critical thinking
The Anglo-European College of Chiropractic (AECC) has been promoting pediatric chiropractic for some time, and I have posted about the subject before (see, for instance, here). Now the AECC has gone one decisive step further. On the website, the AECC announced an MSc ‘Musculoskeletal Paediatric Health‘:
The MSc Musculoskeletal Paediatric Health degree is designed to develop your knowledge and skills in the safe and competent care of children of all ages. Our part-time, distance-based course blends live online classes with ready to use resources through our virtual learning environment. In addition, you will have the opportunity to observe in the AECC University College clinical services at our Bournemouth campus. The course covers topics in paediatric musculoskeletal practice with specific units on paediatric development, paediatric musculoskeletal examination, paediatric musculoskeletal interventions, and paediatric musculoskeletal management. You will address issues such as risk factors and public health, including breastfeeding, supine sleep in infancy, physical activity in children and conditions affecting the musculoskeletal health of children from birth. The paediatric specific topics are completed by other optional units such as professional development, evidence-based practice, and leadership and inter-professional collaboration. In the dissertation unit you will conduct a study relevant to musculoskeletal paediatric health.
Your learning will happen through a mix of live and recorded lectures, access to online reading materials, and access to the literature through our learning services. You will also engage with the contents taught through guided activities with your peers and staff. Clinical paediatric experience is recommended to fully engage with the course. For students with limited access to a suitable clinical environment to support their studies, or for student who wants to add to their clinical experience, we are able to offer a limited number of opportunities to observe and work alongside our clinical educators within the AECC University College clinical services. Assessments are tailor made to each unit and may include a variety of methods such as critical reviews, reflective accounts, portfolios and in the last year a research dissertation.
___________________________
The AECC emphasizes its commitment to being a leading higher education institution in healthcare disciplines, nationally and internationally recognised for quality and excellence. Therefore, it seems only fair to have another look at the science behind pediatric chiropractic. Specifically, is there any good science to show that would justify a Master of Science in ‘Musculoskeletal Paediatric Health’?
So, let’s have a look and see whether there are any good review articles supporting such a degree. Here is what I found with several Medline searches (date of the review on chiropractic for any pediatric conditions, followed by its conclusion + link [so that the reader can look up the evidence]):
2008
I am unable to find convincing evidence for any of the above-named conditions.
2009
Previous research has shown that professional chiropractic organisations ‘make claims for the clinical art of chiropractic that are not currently available scientific evidence…’. The claim to effectively treat otitis seems to
be one of them. It is time now, I think, that chiropractors either produce the evidence or abandon the claim.
2009
The … evidence is neither complete nor, in my view, “substantial.”
2010
2018
What seems to emerge is rather disappointing:
- There are no really new reviews.
- Most of the existing reviews are not on musculoskeletal conditions.
- All of the reviews cast considerable doubt on the notion that chiropractors should go anywhere near children.
But perhaps I was too ambitious. Perhaps there are some new rigorous clinical trials of chiropractic for musculoskeletal conditions. A few further searches found this (again year and conclusion):
2019
2018
I might have missed one or two trials because I only conducted rather ‘rough and ready’ searches, but even if I did: would this amount to convincing evidence? Would it be good science?
No! and No!
So, why does the AECC offer a Master of Science in ‘Musculoskeletal Paediatric Health’?
Search me!
…
…
It wouldn’t have something to do with the notion that it is good for business?
Or perhaps they just want to give science a bad name?
Anyone who has been following this blog will have noticed that we have our very own ‘resident chiro’ who comments every single time I post about spinal manipulation/chiropractic/back pain. He uses (mostly?) the pseudonym ‘DC’. Recently, DC explained why he is such an avid poster of comments:
” I read and occasionally comment on this blog for two main reasons. 1. In my opinion Ernst doesn’t do a balance reporting on the papers his shares regarding spinal manipulation and chiropractic. Thus, I offer additional insight, a more balanced perspective for the readers. 2. There are a couple of skeptics who occasionally post that do a good job of analyzing papers or topics and they do so in a respectful manner. I enjoy reading their comments. I will add a third. 3. Ernst, from what I can tell, doesn’t censor people just because they have a different view.”
So, DC aims at offering additional insights and a more balanced perspective. That would certainly be laudable and welcome. Yet, over the years, I have gained a somewhat different impression. Almost invariably, my posts on the named subjects cast doubt on the notion that chiropractic generates more good than harm. This, of course, cannot be to the liking of chiropractors, who therefore try to undermine me and my arguments. In a way, that is fair enough.
DC, however, seems to have long pursued a very specific and slightly different strategy. He systematically attempts to distract from the evidence and arguments I present. He does that by throwing in the odd red herring or by deviating from the subject in some other way. Thus he hopes, I assume, to distract from the point that chiropractic fails to generate more good than harm. In other words, DC is a tireless (and often tiresome) fighter for the chiropractic cause and reputation.
To check whether my impression is correct, I went through the last 10 blogs on spinal manipulation/ chiropractic/ back pain. Here are my findings (first the title of and link to the blog in question, followed by one of DC’s originals distractions)
No 1
Chiropractic: “a safe form of treatment”? (edzardernst.com)
“It appears conventional medicine has a greater number of AE. This is not surprising.”
correct!
real doctors treat really sick patients
So the probability of an AE increases based upon how sick a patient is? Is there research that supports that?
No 2
Malpractice Litigation Involving Chiropractic Spinal Manipulation (edzardernst.com)
It would be interesting to know more about these 38 cases that weren’t included since that’s almost half of the 86 cases. What percentage of those cases involved SMT by a non chiropractor?
“Query of the VerdictSearch online legal database for “chiropractor” OR “chiropractic” OR “spinal manipulation” within the 22,566 listed cases classified as “medical malpractice” yielded 86 cases. Of these, 48 cases met the inclusion criteria by featuring a chiropractic practitioner as the primary defendant.”
No 3
there are three basic types of disc herniation
contained herniation
non-contained herniation
sequestered herniation
Some add a forth which are:
disc protrusion
prolapsed disc
disc extrusion
sequestered disc
where the first two are considered incomplete (contained) and the last two are called complete (non-contained) but they are all classified as a disc herniation.
You’re welcome
No 4
Multidisciplinary versus chiropractic care for low back pain (edzardernst.com)
Elaborate on what you think was my mistake regarding clinical significance.
No 5
An evidence based approach has three legs. If you wish to focus on the research leg, what does the research reveal regarding maintenance care and LBP? Have you even looked into it?
No 6
Meditation for Chronic Low Back Pain Management? (edzardernst.com)
CRITERIA in assessing the credibility of subgroup analysis.
https://www.nature.com/articles/s41433-022-01948-0/tables/1
No 7
Acute Subdural Hemorrhage Following Cervical Chiropractic Manipulation (edzardernst.com)
sigh, my use of the word require was pointing out that different problems require different solutions.
You confuse a lack of concern with my critical analysis of what some use as evidence of serious harm.
I have only used one other identifier on this blog. Some objected to my use of the word Dr in that identifier so I changed it to DC as it wasn’t worth my time to argue with them (which of course DC still refers to Doctor but it seemed to appease them).
In healthcare and particularly in manual therapy we look at increasing comfort and function because most come to us because…wait for it…a loss of comfort and function.
Yes, there is the potential to cause harm, I have never said otherwise. Most case reports suggest that serious harm is due to an improper history and exam (although other reasons may exist such as improper technique). Thus, most cases appear to be preventable with a proper history, exam and technique. That, is a different problem that, yes, requires a different solution.
So yes, spinal manipulation isn’t “required” anymore than physical therapy, NSAIDs, etc for most cases. The question is: does the intervention increase comfort and function over doing nothing and is that justified due the potential risk of harm….benefit vs risk.
Now, i shall excuse my self to prepare for a research presentation that deals with a possible new contraindication to cSMT (because I have a lack of concern, right?)
No 8
Hmmm, let’s change that a bit…
The best approach is to consider the totality of the available evidence. By doing this, one cannot exclude the possibility that NSAIDs and opioids cause serious adverse effects. If that is so, we must abide by the precautionary principle which tells us to use other treatments that seem safer and at least as effective.
So based upon the totality of the available evidence, which is safer and at least as effective: cervical spinal manipulation vs NSAIDs/opioids?
No 9
Chiropractic spinal manipulation is not safe! (edzardernst.com)
getting the patient to sign something describing the risks. This is apparently something chiropractors don’t do before a neck manipulation.
Apparently?
No 10
Vertebral artery dissection in a pregnant woman after cervical spine manipulation (edzardernst.com)
Most case reports fail on one of two criteria, sometimes both.
1. No clear record of why the patient sought chiropractic care (symptoms that may indicate a VAD in progress or not)
2. Eliminating any other possible causes of the VAD especially in the week prior to SMT.
I would have to search but I recall a case report of a woman presenting for maintenance care (no head or neck symptoms at the time) and after cSMT was dx with a VAD. Asymptomatic VADs are very rare thus there is a high probability that cSMT induced the VAD in that case, IMO.
Although not published I had a dialogue with a MD where a patient underwent a MRI, had cSMT the next day and developed new symptoms thus another MRI was shortly done and was dx with a VAD. I encouraged her to publish the case but apparently she did not.
There was a paper published that looked at the quality of these case reports, most are poor.
__________________________________
I might be mistaken but DC systematically tries to distract from the fact that chiropractic does not generate more good than harm and that there is a continuous flow of evidence suggesting it does, in fact, the exact opposite. He (I presume he is male) might not even do this consciously in which case it would suggest to me that he is full of quasi-religious zeal and unable to think critically about his own profession and creeds.
Reviewing the material above, I also realized that, by engaging with DC (and other zealots of this type), it is I who often gives him the opportunity to play his game. Therefore, I will from now on try harder to stick to my own rules that say:
- Comments must be on-topic.
- I will not post comments which are overtly nonsensical.
- I will not normally enter into discussions with people who do not disclose their full identity.
A press release informs us that the World Health Organization (WHO) and the Government of India recently signed an agreement to establish the ‘WHO Global Centre for Traditional Medicine’. This global knowledge centre for traditional medicine, supported by an investment of USD 250 million from the Government of India, aims to harness the potential of traditional medicine from across the world through modern science and technology to improve the health of people and the planet.
“For many millions of people around the world, traditional medicine is the first port of call to treat many diseases,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “Ensuring all people have access to safe and effective treatment is an essential part of WHO’s mission, and this new center will help to harness the power of science to strengthen the evidence base for traditional medicine. I’m grateful to the Government of India for its support, and we look forward to making it a success.”
The term traditional medicine describes the total sum of the knowledge, skills and practices indigenous and different cultures have used over time to maintain health and prevent, diagnose and treat physical and mental illness. Its reach encompasses ancient practices such as acupuncture, ayurvedic medicine and herbal mixtures as well as modern medicines.
“It is heartening to learn about the signing of the Host Country Agreement for the establishment of Global Centre for Traditional Medicine (GCTM). The agreement between Ministry of Ayush and World Health Organization (WHO) to establish the WHO-GCTM at Jamnagar, Gujarat, is a commendable initiative,” said Narendra Modi, Prime Minister of India. “Through various initiatives, our government has been tireless in its endeavour to make preventive and curative healthcare, affordable and accessible to all. May the global centre at Jamnagar help in providing the best healthcare solutions to the world.”
The new WHO centre will concentrate on building a solid evidence base for policies and standards on traditional medicine practices and products and help countries integrate it as appropriate into their health systems and regulate its quality and safety for optimal and sustainable impact.
The new centre focuses on four main strategic areas: evidence and learning; data and analytics; sustainability and equity; and innovation and technology to optimize the contribution of traditional medicine to global health and sustainable development.
The onsite launch of the new WHO global centre for traditional medicine in Jamnagar, Gujarat, India will take place on April 21, 2022.
__________________________
Of course, one must wait and see who will direct the unit and what work the new centre produces. But I cannot help feeling a little anxious. The press release is full of hot air and platitudes and the track record of the Indian Ministry of Ayush is quite frankly abominable. Here are a few of my previous posts that, I think, justify this statement:
- Mucormycosis (black fungus): is the Indian AYUSH ministry trying to decimate the population?
- The ‘AYUSH COVID-19 Helpline’: have they gone bonkers?
- Individualized Homeopathic Medicines for Cutaneous Warts – the dishonesty of homeopaths continues
- Ever wondered what a homeopathic egg on the face looks like?
- An RCT on the efficacy of ayurvedic treatment on asymptomatic COVID-19 patients
- Has homeopathy caused the dramatic decline of COVID-19 cases in India?
- Eight new products aimed at mitigating COVID-19. But do they really work?
- Siddha doctors have joined those claiming to have found a cure for COVID-19
- COVID-19: homeopathy gone berserk in Mumbai
- Brazil and India collaborate in the promotion of quackery
- Hard to believe: dangerous GOVERNMENTAL advice regarding SCAM for the corona virus pandemic
WATCH THIS SPACE!
This randomized, double-blind, two-armed, parallel, single-center, placebo-controlled study investigated the effectiveness and safety of the homeopathic medicine, Natrum muriaticum LM2, for mild cases of COVID-19.
Participants aged > 18 years, with influenza-like symptoms and a positive COVID test were recruited and randomized (1:1) into two groups that received different treatments during a period of at-home isolation. One group received the homeopathic medicine Natrum muriaticum, prepared with the second degree of the fifty-millesimal dynamization (LM2; Natrum muriaticum LM2), while the other group received a placebo.
The primary endpoint was time until recovery from COVID-19 influenza-like symptoms. Secondary measures included a survival analysis of the number and severity of COVID-19 symptoms (influenza-like symptoms plus anosmia and ageusia) from a symptom grading scale that was informed by the participant, hospital admissions, and adverse events. Kaplan-Meier curves were used to estimate time-to-event (survival) measures.
Data from 86 participants were analyzed (homeopathy, n = 42; placebo, n = 44). There was no difference in time to recovery between the two groups (homeopathy, n = 41; placebo, n = 41; P = 0.56), nor in a sub-group that had at least 5 moderate to severe influenza-like symptoms at the beginning of monitoring (homeopathy, n = 15; placebo, n = 17; P = 0.06). Secondary outcomes indicated that a 50% reduction in symptom score was achieved significantly earlier in the homeopathy group (homeopathy, n = 24; placebo, n = 25; P = 0.04), among the participants with a basal symptom score ≥ 5. Moreover, values of restricted mean survival time indicated that patients receiving homeopathy might have improved 0.9 days faster during the first five days of follow-up (P = 0.022). Hospitalization rates were 2.4% in the homeopathy group and 6.8% in the placebo group (P = 0.62). Participants reported 3 adverse events in the homeopathy group and 6 in the placebo group.
The authors concluded that the results showed that Natrum muriaticum LM2 was safe to use for COVID-19, but there was no statistically significant difference in the primary endpoints of Natrum muriaticum LM2 and placebo for mild COVID-19 cases. Although some secondary measures do not support the null hypothesis, the wide confidence intervals suggest that further studies with larger sample sizes and more symptomatic participants are needed to test the effectiveness of homeopathic Natrum muriaticum LM2 for COVID-19.
Homeopaths will probably claim that the trial was negative because homeopathic treatments must be individualized (true only for one school of homeopathy). More rational thinkers might point out that the study was woefully underpowered and therefore the positive trends seen in some of the subgroups are nothing other than background noise. Others again might notice that, due to the small sample size, the randomization was not successful in generating comparable groups: the placebo group was older, had more pre-existing conditions, and took more conventional medication than the homeopathy group. And they might point out that these differences could easily explain some of the findings.
Whichever way we turn it, the bottom line is simple:
Homeopathy is ineffective for COVID infections.
Today is the start of chiropractic awareness week 2022. On this occasion the BCA states most categorically: First and foremost, chiropractic is a statutorily regulated healthcare profession, supported by evidence, which offers a safe form of treatment for patients with a range of conditions. Here I am tempted to cite my friend Simon Singh:
THEY HAPPILY PROMOTE BOGUS TREATMENTS
I am, of course, particularly impressed by the BCA’s assurance of safety. In my view, the safety issue needs to be addressed more urgently than any other in the realm of chiropractic. So, to make a meaningful contribution to the current chiropractic awareness week, I conducted a few Medline searches to identify all publications of 2022 on chiropractic/spinal manipulation risks.
This is what I found:
Objective: Patients can be at risk of carotid artery dissection and ischemic stroke after cervical chiropractic manipulation. However, such risks are rarely reported and raising awareness can increase the safety of chiropractic manipulations.
Case report: We present two middle-aged patients with carotid artery dissection leading to ischemic stroke after receiving chiropractic manipulation in Foshan, Guangdong Province, China. Both patients had new-onset pain in their necks after receiving chiropractic manipulations. Excess physical force during chiropractic manipulation may present a risk to patients. Patient was administered with recombinant tissue plasminogen activator after radiological diagnoses. They were prescribed 100 mg and clopidogrel 75 mg daily for 3 months as dual antiplatelet therapy. There were no complications over the follow-up period.
Conclusion: These cases suggest that dissection of the carotid artery can occur as the result of chiropractic manipulations. Patients should be diagnosed and treated early to achieve positive outcomes. The safety of chiropractic manipulations should be increased by raising awareness about the potential risks.
Spontaneous intracranial hypotension (SIH) still remains an underdiagnosed etiology of new-onset headache. Important risk factors include chiropractic manipulation (CM). We present a case of a 36-year-old Filipino woman who presented with severe bifrontal and postural headache associated with dizziness, vomiting, and doubling of vision. A cranial computed tomography scan was done which showed an acute subdural hematoma (SDH) at the interhemispheric area. Pain medications were given which afforded minimal relief. On history, the headaches occurred 2 weeks after cervical CM. Cranial and cervical magnetic resonance imaging revealed findings supportive of intracranial hypotension and neck trauma, respectively. The patient improved with conservative management. We found 12 articles on SIH and CM after a systematic review of literature. Eleven patients (90.9%) initially presented with orthostatic headache. Eight patients (66.7%) were initially treated conservatively but only 5 (62.5%) had complete recovery. Recovery was achieved within 14 days from start of supportive therapy. Among the 3 patients who failed conservative treatment, 2 underwent non-directed epidural blood patch and one required neurosurgical intervention. This report highlights that a thorough history is warranted in patients with new onset headache. A history of CM must be actively sought. The limited evidence from the case reports showed that patients with SIH and SDH but with normal neurologic examination and minor spinal pathology can be managed conservatively for less than 2 weeks. This review showed that conservative treatment in a closely monitored environment may be an appropriate first line treatment.
Introduction: Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. We evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement.
Methods: COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
Results: One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including sneezing, carrying heavy load, chiropractic manipulation. Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
Conclusion: In this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Background: Manipulation and mobilisation for low back pain are presented in an evidence-based manner with regard to mechanisms of action, indications, efficacy, cost-effectiveness ratio, user criteria and adverse effects. Terms such as non-specific or specific are replaced by the introduction of “entities” related to possible different low back pain forms.
Efficacy: MM is effective for acute and chronic low back pain in terms of pain relief, recovery of function and relapse prevention. It is equally effective but less risky compared to other recommended therapies. MM can be used alone in acute cases and not only in the case of chronic low back pain where it is always and necessarily part of a multimodal therapy programme, especially in combination with activating measures. The users of MM should exclusively be physician specialists trained according to the criteria of the German Medical Association (Bundesärztekammer) with an additional competence in manual medicine or appropriately trained certified therapists. The application of MM follows all rules of Good Clinical Practice.
Adverse effects: Significant adverse effects of MM for low back pain are reported in the international literature with a frequency of 1 per 50,000 to 1 per 3.7 million applications, i.e. MM for low back pain is practically risk-free and safe if performed according to the rules of the European Training Requirements of the UEMS.
Studies have reported that mild adverse events (AEs) are common after manual therapy and that there is a risk of serious injury. We aimed to assess the safety of Chuna manipulation therapy (CMT), a traditional manual Korean therapy, by analysing AEs in patients who underwent this treatment. Patients who received at least one session of CMT between December 2009 and March 2019 at 14 Korean medicine hospitals were included. Electronic patient charts and internal audit data obtained from situation report logs were retrospectively analysed. All data were reviewed by two researchers. The inter-rater agreement was assessed using the Cohen’s kappa coefficient, and reliability analysis among hospitals was assessed using Cronbach’s Alpha coefficient. In total, 2,682,258 CMT procedures were performed in 289,953 patients during the study period. There were 50 AEs, including worsened pain (n = 29), rib fracture (n = 11), falls during treatment (n = 6), chest pain (n = 2), dizziness (n = 1), and unpleasant feeling (n = 1). The incidence of mild to moderate AEs was 1.83 (95% confidence interval [CI] 1.36-2.39) per 100,000 treatment sessions, and that of severe AEs was 0.04 (95% CI 0.00-0.16) per 100,000 treatment sessions. Thus, AEs of any level of severity were very rare after CMT. Moreover, there were no instances of carotid artery dissection or spinal cord injury, which are the most severe AEs associated with manual therapy in other countries.
_______________________________
This is not too bad after all!
Five papers are clearly better than nothing.
What conclusions might be drawn from my mini-review?
I think it might be safe to say:
- There is not much but at least some research going on in this area.
- The risks of chiropractic/spinal manipulation are real and are being recognized.
- BUT NOT BY CHIROPRACTORS! The most remarkable feature of the 5 papers, I think, is that none originates from a chiropractic team.
Thus, allow me to make a suggestion to chiropractors worldwide: Instead of continuing with HAPPILY PROMOTING BOGUS TREATMENTS, what about using the ‘chiropractic awareness week’ to raise awareness of the urgent necessity to research the safety of your treatments?
The pandemic has shown how difficult it can be to pass laws stopping healthcare professionals from giving unsound medical advice has proved challenging. The right to freedom of speech regularly conflicts with the duty to protect the public. How can a government best sail between Scylla and Charybdis? JAMA has just published an interesting paper addressing these issues. Here is an excerpt from the article that might stimulate some discussion:
The government can take several actions, including:
- Imposing sanctions on COVID-19–related practices by licensed professionals that flout substantive laws in connection with providing medical services, even if those medical services include speech. This includes physicians failing to comply with COVID-19–related public health laws applicable to medical offices and health facilities, such as mask wearing, social distancing, and restrictions on elective procedures.
- Sanctioning recommendations by professionals that patients take illegal medications or controlled substances without following legally required procedures. The government can also sanction the marketing by others of prescription medications for unapproved indications. However, “off-label” prescribing by physicians (eg, for hydroxychloroquine or ivermectin) remains lawful as long as a medication is approved by the US Food and Drug Administration for any indication and no specific legal conditions on use are in effect.
- Enforcing tort law actions (eg, malpractice, lack of informed consent) in cases of alleged patient injury that result from recommending a potentially dangerous treatment or failing to recommend a necessary treatment.
- Imposing sanctions on individualized medical advice by unlicensed individuals or organizations if giving that advice constitutes the unlawful practice of medicine.
In addition, the government probably can:
- Impose sanctions for false or misleading information offered to obtain a financial or personal benefit, particularly if giving the information constitutes fraud under applicable law. This would encompass physicians who knowingly spread false information to create celebrity or attract patients.
- Threaten disciplinary action by licensing boards against health professionals whose speech to patients conveys incorrect science or substandard medicine.
- Specify the information that may and may not be imparted by private organizations and professionals as part of specific clinical services paid for by government, such as special programs for COVID-19 testing or treatment.
- Reject legal challenges to, and enforce through generally applicable contract or employment laws, any restrictions private health care organizations place on speech by affiliated health professionals, particularly in the absence of special laws conferring “conscience” protections. This would include medical staff membership and privileges, hospital or other employment agreements, and insurance network participation.
- Enforce restrictions on speech adopted by private professional or self-regulatory organizations if the consequences for violations are limited to revoking organizational membership or accreditation.
However, the government probably cannot:
- Compel or limit health professional speech not made in connection with patient care, even if the speech is false or misleading, regardless of its alleged effect on public trust in health professions.
- Sanction speech to the general public rather than to patients, whether or not by health professionals, especially if conveyed with a disclaimer that the speech is “not intended as medical advice.”
- Sanction speech by health professionals to patients conveying political views or skepticism of government policy.
- Enforce restrictions involving information by public universities and public hospitals that legislatures, regulatory agencies, and professional licensing boards would not be constitutionally permitted to impose directly.
- Adopt restrictions on information related to overall clinical services funded by large government health programs, such as Medicare and Medicaid.
_____________________________
The article was obviously written with MDs in mind and applies only to US law. As we have seen in previous posts and comments, the debate is, however, wider. We should, I think, also have it in relation to practitioners of so-called alternative medicine (SCAM) and medical ethics. Moreover, it should go beyond advice about COVID and be extended to any medical advice given by any type of healthcare practitioner.
No 10-year follow-up study of so-called alternative medicine (SCAM) for lumbar intervertebral disc herniation (LDH) has so far been published. Therefore, the authors of this paper performed a prospective 10-year follow-up study on the integrated treatment of LDH in Korea.
One hundred and fifty patients from the baseline study, who initially met the LDH diagnostic criteria with a chief complaint of radiating pain and received integrated treatment, were recruited for this follow-up study. The 10-year follow-up was conducted from February 2018 to March 2018 on pain, disability, satisfaction, quality of life, and changes in a herniated disc, muscles, and fat through magnetic resonance imaging.
Sixty-five patients were included in this follow-up study. Visual analogue scale score for lower back pain and radiating leg pain were maintained at a significantly lower level than the baseline level. Significant improvements in Oswestry disability index and quality of life were consistently present. MRI confirmed that disc herniation size was reduced over the 10-year follow-up. In total, 95.38% of the patients were either “satisfied” or “extremely satisfied” with the treatment outcomes and 89.23% of the patients claimed their condition “improved” or “highly improved” at the 10-year follow-up.
The authors concluded that the reduced pain and improved disability was maintained over 10 years in patients with LDH who were treated with nonsurgical Korean medical treatment 10 years ago. Nonsurgical traditional Korean medical treatment for LDH produced beneficial long-term effects, but future large-scale randomized controlled trials for LDH are needed.
This study and its conclusion beg several questions:
WHAT DID THE SCAM CONSIST OF?
The answer is not provided in the paper; instead, the authors refer to 3 previous articles where they claim to have published the treatment schedule:
The treatment package included herbal medicine, acupuncture, bee venom pharmacopuncture and Chuna therapy (Korean spinal manipulation). Treatment was conducted once a week for 24 weeks, except herbal medication which was taken twice daily for 24 weeks; (1) Acupuncture: frequently used acupoints (BL23, BL24, BL25, BL31, BL32, BL33, BL34, BL40, BL60, GB30, GV3 and GV4)10 ,11 and the site of pain were selected and the needles were left in situ for 20 min. Sterilised disposable needles (stainless steel, 0.30×40 mm, Dong Bang Acupuncture Co., Korea) were used; (2) Chuna therapy12 ,13: Chuna is a Korean spinal manipulation that includes high-velocity, low-amplitude thrusts to spinal joints slightly beyond the passive range of motion for spinal mobilisation, and manual force to joints within the passive range; (3) Bee venom pharmacopuncture14: 0.5–1 cc of diluted bee venom solution (saline: bee venom ratio, 1000:1) was injected into 4–5 acupoints around the lumbar spine area to a total amount of 1 cc using disposable injection needles (CPL, 1 cc, 26G×1.5 syringe, Shinchang medical Co., Korea); (4) Herbal medicine was taken twice a day in dry powder (2 g) and water extracted decoction form (120 mL) (Ostericum koreanum, Eucommia ulmoides, Acanthopanax sessiliflorus, Achyranthes bidentata, Psoralea corylifolia, Peucedanum japonicum, Cibotium barometz, Lycium chinense, Boschniakia rossica, Cuscuta chinensis and Atractylodes japonica). These herbs were selected from herbs frequently prescribed for LBP (or nerve root pain) treatment in Korean medicine and traditional Chinese medicine,15 and the prescription was further developed through clinical practice at Jaseng Hospital of Korean Medicine.9 In addition, recent investigations report that compounds of C. barometz inhibit osteoclast formation in vitro16 and A. japonica extracts protect osteoblast cells from oxidative stress.17 E. ulmoides has been reported to have osteoclast inhibitive,18 osteoblast-like cell proliferative and bone mineral density enhancing effects.19 Patients were given instructions by their physician at treatment sessions to remain active and continue with daily activities while not aggravating pre-existing symptoms. Also, ample information about the favourable prognosis and encouragement for non-surgical treatment was given.
The traditional Korean spinal manipulations used (‘Chuna therapy’ – the references provided for it do NOT refer to this specific way of manipulation) seemed interesting, I thought. Here is an explanation from an unrelated paper:
Chuna, which is a traditional manual therapy practiced by Korean medicine doctors, has been applied to various diseases in Korea. Chuna manual therapy (CMT) is a technique that uses the hand, other parts of the doctor’s body or other supplementary devices such as a table to restore the normal function and structure of pathological somatic tissues by mobilization and manipulation. CMT includes various techniques such as thrust, mobilization, distraction of the spine and joints, and soft tissue release. These techniques were developed by combining aspects of Chinese Tuina, chiropratic, and osteopathic medicine.[13] It has been actively growing in Korea, academically and clinically, since the establishment of the Chuna Society (the Korean Society of Chuna Manual Medicine for Spine and Nerves, KSCMM) in 1991.[14] Recently, Chuna has had its effects nationally recognized and was included in the Korean national health insurance in March 2019.[15]
This almost answers the other questions I had. Almost, but not quite. Here are two more:
- The authors conclude that the SCAM produced beneficial long-term effects. But isn’t it much more likely that the outcomes their uncontrolled observations describe are purely or at least mostly a reflection of the natural history of lumbar disc herniation?
- If I remember correctly, I learned a long time ago in medical school that spinal manipulation is contraindicated in lumbar disc herniation. If that is so, the results might have been better, if the patients of this study had not received any SCAM at all. In other words, are the results perhaps due to firstly the natural history of the condition and secondly to the detrimental effects of the SCAM the investigators applied?
If I am correct, this would then be the 4th article reporting the findings of a SCAM intervention that aggravated lumbar disc herniation.
PS
I know that this is a mere hypothesis but it is at least as plausible as the conclusion drawn by the authors.
Low back pain (LBP) is influenced by interrelated biological, psychological, and social factors, however current back pain management is largely dominated by one-size fits all unimodal treatments. Team based models with multiple provider types from complementary professional disciplines is one way of integrating therapies to address patients’ needs more comprehensively.
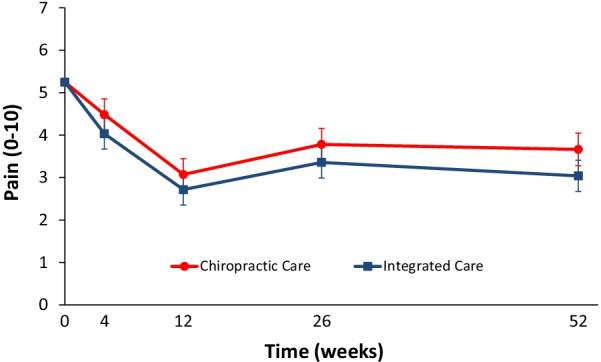
This parallel-group randomized clinical trial conducted from May 2007 to August 2010 aimed to evaluate the relative clinical effectiveness of 12 weeks of monodisciplinary chiropractic care (CC), versus multidisciplinary integrative care (IC), for adults with sub-acute and chronic LBP. The primary outcome was pain intensity and secondary outcomes were disability, improvement, medication use, quality of life, satisfaction, frequency of symptoms, missed work or reduced activities days, fear-avoidance beliefs, self-efficacy, pain coping strategies, and kinesiophobia measured at baseline and 4, 12, 26 and 52 weeks. Linear mixed models were used to analyze outcomes.
In total, 201 participants were enrolled. The largest reductions in pain intensity occurred at the end of treatment and were 43% for CC and 47% for IC. The primary analysis found IC to be significantly superior to CC over the 1-year period (P = 0.02). The long-term profile for pain intensity which included data from weeks 4 through 52, showed a significant advantage of 0.5 for IC over CC (95% CI 0.1 to 0.9; P = 0.02; 0 to 10 scale). The short-term profile (weeks 4 to 12) favored IC by 0.4, but was not statistically significant (95% CI – 0.02 to 0.9; P = 0.06). There was also a significant advantage over the long term for IC in some secondary measures (disability, improvement, satisfaction, and low back symptom frequency), but not for others (medication use, quality of life, leg symptom frequency, fear-avoidance beliefs, self-efficacy, active pain coping, and kinesiophobia). No serious adverse events resulted from either of the interventions.
The authors concluded that participants in the IC group tended to have better outcomes than the CC group, however, the magnitude of the group differences was relatively small. Given the resources required to successfully implement multidisciplinary integrative care teams, they may not be worthwhile, compared to monodisciplinary approaches like chiropractic care, for treating LBP.
The obvious question is: what were the exact treatments used in both groups? The authors provide the following explanations:
All participants in the study received 12 weeks of either monodisciplinary chiropractic care (CC) or multidisciplinary team-based integrative care (IC). CC was delivered by a team of chiropractors allowed to utilize any non-proprietary treatment under their scope of practice not shown to be ineffective or harmful including manual spinal manipulation (i.e., high velocity, low amplitude thrust techniques, with or without the assistance of a drop table) and mobilization (i.e., low velocity, low amplitude thrust techniques, with or without the assistance of a flexion-distraction table). Chiropractors also used hot and cold packs, soft tissue massage, teach and supervise exercise, and administer exercise and self-care education materials at their discretion. IC was delivered by a team of six different provider types: acupuncturists, chiropractors, psychologists, exercise therapists, massage therapists, and primary care physicians, with case managers coordinating care delivery. Interventions included acupuncture and Oriental medicine (AOM), spinal manipulation or mobilization (SMT), cognitive behavioral therapy (CBT), exercise therapy (ET), massage therapy (MT), medication (Med), and self-care education (SCE), provided either alone or in combination and delivered by their respective profession. Participants were asked not to seek any additional treatment for their back pain during the intervention period. Standardized forms were used to document the details of treatment, as well as adverse events. It was not possible to blind patients or providers to treatment due to the nature of the study interventions. Patients in both groups received individualized care developed by clinical care teams unique to each intervention arm. Care team training was conducted to develop and support group dynamics and shared clinical decision making. A clinical care pathway, designed to standardize the process of developing recommendations, guided team-based practitioner in both intervention arms. Evidence based treatment plans were based on patient biopsychosocial profiles derived from the history and clinical examination, as well as baseline patient rated outcomes. The pathway has been fully described elsewhere [23]. Case managers facilitated patient care team meetings, held weekly for each intervention group, to discuss enrolled participants and achieve treatment plan recommendation consensus. Participants in both intervention groups were presented individualized treatment plan options generated by the patient care teams, from which they could choose based on their preferences.
This is undoubtedly an interesting study. It begs many questions. The two that puzzle me most are:
- Why publish the results only 12 years after the trial was concluded? The authors provide a weak explanation, but I would argue that it is unethical to sit on a publicly funded study for so long.
- Why did the researchers not include a third group of patients who were treated by their GP like in normal routine?
The 2nd question is, I think, important because the findings could mostly be a reflection of the natural history of LBP. We can probably all agree that, at present, the optimal treatment for LBP has not been found. To me, the results look as though they indicate that it hardly matters how we treat LBP, the outcome is always very similar. If we throw the maximum amount of care at it, the results tend to be marginally better. But, as the authors admit, there comes a point where we have to ask, is it worth the investment?
Perhaps the old wisdom is not entirely wrong (old because I learned it at medical school some 50 years ago): make sure LBP patients keep as active as they can while trying to ignore their pain as best as they can. It’s not a notion that would make many practitioners of so-called alternative medicine (SCAM) happy – LBP is their No 1 cash cow! – but it would surely save huge amounts of public expenditure.
Ginseng plants belong to the genus Panax and include:
- Panax ginseng (Korean ginseng),
- Panax notoginseng (South China ginseng),
- and Panax quinquefolius (American ginseng).
They are said to have a range of therapeutic activities, some of which could render ginseng a potential therapy for viral or post-viral infections. Ginseng has therefore been used to treat fatigue in various patient groups and conditions. But does it work for chronic fatigue syndrome (CFS), also often called myalgic encephalomyelitis (ME)? This condition is a complex, little-understood, and often disabling chronic illness for which no curative or definitive therapy has yet been identified.
This systematic review aimed to assess the current state of evidence regarding ginseng for CFS. Multiple databases were searched from inception to October 2020. All data was extracted independently and in duplicates. Outcomes of interest included the effectiveness and safety of ginseng in patients with CFS.
A total of two studies enrolling 68 patients were deemed eligible: one randomized clinical trial and one prospective observational study. The certainty of evidence in the effectiveness outcome was low and moderate in both studies, while the safety evidence was very low as reported from one study.
The authors concluded that the study findings highlight a potential benefit of ginseng therapy in the treatment of CFS. However, we are not able to draw firm conclusions due to limited clinical studies. The paucity of data warrants limited confidence. There is a need for future rigorous studies to provide further evidence.
To get a feeling of how good or bad the evidence truly is, we must of course look at the primary studies.
The prospective observational study turns out to be a mere survey of patients using all sorts of treatments. It included 155 subjects who provided information on fatigue and treatments at baseline and follow-up. Of these subjects, 87% were female and 79% were middle-aged. The median duration of fatigue was 6.7 years. The percentage of users who found a treatment helpful was greatest for coenzyme Q10 (69% of 13 subjects), dehydroepiandrosterone (DHEA) (65% of 17 subjects), and ginseng (56% of 18 subjects). Treatments at 6 months that predicted subsequent fatigue improvement were vitamins (p = .08), vigorous exercise (p = .09), and yoga (p = .002). Magnesium (p = .002) and support groups (p = .06) were strongly associated with fatigue worsening from 6 months to 2 years. Yoga appeared to be most effective for subjects who did not have unclear thinking associated with fatigue.
The second study investigated the effect of Korean Red Ginseng (KRG) on chronic fatigue (CF) by various measurements and objective indicators. Participants were randomized to KRG or placebo group (1:1 ratio) and visited the hospital every 2 weeks while taking 3 g KRG or placebo for 6 weeks and followed up 4 weeks after the treatment. The fatigue visual analog score (VAS) declined significantly in each group, but there were no significant differences between the groups. The 2 groups also had no significant differences in the secondary outcome measurements and there were no adverse events. Sub-group analysis indicated that patients with initial fatigue VAS below 80 mm and older than 50 years had significantly greater reductions in the fatigue VAS if they used KRG rather than placebo. The authors concluded that KRG did not show absolute anti-fatigue effect but provided the objective evidence of fatigue-related measurement and the therapeutic potential for middle-aged individuals with moderate fatigue.
I am at a loss in comprehending how the authors of the above-named review could speak of evidence for potential benefit. The evidence from the ‘observational study’ is largely irrelevant for deciding on the effectiveness of ginseng, and the second, more rigorous study fails to show that ginseng has an effect.
So, is ginseng a promising treatment for ME?
I doubt it.
Brite is an herbal energy drink that is currently being marketed aggressively. It is even for sale in one leading UK supermarket. It comes in various flavors the ingredients of which vary slightly.
The pineapple/mango drink, for instance, contains:
- guarana extract,
- green tea extract,
- guayusa extract,
- ashwagandha extract,
- matcha tea,
- ascorbic acid (vitamin C),
- natural caffeine.
The website of the manufacturer tells us that Brite uses ingredients and dosages that are safe and effective, utilising the power of nootropic superfoods organic Matcha, Guarana and Guayusa to provide a long-lasting boost.
Brite is based on peer reviewed, double-blind, placebo-controlled clinical trials and studies that can be found here.
It does not tell us the dosages of the ingredients, and I am puzzled by the claim that the drink is safe. A quick search seems to cast considerable doubt on it.
_____________________________
Guarana (Paullinia cupana) is a plant from the Amazon region with a high content of bioactive compounds. It is by no means free of adverse effects. It is known to interact with:
- armodafinil
- caffeine
- dexmethylphenidate
- dextroamphetamine
- green tea
- lisdexamfetamine
- methamphetamine
- methylenedioxymethamphetamine
- methylphenidate
- modafinil
- phentermine
- yohimbine
And it can cause the following adverse effects:
- Abdominal spasms (from overdose)
- Agitation
- Anxiety
- Convulsions
- Delirium
- Dependence
- Diarrhea
- Dizziness
- Fast heart rate
- Gastrointestinal (GI) upset
- Headache
- High blood pressure (hypertension)
- High blood sugar (hyperglycemia)
- Increased respiration
- Increased urination
- Insomnia
- Irregular heartbeats (arrhythmias)
- Irritability
- Muscle spasms
- Nausea/vomiting
- Nervousness
- Painful urination (from overdose)
- Rapid breathing
- Restlessness
- Ringing in the ears (tinnitus)
- Stomach cramps or irritation
- Tremors
- Withdrawal symptoms
Green tea is made from the leaves of the Camellia sinensis plant. It can cause the following adverse effects:
- headache,
- nervousness,
- sleep problems,
- vomiting,
- diarrhea,
- irritability,
- irregular heartbeat,
- tremor,
- heartburn,
- dizziness,
- ringing in the ears,
- convulsions,
- confusion.
Guayusa is a plant native to the Amazon rainforest that contains plenty of caffeine. Its adverse effects include:
- High Blood Pressure
- Rapid Heartbeat
- Anxiety
- Jitters
- Energy Crashes
- Insomnia
- Headaches
- Upset Stomach
Ashwagandha is a plant from India; the root and berry are used in Ayurvedic medicine. Its adverse effects include:
- stomach upset,
- diarrhea,
- vomiting.
Matcha tea also contains a high amount of caffeine. It is associated with the following adverse effects:
- nervousness,
- irritability,
- dizziness,
- anxiety,
- digestive disorders such as irritable bowel syndrome, or diarrhea,
- sleeping disorders,
- cardiac arrhythmia.
Caffeine is a chemical found in coffee, tea, cola, guarana, mate, and other products. Adverse effects include:
- insomnia,
- nervousness,
- restlessness,
- stomach irritation,
- nausea and vomiting,
- increased heart rate and respiration,
- headache,
- anxiety,
- agitation,
- chest pain,
- ringing in the ears.
A case report documented a case of myocardial infarction in a 25-year-old man who presented to the emergency department with chest pain. The patient had been consuming massive quantities of caffeinated energy drinks daily for the past week. This case report and previously documented studies support a possible connection between caffeinated energy drinks and myocardial infarction.
________________________
Yes, the adverse effects are predominantly (but not exclusively) caused by high doses. Yet, the claim that Brite is safe should nevertheless be taken with a very large pinch of salt. If I like the taste of the drink and thus consume a few bottles per day, the dosages of the ingredients would surely be high!
And what about the claim that it is effective? Here the pinch of salt must be even larger, I am afraid. I could not find a single trial that confirmed the notion. For backing up their claims, the manufacturers offer a few references, but if you look them up, you will find that they were not done with the mixture of ingredients contained in Brite.
So, what is the conclusion?
Based on the evidence that I have seen, the herbal drink ‘Brite’ has not been shown to be an effective nootropic. In addition, there are legitimate concerns about the safety of the product. I for one will therefore not purchase the (rather expensive) drink.