critical thinking
It has been reported that the Regional Court of Dortmund has prohibited the manufacturer of the homeopathic cold remedy Meditonsin from advertising with false health claims. The court did not see sufficient evidence for the advertising claims.
The Consumer Advice Centre (VZ) of North Rhine-Westphalia issued a warning to the Meditonsin manufacturer (MEDICE Arzneimittel Pütter GmbH & Co.) for misleading advertising statements and sued them. The complaint was:
- that the advertising gave the false impression that an improvement in health could be expected with certainty after taking the product,
- that no side effects were to be expected,
- that the product was superior to “chemical-synthetic medicines”.
The Dortmund Regional Court was not convinced by a study referred to by the manufacturer. On its website, the manufacturer of Meditonsin presents the results of a “current, large-scale user study with more than 1,000 patients” under the heading “Proven efficacy & tolerability”. According to a pie chart, 90% of the patients were satisfied or very satisfied with the effect of Meditonsin.
However, according to the VZ, the study was only a “pharmacy-based observational study” with little scientific validity. Despite the lack of evidence, the manufacturer claimed that “the good efficacy and tolerability of Meditonsin® Drops could once again be impressively confirmed”. The Dortmund Regional Court, however, followed the VZ’s statement of grounds for action. “It is not allowed to advertise with statements that give the false impression that a successful treatment can be expected with certainty, as the advertisement for Meditonsin drops suggests,” emphasized Gesa Schölgens, head of “Faktencheck Gesundheitswerbung”, a joint project of the consumer centres of North Rhine-Westphalia and Rhineland-Palatinate. According to the Therapeutic Products Advertising Act, this is prohibited.
The Dortmund Regional Court also found that consumers were misled by the advertising because it gave a false impression that no harmful side effects were to be expected when taking Meditonsin. The package leaflet of the drug listed several side effects. According to this, there could even be an initial worsening of the symptoms after taking the medicine.
According to the VZ, the alleged advantage of the “natural medicinal product” over “many chemical-synthetic medicinal products that only suppress the symptoms”, as presented by the manufacturer, is also inadmissible. This is because it is not permissible to advertise to consumers with claims that the effect is equivalent or superior to that of another medicinal product. This, too, was confirmed by the court.
_________________________
In case you like to know more about the remedy, this is from its English language site:
Meditonsin consists of Aconitum, Atropinum Sulfuricum, Mercurius Cyanatus. Active ingredient is the part of the drug or medicine which is biologically active. This portion of the drug is responsible for the main action of the drug which is intended to cure or reduce the symptom or disease.
Quackery is rife in India. On this blog, I have occasionally reported on this situation, e.g.:
- The new ‘WHO Global Centre for Traditional Medicine’ in India
- Mucormycosis (black fungus): is the Indian AYUSH ministry trying to decimate the population?
- Homeopathy, COVID, India and Prince Charles: not a good mixture!
- Has homeopathy caused the dramatic decline of COVID-19 cases in India?
- Homeopathy research from India is far from trustworthy, and today I can show you why
- Brazil and India collaborate in the promotion of quackery
- Taking the piss again? The story of urine therapy in India
- The intriguing case of homeopathy in India
- Prince Charles’ advocacy of quackery is by no means harmless
- Patient Dies After Homeopath Gives Wrong Injection
- Herbal remedies are good for you … except for the ones that injure your liver
- The ‘AYUSH COVID-19 Helpline’: have they gone bonkers?
Now the Chief Justice of India (CJI) NV Ramana has pointed out that legislation needs to be brought in to save people “from falling prey to fraudulent practices in the name of treatment”. Speaking at the inaugural National Academy of Medical Sciences on ‘Law and Medicine’, the CJI said: “Quackery is the biggest disease affecting India” and that hospitals are “being run like companies, where profit-making is more important than service to society”. The CJI added, “another side of lack of accessible healthcare is giving space to quacks. Quackery begins where awareness ends. Where there is room for myths, there is room for quackery”. He continued, “Owing to the financial and time constraints, a huge majority of the Indian population approaches these untrained and uncertified doctors. Lack of awareness and knowledge, misplaced belief, and sheer inaccessibility have massive ramifications on the health of the country, particularly the rural and underprivileged Indian … The need of the hour is to bring in legislation to save people from falling prey to fraudulent practices in the name of treatment … Private hospitals are being opened at an exponential rate. This is not necessarily a bad thing, but there is a glaring need for balance. We are seeing hospitals being run like companies, where profit-making is more important than service to society.”
I am sure the CJI is correct; India does have a quackery problem. If nothing else, the fact that one website lists a total of 746 Alternative Medicine Colleges in India, leaves little doubt about it.
It has been reported that America’s Frontline Doctors (a right-wing organization that is associated with the ‘Tea Party’) is suing one of its founders in a battle for control over the controversial group, which gained national notoriety for spreading misinformation about COVID-19 treatments and vaccines during the pandemic.
The organization and its current board chairman have sued Simone Gold, MD, alleging that she misused the nonprofit organization’s funds to buy a $3.6 million Florida mansion, purchase a Mercedes-Benz and other luxury vehicles, and take trips on private planes.
The lawsuit, filed November 4 in federal court, comes just months after Gold was released from prison for her role in the January 6 US Capitol insurrection. Gold pleaded guilty to trespassing in the Capitol and was sentenced to 60 days in federal prison.
The group and the board chairman, Joseph Gilbert, claim that after her release from prison, Gold attempted to reassert control of the group, take over its website, and fraudulently represent herself as its director, according to the complaint. The complaint referred to Gold as a “rogue founder,” alleging that she spent almost $50,000 monthly on personal expenses using the organization’s credit cards.
Gold resigned from the group’s board in February ― before she pled guilty ― so that she could pursue her goal of opening health and wellness centers nationwide, according to the complaint. At that time, the board voted Gilbert to be its chairman and agreed to have Gilbert negotiate an agreement for Gold to serve as a consultant. Gold sought a “signing bonus” of $1.5 million, along with $50,000 to be paid monthly as a consulting fee, according to the complaint.
Another report has more details on Gold’s alleged wrong-doing: The complaint claims that in November 2021, Gold used “AFLDS charitable funds to purchase a $3.6 million home in Naples, Florida for her personal rent-free use, and at least three vehicles and has otherwise used AFLDS funds to resource her personal lifestyle and expenses since she formed AFLDS.” Plaintiffs also allege that Gold “currently lives in this home with John Strand, rent free.” Strand is a former underwear model and boyfriend of Gold’s who was arrested with her in connection with the January 6, 2021 insurrection in the U.S. Capitol. She moved with Strand to Florida this year from Los Angeles, where she had been an emergency room physician. Strand allegedly was paid $10,000 per month as an AFLDS employee and allegedly spent $15,000 to $17,000 a month using those credit cards. He was terminated from AFLDS in summer 2022, according to the complaint. In addition to purchasing the house with AFLDS funds, the complaint said Gold purchased a Mercedes Benz Sprinter van, a Hyundai Genesis, and a GMC Denali. After taking possession of the Naples home, she used AFLDS funds to pay a personal security officer $12,000, a personal housekeeper $5,600 a month, and charged “nearly $50,000 per month” to AFLDS credit cards.
I tried to find some information on th health and wellness centers that Simone Gold wanted or did open. Alas I was unsuccessful in my endeavor. However, I found an interesting passage she once wrote:
The World Health Organization, the FDA, the NIH, and the CDC are proven liars who have lost all credibility and common-sense, while jeopardizing YOUR health and safety. What disgusts me most is how their failed prescriptions have exposed the most vulnerable: our elderly and our children. The New York Times, CNN, NPR, and hundreds of other news outlets have censored the truth in order to preserve their power. Twitter, Facebook, Google/YouTube, Apple, and dozens of other Tech companies are throttling down content, suppressing information, and de-platforming those with whom they disagree.
I find it hard to find words for a comment – except perhaps this: maybe it is not such a bad thing when anti-vaxxers fight each other; it means they have less time, energy, and money to confuse the public with their lies.
A review conducted in 2015 reported community pharmacists are willing to adopt a professional role in counselling consumers about the appropriate and safe use of so-called alternative medicine (SCAM) but faced multiple barriers in doing so. This current review aimed to update and extend these findings, by identifying studies published since 2015 that reported on pharmacists across any setting.
Eligible studies published between January 01, 2016, and December 31, 2021, were identified across 6 databases (PubMed, Scopus, Web of Science, EMBASE, ScienceDirect and MEDLINE). A grounded theory approach was used to thematically synthesize the data extracted.
A total of 64studies representing pharmacists across 30 countries were included for review. The study designs varied and included:
- cross-sectional surveys (n = 36),
- qualitative studies (n = 14),
- pseudo-patient studies (n = 3).
Eight studies reported on practice and/or bioethical responsibilities and 19 studies documented factors that would enable pharmacists to fulfill these responsibilities, while 37 studies reported on both.
The authors concluded that these findings indicate research about pharmacists’ responsibilities associated with SCAM is evolving from gap analysis towards research that is proactive in advocating for change in multiple areas. These findings can be used to inform a consensus discussion among pharmacists and key stakeholders regarding a set of professional responsibilities that would serve in the development of: a clearly defined role and associated practice standards, and competency requirements that inform educational learning objectives for inclusion in undergraduate, post-graduate and continuing professional pharmacy education.
I am puzzled why so many researchers in this specific area seem to avoid clearer language plainly stating the essential, simple, and undeniable facts. I am equally puzzled why so few pharmacists speak out.
It is obvious that community pharmacists are firstly healthcare professionals and only secondly shopkeepers. As such, they have important professional and ethical duties. Foremost, they are obliged to inform their customers responsibly – and responsible means telling them about the evidence for or against the SCAM product they are about to purchase. This duty also entails that pharmacists must inform themselves about the best current evidence. In turn, this means they must stop tolerating the current plethora of under- or post-graduate SCAM courses that are not evidence-based.
As we have discussed ad nauseam on this blog, none of this is actually happening (except in very few laudable cases)!
By and large, pharmacists continue to go along with the double standards of a) evidence for conventional drugs and b) fairy tales for SCAM. In the interest of progress, patient safety, and public health, it is time that pharmacists wake up and remind themselves that they are not commercially orientated shopkeepers but ethical healthcare professionals.
In recent weeks, I have been thinking a lot about ‘INTEGRATIVE MEDICINE‘. Skeptics mostly see it as a way of smuggling quackery into conventional healthcare. This is undoubtedly true and important. But it occurred to me that there also is a somewhat different perspective that has so far been neglected. Let me try to explain by recounting a story. It is fictive, of course, but the fiction is based on the observation of many cases during previous decades.
The story is about a doctor – let’s call him George – who, to be frank, is not the most gifted of his colleagues. Already at medical school, he was not as dedicated as his teachers would have hoped. In fact, medicine had not been his first choice at all. Yet he ended up as a general practitioner and eventually became a partner in a practice with 5 GPs.
Over the years, it became clear that George lacked something to be a good doctor. He knew his stuff, alright, got most of the diagnoses correct, and made not too many mistakes. But something was not quite right. One could say that, relative to his colleagues, he lacked kindness, dedication, compassion, and empathy. He often found it unnecessary to respect his patients. Sometimes, he even joked about them and about what he perceived as their stupidity.
If we view medicine as being both a science and an art, one might conclude that George was just about alright with the science but notably deficient in the art of healthcare. Most of his patients were aware that something was amiss; many even avoided him and tried to consult one of his colleagues instead. On more than one occasion, patients had told George that they were disappointed with his attitude. Some had even told him to the face that he lacked kindness. Such conversations made George think. He had to admit to himself that his colleagues were better at building good relationships with their patients. Eventually, George decided that something ought to change.
As it happened, George’s wife had a friend who was a Reiki healer. One day, he asked the healer – let’s call her Liz – whether she would like to try working alongside the GPs in his practice. Liz was delighted and accepted. George did not believe for a minute that Reiki was more than hocus-pocus, but he knew that Liz was kind and had loads of the compassion that he was so obviously lacking.
Hence force George and Liz formed a team: George looked after his patients the best he could and whenever he felt that more empathy and compassion were required, he would send the patient to Liz. This partnership changed everything. The patients were content, George was happy, and Liz was beaming.
As some patients frowned at the idea of Reiki, George soon recruited an aromatherapist as well. After that, a lay homeopath and a reflexologist were employed. George’s GP partners (who made little use of the alternative practitioners) were sure that none of these therapies had any specific effects (incidentally, a belief not shared by the practitioners in question who felt they were doing wonders). But for George, the therapists clearly did supplement his limited interpersonal skills. Patients were delighted and the GP practice began to thrive. As for George, he became an increasingly outspoken and prominent advocate of INTEGRATED MEDICINE. The fact that there was no evidence to support it did hardly matter to him; what counted was that it rendered his own incompetence less visible.
About a year later, George convinced his slightly bewildered partners to rename their practice ‘THE INTEGRATIVE HEALTH CENTRE’.
End of story
In case you did not get my point, let me make it more bluntly: INTEGRATIVE MEDICINE can be a way for some doctors to delegate the art of medicine to quacks. Good doctors don’t need to do this because they are able to show compassion and treat their patients as whole human beings. Less gifted doctors, however, find INTEGRATIVE MEDICINE a practical solution to their own incompetence.
So, is INTEGRATIVE MEDICINE a good compromise then?
No, certainly not!
The last thing we need in healthcare is for doctors to start delegating the art of medicine to others. It would be a serious mistake, nothing less than abandoning the core values of medicine to charlatans.
But what is the solution?
Obviously, it is to make sure all doctors are competent. We need to select medical students adequately, tell them much more about the importance of kindness, compassion, empathy, holism, etc., and teach them how to show and use these qualities. We need to train doctors to be competent in both the science and the art of medicine. This has to begin in medical school and must continue throughout their professional career. We need to make sure that doctors like George understand the message; if they prove to be unable to do so, we should direct them to professions where compassion is not essential.
The worst solution we can possibly envisage is to allow charlatans to cover up the incompetence of people like George and call it INTEGRATED MEDICINE.
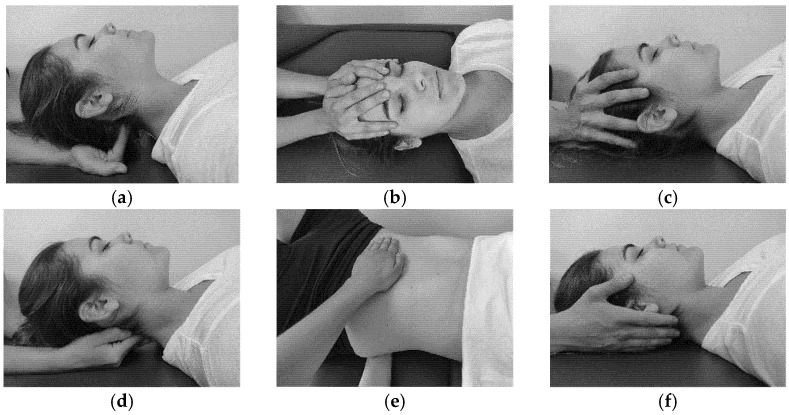
The aim of this study was to evaluate the effectiveness of craniosacral therapy on different features in migraine patients.
Fifty individuals with migraine were randomly divided into two groups (n = 25 per group):
- craniosacral therapy group (CTG),
- sham control group (SCG).
The interventions were carried out with the patient in the supine position. The CTG received a manual therapy treatment focused on the craniosacral region including five techniques, and the SCG received a hands-on placebo intervention. After the intervention, individuals remained supine with a neutral neck and head position for 10 min, to relax and diminish tension after treatment. The techniques were executed by the same experienced physiotherapist in both groups.
The analyzed variables were pain, migraine severity, and frequency of episodes, functional, emotional, and overall disability, medication intake, and self-reported perceived changes, at baseline, after a 4-week intervention, and at an 8-week follow-up.
After the intervention, the CTG significantly reduced pain (p = 0.01), frequency of episodes (p = 0.001), functional (p = 0.001) and overall disability (p = 0.02), and medication intake (p = 0.01), as well as led to a significantly higher self-reported perception of change (p = 0.01), when compared to SCG. The results were maintained at follow-up evaluation in all variables.
The authors concluded that a protocol based on craniosacral therapy is effective in improving pain, frequency of episodes, functional and overall disability, and medication intake in migraineurs. This protocol may be considered as a therapeutic approach in migraine patients.
Sorry, but I disagree!
And I have several reasons for it:
- The study was far too small for such strong conclusions.
- For considering any treatment as a therapeutic approach in migraine patients, we would need at least one independent replication.
- There is no plausible rationale for craniosacral therapy to work for migraine.
- The blinding of patients was not checked, and it is likely that some patients knew what group they belonged to.
- There could have been a considerable influence of the non-blinded therapists on the outcomes.
- There was a near-total absence of a placebo response in the control group.
Altogether, the findings seem far too good to be true.
I just got this email with sad news: Ken Frazier “died peacefully this morning, three weeks after being diagnosed with acute myeloid leukemia. Judy and I were fortunate to spend time with Ken and Ruth last week and tell Ken personally how much he has meant to us over our entire lives.”
Ken was a part of CFI history quite literally from Day One. In May 1976, writing for Science News, Ken reported on the formation of the Committee for the Scientific Investigation of Claims of the Paranormal (CSICOP). In 1977, Ken joined CSICOP to serve as editor of The Zetetic, which became Skeptical Inquirer in 1978. He held that position ever since, spending the better part of five decades defining and steering the work of the skeptical community in combatting disinformation and pseudoscience. Ken has also published numerous papers and books, e.g.:
Ken’s book Science Under Siege: Defending Science, Exposing Pseudoscience was featured by Science News for its “engaging, insightful, and often surprising essays by researchers and journalists” about “what science is and is not, and what happens when the facts get twisted.” And he was working on yet another book; only a few months ago he wrote to me taking me for help with it:
… I am completing [ a book] on science and pseudoscience, titled Shadows of Science. It was just accepted by Prometheus Books for publication in Fall 2023. I am now working on a final chapter on “Pseudomedicine,” pseudoscience in medicine. This is not my area of expertise so I am relying on many medical professionals who have investigated and written about medical pseudoscience, most prominently you.
My chapter is mainly concerned with broad points and principles in identifying and describing pseudoscience in medicine — SCAM.
I merely ask if you mind if I quote from and paraphrase from a number of your writings—all with full credit to you in the text itself in addition to in the bibliography
I have always been particularly impressed with the Introduction to your So-Called Alternative Medicine (SCAM) for Cancer as well as parts of your earlier book SCAM: So-Called Alternative Medicine (which carries my testimonial to you on the back cover!). This includes your definition of SCAM and your list of popular therapies and perhaps some of your common assumptions about SCAM. I also would love to draw upon some of the information in your boxes in the opening parts of SCAM…
Ken has on many occasions been most helpful and kind to me, and it goes without saying that I was delighted to assist.
He was a giant amongst the US skeptics, and we will all miss him badly.
This study described osteopathic practise activity, scope of practice and the osteopathic patient profile in order to understand the role osteopathy plays within the United Kingdom’s (UK) health system a decade after the authors’ previous survey.
The researchers used a retrospective questionnaire survey design to ask about osteopathic practice and audit patient case notes. All UK-registered osteopaths were invited to participate in the survey. The survey was conducted using a web-based system. Each participating osteopath was asked about themselves, and their practice and asked to randomly select and extract data from up to 8 random new patient health records during 2018. All patient-related data were anonymized.
The survey response rate was 500 osteopaths (9.4% of the profession) who provided information about 395 patients and 2,215 consultations. Most osteopaths were:
- self-employed (81.1%; 344/424 responses),
- working alone either exclusively or often (63.9%; 237/371),
- able to offer 48.6% of patients an appointment within 3 days (184/379).
Patient ages ranged from 1 month to 96 years (mean 44.7 years, Std Dev. 21.5), of these 58.4% (227/389) were female. Infants <1 years old represented 4.8% (18/379) of patients. The majority of patients presented with musculoskeletal complaints (81.0%; 306/378) followed by pediatric conditions (5%). Persistent complaints (present for more than 12 weeks before the appointment) were the most common (67.9%; 256/377) and 41.7% (156/374) of patients had co-existing medical conditions.
The most common treatment approaches used at the first appointment were:
- soft-tissue techniques (73.9%; 292/395),
- articulatory techniques (69.4%; 274/395),
- high-velocity low-amplitude thrust (34.4%; 136/395),
- cranial techniques (23%).
The mean number of treatments per patient was 7 (mode 4). Osteopaths’ referral to other healthcare practitioners amounted to:
- GPs 29%
- Other complementary therapists 21%
- Other osteopaths 18%
The authors concluded that osteopaths predominantly provide care of musculoskeletal conditions, typically in private practice. To better understand the role of osteopathy in UK health service delivery, the profession needs to do more research with patients in order to understand their needs and their expected outcomes of care, and for this to inform osteopathic practice and education.
What can we conclude from a survey that has a 9% response rate?
Nothing!
If I ignore this fact, do I find anything of interest here?
Not a lot!
Perhaps just three points:
- Osteopaths use high-velocity low-amplitude thrusts, the type of manipulation that has most frequently been associated with serious complications, too frequently.
- They also employ cranial osteopathy, which is probably the least plausible technique in their repertoire, too often.
- They refer patients too frequently to other SCAM practitioners and too rarely to GPs.
To come back to the question asked in the title of this post: What do UK osteopaths do? My answer is
ALMOST NOTHING THAT MIGHT BE USEFUL.
Camilla spent ten days at the end of October in a sophisticated meditation and fitness center in southern India. Life has recently been hectic for the Queen Consort: at 75, she has been in a non-stop succession of various ceremonies for the funeral of Elizabeth II, always one step behind her husband, not to mention her new status as sovereign… Enough to block her chakras in no time.
She came to the resort with her bodyguards and a handful of friends and was able to take advantage of the tailor-made treatments concocted for her by the master of the house, Dr Issac Mathai, who created this high-end holistic centre on a dozen hectares of scented gardens near Bangalore. The program includes massages, herbal steam baths, yoga, naturopathy, homeopathy, meditation, and Ayurvedic treatments to “cleanse, de-stress, soothe and revitalize the mind, body and soul”, as the establishment’s website states.
Guests are required to follow an individualized, meat-free diet, with organic food from the resort’s vegetable gardens, based on lots of salads or soups – Camilla is said to be a fan of sweet corn soup with spinach. Cigarettes and mobile phones are not allowed, although it is assumed that Camilla must have some privileges due to her status… and the basic rate for the suites, which starts at $950 a night – the price of the rooms varies between $260 and $760, the rate including a consultation with the doctors.
Charles and Camilla have been fans of the Soukya Centre in India for a decade. The place corresponds in every way to their deep-rooted convictions about health. Like her husband, Camilla is a follower of organic food, she also practices yoga and treats her face with creams made from nettle and bee venom. For his part, Charles has long been an advocate of alternative medicine, homeopathy, acupuncture, aromatherapy, and also hypnosis… He even set up a foundation to support complementary medicine by lobbying the British health service to include it in complementary therapies for certain patients, which caused an uproar among the pundits of traditional medicine.
________________________
If you suspected I was (yet again) sarcastic about the royal couple, you are mistaken. The text above is only my (slightly shortened) translation of an article published in the French magazine LE POINT (even the title is theirs). I found the article amusing and interesting; so, I looked up the Indian health center. Here are some of the things I found:
The 1st impression is that they are not shy about promotion calling themselves THE WORLD’S BEST AYURVEDA TREATMENT CENTER. The doctor in charge was once a ‘Consultant Physician’ at the Hale Clinic in London, where he treated a number of high-profile people. As his professional background, he offers this:
M.D. (Homeopathy); Hahnemann Post-Graduate Institute of Homeopathy, London M.R.C.H, London; Chinese Pulse Diagnosis and Acupuncture, WHO Institute of Traditional Chinese Medicine, Nanjing, China; Trained (Mind-Body Medicine Programme) at Harvard Medical School, USA
The approach of the center is described as follows:
The fundamental principle underlying Holistic Treatment is that the natural defense and immune system of an individual when strengthened, has the potential to heal and prevent diseases. In the age of super-specialisation where human beings are often viewed as a conglomeration of organs, it is crucial to understand ourselves as multi-dimensional beings with a body, mind and spirit. These interconnected dimensions need to be in perfect harmony to ensure real well-being.
And about homeopathy, they claim this:
Homeopathy originated in 1796 in Germany, and was discovered by Dr. Samuel Hahnemann, a German scientist. Homeopathy is popular today as a non-intrusive, holistic system of medicine. Instead of different medicines for different parts of the body, one single constitutional remedy is prescribed. As a system of medicine, Homeopathy is highly scientific, safe, logical and an extremely effective method of healing. For over 200 years people have used Homeopathy to maintain their good health, and also to treat and cure a wide range of illnesses like allergies, metabolic disorders, atopic dermatitis, Rheumatoid arthritis, Auto-immune disorders.
At this stage, I felt I had seen enough. Yes, you are right, we did not learn a lot from this little exploration. No, hold on! We did learn that homeopathy is highly scientific, safe, logical, and extremely effective!
The question, however, is should we believe it?
Shiatsu is a Japanese form of so-called alternative medicine (SCAM) derived from Traditional Chinese Medicine using deep pressure on the paths of the postulated acupuncture meridians. Clinical observations on this topic are said to be encouraging, especially for the treatment of sleep and conduct disorders, but there is a lack of empirical data.
The objective of this study was to examine the possible therapeutic effects of shiatsu in a clinical population of children treated in child and adolescent psychiatry. It was designed as a qualitative descriptive and non-interventional study, conducted on children treated in day-care hospital units and outpatient clinical settings. Shiatsu was administered, at least during 3 sessions, to children with an autism spectrum disorder or other disorders according to ICD-11 criteria (such as conduct disorders with impulsivity or attention deficit).
The evaluation was performed by two independent researchers (a child psychiatrist and a psychologist who were not the caregivers) based on direct observation of children during the shiatsu sessions, combined with semi-structured non-inductive interviews with their parents, and data collected from focus groups conducted with the children’s caregivers. A phenomenological interpretive analysis (IPA) approach with Nvivo coding software was used to analyze the data.
Based on semi-structured interviews with 13 parents cross-referenced with data from 2 focus groups and direct observations of 7 children during 2 full shiatsu sessions for each observation, the results show that shiatsu has positive effects on
- internal tension (a relief effect, notably on aggressive behaviors directed against others or self),
- sleep (including improvement of sleep quality),
- social interaction,
- attention,
- verbalization of affects and traumatic memories of early childhood,
- perception of bodily limits.
As these children had several other treatments as well, it cannot be proved that the positive effects observed in this study are related specifically to shiatsu practice. Shiatsu may participate and facilitate the effects of other treatments. It is noteworthy that most of the children came willingly to the shiatsu sessions, ask their parents to repeat the shiatsu sessions at home, and indicate to the practitioner, from one session to the next, their elective body points where they wish to receive the application of shiatsu.
The authors concluded that the findings suggest therapeutic benefits of shiatsu, especially on externalize violence with a relief of aggressive behavior directed against others or self (knowing, moreover, that internal tension, sleep disorders and non-verbalization of affects or traumatic memories, all improved by shiatsu, are also all risk factors for externalize violence). These results highlight, therefore, the need to develop a daily practice of shiatsu in child and adolescent psychiatry. Further research is required to clarify the effects of shiatsu and ascertain better its underlying mechanisms based on this exploratory pilot study.
I do appreciate that, with a treatment that has not been submitted to many controlled clinical trials, researchers feel that they have to start from scratch, e.g. simple observations. However, they also must realize that their observations do not lend themselves to firm conclusions about the effects of the treatment. In the present case, the researchers do seem to be aware of this caveat but nevertheless make statements that go way beyond of what is warranted:
- the results show that shiatsu has positive effects on …
- Shiatsu may participate and facilitate the effects of other treatments
- the findings suggest therapeutic benefits of shiatsu, especially on externalize violence
- These results highlight, therefore, the need to develop a daily practice of shiatsu in child and adolescent psychiatry
I fear that these statements are not merely exaggerated but suspect they are also untrue. Testing them in properly controlled clinical trials would show whether my suspicion is correct. Meanwhile, I would like to remind
- researchers,
- reviewers,
- and journal editors
of their duty to be truthful and not mislead the public.