yoga
The American Heart Association has issued a statement outlining research on so-called alternative medicine (SCAM) for heart failure. They found some SCAMs that work, some that don’t work, and some that are harmful.
Alternative therapies that may benefit people with heart failure include:
- Omega-3 polyunsaturated fatty acids (PUFA, fish oil) have the strongest evidence among complementary and alternative agents for clinical benefit in people with heart failure and may be used safely, in moderation, in consultation with their health care team. Omega-3 PUFA is associated with a lower risk of developing heart failure and, for those who already have heart failure, improvements in the heart’s pumping ability. There appears to be a dose-related increase in atrial fibrillation (an irregular heart rhythm), so doses of 4 grams or more should be avoided.
- Yoga and Tai Chi, in addition to standard treatment, may help improve exercise tolerance and quality of life and decrease blood pressure.
Meanwhile, some therapies were found to have harmful effects, such as interactions with common heart failure medications and changes in heart contraction, blood pressure, electrolytes and fluid levels:
- While low blood levels of vitamin D are associated with worse heart failure outcomes, supplementation hasn’t shown benefit and may be harmful when taken with heart failure medications such as digoxin, calcium channel blockers and diuretics.
- The herbal supplement blue cohosh, from the root of a flowering plant found in hardwood forests, might cause a fast heart rate called tachycardia, high blood pressure, chest pain and may increase blood glucose. It may also decrease the effect of medications taken to treat high blood pressure and Type 2 diabetes.
- Lily of the valley, the root, stems and flower of which are used in supplements, has long been used in mild heart failure because it contains active chemicals similar to, but less potent than, the heart failure medicine digoxin. It may be harmful when taken with digoxin by causing very low potassium levels, a condition known as hypokalemia. Lily of the valley also may cause irregular heartbeat, confusion and tiredness.
Other therapies have been shown as ineffective based on current data, or have mixed findings, highlighting the importance of patients having a discussion with a health care professional about any non-prescribed treatments:
- Routine thiamine supplementation isn’t shown to be effective for heart failure treatment unless someone has this specific nutrient deficiency.
- Research on alcohol varies, with some data showing that drinking low-to-moderate amounts (1 to 2 drinks per day) is associated with preventing heart failure, while habitual drinking or intake of higher amounts is toxic to the heart muscle and known to contribute to heart failure.
- There are mixed findings about vitamin E. It may have some benefit in reducing the risk of heart failure with preserved ejection fraction, a type of heart failure in which the left ventricle is unable to properly fill with blood between heartbeats. However, it has also been associated with an increased risk of hospitalization in people with heart failure.
- Co-Q10, or coenzyme Q10, is an antioxidant found in small amounts in organ meats, oily fish and soybean oil, and commonly taken as a dietary supplement. Small studies show it may help improve heart failure class, symptoms and quality of life, however, it may interact with blood pressure lowering and anti-clotting medicines. Larger trials are needed to better understand its effects.
- Hawthorn, a flowering shrub, has been shown in some studies to increase exercise tolerance and improve heart failure symptoms such as fatigue. Yet it also has the potential to worsen heart failure, and there is conflicting research about whether it interacts with digoxin.
“Overall, more quality research and well-powered randomized controlled trials are needed to better understand the risks and benefits of complementary and alternative medicine therapies for people with heart failure,” said Chow. “This scientific statement provides critical information to health care professionals who treat people with heart failure and may be used as a resource for consumers about the potential benefit and harm associated with complementary and alternative medicine products.”
____________________
No doubt, this assessment is a laudable attempt to inform patients responsibly. Personally, I am always a bit skeptical about such broad statements. SCAM encompasses some 400 different therapies, and I doubt that these can all be assessed in one single overview.
It is not difficult to find SCAMs that seem to have not been considered. Take this systematic review, for instance. It included 24 RCTs (n = 1314 participants) of 9 different mind-body interventions (MBI) types: Tai Chi (n = 7), yoga (n = 4), relaxation (n = 4), meditation (n = 2), acupuncture (n = 2), biofeedback (n = 2), stress management (n = 1), Pilates (n = 1), and reflexology (n = 1). Most (n = 22, 95.8%) reported small-to-moderate improvements in quality of life (14/14 studies), exercise capacity (8/9 studies), depression (5/5 studies), anxiety and fatigue (4/4 studies), blood pressure (3/5 studies), heart rate (5/6 studies), heart rate variability (7/9 studies), and B-type natriuretic peptide (3/4 studies). Studies ranged from 4 minutes to 26 weeks and group sizes ranged from 8 to 65 patients per study arm.
The authors concluded that, although wide variability exists in the types and delivery, RCTs of MBIs have demonstrated small-to-moderate positive effects on HF patients’ objective and subjective outcomes. Future research should examine the mechanisms by which different MBIs exert their effects.
Or take this systematic review of 38 RCTs of oral TCM remedies. The majority of the included trials were assessed to be of high clinical heterogeneity and poor methodological quality. The main results of the meta-analysis showed improvement in total MLHFQ score when oral Chinese herbal medicine plus conventional medical treatment (CMT) compared with CMT with or without placebo [MD = -5.71 (-7.07, -4.36), p < 0.01].
The authors concluded that there is some encouraging evidence of oral Chinese herbal medicine combined with CMT for the improvement of QoL in CHF patients. However, the evidence remains weak due to the small sample size, high clinical heterogeneity, and poor methodological quality of the included trials. Further, large sample size and well-designed trials are needed.
Don’t get me wrong: I am not saying that TCM remedies are a viable option – in fact, I very much doubt it – but I am saying that attempts to provide comprehensive overviews of all SCAMs are problematic, and that incomplete overviews are just that: incomplete.
Camilla spent ten days at the end of October in a sophisticated meditation and fitness center in southern India. Life has recently been hectic for the Queen Consort: at 75, she has been in a non-stop succession of various ceremonies for the funeral of Elizabeth II, always one step behind her husband, not to mention her new status as sovereign… Enough to block her chakras in no time.
She came to the resort with her bodyguards and a handful of friends and was able to take advantage of the tailor-made treatments concocted for her by the master of the house, Dr Issac Mathai, who created this high-end holistic centre on a dozen hectares of scented gardens near Bangalore. The program includes massages, herbal steam baths, yoga, naturopathy, homeopathy, meditation, and Ayurvedic treatments to “cleanse, de-stress, soothe and revitalize the mind, body and soul”, as the establishment’s website states.
Guests are required to follow an individualized, meat-free diet, with organic food from the resort’s vegetable gardens, based on lots of salads or soups – Camilla is said to be a fan of sweet corn soup with spinach. Cigarettes and mobile phones are not allowed, although it is assumed that Camilla must have some privileges due to her status… and the basic rate for the suites, which starts at $950 a night – the price of the rooms varies between $260 and $760, the rate including a consultation with the doctors.
Charles and Camilla have been fans of the Soukya Centre in India for a decade. The place corresponds in every way to their deep-rooted convictions about health. Like her husband, Camilla is a follower of organic food, she also practices yoga and treats her face with creams made from nettle and bee venom. For his part, Charles has long been an advocate of alternative medicine, homeopathy, acupuncture, aromatherapy, and also hypnosis… He even set up a foundation to support complementary medicine by lobbying the British health service to include it in complementary therapies for certain patients, which caused an uproar among the pundits of traditional medicine.
________________________
If you suspected I was (yet again) sarcastic about the royal couple, you are mistaken. The text above is only my (slightly shortened) translation of an article published in the French magazine LE POINT (even the title is theirs). I found the article amusing and interesting; so, I looked up the Indian health center. Here are some of the things I found:
The 1st impression is that they are not shy about promotion calling themselves THE WORLD’S BEST AYURVEDA TREATMENT CENTER. The doctor in charge was once a ‘Consultant Physician’ at the Hale Clinic in London, where he treated a number of high-profile people. As his professional background, he offers this:
M.D. (Homeopathy); Hahnemann Post-Graduate Institute of Homeopathy, London M.R.C.H, London; Chinese Pulse Diagnosis and Acupuncture, WHO Institute of Traditional Chinese Medicine, Nanjing, China; Trained (Mind-Body Medicine Programme) at Harvard Medical School, USA
The approach of the center is described as follows:
The fundamental principle underlying Holistic Treatment is that the natural defense and immune system of an individual when strengthened, has the potential to heal and prevent diseases. In the age of super-specialisation where human beings are often viewed as a conglomeration of organs, it is crucial to understand ourselves as multi-dimensional beings with a body, mind and spirit. These interconnected dimensions need to be in perfect harmony to ensure real well-being.
And about homeopathy, they claim this:
Homeopathy originated in 1796 in Germany, and was discovered by Dr. Samuel Hahnemann, a German scientist. Homeopathy is popular today as a non-intrusive, holistic system of medicine. Instead of different medicines for different parts of the body, one single constitutional remedy is prescribed. As a system of medicine, Homeopathy is highly scientific, safe, logical and an extremely effective method of healing. For over 200 years people have used Homeopathy to maintain their good health, and also to treat and cure a wide range of illnesses like allergies, metabolic disorders, atopic dermatitis, Rheumatoid arthritis, Auto-immune disorders.
At this stage, I felt I had seen enough. Yes, you are right, we did not learn a lot from this little exploration. No, hold on! We did learn that homeopathy is highly scientific, safe, logical, and extremely effective!
The question, however, is should we believe it?
Yesterday, L’EXPRESS published an interview with me. It was introduced with these words (my translation):
Professor emeritus at the University of Exeter in the United Kingdom, Edzard Ernst is certainly the best connoisseur of unconventional healing practices. For 25 years, he has been sifting through the scientific evaluation of these so-called “alternative” medicines. With a single goal: to provide an objective view, based on solid evidence, of the reality of the benefits and risks of these therapies. While this former homeopathic doctor initially thought he was bringing them a certain legitimacy, he has become one of their most enlightened critics. It is notable as a result of his work that the British health system, the NHS, gave up covering homeopathy. Since then, he has never ceased to alert us to the abuses and lies associated with these practices. For L’Express, he looks back at the challenges of regulating this vast sector and deciphers the main concepts put forward by “wellness” professionals – holism, detox, prevention, strengthening the immune system, etc.
The interview itself is quite extraordinary, in my view. While UK, US, and German journalists usually are at pains to tone down my often outspoken answers, the French journalists (there were two doing the interview with me) did nothing of the sort. This starts with the title of the piece: “Homeopathy is implausible but energy healing takes the biscuit”.
The overall result is one of the most outspoken interviews of my entire career. Let me offer you a few examples (again my translation):
Why are you so critical of celebrities like Gwyneth Paltrow who promote these wellness methods?
Sadly, we have gone from evidence-based medicine to celebrity-based medicine. A celebrity without any medical background becomes infatuated with a certain method. They popularize this form of treatment, very often making money from it. The best example of this is Prince Charles, sorry Charles III, who spent forty years of his life promoting very strange things under the guise of defending alternative medicine. He even tried to market a “detox” tincture, based on artichoke and dandelion, which was quickly withdrawn from the market.
How to regulate this sector of wellness and alternative medicines? Today, anyone can present himself as a naturopath or yoga teacher…
Each country has its own regulation, or rather its own lack of regulation. In Germany, for instance, we have the “Heilpraktikter”. Anyone can get this paramedical status, you just have to pass an exam showing that you are not a danger to the public. You can retake this exam as often as you want. Even the dumbest will eventually pass. But these practitioners have an incredible amount of freedom, they even may give infusions and injections. So there is a two-tier health care system, with university-trained doctors and these practitioners.
In France, you have non-medical practitioners who are fighting for recognition. Osteopaths are a good example. They are not officially recognized as a health profession. Many schools have popped up to train them, promising a good income to their students, but today there are too many osteopaths compared to the demand of the patients (knowing that nobody really needs an osteopath to begin with…). Naturopaths are in the same situation.
In Great Britain, osteopaths and chiropractors are regulated by statute. There is even a Royal College dedicated to chiropractic. It’s a bit like having a Royal College for hairdressers! It’s stupid, but we have that. We also have professionals like naturopaths, acupuncturists, or herbalists who have an intermediate status. So it’s a very complex area, depending on the state. It is high time to have more uniform regulations in Europe.
But what would adequate regulation look like?
From my point of view, if you really regulate a profession like homeopaths, it means that these professionals may only practice according to the best scientific evidence available. Which, in practice, means that a homeopath cannot practice homeopathy. This is why these practitioners have a schizophrenic attitude toward regulation. On the one hand, they would like to be recognized to gain credibility. But on the other hand, they know very well that a real regulation would mean that they would have to close shop…
What about the side effects of these practices?
If you ask an alternative practitioner about the risks involved, he or she will take exception. The problem is that there is no system in alternative medicine to monitor side effects and risks. However, there have been cases where chiropractors or acupuncturists have killed people. These cases end up in court, but not in the medical literature. The acupuncturists have no problem saying that a hundred deaths due to acupuncture – a figure that can be found in the scientific literature – is negligible compared to the millions of treatments performed every day in this discipline. But this is only the tip of the iceberg. There are many cases that are not published and therefore not included in the data, because there is no real surveillance system for these disciplines.
Do you see a connection between the wellness sector and conspiracy theories? In the US, we saw that Qanon was thriving in the yoga sector, for example…
Several studies have confirmed these links: people who adhere to conspiracy theories also tend to turn to alternative medicine. If you think about it, alternative medicine is itself a conspiracy theory. It is the idea that conventional medicine, in the name of pharmaceutical interests, in particular, wants to suppress certain treatments, which can therefore only exist in an alternative world. But in reality, the pharmaceutical industry is only too eager to take advantage of this craze for alternative products and well-being. Similarly, universities, hospitals, and other health organizations are all too willing to open their doors to these disciplines, despite the lack of evidence of their effectiveness.
Today is WORLD ASTHMA DAY, a good opportunity perhaps to revisit a few of our own evaluations of so-called alternative medicine (SCAM) for asthma. Here are the abstracts of some of our systematic reviews on the subject:
Objective: The objective of this systematic review was to assess the effectiveness of yoga as a treatment option for asthma.
Method: Seven databases were searched from their inception to October 2010. Randomized clinical trials (RCTs) and non-randomized clinical trials (NRCTs) were considered, if they investigated any type of yoga in patients with asthma. The selection of studies, data extraction, and validation were performed independently by two reviewers.
Results: Six RCTs and one NRCT met the inclusion criteria. Their methodological quality was mostly poor. Three RCTs and one NRCT suggested that yoga leads to a significantly greater reduction in spirometric measures, airway hyperresponsivity, dose of histamine needed to provoke a 20% reduction in forced expiratory volume in the first second, weekly number of asthma attacks, and need for drug treatment. Three RCTs showed no positive effects compared to various control interventions.
Conclusions: The belief that yoga alleviates asthma is not supported by sound evidence. Further, more rigorous trials are warranted.
Some clinicians believe that spinal manipulation is an effective treatment for asthma. The aim of this systematic review was to critically evaluate the evidence for or against this claim. Four electronic databases were searched without language restrictions from their inceptions to September 2008. Bibliographies and departmental files were hand-searched. The methodological quality of all included studies was assessed with the Jadad score. Only randomised clinical trials of spinal manipulation as a treatment of asthma were included. Three studies met these criteria. All of them were of excellent methodological quality (Jadad score 5) and all used sham-manipulation as the control intervention. None of the studies showed that real manipulation was more effective than sham-manipulation in improving lung function or subjective symptoms. It is concluded that, according to the evidence of the most rigorous studies available to date, spinal manipulation is not an effective treatment for asthma.
Contradictory results from randomised controlled trials of acupuncture in asthma suggest both a beneficial and detrimental effect. The authors conducted a formal systematic review and meta-analysis of all randomised clinical trials in the published literature that have compared acupuncture at real and placebo points in asthma patients. The authors searched for trials published in the period 1970-2000. Trials had to measure at least one of the following objective outcomes: peak expiratory flow rate, forced expiratory volume in one second (FEV1) and forced vital capacity. Estimates of the standarised mean difference, between acupuncture and placebo were computed for each trial and combined to estimate the overall effect. Hetereogeneity was investigated in terms of the characteristics of the individual studies. Twelve trials met the inclusion criteria but data from one could not be obtained. Individual patient data were available in only three. Standardised differences between means ranging from 0.071 to 0.133, in favour of acupuncture, were obtained. The overall effect was not conventionally significant and it corresponds to an approximate difference in FEV1 means of 1.7. After exploring hetereogenenity, it was found that studies where bronchoconstriction was induced during the experiment showed a conventionally significant effect. This meta-analysis did not find evidence of an effect of acupuncture in reducing asthma. However, the meta-analysis was limited by shortcomings of the individual trials, in terms of sample size, missing information, adjustment of baseline characteristics and a possible bias against acupuncture introduced by the use of placebo points that may not be completely inactive. There was a suggestion of preferential publication of trials in favour of acupuncture. There is an obvious need to conduct a full-scale randomised clinical trial addressing these limitations and the prognostic value of the aetiology of the disease.
Background: Emotional stress can either precipitate or exacerbate both acute and chronic asthma. There is a large body of literature available on the use of relaxation techniques for the treatment of asthma symptoms. The aim of this systematic review was to determine if there is any evidence for or against the clinical efficacy of such interventions.
Methods: Four independent literature searches were performed on Medline, Cochrane Library, CISCOM, and Embase. Only randomised clinical trials (RCTs) were included. There were no restrictions on the language of publication. The data from trials that statistically compared the treatment group with that of the control were extracted in a standardised predefined manner and assessed critically by two independent reviewers.
Results: Fifteen trials were identified, of which nine compared the treatment group with the control group appropriately. Five RCTs tested progressive muscle relaxation or mental and muscular relaxation, two of which showed significant effects of therapy. One RCT investigating hypnotherapy, one of autogenic training, and two of biofeedback techniques revealed no therapeutic effects. Overall, the methodological quality of the studies was poor.
Conclusions: There is a lack of evidence for the efficacy of relaxation therapies in the management of asthma. This deficiency is due to the poor methodology of the studies as well as the inherent problems of conducting such trials. There is some evidence that muscular relaxation improves lung function of patients with asthma but no evidence for any other relaxation technique.
Background: Asthma is one of the most common chronic diseases in modern society and there is increasing evidence to suggest that its incidence and severity are increasing. There is a high prevalence of usage of complementary medicine for asthma. Herbal preparations have been cited as the third most popular complementary treatment modality by British asthma sufferers. This study was undertaken to determine if there is any evidence for the clinical efficacy of herbal preparations for the treatment of asthma symptoms.
Methods: Four independent literature searches were performed on Medline, Pubmed, Cochrane Library, and Embase. Only randomised clinical trials were included. There were no restrictions on the language of publication. The data were extracted in a standardised, predefined manner and assessed critically.
Results: Seventeen randomised clinical trials were found, six of which concerned the use of traditional Chinese herbal medicine and eight described traditional Indian medicine, of which five investigated Tylophora indica. Three other randomised trials tested a Japanese Kampo medicine, marihuana, and dried ivy leaf extract. Nine of the 17 trials reported a clinically relevant improvement in lung function and/or symptom scores.
Conclusions: No definitive evidence for any of the herbal preparations emerged. Considering the popularity of herbal medicine with asthma patients, there is urgent need for stringently designed clinically relevant randomised clinical trials for herbal preparations in the treatment of asthma.
Breathing techniques are used by a large proportion of asthma sufferers. This systematic review was aimed at determining whether or not these interventions are effective. Four independent literature searches identified six randomized controlled trials. The results of these studies are not uniform. Collectively the data imply that physiotherapeutic breathing techniques may have some potential in benefiting patients with asthma. The safety issue has so far not been addressed satisfactorily. It is concluded that too few studies have been carried out to warrant firm judgements. Further rigorous trials should be carried out in order to redress this situation.
__________________________________
So, if you suffer from asthma, my advice is to stay away from SCAM. This might be easier said than done because SCAM practitioners are only too willing to lure asthma patients into their cult. In 2003, we have demonstrated this phenomenon by conducting a survey with chiropractors. Here is our short paper in full:
Classic chiropractic theory claims that vertebral subluxation blocks the flow of ‘‘innate intelligence’’ which, in turn, affects the health of asthma patients (1). Chiropractictors often use spinal manipulation (SM) to correct such malalignments and treat asthma (2). Several clinical trials of chiropractic SM exist, but the most rigorous ones are clearly negative (3,4). Chronic medication with corticosteroids can lead to osteoporosis, a condition, which is a contra-indication to chiropractic SM (5). Given this background, we aimed to determine whether chiropractors would advise an asthma patient on long-term corticosteroids (5 years) to try chiropractic as a treatment for this condition.
All 350 e-mail addresses listed at www.interadcom.com/chiro/html were randomised into two groups. A (deceptive) letter from a (fictitious) patient was sent to group A while group B was asked for advice on chiropractic treatment for asthma as part of a research project. Thus, groups A and B were asked the same question in di¡erent contexts: is chiropractic safe and e¡ective for an asthma patient on long-term steroids. After data collection, respondents from group A were informed that the e-mail had been part of a research project.
Of 97 e-mails in group A, we received 31 responses (response rate = 32% (95% CI, 0.23^ 0.41)). Seventy-four per cent (23 respondents) recommended visiting a chiropractor (95% CI, 0.59^ 0.89). Thirty-five per cent (11 respondents) mentioned minimal or no adverse effects of SM (95% CI, 0.18 ^ 0.52). Three chiropractors responded that some adverse e¡ects exist, e.g. risk of bone fracture, or stroke. Two respondents noted that other investigations (X-rays, spinal and neurological examination) were required before chiropractic treatment. Three respondents suggested additional treatments and one warned about a possible connection between asthma and the measles vaccine. Of 77 e-mails sent to group B, we received 16 responses (response rate = 21% (95% CI, 0.17^ 0.25)). Eleven respondents (69%) recommended visiting a chiropractor (95% CI, 0.46 ^ 0.91). Ten respondents mentioned minimal or no adverse effects of SM (95% CI, 0.39^ 0.87). Five chiropractors responded that adverse effects of SM exist (e.g. bone fracture). Five respondents suggested pre-testing the patient to check bone density, allergy, diet, exercise level, hydration and blood. Additional treatments were recommended by three respondents. The pooled results of groups A and B suggested that the majority of chiropractors recommend chiropractic treatment for asthma and the minority mention any adverse effects.
Our results demonstrate that chiropractic advice on asthma therapy is as readily available over the Internet as it is likely to be misleading. The majority of respondents from both groups (72%) recommended chiropractic treatment. This usually entails SM, a treatment modality which has been demonstrated to be ineffective in rigorous clinical trials (3,4,6). The advice may also be dangerous: the minority of the respondents of both groups (17%) caution of the risk of bone fracture. Our findings also suggest that, for the research question asked, a degree of deception is necessary. The response rate in group B was 12% lower than that of group A, and the answers received differed considerably between groups. In group A, 10% acknowledged the possibility of adverse e¡ects, this figure was 33% in group B. In conclusion, chiropractors readily provide advice regarding asthma treatment, which is often not evidence-based and has the potential to put patients at risk.
__________________________
As I stated above: if you suffer from asthma, my advice is to
stay away from SCAM.
A press release informs us that the World Health Organization (WHO) and the Government of India recently signed an agreement to establish the ‘WHO Global Centre for Traditional Medicine’. This global knowledge centre for traditional medicine, supported by an investment of USD 250 million from the Government of India, aims to harness the potential of traditional medicine from across the world through modern science and technology to improve the health of people and the planet.
“For many millions of people around the world, traditional medicine is the first port of call to treat many diseases,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “Ensuring all people have access to safe and effective treatment is an essential part of WHO’s mission, and this new center will help to harness the power of science to strengthen the evidence base for traditional medicine. I’m grateful to the Government of India for its support, and we look forward to making it a success.”
The term traditional medicine describes the total sum of the knowledge, skills and practices indigenous and different cultures have used over time to maintain health and prevent, diagnose and treat physical and mental illness. Its reach encompasses ancient practices such as acupuncture, ayurvedic medicine and herbal mixtures as well as modern medicines.
“It is heartening to learn about the signing of the Host Country Agreement for the establishment of Global Centre for Traditional Medicine (GCTM). The agreement between Ministry of Ayush and World Health Organization (WHO) to establish the WHO-GCTM at Jamnagar, Gujarat, is a commendable initiative,” said Narendra Modi, Prime Minister of India. “Through various initiatives, our government has been tireless in its endeavour to make preventive and curative healthcare, affordable and accessible to all. May the global centre at Jamnagar help in providing the best healthcare solutions to the world.”
The new WHO centre will concentrate on building a solid evidence base for policies and standards on traditional medicine practices and products and help countries integrate it as appropriate into their health systems and regulate its quality and safety for optimal and sustainable impact.
The new centre focuses on four main strategic areas: evidence and learning; data and analytics; sustainability and equity; and innovation and technology to optimize the contribution of traditional medicine to global health and sustainable development.
The onsite launch of the new WHO global centre for traditional medicine in Jamnagar, Gujarat, India will take place on April 21, 2022.
__________________________
Of course, one must wait and see who will direct the unit and what work the new centre produces. But I cannot help feeling a little anxious. The press release is full of hot air and platitudes and the track record of the Indian Ministry of Ayush is quite frankly abominable. Here are a few of my previous posts that, I think, justify this statement:
- Mucormycosis (black fungus): is the Indian AYUSH ministry trying to decimate the population?
- The ‘AYUSH COVID-19 Helpline’: have they gone bonkers?
- Individualized Homeopathic Medicines for Cutaneous Warts – the dishonesty of homeopaths continues
- Ever wondered what a homeopathic egg on the face looks like?
- An RCT on the efficacy of ayurvedic treatment on asymptomatic COVID-19 patients
- Has homeopathy caused the dramatic decline of COVID-19 cases in India?
- Eight new products aimed at mitigating COVID-19. But do they really work?
- Siddha doctors have joined those claiming to have found a cure for COVID-19
- COVID-19: homeopathy gone berserk in Mumbai
- Brazil and India collaborate in the promotion of quackery
- Hard to believe: dangerous GOVERNMENTAL advice regarding SCAM for the corona virus pandemic
WATCH THIS SPACE!
Boris Johnson has recently bent over backward in order to please the Indian PM, Narendra Mondi. Some even say that a trade agreement between the two countries was achieved at the cost of letting the Delta variant into the UK. Now it seems that political considerations are at the heart of the decision to lend official support to Indian traditional medicine in the UK. The ‘2030 Roadmap for India-UK future relations‘ is a policy document of the UK government. In it, we find that the UK government intends to:
- Explore cooperation on research into Ayurveda and promote yoga in the UK.
- Increase opportunities for generic medicine supply from India to the UK by seeking access for Indian pharma products to the NHS and recognition of Indian generic and Ayurvedic medicines that meet UK regulatory standards.
This clearly begs the question, are these plans good or bad for UK public health?
Ayurveda is a system of healthcare developed in India around the mid-first millennium BCE. Ayurvedic medicine involves a range of techniques, including meditation, physical exercises, nutrition, relaxation, massage, and medication. Ayurvedic medicine thrives for balance and claims that the suppression of natural urges leads to illness. Emphasis is placed on moderation. Ayurvedic medicines are extremely varied. They usually are mixtures of multiple ingredients and can consist of plants, animal products, and minerals. They often also contain toxic substances, such as heavy metals which are deliberately added in the ancient belief that they can have positive health effects. The truth, however, is that they can cause serious adverse effects.
Relatively few studies of Ayurvedic remedies exist and most are methodologically weak. A Cochrane review, for instance, concluded that” although there were significant glucose-lowering effects with the use of some herbal mixtures, due to methodological deficiencies and small sample sizes we are unable to draw any definite conclusions regarding their efficacy. Though no significant adverse events were reported, there is insufficient evidence at present to recommend the use of these interventions in routine clinical practice and further studies are needed.”
The efficacy of Ayurvedic remedies obviously depends on the exact nature of the ingredients. Generalizations are therefore problematic. Promising findings exist for a relatively small number of ingredients, including Boswellia, Frankincense, Andrographis paniculata.
Yoga has been defined in several different ways in the various Indian philosophical and religious traditions. From the perspective of alternative medicine, it is a practice of gentle stretching exercises, breathing control, meditation, and lifestyles. The aim is to strengthen prana, the vital force as understood in traditional Indian medicine. Thus, it is claimed to be helpful for most conditions affecting mankind. Most people who practice yoga in the West practise ‘Hatha yoga’, which includes postural exercises (asanas), breath control (pranayama), and meditation (dhyana). It is claimed that these techniques bring an individual to a state of perfect health, stillness, and heightened awareness. Other alleged benefits of regular yoga practice include suppleness, muscular strength, feelings of well-being, reduction of sympathetic drive, pain control, and longevity. Yogic breathing exercises are said to reduce muscular spasms, expand available lung capacity and thus alleviate the symptoms of asthma and other respiratory conditions.
There have been numerous clinical trials of various yoga techniques. They tend to suffer from poor study design and incomplete reporting. Their results are therefore not always reliable. Several systematic reviews have summarised the findings of these studies. An overview included 21 systematic reviews relating to a wide range of conditions. Nine systematic reviews arrived at positive conclusions, but many were associated with a high risk of bias. Unanimously positive evidence emerged only for depression and cardiovascular risk reduction (Ernst E, Lee MS: Focus on Alternative and Complementary Therapies Volume 15(4) December 2010 274–27).
Yoga is generally considered to be safe. However, the only large-scale survey specifically addressing the question of adverse effects found that approximately 30% of yoga class attendees had experienced some type of adverse event. Although the majority had mild symptoms, the survey results indicated that attendees with chronic diseases were more likely to experience adverse events associated with their disease. Therefore, special attention is necessary when yoga is introduced to patients with stress-related, chronic diseases.
So, should we be pleased about the UK government’s plan to promote Ayurveda and yoga? In view of the mixed and inconclusive evidence, I feel that a cautious approach would be wise. Research into these subjects could be a good idea, particularly if it were aimed at finding out what the exact risks are. Whole-sale integration does, however, not seem prudent at this stage. In other words, let’s find out what generates more good than harm for which conditions and subsequently consider adopting those elements that fulfill this vital criterium.
Prince Charles has claimed that people struggling to return to full health after having the coronavirus should practice yoga. This is what the GUARDIAN reported about it on Friday:
In a video statement on Friday to the virtual yoga and healthcare symposium Wellness After Covid, the heir apparent said doctors should work together with “complementary healthcare specialists” to “build a roadmap to hope and healing” after Covid. “This pandemic has emphasised the importance of preparedness, resilience and the need for an approach which addresses the health and welfare of the whole person as part of society, and which does not merely focus on the symptoms alone,” Charles said. “As part of that approach, therapeutic, evidenced-informed yoga can contribute to health and healing. By its very nature, yoga is an accessible practice which provides practitioners with ways to manage stress, build resilience and promote healing…”
… Charles, who has previously espoused the benefits of yoga, is not the only fan in the royal family. His wife, the Duchess of Cornwall, has said “it makes you less stiff” and “more supple”, while Prince William has also been pictured doing yogic poses. In 2019, the Prince of Wales said yoga had “proven beneficial effects on both body and mind”, and delivered “tremendous social benefits” that help build “discipline, self-reliance and self-care”.
__________________
END OF QUOTE
Yoga is a complex subject because it entails a host of different techniques, attitudes, and life-styles. There have been numerous clinical trials of various yoga techniques. They tend to suffer from poor study design as well as incomplete reporting and are thus no always reliable. Several systematic reviews have summarised the findings of these studies. A 2010 overview included 21 systematic reviews relating to a wide range of conditions. Nine systematic reviews arrived at positive conclusions, but many were associated with a high risk of bias. Unanimously positive evidence emerged only for depression and cardiovascular risk reduction.[1] There is no evidence that yoga speeds the recovery after COVID-19 or any other severe infectious disease, as Charles suggested.
Yoga is generally considered to be safe. However, a large-scale survey found that approximately 30% of yoga class attendees had experienced some type of adverse event. Although the majority had mild symptoms, the survey results indicated that patients with chronic diseases were more likely to experience adverse events.[2] It, therefore, seems unlikely that yoga is suited for many patients recovering from a COVID-19 infection.
The warning by the Vatican’s chief exorcist that yoga leads to ‘demonic possession’[3] might not be taken seriously by rational thinkers. Yet, experts have long warned that many yoga teachers try to recruit their clients into the more cult-like aspects of yoga.[4]
Perhaps the most remarkable expression in Charles’ quotes is the term ‘EVIDENCE-INFORMED‘. It crops up regularly when Charles (or his advisor Dr. Michael Dixon) speaks or writes about so-called alternative medicine (SCAM). It is a clever term that sounds almost like ‘evidence-based’ but means something entirely different. If a SCAM is not evidence-based, it can still be legitimately put under the umbrella of ‘evidence-informed’: we know the evidence is not positive, we were well-informed of this fact, we nevertheless conclude that yoga (or any other SCAM) might be a good idea!
In my view, the regular use of the term ‘evidence-informed’ in the realm of SCAM discloses a lack of clarity that suits all snake-oil salesmen very well.
[1] Ernst E, Lee MS: Focus on Alternative and Complementary Therapies Volume 15(4) December 2010 274–27
[2] Matsushita T, Oka T. A large-scale survey of adverse events experienced in yoga classes. Biopsychosoc Med. 2015 Mar 18;9:9. doi: 10.1186/s13030-015-0037-1. PMID: 25844090; PMCID: PMC4384376.
[3] https://www.social-consciousness.com/2017/06/vaticans-chief-exorcist-warns-that-yoga-causes-demonic-possession.html
[4] https://www.theguardian.com/lifeandstyle/2020/jun/26/experience-my-yoga-class-turned-out-to-be-a-cult
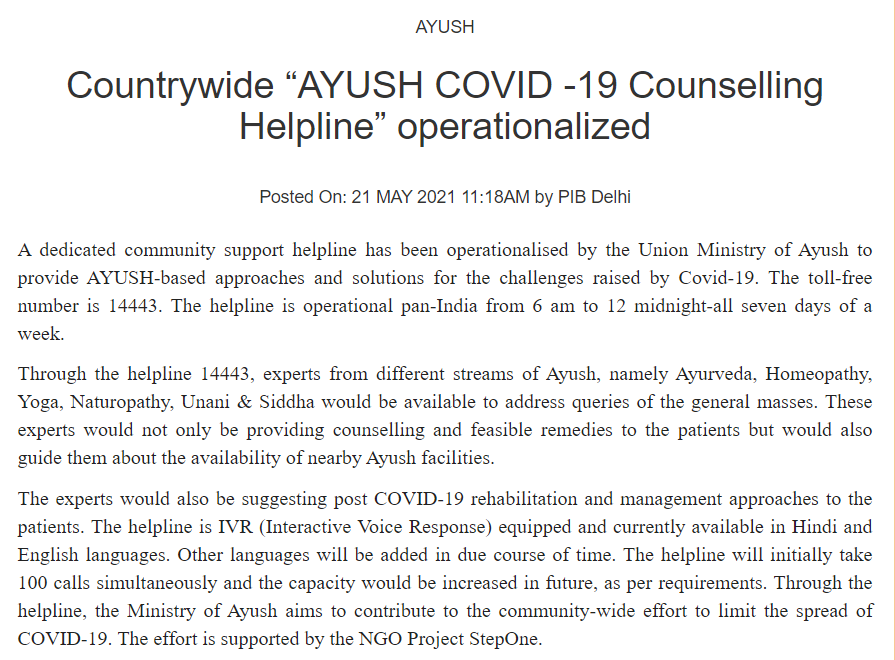
This amazing announcement reached me via Twitter. It seems that the people in the AYUSH ministry are highly delusional. According to Wikipedia, the Ministry of Ayurveda, Yoga, Naturopathy, Unani, Siddha, Sowa-Rigpa and Homoeopathy (abbreviated as AYUSH) is purposed with developing education, research and propagation of indigenous alternative medicine systems in India. As per a recent notification published in the Gazette of India on 13 April 2021, the Ministry of AYUSH (Ayurveda, Yoga & Naturopathy, Unani, Siddha and Homoeopathy), will now be known as the Ministry of Ayush.
India is suffering from a very severe health crisis, and the ministry should stop its propaganda for useless solutions.
- Ayurveda,
- Homeopathy (considered to be indigenous in India),
- Yoga,
- Naturopathy,
- Unani,
- Sidda,
- Sowa-Rigpa (the traditional medicine of Tibet)
have in common that they can offer very little help to patients infected by COVID-19. In view of this fact, the announcement is ununderstandable and irresponsible, in my view.
A new study evaluated the effects of yoga and eurythmy therapy compared to conventional physiotherapy exercises in patients with chronic low back pain.
In this three-armed, multicentre, randomized trial, patients with chronic low back pain were treated for 8 weeks in group sessions (75 minutes once per week). They received either:
- Yoga exercises
- Eurythmy
- Physiotherapy
The primary outcome was patients’ physical disability (measured by RMDQ) from baseline to week 8. Secondary outcome variables were pain intensity and pain-related bothersomeness (VAS), health-related quality of life (SF-12), and life satisfaction (BMLSS). Outcomes were assessed at baseline, after the intervention at 8 weeks, and at a 16-week follow-up. Data of 274 participants were used for statistical analyses.
The results showed no significant differences between the three groups for the primary and secondary outcomes. In all groups, RMDQ decreased comparably at 8 weeks but did not reach clinical meaningfulness. Pain intensity and pain-related bothersomeness decreased, while the quality of life increased in all 3 groups. In explorative general linear models for the SF-12’s mental health component, participants in the eurythmy arm benefitted significantly more compared to physiotherapy and yoga. Furthermore, within-group analyses showed improvements of SF-12 mental score for yoga and eurythmy therapy only. All interventions were safe.
Everyone knows what physiotherapy or yoga is, I suppose. But what is eurythmy?
It is an exercise therapy that is part of anthroposophic medicine. It consists of a set of specific movements that were developed by Rudolf Steiner (1861–1925), the inventor of anthroposophic medicine, in conjunction with Marie von Sievers (1867-1948), his second wife.
Steiner stated in 1923 that eurythmy has grown out of the soil of the Anthroposophical Movement, and the history of its origin makes it almost appear to be a gift of the forces of destiny. Steiner also wrote that it is the task of the Anthroposophical Movement to reveal to our present age that spiritual impulse that is suited to it. He claimed that, within the Anthroposophical Movement, there is a firm conviction that a spiritual impulse of this kind must enter once more into human evolution. And this spiritual impulse must perforce, among its other means of expression, embody itself in a new form of art. It will increasingly be realized that this particular form of art has been given to the world in Eurythmy.
Consumers learning eurythmy are taught exercises that allegedly integrate cognitive, emotional, and volitional elements. Eurythmy exercises are based on speech and direct the patient’s attention to their own perceived intentionality. Proponents of Eurythmy believe that, through this treatment, a connection between internal and external activity can be experienced. They also make many diffuse health claims for this therapy ranging from stress management to pain control.
There is hardly any reliable evidence for eurythmy, and therefore the present study is exceptional and noteworthy. One review concluded that “eurythmy seems to be a beneficial add-on in a therapeutic context that can improve the health conditions of affected persons. More methodologically sound studies are needed to substantiate this positive impression.” This positive conclusion is, however, of doubtful validity. The authors of the review are from an anthroposophical university in Germany. They included studies in their review that were methodologically too weak to allow any conclusions.
So, does the new study provide the reliable evidence that was so far missing? I am afraid not!
The study compared three different exercise therapies. Its results imply that all three were roughly equal. Yet, we cannot tell whether they were equally effective or equally ineffective. The trial was essentially an equivalence study, and I suspect that much larger sample sizes would have been required in order to identify any true differences if they at all exist. Lastly, the study (like the above-mentioned review) was conducted by proponents of anthroposophical medicine affiliated with institutions of anthroposophical medicine. I fear that more independent research would be needed to convince me of the value of eurythmy.
The purpose of this survey (the authors call it a ‘study’) was to evaluate the patient-perceived benefit of yoga for symptoms commonly experienced by breast cancer survivors.
A total of 1,049 breast cancer survivors who had self-reported use of yoga on a follow-up survey, in an ongoing prospective Mayo Clinic Breast Disease Registry (MCBDR), received an additional mailed yoga-focused survey asking about the impact of yoga on a variety of symptoms. Differences between pre-and post- scores were assessed using Wilcoxon Signed Rank Test.
802/1,049 (76%) of women who were approached to participate, consented and returned the survey. 507/802 (63%) reported use of yoga during and/or after their cancer diagnosis. The vast majority of respondents (89.4%) reported some symptomatic benefit from yoga. The most common symptoms that prompted the use of yoga were breast/chest wall pain, lymphedema, and anxiety. Only 9% of patients reported that they had been referred to yoga by a medical professional. While the greatest symptom improvement was reported with breast/chest wall pain and anxiety, significant improvement was also perceived in joint pain, muscle pain, fatigue, headache, quality of life, hot flashes, nausea/vomiting, depression, insomnia, lymphedema, and peripheral neuropathy, (all p-values <0.004).
The authors concluded that data supporting the use of yoga for symptom management after cancer are limited and typically focus on mental health. In this study, users of yoga often reported physical benefits as well as mental health benefits. Further prospective studies investigating the efficacy of yoga in survivorship are warranted.
I have little doubt that yoga is helpful during palliative and supportive cancer care (but all the more doubts that this new paper will further the reputation of research in this area). In fact, contrary to what the conclusions state, there is quite good evidence for this assumption:
- A 2009 systematic review included 10 clinical trials. Its authors concluded that although some positive results were noted, variability across studies and methodological drawbacks limit the extent to which yoga can be deemed effective for managing cancer-related symptoms.
- A 2017 systematic review with 25 clinical trials concluded that among adults undergoing cancer treatment, evidence supports recommending yoga for improving psychological outcomes, with potential for also improving physical symptoms. Evidence is insufficient to evaluate the efficacy of yoga in pediatric oncology.
- A 2017 Cochrane review included 24 studies and found that moderate-quality evidence supports the recommendation of yoga as a supportive intervention for improving health-related quality of life and reducing fatigue and sleep disturbances when compared with no therapy, as well as for reducing depression, anxiety and fatigue, when compared with psychosocial/educational interventions. Very low-quality evidence suggests that yoga might be as effective as other exercise interventions and might be used as an alternative to other exercise programmes.[3]
So, why publish a paper like the one above?
Search me!
To be able to add one more publication to the authors’ lists?
And why would the journal editor go along with this nonsense?
Search me again!
No, hold on: Global Advances in Health and Medicine, the journal that carried the survey, is published in association with Academic Consortium for Integrative Medicine & Health.
Yes, that explains a lot.
As I have pointed out several times before, surveys of this nature are like going into a Mac Donald’s and asking the customers whether they like Hamburgers. You might then also find that “the vast majority of respondents (89.4%) reported”… blah, blah, blah.
The title of the paper is ‘Real-World Experiences With Yoga on Cancer-Related Symptoms in Women With Breast Cancer‘.
PS
NOTE TO MYSELF: never touch a paper with ‘real-world experience’ in the title.