efficacy of classical massage (KMT, n = 66) with acupuncture therapy (AKU, n = 66) in patients with chronic back pain. The primary endpoint was the non-inferiority of classical massage compared with the acupuncture treatment in respect of the impairment in everyday life, with the help of the Hannover function questionnaire (HFAQ) and the reduction in pain (“Von Korff”-Questionnaire) at the follow-up after one month.
In the per-protocol analysis during the period between enrollment in the study and follow-up, the responder rate of the KMT was 56.5% and thus tended to be inferior to the responder rate of the AKU with 62.5% (Δ = - 6%; KIΔ: - 23.5 to + 11.4%).
The authors concluded that classical massage therapy is not significantly inferior to acupuncture therapy in the period from admission to follow-up. Thus, the non-inferiority of the KMT to the AKU cannot be proven in the context of the defined irrelevance area.
I find such studies oddly useless.
To conduct a controlled trial, one needs an experimental treatment (the therapy that is not understood) and compare it with an intervention that is understood (such as a placebo that has no specific effects, or a treatment that has been shown to work). In comparative studies like the one above, one compares one unknown with another unknown. I do not see how such a comparison can ever produce a meaningful result.
In a way, it is like an equation with two unknowns: x + 5 = y. It is simply not possible to define either x nor y, and the equation is unsolvable.
For comparative studies of two back-pain treatments to make sense, we would need one of which the effect size is well-established. I do not think that we currently have identified such a therapy. Certainly, we cannot say that we know it for massage or acupuncture.
In other words, comparative studies like the one above are a waste of resources that cannot possibly make a meaningful contribution to our knowledge.
To put it even more bluntly: we ought to stop such pseudo-research.
I came across this article; it is neither new nor particularly scientific. Yet I believe it is sufficiently remarkable to alert you to it, quote a little from it, and hopefully make you chuckle a bit:
The Vatican’s top exorcist has spoken out in condemnation of yoga … , branding [it] as “Satanic” acts that lead[s] to “demonic possession”. Father Cesare Truqui has warned that the Catholic Church has seen a recent spike in worldwide reports of people becoming possessed by demons and that the reason for the sudden uptick is the rise in popularity of pastimes such as watching Harry Potter movies and practicing Vinyasa.
Professor Giuseppe Ferrari … says that … activities such as yoga, “summon satanic spirits” … Monsignor Luigi Negri, the archbishop of Ferrara-Comacchio, who also attended the Vatican crisis meeting, claimed that homosexuality is “another sign” that “Satan is in the Vatican”. The Independent reports: Father Cesare says he’s seen many an individual speaking in tongues and exhibiting unearthly strength, two attributes that his religion says indicate the possibility of evil spirits inhabiting a person’s body. “There are those who try to turn people into vampires and make them drink other people’s blood, or encourage them to have special sexual relations to obtain special powers,” stated Professor Ferrari at the meeting. “These groups are attracted by the so-called beautiful young vampires that we’ve seen so much of in recent years.”
Is yoga about worshiping Hindu gods, or is it about engaging in advanced stretching and exercise? At its roots, yoga is said to have originated from the ancient worship of Hindu gods, with the various poses representing unique forms of paying homage to these entities. From this, other religions such as Catholicism and Christianity have concluded that the practice is out of sync with their own and that it may result in demonic spirits entering a person’s body.
… Father Truqui sees yoga as being satanic, claiming that “it leads to evil just like reading Harry Potter.” And in order to deal with the consequences of this, his religion has had to bring on an additional six exorcists, bringing the total number to 12, just to deal with what he says is a 100% rise in the number of requests for exorcisms over the past 15 years. “The ministry of performing an exorcism is little known among priests … It’s like training to be a journalist without knowing how to do an interview.” At the same time, Father Amorth admits that the Roman Catholic Church’s notoriety for all kinds of perverted sex scandals is also indicative of demonic activity – he stated that it represents proof that “the Devil is at work inside the Vatican.” “There’s homosexual marriage, homosexual adoption, IVF [in vitro fertilization] and a host of other things,” added Monsignor Luigi Negri, the archbishop of Ferrara-Comacchio, about what he says is evidence of the existential evil in society. “There’s the glamorous appearance of the negation of man as defined by the Bible.”
END OF QUOTES
Speechless?
Me too!
Just one thought, if I may: according to Father Truqui, the most satanic man must be a ‘perverted’ catholic priest practising Yoga and reading Harry Potter!
Yesterday was the 80th anniversary of the Kristallnacht, the infamous start of the Nazi holocaust. For Cristian Becker, a German PR man who is currently spending much of his time promoting homeopathy and attacking critics of homeopathy, it was the occasion to publish this tweet:
 I will try to translate it for you:
I will try to translate it for you:
Today, on 9 November, all fundamentalist GWUP-sceptics such as Natalie Grams and Edzard Ernst reflect on what hate can bring about. First, one hates homeopathy, then advocates of homeopathy, and then it can seem as though one tolerates violence.
I struggle to respond to such vitriolic stupidity.
What makes this even more shocking is the fact that, as far as I see, none of the professional bodies of German homeopathy have distanced themselves for it.
I know Dr Grams a little, and can honestly say that neither of us ‘hates’ homeopathy nor homeopaths. And crucially, we both detest violence.
If such pseudo-arguments are now being used by the defenders of homeopathy, it mainly shows, I think, two things:
- They clearly have run out of real arguments which, in turn, suggests that the end of publicly funded homeopathy is imminent.
- Homeopathic remedies are not an effective therapy against feeble-mindedness.
The Clinic for Complementary Medicine and Diet in Oncology was opened, in collaboration with the oncology department, at the Hospital of Lucca (Italy) in 2013. It uses a range of alternative therapies aimed at reducing the adverse effects of conventional oncology treatments.
Their latest paper presents the results of complementary medicine (CM) treatment targeted toward reducing the adverse effects of anticancer therapy and cancer symptoms, and improving patient quality of life. Dietary advice was aimed at the reduction of foods that promote inflammation in favour of those with antioxidant and anti-inflammatory properties.
This is a retrospective observational study on 357 patients consecutively visited from September 2013 to December 2017. The intensity of symptoms was evaluated according to a grading system from G0 (absent) to G1 (slight), G2 (moderate), and G3 (strong). The severity of radiodermatitis was evaluated with the Radiation Therapy Oncology Group (RTOG) scale. Almost all the patients (91.6%) were receiving or had just finished some form of conventional anticancer therapy.
The main types of cancer were breast (57.1%), colon (7.3%), lung (5.0%), ovary (3.9%), stomach (2.5%), prostate (2.2%), and uterus (2.5%). Comparison of clinical conditions before and after treatment showed a significant amelioration of all symptoms evaluated: nausea, insomnia, depression, anxiety, fatigue, mucositis, hot flashes, joint pain, dysgeusia, neuropathy.
The authors concluded that the integration of evidence-based complementary treatments seems to provide an effective response to cancer patients’ demand for a reduction of the adverse effects of anticancer treatments and the symptoms of cancer itself, thus improving patient’s quality of life and combining safety and equity of access within public healthcare systems. It is, therefore, necessary for physicians (primarily oncologists) and other healthcare professionals in this field to be appropriately informed about the potential benefits of CMs.
Why do I call this ‘wishful thinking’?
I have several reasons:
- A retrospective observational study cannot establish cause and effect. It is likely that the findings were due to a range of factors unrelated to the interventions used, including time, extra attention, placebo, social desirability, etc.
- Some of the treatments in the therapeutic package were not CM, reasonable and evidence-based. Therefore, it is likely that these interventions had positive effects, while CM might have been totally useless.
- To claim that the integration of evidence-based complementary treatments seems to provide an effective response to cancer patients’ is pure fantasy. Firstly, some of the CMs were certainly not evidence-based (the clinic’s prime focus is on homeopathy). Secondly, as already pointed out, the study does not establish cause and effect.
- The notion that it is necessary for physicians (primarily oncologists) and other healthcare professionals in this field to be appropriately informed about the potential benefits of CMs is not what follows from the data. The paper shows, however, that the authors of this study are in need to be appropriately informed about EBM as well as CM.
I stumbled across this paper because a homeopath cited it on Twitter claiming that it proves the effectiveness of homeopathy for cancer patients. This fact highlights why such publications are not just annoyingly useless but acutely dangerous. They mislead many cancer patients to opt for bogus treatments. In turn, this demonstrates why it is important to counterbalance such misinformation, critically evaluate it and minimise the risk of patients getting harmed.
