politics
I think this press release might interest you:
Science advocates have filed a groundbreaking lawsuit against Boiron, Inc., one of the largest manufacturers of homeopathic products in the world, for deceiving vulnerable consumers with useless products dressed up to look like real medicine. The Center for Inquiry (CFI), which fights on behalf of consumers against pseudoscience, says Boiron routinely made false claims about what its products will treat and heal, misleading the public about the absurd pseudoscientific basis for Boiron products, and even lying about the ingredients their products contain.
“The facts could not be more clear. Boiron profits massively by deceiving consumers in their time of need,” said CFI Vice President and Legal Counsel Nick Little. “Boiron knows its products are worthless junk, so they do everything they can to obscure the truth in order to offload their snake oil upon the unwitting, the ill-informed, and the vulnerable. They can’t be allowed to get away with it any longer.”
Adherents of homeopathy claim, without evidence, that a substance which causes harm to a healthy person will cure anyone else suffering the same type of harm. In homeopathic products, the “active” ingredients are highly diluted mixtures of the so-called cures; the ingredient ends up so diluted, often literally no trace of the original substance remains. Manufacturers like Boiron then sell miniscule amounts of the already incredibly diluted ingredients and promise astounding results.
In its lawsuit, brought under the District of Columbia Consumer Protection Procedures Act, CFI alleges that Boiron sold a plethora of materially identical products, each made up of sugar pills and powders. Despite no scientifically detectable active ingredient, Boiron falsely promised consumers that each item would treat and cure a particular illness, injury, or health condition.
“Boiron sells little pills of sugar with grandiose claims. It’s hard to believe anyone would try to pass off such junk as a surefire way to treat painful skin problems, heal mental health issues, and even to counteract menopause,” said CFI Staff Attorney Aaron D. Green. “But Boiroin has been doing just that by tricking consumers into risking their health and throwing away their money on its fancy faux ‘medicines.’ It’s time for Boiron and all homeopathy hucksters to be held accountable.”
In its complaint, CFI notes that Boiron sells Saccharum officinale as a treatment for “nervous agitation in children after overindulgence.”
“Most parents would rightfully be skeptical of this product if Boiron told them what Saccharum officinale actually is,” said Green. “Table sugar.”
According to recent industry accounts, 85 percent of consumers who purchased homeopathic products did not realize they were homeopathic, and nine out of ten consumers did not even know what the term homeopathic meant.
Apart from selling products they know are useless, Boiron also misrepresented the products’ ingredients. Four Boiron products were analyzed by an independent lab, and, not only were no traces of the supposed active ingredient found, even one of the inactive ingredients could not be scientifically detected.
The Center for Inquiry is currently engaged in other lawsuits regarding homeopathy, including consumer protection cases against megaretailers CVS and Walmart for their sale and marketing of homeopathic products, the matter recently heard by the DC Court of Appeals. CFI is also engaged in an active Freedom of Information Act lawsuit that demands the Department of Health and Human Services grant the public access to the Homeopathic Pharmacopoeia of the United States (HPUS), the “bible of homeopathy” upon which federal regulation of homeopathy is based and to which the industry restricts access but for those willing to pay thousands of dollars for the privilege.
_________________________
All I can add to this is: good luck to the CFI and let’s hope reason will prevail!
An article in PULSE entitled ‘ Revolutionising Chiropractic Care for Today’s Healthcare System’ deserves a comment, I think. Here I give you first the article followed by my comments. The references in square brackets refer to the latter and were inserted by me; otherwise, the article is unchanged.
___________________________
This Chiropractic Awareness Week (4th – 10th April), Catherine Quinn, President of the British Chiropractic Association (BCA), is exploring the opportunity and need for a more integrated healthcare eco-system, putting the spotlight on how chiropractors can help alleviate pressures and support improved patient outcomes.
Chiropractic treatment and its role within today’s health system often prompts questions and some debate – what treatments fit under chiropractic care? Is the profession evidence based? How can it support primary health services, with the blend of public and private practice in mind? This Chiropractic Awareness Week, I want to address these questions and share the British Chiropractic Association’s ambition for the future of the profession.
The role of chiropractic today
The need for effective and efficient musculoskeletal (MSK) treatment is clear – in the UK, an estimated 17.8 million people live with a MSK condition, equivalent to approximately 28.9% of the total population.1 Lower back and neck pain specifically are the greatest causes of years lost to disability in the UK, with chronic joint pain or osteoarthritis affecting more than 8.75 million people.2 In addition to this, musculoskeletal conditions also account for 30% of all GP appointments, placing immense pressure on a system which is already under stress.3 The impact of the COVID-19 pandemic is still being felt by these patients and their healthcare professionals alike. Patients with MSK conditions are still having their care impacted by issues such as having clinic appointments cancelled, difficulty in accessing face-to-face care and some unable to continue regular prescribed exercise.
With these numbers and issues in mind, there is a lot of opportunity to more closely integrate chiropractic within health and community services to help alleviate pressures on primary care [1]. This is something we’re really passionate about at the BCA. However, we recognise that there are varying perceptions of chiropractic care – not just from the public but across our health peers too. We want to address this, so every health discipline has a consistent understanding.
First and foremost, chiropractic is a registered primary healthcare profession [2] and a safe form of treatment [3], qualified individuals in this profession are working as fully regulated healthcare professionals with at least four years of Masters level training. In the UK, chiropractors are regulated by law and required to adhere to strict codes of practice [4], in exactly the same ways as dentists and doctors [5]. At the BCA we want to represent the highest quality chiropractic care, which is encapsulated by a patient centred approach, driven by evidence and science [6].
As a patient-first organisation [7], our primary goal is to equip our members to provide the best treatment possible for those who need our care [8]. We truly believe that working collaboratively with other primary care and NHS services is the way to reach this goal [9].
The benefits of collaborative healthcare
As chiropractors, we see huge potential in working more closely with primary care providers and recognise there’s mutual benefits for both parties [10]. Healthcare professionals can tap into chiropractors’ expertise in MSK conditions, leaning on them for support with patient caseloads. Equally, chiropractors can use the experience of working with other healthcare experts to grow as professionals.
At the BCA, our aim is to grow this collaborative approach, working closely with the wider health community to offer patients the best level of care that we can [11]. Looking at primary healthcare services in the UK, we understand the pressures that individual professionals, workforces, and organisations face [12]. We see the large patient rosters and longer waiting times and truly believe that chiropractors can alleviate some of those stresses by treating those with MSK concerns [13].
One way the industry is beginning to work in a more integrated way is through First Contact Practitioners (FCPs) [14]. These are healthcare professionals like chiropractors who provide the first point of contact to GP patients with MSK conditions [15]. We’ve already seen a lot of evidence showing that primary care services using FCPs have been able to improve quality of care [16]. Through this service MSK patients are also seeing much shorter wait times for treatment (as little as 2-3 days), so the benefits speak for themselves for both the patient and GP [17].
By working as part of an integrated care model, with chiropractors, GPs, physiotherapists and other medical professionals, we’re creating a system that provides patients with direct routes to the treatments that they need, with greater choice. Our role within this system is very much to contribute to the health of our country, support primary care workers and reinforce the incredible work of the NHS [18].
Overcoming integrated healthcare challenges
To continue to see the chiropractic sector develop over the coming years, it’s important for us to face some of the challenges currently impacting progress towards a more integrated healthcare service.
One example is that there is a level of uncertainty about where chiropractic sits in the public/private blend. This is something we’re ready to tackle head on by showing exactly how chiropractic care benefits different individuals, whether that’s through reducing pain, improving physical function or increasing mobility [19]. We also need to encourage more awareness amongst both chiropractors and other healthcare providers about how an integrated workforce could benefit medical professionals and patients alike [20]. For example, there’s only two FCP chiropractors to date, and that’s something we’re looking to change [14].
This is the start of a much bigger conversation and, at the BCA, we’ll continue to work on driving peer acceptance, trust and inclusion to demonstrate the value of our place within the healthcare industry [21]. We’re ready to support the wider health community and primary carers, alleviating some of the pressures already facing the NHS; we’re placed in the perfect position as we have the knowledge and experience to provide essential support [22]. My main takeaway from this year’s Chiropractic Awareness Week would be to simply start a conversation with us about how [23].
About the British Chiropractic Association:
The BCA is the largest and longest-standing association for chiropractors in the UK. As well as promoting international standards of education and exemplary conduct, the BCA supports chiropractors to progress and develop to fulfil their professional ambitions with honour and integrity, at every step [24]. This Chiropractic Awareness Week, the BCA is raising awareness about the rigour, relevance and evidence driving the profession and the association’s ambition for chiropractic to be more closely embedded within mainstream healthcare [25].
- https://bjgp.org/content/70/suppl_1/bjgp20X711497
- https://www.versusarthritis.org/about-arthritis/data-and-statistics/the-state-of-musculoskeletal-health/
- https://www.england.nhs.uk/elective-care-transformation/best-practice-solutions/musculoskeletal/#:~:text=Musculoskeletal%20(MSK)%20conditions%20account%20for,million%20people%20in%20the%20UK
__________________________________
And here are my comments:
- Non sequitur = a conclusion or statement that does not logically follow from the previous argument or statement.
- A primary healthcare profession is a profession providing primary healthcare which, according to standard definitions, is the provision of health services, including diagnosis and treatment of a health condition, and support in managing long-term healthcare, including chronic conditions like diabetes. Thus chiropractors are not in that category.
- This is just wishful thinking. Chiropractic spinal manipulation is not safe!
- “Required to adhere to strict codes of practice”. Required yes, but how often do they not comply?
- This is not true.
- Chiropractic is very far from being “driven by evidence and science”.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Judging from past experience, the primary goal seems to be to protect chiropractors (see, for instance, here).
- Belief is for religion, in healthcare you need evidence. Have you looked at the referral rates of chiropractors to GPs, for instance?
- For chiropractors, the benefit is usually measured in £s.
- To offer the ” best level of care” you need research and evidence, not politically correct statements.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Belief is for religion, in healthcare you need evidence.
- First Contact Practitioners are “regulated, advanced and autonomous health CARE PROFESSIONALS who are trained to provide expert PATIENT assessment, diagnosis and first-line treatment, self-care advice and, if required, appropriate onward referral to other SERVICES.” I doubt that many chiropractors fulfill these criteria.
- Not quite; see above.
- “A lot of evidence”? Really? Where is it?
- “The benefits speak for themselves” only if the treatments used are evidence-based.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Where is the evidence?
- Awareness is not needed as much as evidence?
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Platitude = a remark or statement, especially one with a moral content, that has been used too often to be interesting or thoughtful.
- Fine, let’s start the conversation: where is your evidence?
- Judging from past experience honor and integrity seem rather thin on the ground (see, for instance here).
The article promised to ‘revolutionize chiropractic care and to answer questions like what treatments fit under chiropractic care? Is the profession evidence-based? Sadly, none of this emerged. Instead, we were offered politically correct platitudes, half-truths, and obscurations.
The revolution in chiropractic, it thus seems, is not in sight.
On this blog, I have almost exclusively written about so-called alternative medicine (SCAM), and I intend to continue along these lines. But today, I have to make an exception. The reason is the UK government’s ‘Rwanda Project’. I heard about it this morning while listening to the BBC, and I am too shocked to not write about it.
Already in 2020, it had been reported that the UK home secretary, Priti Patel, had asked officials to look into the possibility of sending all asylum seekers to Ascension, an isolated volcanic British island south of the Equator in the Atlantic Ocean.[1] At the time, the idea was met with much criticism and opposition. Today she is about to announce that a modification of her plan will, in fact, be implemented; our government is about to unveil plans to send ‘illegal migrants’ who reach Britain to Rwanda:
Flying asylum seekers to Rwanda to be processed is “despicable” and “evil”, critics have said as they hit out at government plans expected to be announced on Monday. ITV News has seen a government document that raises issues over the legality of such a policy, as ministers attempt to tackle small boat crossings of the Channel. The government document says the policy would carry the risk of legal challenges but is possible under current legislation should the government wish to push ahead. Boris Johnson is set to argue on Thursday that action is needed to combat the “vile people smugglers” turning the ocean into a “watery graveyard”. Many details of the expected announcement, such as whether it would apply just to those who arrived by what the government calls illegal means, remain unclear. The document seen by ITV News also states that any agreement of this nature would require the government to financially incentivise whichever country it reaches a deal with. Initial estimates had the policy costing in the tens of millions of pounds, but the document says this has been revised to the hundreds of millions of pounds.
The plan sounds utterly cynical, irrational, illegal, and expensive; and again there is an outrage; QC tweeted, for instance, this: “And if an asylum applicant who’s been dumped in Rwanda is then refused, what happens then? The whole thing is the stuff of nightmares. It feels like things are becoming increasingly dystopian as the days pass. Why oh why can’t we have some creative and humane people in charge.”
One might well ask, where does such an inhumane concept come from?
It turns out that it resembles an idea of the Third Reich that was equally baffling and similarly cruel.
Anticipating the German invasion of France in 1940, the German diplomat, Franz Rademacher, developed his Madagascar project, a bizarre plan to rid Europe of all Jews. It envisaged that:
- once defeated, France would agree to make Madagascar available,
- American Jewry would be blackmailed into funding the operation,
- France would be forced to find an alternate home for the 25,000 French inhabitants of Madagascar.
The plan may now sound ridiculous but, in 1940, it was seriously considered by the Nazi leadership. In June of that year, Rademacher, who then was the head of the German Foreign Ministry’s Jewish Department, presented the idea to his boss, Joachim von Ribbentrop, who then explained it to Hitler. Hitler was sufficiently impressed to discuss it with Mussolini. Rademacher wrote that “The approaching victory gives Germany the possibility, and in my view also the duty, of solving the Jewish question in Europe. The desirable solution is: All Jews out of Europe.” [2]
When Reinhard Heydrich, chief of the Reich Main Security Office, learned about the “Madagascar Project”, he highjacked it and swiftly put Adolf Eichmann in charge of it. On August 15, 1940, Eichmann published a pamphlet on the “Madagascar Project.” It envisaged that the deportation of the Jews would be carried out by the British merchant marine, after the anticipated invasion and defeat of the United Kingdom. Two ships per day would then leave Europe for Madagascar, each one carrying 1,500 Jews. In just a few years, Europe would thus become ‘Juden-frei’, free of Jews.
The Madagascar plan envisaged turning Madagascar into a monumental concentration camp under German control. The island is merely 228,900 square miles in size and would not have provided sufficient room for millions. It was therefore understood that many of the prisoners would perish, not least because of the lack of food, housing and healthcare as well as the difficult climate. 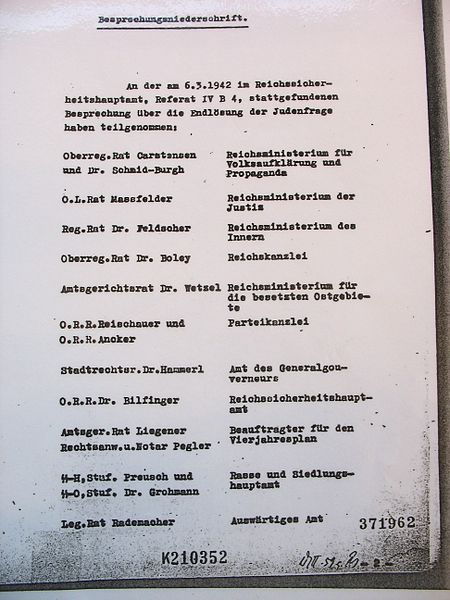
Eventually, the Madagascar plan had to be abandoned. What was decided subsequently with Rademacher’s cooperation about the fate of the Jews, the ‘final solution’, was even more unspeakably outrageously abhorrent.
The main players involved in the Madagascar project did all perish:
- Ribbentrop was sentenced to death at the Nuremberg trials.
- Hitler committed suicide.
- Heydrich was assassinated.
- Eichmann was sentenced to death in Israel.
Only Rademacher survived. After the war, he was imprisoned by British military police who mistook him for ‘small fry’ and promptly released him. In 1952, he was put on trial in West Germany for the murders of Jews he had supervised in Serbia. Yet, aided by a network of Nazi sympathizers, he managed to flee to Syria. The German court then convicted him in his absence and sentenced him to 3 years and 5 months imprisonment. In 1962, an Israeli spy delivered a letter bomb to Rademacher in Syria who, however, remained unharmed. In 1966, Rademacher returned voluntarily to West Germany and was promptly re-arrested. This time, he was sentenced to five and half years, but never actually served a prison sentence. In 1971, the German high court overruled the former judgment and ordered a new trial to take place. However, Rademacher died on 17 March 1973, before it could take place.[3]
I hope that I am wrong and that the UK government’s plan is not similar to the Nazi’s “Madagascar Project”. Maybe it is just a PR stunt of our PM to distract from his very own lawbreaking, and the ‘Rwanda project’ will never be implemented. In any case, we should urgently remind everyone of George Santayana’s wise words: “Those who cannot remember the past are condemned to repeat it.”
[1] https://www.independent.co.uk/news/uk/politics/priti-patel-asylum-ascensi on-island-atlantic-immigration-process-centre-b703625.html
[2] https://www.haaretz.com/jewish/.premium-1940-eichmann-plans-to-deport-jews-to-madagascar-1.5424692
A press release informs us that the World Health Organization (WHO) and the Government of India recently signed an agreement to establish the ‘WHO Global Centre for Traditional Medicine’. This global knowledge centre for traditional medicine, supported by an investment of USD 250 million from the Government of India, aims to harness the potential of traditional medicine from across the world through modern science and technology to improve the health of people and the planet.
“For many millions of people around the world, traditional medicine is the first port of call to treat many diseases,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “Ensuring all people have access to safe and effective treatment is an essential part of WHO’s mission, and this new center will help to harness the power of science to strengthen the evidence base for traditional medicine. I’m grateful to the Government of India for its support, and we look forward to making it a success.”
The term traditional medicine describes the total sum of the knowledge, skills and practices indigenous and different cultures have used over time to maintain health and prevent, diagnose and treat physical and mental illness. Its reach encompasses ancient practices such as acupuncture, ayurvedic medicine and herbal mixtures as well as modern medicines.
“It is heartening to learn about the signing of the Host Country Agreement for the establishment of Global Centre for Traditional Medicine (GCTM). The agreement between Ministry of Ayush and World Health Organization (WHO) to establish the WHO-GCTM at Jamnagar, Gujarat, is a commendable initiative,” said Narendra Modi, Prime Minister of India. “Through various initiatives, our government has been tireless in its endeavour to make preventive and curative healthcare, affordable and accessible to all. May the global centre at Jamnagar help in providing the best healthcare solutions to the world.”
The new WHO centre will concentrate on building a solid evidence base for policies and standards on traditional medicine practices and products and help countries integrate it as appropriate into their health systems and regulate its quality and safety for optimal and sustainable impact.
The new centre focuses on four main strategic areas: evidence and learning; data and analytics; sustainability and equity; and innovation and technology to optimize the contribution of traditional medicine to global health and sustainable development.
The onsite launch of the new WHO global centre for traditional medicine in Jamnagar, Gujarat, India will take place on April 21, 2022.
__________________________
Of course, one must wait and see who will direct the unit and what work the new centre produces. But I cannot help feeling a little anxious. The press release is full of hot air and platitudes and the track record of the Indian Ministry of Ayush is quite frankly abominable. Here are a few of my previous posts that, I think, justify this statement:
- Mucormycosis (black fungus): is the Indian AYUSH ministry trying to decimate the population?
- The ‘AYUSH COVID-19 Helpline’: have they gone bonkers?
- Individualized Homeopathic Medicines for Cutaneous Warts – the dishonesty of homeopaths continues
- Ever wondered what a homeopathic egg on the face looks like?
- An RCT on the efficacy of ayurvedic treatment on asymptomatic COVID-19 patients
- Has homeopathy caused the dramatic decline of COVID-19 cases in India?
- Eight new products aimed at mitigating COVID-19. But do they really work?
- Siddha doctors have joined those claiming to have found a cure for COVID-19
- COVID-19: homeopathy gone berserk in Mumbai
- Brazil and India collaborate in the promotion of quackery
- Hard to believe: dangerous GOVERNMENTAL advice regarding SCAM for the corona virus pandemic
WATCH THIS SPACE!
The pandemic has shown how difficult it can be to pass laws stopping healthcare professionals from giving unsound medical advice has proved challenging. The right to freedom of speech regularly conflicts with the duty to protect the public. How can a government best sail between Scylla and Charybdis? JAMA has just published an interesting paper addressing these issues. Here is an excerpt from the article that might stimulate some discussion:
The government can take several actions, including:
- Imposing sanctions on COVID-19–related practices by licensed professionals that flout substantive laws in connection with providing medical services, even if those medical services include speech. This includes physicians failing to comply with COVID-19–related public health laws applicable to medical offices and health facilities, such as mask wearing, social distancing, and restrictions on elective procedures.
- Sanctioning recommendations by professionals that patients take illegal medications or controlled substances without following legally required procedures. The government can also sanction the marketing by others of prescription medications for unapproved indications. However, “off-label” prescribing by physicians (eg, for hydroxychloroquine or ivermectin) remains lawful as long as a medication is approved by the US Food and Drug Administration for any indication and no specific legal conditions on use are in effect.
- Enforcing tort law actions (eg, malpractice, lack of informed consent) in cases of alleged patient injury that result from recommending a potentially dangerous treatment or failing to recommend a necessary treatment.
- Imposing sanctions on individualized medical advice by unlicensed individuals or organizations if giving that advice constitutes the unlawful practice of medicine.
In addition, the government probably can:
- Impose sanctions for false or misleading information offered to obtain a financial or personal benefit, particularly if giving the information constitutes fraud under applicable law. This would encompass physicians who knowingly spread false information to create celebrity or attract patients.
- Threaten disciplinary action by licensing boards against health professionals whose speech to patients conveys incorrect science or substandard medicine.
- Specify the information that may and may not be imparted by private organizations and professionals as part of specific clinical services paid for by government, such as special programs for COVID-19 testing or treatment.
- Reject legal challenges to, and enforce through generally applicable contract or employment laws, any restrictions private health care organizations place on speech by affiliated health professionals, particularly in the absence of special laws conferring “conscience” protections. This would include medical staff membership and privileges, hospital or other employment agreements, and insurance network participation.
- Enforce restrictions on speech adopted by private professional or self-regulatory organizations if the consequences for violations are limited to revoking organizational membership or accreditation.
However, the government probably cannot:
- Compel or limit health professional speech not made in connection with patient care, even if the speech is false or misleading, regardless of its alleged effect on public trust in health professions.
- Sanction speech to the general public rather than to patients, whether or not by health professionals, especially if conveyed with a disclaimer that the speech is “not intended as medical advice.”
- Sanction speech by health professionals to patients conveying political views or skepticism of government policy.
- Enforce restrictions involving information by public universities and public hospitals that legislatures, regulatory agencies, and professional licensing boards would not be constitutionally permitted to impose directly.
- Adopt restrictions on information related to overall clinical services funded by large government health programs, such as Medicare and Medicaid.
_____________________________
The article was obviously written with MDs in mind and applies only to US law. As we have seen in previous posts and comments, the debate is, however, wider. We should, I think, also have it in relation to practitioners of so-called alternative medicine (SCAM) and medical ethics. Moreover, it should go beyond advice about COVID and be extended to any medical advice given by any type of healthcare practitioner.
The German Heilpraktiker has been the subject of several of my posts. Some claim that it is an example of a well-established and well-regulated profession. Others insist that it is a menace endangering public health in Germany.
Who is right?
One answer might be found by looking at the training the German Heilpraktiker receives.
In Germany, non-medical practitioners (NMPs; or ‘Heilpraktiker’) offer a broad range of so-called alternative medicine (SCAM) methods. The aim of this investigation was to characterize schools for NMPs in Germany in terms of basic (medical) training and advanced education.
The researchers found 165 schools for NMPs in a systematic web-based search. As the medical board examination NMPs must take before building a practice exclusively tests their knowledge in conventional medicine, schools hardly include training in SCAM methods. Only a few schools offered education in SCAM methods in their NMP training. Although NMP associations framed requirements for NMP education, 83.0% (137/165) of schools did not meet these requirements.
The authors concluded that patients and physicians should be aware of the lack of training and consequent risks, such as harm to the body, delay of necessary treatment, and interaction with conventional drugs. Disestablishing the profession of NMPs might be a reasonable step.
Other interesting facts disclosed by this investigation include the following:
- There is no mandatory training for NMPs. Some attend schools but many do not and prefer to learn exclusively from books.
- The training programs of the NMP schools comprise an average of 7.4 hours per week of classroom teaching for an average of 27.1 months.
- Course participants thus complete an average of ~600 hours of training. (A degree in medicine takes an average of 12.9 semesters. With a weekly working time of 38.9 hours, this amounts to ~15,000 hours of training excluding internships etc.)
- Three-quarters of all NMP schools do not offer any practical teaching units.
- If training programs do contain practical instruction, it is usually limited to individual weekend workshops in which the measurement of vital data, physical examinations, and injections and infusions are practiced.
- The exam that NMPs have to pass consists of a written test with sixty multiple-choice questions and a 30 to 60-minute interview on case studies.
- The examination covers professional and legal anatomical and physiological basics, methods of anamnesis and diagnosis, the significance of basic laboratory values as well as practice hygiene and disinfection.
- Not included are competence in pharmacology, pathophysiology, biochemistry, microbiology, human genetics and immunology.
- The average 600 hours of training of an NMP is thus ~5% of that of a medical student.
- If an NMP fails the exam, she can repeat it as often as she needs to pass.
- The day after the exam, an NMP can open her own practice and is allowed (with only very few exceptions) to do most of what proper doctors do.
So are NMPs a danger to public health in Germany?
I let you answer this question yourself.
Homeopathy was born in Germany about 200 years ago. Now we are witnessing its slow demise due to a lack of convincing evidence.
It is only a small announcement by, but it sends out a big signal: Bremen’s doctors’ parliament has decided to cancel all homeopathy contracts.
Opponents and supporters of homeopathy agree on one thing: the latest decision of the Association of Statutory Health Insurance (KV) Bremen is an important nail in the coffin for alternative medicine. The KV representative assembly has just decided to terminate all selective contracts concerning the reimbursement of homeopathic services.
Some are rejoicing: “In Bremen it’s over” tweeted Dr. Hans-Werner Bertelsen, for example. The “sugar-sugar affine clientele” will have a harder time in the future, he stated. And: “The financing of woo must be stopped politically.”
Oliver Borrmann, a general practitioner and homeopath from Bremen, on the other hand, is outraged. He speaks of discrimination, of a conflagration, and of being the “whipping boy for everything”. “They are watching alternative medicine die right now,” he professes. It is considered chic to rise above homeopathy, he claims, and anyone who defends it is put down.
In Bremen, three contracts existed with several companies and health insurance funds which extended the range of paid services to include homeopathy for their patients. Both the KV Bremen and the homeopath Borrmann speak of a group of insured persons that is not particularly large – in Borrmann’s practice there are about 30 patients – but of a political signal that emanates from the decision.
It is the reason for the termination that makes him concerned and take notice, says Borrmann. It states: “As long as not all treatments whose benefits have already been scientifically proven can be fully financed in the statutory health insurance system, there will be no funds left for procedures for whose concrete benefits there is no evidence.”
This phraseology which quotes the KV board members Bernhard Rochell and Peter Kurt Josenhans sounds unwieldy – but it contains a clear message: homeopathy is considered useless by the KV.
——————————————-
One does not need to be a clairvoyant to predict that other parts of Germany will follow Bremen’s example. Effective lobbying and financial interests have protected German homeopathy for decades, but the eventual victory of reason, science, and evidence was inevitable.
The new German secretary of health, Prof Lauterbach, tweeted in connection with the news from Bremen:
“Mit der Wissenschaft werden Pandemien bekämpft und Krankheiten geheilt. Wir brauchen mehr Wissenschaft in der Behandlung, nicht weniger. Die Homöopathie hat keinen Platz in der modernen Medizin.”
(Science is used to fight pandemics and cure diseases. We need more science in treatment, not less. Homeopathy has no place in modern medicine.)
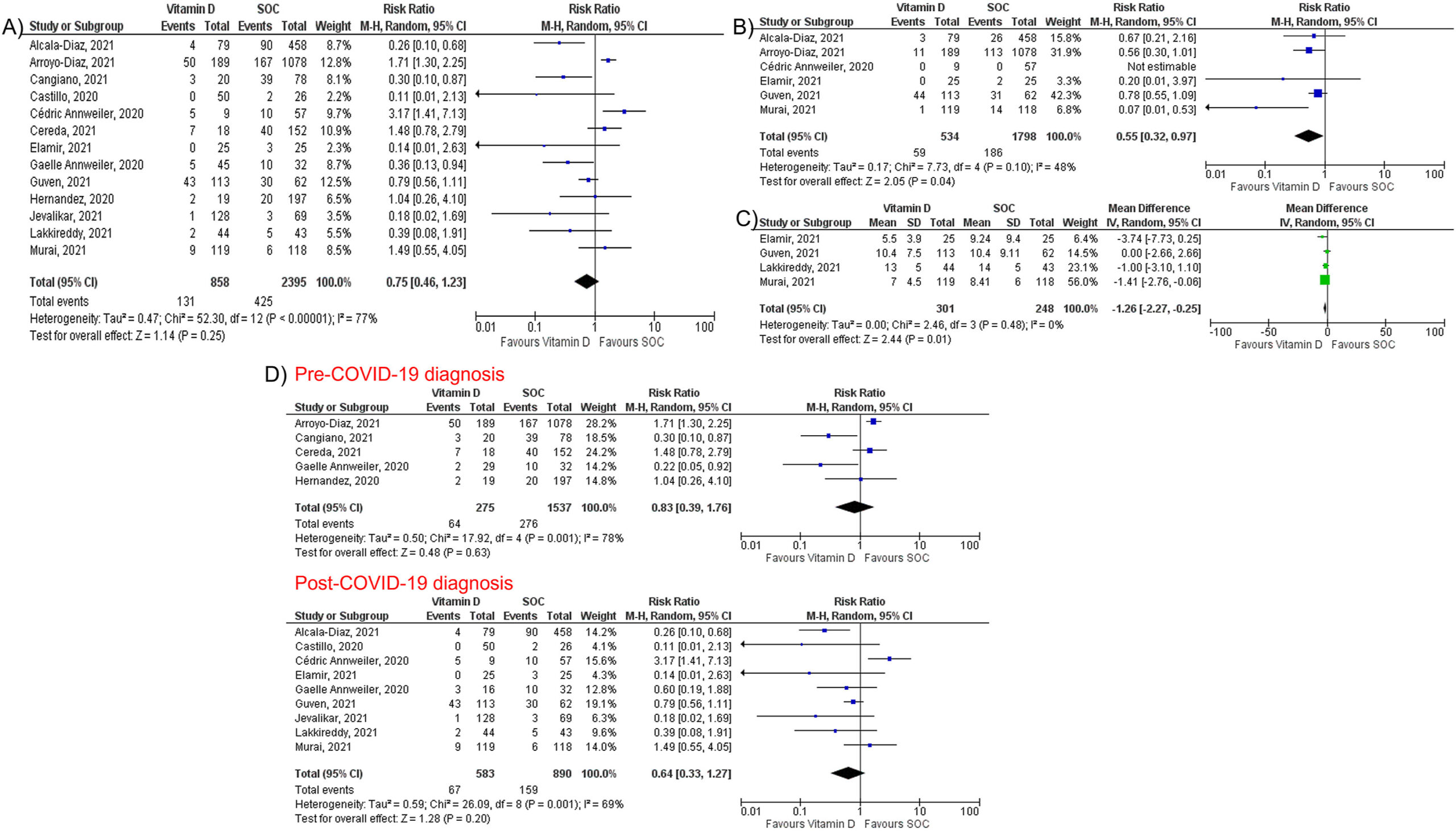
Micronutrient supplements such as vitamin D, vitamin C, and zinc have been used in managing viral illnesses. However, the clinical significance of these individual micronutrients in patients with Coronavirus disease 2019 (COVID-19) remains unclear. A team of researchers conducted this meta-analysis to provide a quantitative assessment of the clinical significance of these individual micronutrients in COVID-19.
They performed a literature search using MEDLINE, Embase, and Cochrane databases through December 5th, 2021. All individual micronutrients reported by ≥ 3 studies and compared with standard-of-care (SOC) were included. The primary outcome was mortality. The secondary outcomes were intubation rate and length of hospital stay (LOS). Pooled risk ratios (RR) and mean difference (MD) with corresponding 95% confidence intervals (CI) were calculated using the random-effects model.
The authors identified 26 studies (10 randomized controlled trials and 16 observational studies) involving 5633 COVID-19 patients that compared three individual micronutrient supplements (vitamin C, vitamin D, and zinc) with SOC.
Vitamin C
Nine studies evaluated vitamin C in 1488 patients (605 in vitamin C and 883 in SOC). Vitamin C supplementation had no significant effect on mortality (RR 1.00, 95% CI 0.62–1.62, P = 1.00), intubation rate (RR 1.77, 95% CI 0.56–5.56, P = 0.33), or LOS (MD 0.64; 95% CI -1.70, 2.99; P = 0.59).
Vitamin D
Fourteen studies assessed the impact of vitamin D on mortality among 3497 patients (927 in vitamin D and 2570 in SOC). Vitamin D did not reduce mortality (RR 0.75, 95% CI 0.49–1.17, P = 0.21) but reduced intubation rate (RR 0.55, 95% CI 0.32–0.97, P = 0.04) and LOS (MD -1.26; 95% CI -2.27, −0.25; P = 0.01). Subgroup analysis showed that vitamin D supplementation was not associated with a mortality benefit in patients receiving vitamin D pre or post COVID-19 diagnosis.
Zinc
Five studies, including 738 patients, compared zinc intake with SOC (447 in zinc and 291 in SOC). Zinc supplementation was not associated with a significant reduction of mortality (RR 0.79, 95% CI 0.60–1.03, P = 0.08).
The authors concluded that individual micronutrient supplementations, including vitamin C, vitamin D, and zinc, were not associated with a mortality benefit in COVID-19. Vitamin D may be associated with lower intubation rate and shorter LOS, but vitamin C did not reduce intubation rate or LOS. Further research is needed to validate our findings.
It must have been 17 or 18 years ago that I first met Fiona Fox. We were both giving a lecture at the same meeting. My talk was about a small study we did surveying UK homeopaths’ attitudes toward MMR vaccinations. It had landed me in deep waters: some homeopaths had complained and the Exeter ethics committee retrospectively withdrew their approval and forbade me to publish the findings (which were less than flattering for the homeopaths). I told my committee to go yonder and multiply and published our results swiftly. I was then told that I had violated our research ethics and threatened with disciplinary action by my own university.
Fiona seemed to like my stance and realized why I had to do what I did. A little later, she invited me to give a presentation at the ‘Science Media Centre’ (SMC) for journalists about our research. It was then that I realized what the SMC did and how important its work truly was.
At the time, the SMC consisted of a small team of highly motivated people linking scientists with journalists – potentially a win/win situation:
- The scientists would see with their own eyes how important journalists could be for getting their message across.
- And the journalists might comprehend that things were frequently more complex than expected.
Yet, by no means an easy job; scientists are often (sometimes rightly) nervous about speaking to journalists, and journalists sometimes (rightly) feel that scientists are not from the same planet as they are. But if it works out well – and in the SMC it usually does – the beneficiary is the consumer who can read excellent science journalism.
The concept of the SMC was as simple as it was convincing!
No wonder then that it was a monumental success. The SMC grew and so did his influence nationally and internationally. Today, there is hardly a media outlet in the UK that does not regularly refer to the SMC when reporting on matters of science. Much of the outstanding reputation of the SMC is due to the tireless work of Fiona. Her enthusiasm for science is infectious, her energy is impressive, her skills in dealing with experts are immaculate, and her nose for a good story is infallible.
In ‘BEYOND THE HYPE‘, Fiona has now summarized the first 20 eventful years of the SMC. She recounts her favorite moments and some of the biggest science stories that emerged with the help of the SMC. The book is a true page-turner and a ‘must read’ for everyone with an interest in science – entertaining and educational in equal measure. It takes us behind the scenes of some of the most remarkable recent developments in science. Fiona’s book will be out on 7 April; it is a historical document that teaches us important lessons and deserves to be read widely.
I hope that the next 20 years of the SMC will be as good as the first.
Yes, Today is ‘WORLD SLEEP DAY‘ and you are probably in bed hoping this post will put you back to sleep.
This study aimed to synthesise the best available evidence on the safety and efficacy of using moxibustion and/or acupuncture to manage cancer-related insomnia (CRI).
The PRISMA framework guided the review. Nine databases were searched from its inception to July 2020, published in English or Chinese. Randomised clinical trials (RCTs) of moxibustion and or acupuncture for the treatment of CRI were selected for inclusion. The methodological quality was assessed using the method suggested by the Cochrane collaboration. The Cochrane Review Manager was used to conduct a meta-analysis.
Fourteen RCTs met the eligibility criteria; 7 came from China. Twelve RCTs used the Pittsburgh Sleep Quality Index (PSQI) score as continuous data and a meta-analysis showed positive effects of moxibustion and or acupuncture (n = 997, mean difference (MD) = -1.84, 95% confidence interval (CI) = -2.75 to -0.94, p < 0.01). Five RCTs using continuous data and a meta-analysis in these studies also showed significant difference between two groups (n = 358, risk ratio (RR) = 0.45, 95% CI = 0.26-0.80, I 2 = 39%).
The authors concluded that the meta-analyses demonstrated that moxibustion and or acupuncture showed a positive effect in managing CRI. Such modalities could be considered an add-on option in the current CRI management regimen.
Even at the risk of endangering your sleep, I disagree with this conclusion. Here are some of my reasons:
- Chinese acupuncture trials invariably are positive which means they are as reliable as a 4£ note.
- Most trials were of poor methodological quality.
- Only one made an attempt to control for placebo effects.
- Many followed the A+B versus B design which invariably produces (false-) positive results.
- Only 4 out of 14 studies mentioned adverse events which means that 10 violated research ethics.
Sorry to have disturbed your sleep!