education
The Anglo-European College of Chiropractic (AECC) has been promoting pediatric chiropractic for some time, and I have posted about the subject before (see, for instance, here). Now the AECC has gone one decisive step further. On the website, the AECC announced an MSc ‘Musculoskeletal Paediatric Health‘:
The MSc Musculoskeletal Paediatric Health degree is designed to develop your knowledge and skills in the safe and competent care of children of all ages. Our part-time, distance-based course blends live online classes with ready to use resources through our virtual learning environment. In addition, you will have the opportunity to observe in the AECC University College clinical services at our Bournemouth campus. The course covers topics in paediatric musculoskeletal practice with specific units on paediatric development, paediatric musculoskeletal examination, paediatric musculoskeletal interventions, and paediatric musculoskeletal management. You will address issues such as risk factors and public health, including breastfeeding, supine sleep in infancy, physical activity in children and conditions affecting the musculoskeletal health of children from birth. The paediatric specific topics are completed by other optional units such as professional development, evidence-based practice, and leadership and inter-professional collaboration. In the dissertation unit you will conduct a study relevant to musculoskeletal paediatric health.
Your learning will happen through a mix of live and recorded lectures, access to online reading materials, and access to the literature through our learning services. You will also engage with the contents taught through guided activities with your peers and staff. Clinical paediatric experience is recommended to fully engage with the course. For students with limited access to a suitable clinical environment to support their studies, or for student who wants to add to their clinical experience, we are able to offer a limited number of opportunities to observe and work alongside our clinical educators within the AECC University College clinical services. Assessments are tailor made to each unit and may include a variety of methods such as critical reviews, reflective accounts, portfolios and in the last year a research dissertation.
___________________________
The AECC emphasizes its commitment to being a leading higher education institution in healthcare disciplines, nationally and internationally recognised for quality and excellence. Therefore, it seems only fair to have another look at the science behind pediatric chiropractic. Specifically, is there any good science to show that would justify a Master of Science in ‘Musculoskeletal Paediatric Health’?
So, let’s have a look and see whether there are any good review articles supporting such a degree. Here is what I found with several Medline searches (date of the review on chiropractic for any pediatric conditions, followed by its conclusion + link [so that the reader can look up the evidence]):
2008
I am unable to find convincing evidence for any of the above-named conditions.
2009
Previous research has shown that professional chiropractic organisations ‘make claims for the clinical art of chiropractic that are not currently available scientific evidence…’. The claim to effectively treat otitis seems to
be one of them. It is time now, I think, that chiropractors either produce the evidence or abandon the claim.
2009
The … evidence is neither complete nor, in my view, “substantial.”
2010
2018
What seems to emerge is rather disappointing:
- There are no really new reviews.
- Most of the existing reviews are not on musculoskeletal conditions.
- All of the reviews cast considerable doubt on the notion that chiropractors should go anywhere near children.
But perhaps I was too ambitious. Perhaps there are some new rigorous clinical trials of chiropractic for musculoskeletal conditions. A few further searches found this (again year and conclusion):
2019
2018
I might have missed one or two trials because I only conducted rather ‘rough and ready’ searches, but even if I did: would this amount to convincing evidence? Would it be good science?
No! and No!
So, why does the AECC offer a Master of Science in ‘Musculoskeletal Paediatric Health’?
Search me!
…
…
It wouldn’t have something to do with the notion that it is good for business?
Or perhaps they just want to give science a bad name?
A press release informs us that the World Health Organization (WHO) and the Government of India recently signed an agreement to establish the ‘WHO Global Centre for Traditional Medicine’. This global knowledge centre for traditional medicine, supported by an investment of USD 250 million from the Government of India, aims to harness the potential of traditional medicine from across the world through modern science and technology to improve the health of people and the planet.
“For many millions of people around the world, traditional medicine is the first port of call to treat many diseases,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “Ensuring all people have access to safe and effective treatment is an essential part of WHO’s mission, and this new center will help to harness the power of science to strengthen the evidence base for traditional medicine. I’m grateful to the Government of India for its support, and we look forward to making it a success.”
The term traditional medicine describes the total sum of the knowledge, skills and practices indigenous and different cultures have used over time to maintain health and prevent, diagnose and treat physical and mental illness. Its reach encompasses ancient practices such as acupuncture, ayurvedic medicine and herbal mixtures as well as modern medicines.
“It is heartening to learn about the signing of the Host Country Agreement for the establishment of Global Centre for Traditional Medicine (GCTM). The agreement between Ministry of Ayush and World Health Organization (WHO) to establish the WHO-GCTM at Jamnagar, Gujarat, is a commendable initiative,” said Narendra Modi, Prime Minister of India. “Through various initiatives, our government has been tireless in its endeavour to make preventive and curative healthcare, affordable and accessible to all. May the global centre at Jamnagar help in providing the best healthcare solutions to the world.”
The new WHO centre will concentrate on building a solid evidence base for policies and standards on traditional medicine practices and products and help countries integrate it as appropriate into their health systems and regulate its quality and safety for optimal and sustainable impact.
The new centre focuses on four main strategic areas: evidence and learning; data and analytics; sustainability and equity; and innovation and technology to optimize the contribution of traditional medicine to global health and sustainable development.
The onsite launch of the new WHO global centre for traditional medicine in Jamnagar, Gujarat, India will take place on April 21, 2022.
__________________________
Of course, one must wait and see who will direct the unit and what work the new centre produces. But I cannot help feeling a little anxious. The press release is full of hot air and platitudes and the track record of the Indian Ministry of Ayush is quite frankly abominable. Here are a few of my previous posts that, I think, justify this statement:
- Mucormycosis (black fungus): is the Indian AYUSH ministry trying to decimate the population?
- The ‘AYUSH COVID-19 Helpline’: have they gone bonkers?
- Individualized Homeopathic Medicines for Cutaneous Warts – the dishonesty of homeopaths continues
- Ever wondered what a homeopathic egg on the face looks like?
- An RCT on the efficacy of ayurvedic treatment on asymptomatic COVID-19 patients
- Has homeopathy caused the dramatic decline of COVID-19 cases in India?
- Eight new products aimed at mitigating COVID-19. But do they really work?
- Siddha doctors have joined those claiming to have found a cure for COVID-19
- COVID-19: homeopathy gone berserk in Mumbai
- Brazil and India collaborate in the promotion of quackery
- Hard to believe: dangerous GOVERNMENTAL advice regarding SCAM for the corona virus pandemic
WATCH THIS SPACE!
Today is the start of chiropractic awareness week 2022. On this occasion the BCA states most categorically: First and foremost, chiropractic is a statutorily regulated healthcare profession, supported by evidence, which offers a safe form of treatment for patients with a range of conditions. Here I am tempted to cite my friend Simon Singh:
THEY HAPPILY PROMOTE BOGUS TREATMENTS
I am, of course, particularly impressed by the BCA’s assurance of safety. In my view, the safety issue needs to be addressed more urgently than any other in the realm of chiropractic. So, to make a meaningful contribution to the current chiropractic awareness week, I conducted a few Medline searches to identify all publications of 2022 on chiropractic/spinal manipulation risks.
This is what I found:
Objective: Patients can be at risk of carotid artery dissection and ischemic stroke after cervical chiropractic manipulation. However, such risks are rarely reported and raising awareness can increase the safety of chiropractic manipulations.
Case report: We present two middle-aged patients with carotid artery dissection leading to ischemic stroke after receiving chiropractic manipulation in Foshan, Guangdong Province, China. Both patients had new-onset pain in their necks after receiving chiropractic manipulations. Excess physical force during chiropractic manipulation may present a risk to patients. Patient was administered with recombinant tissue plasminogen activator after radiological diagnoses. They were prescribed 100 mg and clopidogrel 75 mg daily for 3 months as dual antiplatelet therapy. There were no complications over the follow-up period.
Conclusion: These cases suggest that dissection of the carotid artery can occur as the result of chiropractic manipulations. Patients should be diagnosed and treated early to achieve positive outcomes. The safety of chiropractic manipulations should be increased by raising awareness about the potential risks.
Spontaneous intracranial hypotension (SIH) still remains an underdiagnosed etiology of new-onset headache. Important risk factors include chiropractic manipulation (CM). We present a case of a 36-year-old Filipino woman who presented with severe bifrontal and postural headache associated with dizziness, vomiting, and doubling of vision. A cranial computed tomography scan was done which showed an acute subdural hematoma (SDH) at the interhemispheric area. Pain medications were given which afforded minimal relief. On history, the headaches occurred 2 weeks after cervical CM. Cranial and cervical magnetic resonance imaging revealed findings supportive of intracranial hypotension and neck trauma, respectively. The patient improved with conservative management. We found 12 articles on SIH and CM after a systematic review of literature. Eleven patients (90.9%) initially presented with orthostatic headache. Eight patients (66.7%) were initially treated conservatively but only 5 (62.5%) had complete recovery. Recovery was achieved within 14 days from start of supportive therapy. Among the 3 patients who failed conservative treatment, 2 underwent non-directed epidural blood patch and one required neurosurgical intervention. This report highlights that a thorough history is warranted in patients with new onset headache. A history of CM must be actively sought. The limited evidence from the case reports showed that patients with SIH and SDH but with normal neurologic examination and minor spinal pathology can be managed conservatively for less than 2 weeks. This review showed that conservative treatment in a closely monitored environment may be an appropriate first line treatment.
Introduction: Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. We evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement.
Methods: COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
Results: One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including sneezing, carrying heavy load, chiropractic manipulation. Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
Conclusion: In this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Background: Manipulation and mobilisation for low back pain are presented in an evidence-based manner with regard to mechanisms of action, indications, efficacy, cost-effectiveness ratio, user criteria and adverse effects. Terms such as non-specific or specific are replaced by the introduction of “entities” related to possible different low back pain forms.
Efficacy: MM is effective for acute and chronic low back pain in terms of pain relief, recovery of function and relapse prevention. It is equally effective but less risky compared to other recommended therapies. MM can be used alone in acute cases and not only in the case of chronic low back pain where it is always and necessarily part of a multimodal therapy programme, especially in combination with activating measures. The users of MM should exclusively be physician specialists trained according to the criteria of the German Medical Association (Bundesärztekammer) with an additional competence in manual medicine or appropriately trained certified therapists. The application of MM follows all rules of Good Clinical Practice.
Adverse effects: Significant adverse effects of MM for low back pain are reported in the international literature with a frequency of 1 per 50,000 to 1 per 3.7 million applications, i.e. MM for low back pain is practically risk-free and safe if performed according to the rules of the European Training Requirements of the UEMS.
Studies have reported that mild adverse events (AEs) are common after manual therapy and that there is a risk of serious injury. We aimed to assess the safety of Chuna manipulation therapy (CMT), a traditional manual Korean therapy, by analysing AEs in patients who underwent this treatment. Patients who received at least one session of CMT between December 2009 and March 2019 at 14 Korean medicine hospitals were included. Electronic patient charts and internal audit data obtained from situation report logs were retrospectively analysed. All data were reviewed by two researchers. The inter-rater agreement was assessed using the Cohen’s kappa coefficient, and reliability analysis among hospitals was assessed using Cronbach’s Alpha coefficient. In total, 2,682,258 CMT procedures were performed in 289,953 patients during the study period. There were 50 AEs, including worsened pain (n = 29), rib fracture (n = 11), falls during treatment (n = 6), chest pain (n = 2), dizziness (n = 1), and unpleasant feeling (n = 1). The incidence of mild to moderate AEs was 1.83 (95% confidence interval [CI] 1.36-2.39) per 100,000 treatment sessions, and that of severe AEs was 0.04 (95% CI 0.00-0.16) per 100,000 treatment sessions. Thus, AEs of any level of severity were very rare after CMT. Moreover, there were no instances of carotid artery dissection or spinal cord injury, which are the most severe AEs associated with manual therapy in other countries.
_______________________________
This is not too bad after all!
Five papers are clearly better than nothing.
What conclusions might be drawn from my mini-review?
I think it might be safe to say:
- There is not much but at least some research going on in this area.
- The risks of chiropractic/spinal manipulation are real and are being recognized.
- BUT NOT BY CHIROPRACTORS! The most remarkable feature of the 5 papers, I think, is that none originates from a chiropractic team.
Thus, allow me to make a suggestion to chiropractors worldwide: Instead of continuing with HAPPILY PROMOTING BOGUS TREATMENTS, what about using the ‘chiropractic awareness week’ to raise awareness of the urgent necessity to research the safety of your treatments?
The pandemic has shown how difficult it can be to pass laws stopping healthcare professionals from giving unsound medical advice has proved challenging. The right to freedom of speech regularly conflicts with the duty to protect the public. How can a government best sail between Scylla and Charybdis? JAMA has just published an interesting paper addressing these issues. Here is an excerpt from the article that might stimulate some discussion:
The government can take several actions, including:
- Imposing sanctions on COVID-19–related practices by licensed professionals that flout substantive laws in connection with providing medical services, even if those medical services include speech. This includes physicians failing to comply with COVID-19–related public health laws applicable to medical offices and health facilities, such as mask wearing, social distancing, and restrictions on elective procedures.
- Sanctioning recommendations by professionals that patients take illegal medications or controlled substances without following legally required procedures. The government can also sanction the marketing by others of prescription medications for unapproved indications. However, “off-label” prescribing by physicians (eg, for hydroxychloroquine or ivermectin) remains lawful as long as a medication is approved by the US Food and Drug Administration for any indication and no specific legal conditions on use are in effect.
- Enforcing tort law actions (eg, malpractice, lack of informed consent) in cases of alleged patient injury that result from recommending a potentially dangerous treatment or failing to recommend a necessary treatment.
- Imposing sanctions on individualized medical advice by unlicensed individuals or organizations if giving that advice constitutes the unlawful practice of medicine.
In addition, the government probably can:
- Impose sanctions for false or misleading information offered to obtain a financial or personal benefit, particularly if giving the information constitutes fraud under applicable law. This would encompass physicians who knowingly spread false information to create celebrity or attract patients.
- Threaten disciplinary action by licensing boards against health professionals whose speech to patients conveys incorrect science or substandard medicine.
- Specify the information that may and may not be imparted by private organizations and professionals as part of specific clinical services paid for by government, such as special programs for COVID-19 testing or treatment.
- Reject legal challenges to, and enforce through generally applicable contract or employment laws, any restrictions private health care organizations place on speech by affiliated health professionals, particularly in the absence of special laws conferring “conscience” protections. This would include medical staff membership and privileges, hospital or other employment agreements, and insurance network participation.
- Enforce restrictions on speech adopted by private professional or self-regulatory organizations if the consequences for violations are limited to revoking organizational membership or accreditation.
However, the government probably cannot:
- Compel or limit health professional speech not made in connection with patient care, even if the speech is false or misleading, regardless of its alleged effect on public trust in health professions.
- Sanction speech to the general public rather than to patients, whether or not by health professionals, especially if conveyed with a disclaimer that the speech is “not intended as medical advice.”
- Sanction speech by health professionals to patients conveying political views or skepticism of government policy.
- Enforce restrictions involving information by public universities and public hospitals that legislatures, regulatory agencies, and professional licensing boards would not be constitutionally permitted to impose directly.
- Adopt restrictions on information related to overall clinical services funded by large government health programs, such as Medicare and Medicaid.
_____________________________
The article was obviously written with MDs in mind and applies only to US law. As we have seen in previous posts and comments, the debate is, however, wider. We should, I think, also have it in relation to practitioners of so-called alternative medicine (SCAM) and medical ethics. Moreover, it should go beyond advice about COVID and be extended to any medical advice given by any type of healthcare practitioner.
The German Heilpraktiker has been the subject of several of my posts. Some claim that it is an example of a well-established and well-regulated profession. Others insist that it is a menace endangering public health in Germany.
Who is right?
One answer might be found by looking at the training the German Heilpraktiker receives.
In Germany, non-medical practitioners (NMPs; or ‘Heilpraktiker’) offer a broad range of so-called alternative medicine (SCAM) methods. The aim of this investigation was to characterize schools for NMPs in Germany in terms of basic (medical) training and advanced education.
The researchers found 165 schools for NMPs in a systematic web-based search. As the medical board examination NMPs must take before building a practice exclusively tests their knowledge in conventional medicine, schools hardly include training in SCAM methods. Only a few schools offered education in SCAM methods in their NMP training. Although NMP associations framed requirements for NMP education, 83.0% (137/165) of schools did not meet these requirements.
The authors concluded that patients and physicians should be aware of the lack of training and consequent risks, such as harm to the body, delay of necessary treatment, and interaction with conventional drugs. Disestablishing the profession of NMPs might be a reasonable step.
Other interesting facts disclosed by this investigation include the following:
- There is no mandatory training for NMPs. Some attend schools but many do not and prefer to learn exclusively from books.
- The training programs of the NMP schools comprise an average of 7.4 hours per week of classroom teaching for an average of 27.1 months.
- Course participants thus complete an average of ~600 hours of training. (A degree in medicine takes an average of 12.9 semesters. With a weekly working time of 38.9 hours, this amounts to ~15,000 hours of training excluding internships etc.)
- Three-quarters of all NMP schools do not offer any practical teaching units.
- If training programs do contain practical instruction, it is usually limited to individual weekend workshops in which the measurement of vital data, physical examinations, and injections and infusions are practiced.
- The exam that NMPs have to pass consists of a written test with sixty multiple-choice questions and a 30 to 60-minute interview on case studies.
- The examination covers professional and legal anatomical and physiological basics, methods of anamnesis and diagnosis, the significance of basic laboratory values as well as practice hygiene and disinfection.
- Not included are competence in pharmacology, pathophysiology, biochemistry, microbiology, human genetics and immunology.
- The average 600 hours of training of an NMP is thus ~5% of that of a medical student.
- If an NMP fails the exam, she can repeat it as often as she needs to pass.
- The day after the exam, an NMP can open her own practice and is allowed (with only very few exceptions) to do most of what proper doctors do.
So are NMPs a danger to public health in Germany?
I let you answer this question yourself.
Vaccine hesitancy is currently recognized by the WHO as a major threat to global health. During the COVID-19 pandemic, there has been a growing interest in the role of social media in the propagation of false information and fringe narratives regarding vaccination. Using a sample of approximately 60 billion tweets, Danish investigators conducted a large-scale analysis of the vaccine discourse on Twitter. They used methods from deep learning and transfer learning to estimate the vaccine sentiments expressed in tweets, then categorize individual-level user attitudes towards vaccines. Drawing on an interaction graph representing mutual interactions between users, They analyzed the interplay between vaccine stances, interaction network, and the information sources shared by users in vaccine-related contexts.
The results show that strongly anti-vaccine users frequently share content from sources of a commercial nature; typically sources that sell alternative health products for profit. An interesting aspect of this finding is that concerns regarding commercial conflicts of interests are often cited as one of the major factors in vaccine hesitancy.
The authors furthermore demonstrate that the debate is highly polarized, in the sense that users with similar stances on vaccination interact preferentially with one another. Extending this insight, the authors provide evidence of an epistemic echo chamber effect, where users are exposed to highly dissimilar sources of vaccine information, enforcing the vaccination stance of their contacts.
The authors concluded that their findings highlight the importance of understanding and addressing vaccine mis- and disinformation in the context in which they are disseminated in social networks.
In the article, the authors comment that their findings paint a picture of the vaccine discourse on Twitter as highly polarized, where users who express similar sentiments regarding vaccinations are more likely to interact with one another, and tend to share contents from similar sources. Focusing on users whose vaccination stances are the positive and negative extremes of the spectrum, we observe relatively disjoint ‘epistemic echo chambers’ which imply that members of the two groups of users rarely interact, and in which users experience highly dissimilar ‘information landscapes’ depending on their stance. Finally, we find that strongly anti-vaccine users much more frequently share information from actors with a vested commercial interest in promoting medical misinformation.
One implication of these findings is that online (medical) misinformation may present an even greater problem than previously thought, because beliefs and behaviors in tightly knit, internally homogeneous communities are more resilient, and provide fertile ground for fringe narratives, while mainstream information is attenuated. Furthermore, such polarization of communities may become self-perpetuating, because individuals avoid those not sharing their views, or because exposure to mainstream information might further entrench fringe viewpoints.
- COVID vaccinations are not 100% harmless but they generate much more good than harm.
- They are certainly far less dangerous than the disease.
- COVID infections are not ‘just a flu’ but have serious consequences.
The last point was well-documented in a recent Lancet paper. Here is its abstract in full
Mortality statistics are fundamental to public health decision making. Mortality varies by time and location, and its measurement is affected by well known biases that have been exacerbated during the COVID-19 pandemic. This paper aims to estimate excess mortality from the COVID-19 pandemic in 191 countries and territories, and 252 subnational units for selected countries, from Jan 1, 2020, to Dec 31, 2021.
Methods
All-cause mortality reports were collected for 74 countries and territories and 266 subnational locations (including 31 locations in low-income and middle-income countries) that had reported either weekly or monthly deaths from all causes during the pandemic in 2020 and 2021, and for up to 11 year previously. In addition, we obtained excess mortality data for 12 states in India. Excess mortality over time was calculated as observed mortality, after excluding data from periods affected by late registration and anomalies such as heat waves, minus expected mortality. Six models were used to estimate expected mortality; final estimates of expected mortality were based on an ensemble of these models. Ensemble weights were based on root mean squared errors derived from an out-of-sample predictive validity test. As mortality records are incomplete worldwide, we built a statistical model that predicted the excess mortality rate for locations and periods where all-cause mortality data were not available. We used least absolute shrinkage and selection operator (LASSO) regression as a variable selection mechanism and selected 15 covariates, including both covariates pertaining to the COVID-19 pandemic, such as seroprevalence, and to background population health metrics, such as the Healthcare Access and Quality Index, with direction of effects on excess mortality concordant with a meta-analysis by the US Centers for Disease Control and Prevention. With the selected best model, we ran a prediction process using 100 draws for each covariate and 100 draws of estimated coefficients and residuals, estimated from the regressions run at the draw level using draw-level input data on both excess mortality and covariates. Mean values and 95% uncertainty intervals were then generated at national, regional, and global levels. Out-of-sample predictive validity testing was done on the basis of our final model specification.
Findings
Although reported COVID-19 deaths between Jan 1, 2020, and Dec 31, 2021, totalled 5·94 million worldwide, we estimate that 18·2 million (95% uncertainty interval 17·1–19·6) people died worldwide because of the COVID-19 pandemic (as measured by excess mortality) over that period. The global all-age rate of excess mortality due to the COVID-19 pandemic was 120·3 deaths (113·1–129·3) per 100 000 of the population, and excess mortality rate exceeded 300 deaths per 100 000 of the population in 21 countries. The number of excess deaths due to COVID-19 was largest in the regions of south Asia, north Africa and the Middle East, and eastern Europe. At the country level, the highest numbers of cumulative excess deaths due to COVID-19 were estimated in India (4·07 million [3·71–4·36]), the USA (1·13 million [1·08–1·18]), Russia (1·07 million [1·06–1·08]), Mexico (798 000 [741 000–867 000]), Brazil (792 000 [730 000–847 000]), Indonesia (736 000 [594 000–955 000]), and Pakistan (664 000 [498 000–847 000]). Among these countries, the excess mortality rate was highest in Russia (374·6 deaths [369·7–378·4] per 100 000) and Mexico (325·1 [301·6–353·3] per 100 000), and was similar in Brazil (186·9 [172·2–199·8] per 100 000) and the USA (179·3 [170·7–187·5] per 100 000).
Interpretation
The full impact of the pandemic has been much greater than what is indicated by reported deaths due to COVID-19 alone. Strengthening death registration systems around the world, long understood to be crucial to global public health strategy, is necessary for improved monitoring of this pandemic and future pandemics. In addition, further research is warranted to help distinguish the proportion of excess mortality that was directly caused by SARS-CoV-2 infection and the changes in causes of death as an indirect consequence of the pandemic.
I am posting this in the hope that the many proponents of so-called alternative medicine (SCAM) who deny proven facts about COVID might learn and stop falling victim to proctophasia.
On Amazon, someone commented as follows on my biography of Prince Charles:
… Dr. Ernst goes on digressions that mostly seem intended to make Prince Charles look bad. There’s a long chapter on Laurens van der Post, who influenced Prince Charles as a youth, and a lot about somewhat unsavory things he did. So what? …
This made me think. I read the chapter again and find it hard to agree with the comment. To me, this chapter is a short (~2000 words) and essential part of the book. Judge for yourself; here are a few excerpts from it: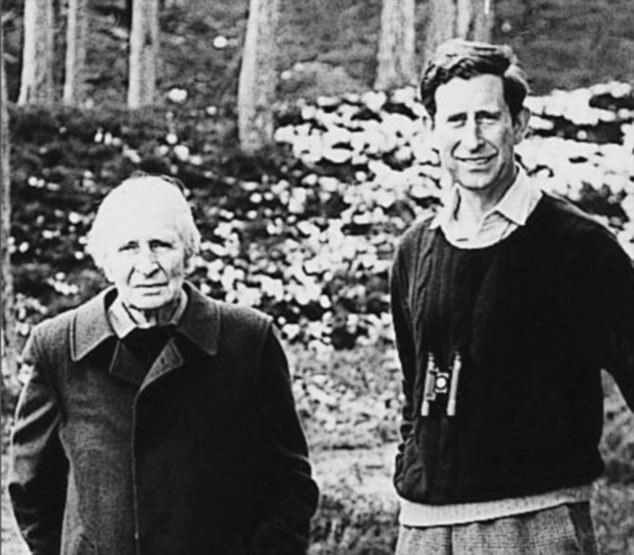
“It seemed to have been a union of mutual needs, between a Prince longing to find meaning in his existence and a storyteller who could weave apparent answers out of thin air.” Laurence van der Post was oozing charm and charisma and sensed that “for the Prince, there was a missing dimension”, as Jonathan Dimbleby put it. By 1975, the two men had formed such a close rapport that van der Post felt able to counsel him about spiritual matters, urging him to explore the ‘old world of the spirit’ and ‘the inward way’ towards truth and understanding. Van der Post suggested the two make a seven week journey into the Kalahari desert. This, he believed, would introduce Charles to the spirit world. Preparations were made in 1977 but, in the end, the plan had to be abandoned. Instead, the two later went to Kenya where they spent 5 days of long walks and “intense conversation”.
Van der Post urged Charles to play “a dynamic and as yet unimagined role to suit the future shape of a fundamentally reappraised and renewed modern society”, a reappraisal that would be “so widespread and go so deep that it will involve a prolonged fight for all that is good and creative in the human imagination.” An aspect of this fight, he claimed, would be “to restore the human being to a lost natural aspect of his own spirit; to restore his relevance for life and his love of nature, and to draw closer to the original blueprint and plan of life…”
Laurence left an interview for posthumous publication; in it, he expressed his hope that Charles would never become king, as this would imprison him, it would be more important that Charles continues to be a great prince. “He’s been brought up in a terrible way … He’s a natural Renaissance man, a man who believes in the wholeness and totality of life … Why should it be that if you try to contemplate your natural self that you should be thought to be peculiar?”
“For 20 years they had most intimate conversations and correspondence … with a steady flow of reassurance and encouragement, political and diplomatic advice, memoranda, draft speeches and guidance for reading”. Van der Post introduced Charles to the teachings of Carl Jung and his concept of the ‘collective unconscious’ that binds all humans together regardless whether they are Kalahari bushmen or princes. On the behest of van der Post, Charles began to record his dreams which van der Post then interpreted according to Jung’s theories. In the late 1970s van der Post tried to convince Charles to give up all his duties and withdraw from the world completely in search for an ‘inner world truth’. This plan too was aborted.
All biographers agree that van der Post was the strongest intellectual influence of Charles’ life.
- Charles sought van der Post’s advice and spiritual guidance on numerous occasions.
- When William was born, he made van der Post his godfather.
- When Charles’ marriage to Diana ran into difficulties, the couple was counselled by van der Post.
- Charles invited Laurence regularly to Highgrove, Sandringham and Balmoral.
- Charles visited van der Post on his deathbed.
- After Laurence’s death, Charles created a series of annual lectures hosted in van der Post’s memory which he hosted in St James’ Palace.
…
…
…
Charles’ notions about medicine were unquestionably inspired by van der Post. Laurence. He, for instance, bemoaned the inadequacy of conventional medicine and wrote: “Even if doctors did … use dreams and their decoding as an essential part of their diagnostic equipment and perhaps could confront cancer at the point of entry, how are they to turn it aside, unless they are humble enough to keep their instruments in their cases and look for some new form of navigation over an uncharted sea of the human spirit?” As we will see in the next chapters, van der Post’s influence shines through in many of Charles’ speeches. Moreover, it contributed to the attitude of many critical observers towards Charles. Christopher Hitchens is but one example for many:
“We have known for a long time that Prince Charles’ empty sails are so rigged as to be swelled by any passing waft or breeze of crankiness and cant. He fell for the fake anthropologist Laurens van der Post. He was bowled over by the charms of homeopathic medicine. He has been believably reported as saying that plants do better if you talk to them in a soothing and encouraging way… The heir to the throne seems to possess the ability to surround himself—perhaps by some mysterious ultramagnetic force?—with every moon-faced spoon-bender, shrub-flatterer, and water-diviner within range.”
The following chapters will show that Hitchens might not have been far off the mark.
___________________________
Yes, I do feel that the chapter is essential for the book. It explains how Charles’ love affair with alternative medicine got started and why it would become so intense and durable. Without it, the reader would not be able to understand the rest of the book. Moreover, it is important to demonstrate that van der Post was a charlatan and an accomplished liar. This is relevant because, in later life, Charles’ skill to choose adequate advisors was often wanting.
Now that the first reviews of, and numerous comments on my new book are in, I thought I bring my readers up to date and perhaps contribute to some fun. My favorite quote comes from a comment on Harriett Hall’s review: “Nothing much new here about Chucky Windsor’s credulity…”
Perhaps I shouldn’t, but I think it is funny and thus I chose it as the title of this post. Apart from being funny, it also has a more serious background. Virtually everyone who contacted me and gave me feedback said that they knew about Charles’ advocacy of alternative medicine. So, the ‘nothing much new’ comment is apt. Yet, they all added that, before reading my book, they had no idea how deeply Charles was involved and how profoundly anti-scientific and irrational his thinking seems to be in this area. Jonathan Stea, for instance, tweeted: “I just finished reading it—review coming soon. Excellent book. I didn’t realize Prince Charles was so stubbornly in love with pseudoscience and trying to promote it for decades under the guise of alternative/integrative medicine.”
Another comment was made on my own blog: “I am an avid consumer of this and other science blogs, books, podcasts and any other media I encounter. One of my earliest exposures was your book Trick or Treat, which I credit with greatly expanding my knowledge of a subject I had dabbled in but had begun to question. I deplore the PoW’s promotion of quackery. I am American and have no dog in the value of Royalty debate. BUT, I don’t see the need to use such a deeply unflattering (and possibly photoshopped) photo of the PoW. I do not think that such a decision is in line with your list of “nots”, and I think it hinders the impact it might otherwise have on fence-sitters. It disappoints me and while I have purchased multiple copies of many of your books to pass on to friends, family, and believers, I will pass on this one.” The photo is perhaps not flattering but there a many out there that are even worse. In any case, it is the publisher who decides on the title page. In the present case, I merely asked them to make my name on the title page a little less prominent than it was on the draft.
And then there were people who emailed me directly, as this medical colleague:
Dear Dr Ernst,
as a GP and ex oral surgeon from a world famous medical school(Edinburgh), also an experienced alternative practitioner,with 51 years in NHS, more than your own clinical exposure, I’m saddened by sponsored? skewed assaults on healing modalities maybe also representing a threat to financial paradigms: I absolved myself of scientific trials “for profit only”, in deference to holistic patient care, & the Hippocratic Oath
In a similar vein, Dr. Larry Malerba, a US homeopath, posted this comment on a Medscape interview with me:
Fortunately, the book reviews were more intelligent. They confirm what I mentioned above: reviewers were amazed at the depth of Charles’ irrationality. Harriett Hall expressed it as follows: “Charles’ efforts to promote alternative medicine have been mentioned many times on SBM, but readers may not appreciate the depth of his folly. I know I didn’t, until I read this book. The full story has never been told until now.” And Paul Benedetti wrote: “In short, readable chapters, Ernst unblinkingly presents how Charles has written books and articles promoting alternative medicine and spearheaded organizations, colleges, and foundations, giving full-throated support to one unproven, often bizarre, alternative health cure after another.”
One of the nicest pieces of praise came from someone who posted this comment on Amazon:
This is a revelatory critique of where vague well-intentioned but ill-informed health ideas promoted by a powerful person do or don’t get us.
Professor Ernst’s explanations are admirably clear – and no-one is more qualified than he to write on this topic. It’s difficult to imagine a more devastating comment on the bad conseqeunces of ill-informed ideas and actions, than that found in the last two paragraphs on Page 88.
There is a great deal of valuable information here on ‘alternative medicine’ approaches, in addition to the explanations of HRH Prince Charles’ involvement with them. A most worthwhile book for anyone wanting to find out more about alternative/complementary treatment modalities.
Yes, publishing a book can be a mixed blessing. The author works tirelessly for many months (for next to no pay) only to get aggressed – not for factual errors (that would be perfectly alright) or unfounded arguments (that would be welcome) but for allegedly being in it for the money or producing ‘prejudicial propaganda’. In the case of the new book, this had to be expected. I hesitated for an entire decade writing it (hoping someone else would tackle the task) because I knew that it would be far from straightforward to criticize the future king of one’s own country.
All the more reason to take this occasion and thank those who stand by me, who find my book relevant, who agree that it is instructive, and who feel that it deserves a wide readership.
THANK YOU
Since about two years, I am regularly trying to warn people of charlatans of all types who mislead the public on COVID-related subjects. In this context, a recent paper in JAMA is noteworthy. Allow me to quote just a few passages from it:
COVID-19 misinformation and disinformation flood the public discourse; physicians are not the only source. But their words and actions “may well be the most egregious of all because they undermine the trust at the center of the patient-physician relationship, and because they are directly responsible for people’s health,” Pawleys Island, South Carolina, family medicine physician Gerald E. Harmon, MD, president of the American Medical Association (AMA), (which publishes JAMA), wrote recently. In November, the AMA House of Delegates adopted a new policy to counteract disinformation by health care professionals.
… Few physicians have been disciplined so far, even though the Federation of State Medical Boards (FSMB), representing the state and territorial boards that license and discipline physicians, and, in some cases, other health care professionals, and the American Board of Medical Specialties (ABMS), consisting of the boards that determine whether physicians can be board-certified, have issued statements cautioning against spreading false COVID-19 claims.
In July 2021, the FSMB warned that spreading COVID-19 misinformation could put a physician’s license at risk. The organization said it was responding “to a dramatic increase in the dissemination of COVID-19 vaccine misinformation and disinformation by physicians and other health care professionals.”
The ABMS released a statement in September 2021. “The spread of misinformation and the misapplication of medical science by physicians and other medical professionals is especially harmful as it threatens the health and well being of our communities and at the same time undermines public trust in the profession and established best practices in care,” the ABMS said.
In an annual survey of its 70 member boards conducted in fall 2021, the FSMB asked about complaints and disciplinary actions related to COVID-19. Of the 58 boards that responded, 67% said they had seen an uptick in complaints about licensees spreading false or misleading COVID-19 misinformation, according to results released in December 2021. But only 12 (21%) of the 58 boards said they’d taken disciplinary action against a physician for that reason…
- What percentage of lay-homeopaths misinform their patients?
- What percentage of chiropractors misinform their patients?
- What percentage of energy healers misinform their patients?
- What percentage of naturopaths misinform their patients?
- What percentage of acupuncturists misinform their patients?
- etc., etc.
As the total number of SCAM practitioners might, in some parts of the world, easily outnumber doctors, these questions are highly relevant. Yet, I am not aware of any reliable data on these issues. Judging from what I have observed (and written about) during the pandemic, I guess that the percentages are likely to be substantial and way higher than those for doctors. To me, this suggests that we ought to focus much more on SCAM practitioners if, in future health crises, we want to prevent the confusion and harm that misinformation inevitably causes.

Medscape and Ernst deserve each other. What a sad old fellow, desperate to live down his homeopathic past by producing a steady stream of deeply prejudicial anti-homeopathy propaganda. What kind of person dedicates his life to hate speech against the second most popular medical therapy worldwide? No doubt, he’s convinced himself that it’s a noble endeavor. Sad and comical.