pseudo-science
Static or motion manual palpation tests of the spine are commonly used by chiropractors and osteopaths to assess pain location and reproduction in low back pain (LBP) patients. But how reliable are they?
The purpose of this review was to evaluate the reliability and validity of manual palpation used for the assessment of LBP in adults. The authors systematically searched five databases from 2000 to 2019 and critically appraised the internal validity of studies using QAREL and QUADAS-2 instruments.
A total of 2023 eligible articles were identified, of which 14 were at low risk of bias. Evidence suggests that reliability of soft tissue structures palpation is inconsistent, and reliability of bony structures and joint mobility palpation is poor. Preliminary evidence was found to suggest that gluteal muscle palpation for tenderness may be valid in differentiating LBP patients with and without radiculopathy.
The authors concluded that the reliability of manual palpation tests in the assessment of LBP patients varies greatly. This is problematic because these tests are commonly used by manual therapists and clinicians. Little is known about the validity of these tests; therefore, their clinical utility is uncertain. High quality validity studies are needed to inform the clinical use of manual palpation tests.
I have repeatedly drawn attention to the fact that the diagnostic methods used by chiropractors and osteopaths are of uncertain or disproven validity (see for instance here, or here). Why is that important?
Imagine you consult a chiropractor or osteopath. Simply put, this is what is likely to happen:
- They listen to your complaint.
- They do a few tests which are of dubious validity.
- They give you a diagnosis that is meaningless.
- They treat you with manual therapies that are neither effective nor safe.
- You pay.
- They persuade you that you need many more sessions.
- You pay regularly.
- When eventually your pain has gone away, they persuade you to have useless maintenance treatment.
- You pay regularly.
In a nutshell, they have very little to offer … which explains why they attack everyone who dares to disclose this.
Prior research has generated inconsistent results regarding vaccination rates among patients using so-called alternative medicine (SCAM). Given that SCAM includes a wide range of therapies – about 400 different treatments have been counted – variable vaccination patterns may occur within consultations with different types of SCAM practitioners.
A recent analysis aimed to evaluate differences between categories of SCAM regarding vaccination behavior among US adults.
Data from the 2017 National Health Interview Survey (NHIS; n = 26,742; response rate 80.7%) were used. Prevalences of flu vaccination, consultations with SCAM practitioners in the past 12 months, and their potential interactions were examined. 42.7% of participants had received the flu vaccination in the past 12 months, 32.4% had seen one or more SCAM practitioners. Users of any type of SCAM were as likely as non-users to have received a flu vaccination (44.8% users versus 41.7% non-users; p = 0,862; adjusted odds ratio [AOR] = 1.01, 95% confidence interval [CI] = 0.95–1.07).
Regarding specific SCAM types,
- individuals consulting with naturopaths (p < 0.001; AOR = 0.67, 95 %CI = 0.54–0.82),
- homeopaths (p < 0.001; AOR = 0.55; 95 %CI = 0.44–0.69)
- chiropractors (p = 0.016; AOR = 0.9, 95 %CI = 0.83–0.98)
were less likely to be vaccinated. Other SCAMs showed no significant association with flu vaccination behavior. Independent predictors for a flu shot were prior diabetes, cancer, current asthma, kidney disease, overweight and current pregnancy. As well, higher educational level, age, ethnicity, health insurance coverage, and having seen a general physician or medical specialist in the past 12 months were also associated with a higher vaccination rate.
The authors concluded that SCAM users were equally likely to receive an influenza vaccination compared with non-users. Different SCAM therapies showed varied associations with vaccination behavior. Further analyses may be needed to distinguish influencing factors among patients’ vaccination behavior.
This survey confirms what we have discussed repeatedly on this blog (see, for instance here, here, here, here, and here). The reason why consumers who consult naturopaths, homeopaths, or chiropractors get vaccinated less regularly is presumably that these practitioners tend to advise against vaccinations. And why do they do that?
- Naturopaths claim that vaccines are toxic and their therapeutic options protect against infections.
- Homeopaths claim that vaccines are toxic and their therapeutic options protect against infections.
- Chiropractors claim that vaccines are toxic and their therapeutic options protect against infections.
Do these ‘therapeutic options’ – detox, nosodes, spinal manipulation – have anything in common?
Yes, they are bogus!
Conclusion:
Many naturopaths, homeopaths, and chiropractors seem to be a risk to public health.
It has recently been reported that a Canadian naturopath claims he can treat autism with fecal transplants at a clinic in Mexico. The College of Naturopathic Physicians of B.C. has thus barred him stating that it has taken “extraordinary action” against Jason Klop in response to a complaint from a whistle-blowing former employee, who alleges that he manufactured these products in a “household lab” in B.C. without standard procedures or quality control.
While the complaint is under investigation, Klop cannot manufacture, advertise or sell fecal microbiota transplants (FMT). He’ll also be subject to random on-site audits to make sure he’s not violating his conditions.
This is the first public sign of concrete action by the college since CBC News reported on Klop’s business in January 2020 — nearly 20 months ago. Klop has been charging about $15,000 US for autistic children as young as two years old to have FMT treatment at a clinic near Tijuana. The process isn’t approved as a treatment of autism and carries serious risks of infection.
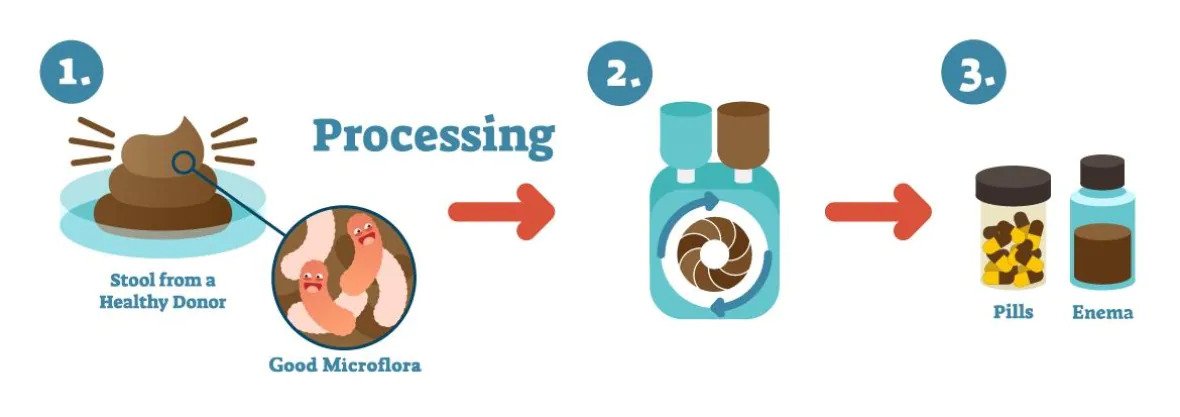
An illustration shows how fecal microbiota transplants are produced. (Vancouver Island Health Authority)
In a promotional video posted in January, Klop says he believes that “precision manipulation of the gut microbiome will solve every single chronic disease.” He also issued an affidavit boasting that he has a new lab that “produces the best and safest FMT materials in the world” and described the former employee who complained as “manifestly unreliable.” Klop argued that “lives are at stake” if he were to stop what he’s doing and described his therapy as a “life-saving measure.”
_____________________
Is there any evidence at all for FMT as a treatment of autism? A recent systematic review drew this conclusion: evidence from human studies suggesting beneficial effects of probiotic, prebiotic, and combination thereof, as well as fecal transplants in autism spectrum disorder, is limited and inconclusive.
Diabetic polyneuropathy is a prevalent, potentially disabling condition. Evidence-based treatments include specific anticonvulsants and antidepressants for pain management. All current guidelines advise a personalized approach with a low-dose start that is tailored to the maximum response having the least side effects or adverse events. Homeopathy has not been shown to be effective, but it is nevertheless promoted by many homeopaths as an effective therapy.
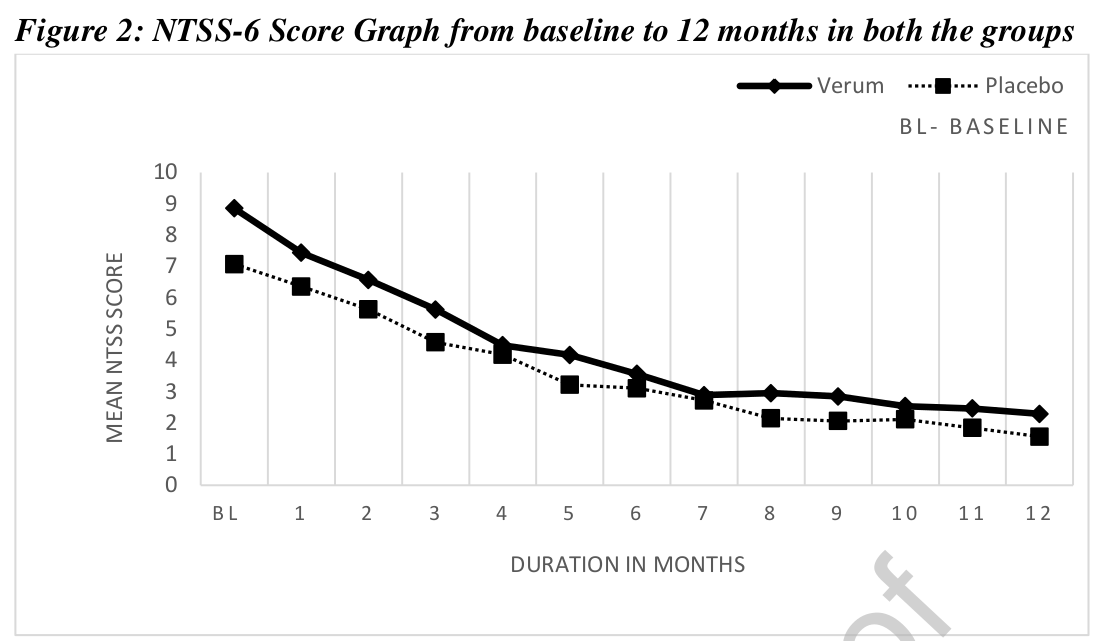
This study assessed the efficacy of individualized homeopathic medicines in the management of diabetic polyneuropathy. A multi-centric double-blind, placebo-controlled, randomized clinical trial was conducted by the Indian Central Council for Research in Homoeopathy at six centers with a sample size of 84. Based on earlier observational studies and repertorial anamnesis of DDSP symptoms 15 homeopathic medicines were shortlisted and validated scales were used for evaluating the outcomes post-intervention. The primary outcome measure was a change in Neuropathy Total Symptom Score-6 (NTSS-6) from baseline to 12 months. Secondary outcomes included changes in peripheral nerve conduction study (NCS), World Health Organization Quality of Life BREF (WHOQOL-BREF) and Diabetic Neuropathy Examination (DNE) score at 12 months.
Data of 68 enrolled cases were considered for data analysis. A statistically significant difference (p<0.014) was found in NTSS-6 post-intervention in the Verum group. A positive trend was noted for the Verum group as per the graph plotted for DNE score and assessment done for NCS. No significant difference was found between the groups for WHOQOL-Bref. Out of 15 pre-identified homeopathic medicines, 11 medicines were prescribed in potencies in ascending order from 6C to 1M.
The authors refrain from drawing conclusions about the efficacy of their homeopathic treatment (which is more than a little odd, as their stated aim was to assess the efficacy of individualized homeopathic medicines in the management of diabetic polyneuropathy). So, please allow me to do it for them:
The findings of this study confirm that homeopathy is a useless treatment.
This study aimed to assess the feasibility of a future definitive trial, with a preliminary assessment of differences between effects of individualized homeopathic (IH) medicines and placebos in the treatment of cutaneous warts.
A double-blind, randomized, placebo-controlled trial (n = 60) was conducted at the dermatology outpatient department of the Homoeopathic Medical College and Hospital, West Bengal. Patients were randomized to receive either IH (n = 30) or identical-looking placebos (n = 30). The primary outcome measures were numbers and sizes of warts; the secondary outcome measure was the Dermatology Life Quality Index (DLQI) questionnaire measured at baseline, and every month up to 3 months. Group differences and effect sizes were calculated on the intention-to-treat sample.
Attrition rate was 11.6% (IH, 3; placebo, 4). Intra-group changes were significantly greater in the IH group than in the placebo group. Inter-group differences were statistically non-significant (all p > 0.05, Mann-Whitney U tests) with small effect sizes, both in the primary outcomes (number of warts after 3 months: IH median [interquartile range; IQR] 1 [1, 3] vs. placebo 1 [1, 2]; p = 0.741; size of warts after 3 months: IH 5.6 mm [2.6, 40.2] vs. placebo 6.3 [0.8, 16.7]; p = 0.515) and in the secondary outcomes (DLQI total after 3 months: IH 4.5 [2, 6.2] vs. placebo 4.5 [2.5, 8]; p = 0.935). Thuja occidentalis (28.3%), Natrum muriaticum (10%), and Sulphur (8.3%) were the most frequently prescribed medicines. No homeopathic aggravations or serious adverse events were reported.
The authors concluded that, as regards efficacy, the preliminary study was inconclusive, with a statistically non-significant direction of effect favoring homeopathy. The trial succeeded in showing that an adequately powered definitive trial is both feasible and warranted.
Partly the same group of authors recently published another trial of homeopathy with similar findings. At the time, I commented as follows:
We have come across this terminology before; homeopaths seem to like it. It prevents them from calling a negative trial by its proper name: A NEGATIVE TRIAL. In their view
- a positive trial is a study where homeopathy yields better results than placebo,
- a negative trial is a study where placebo yields better results than homeopathy,
- an inconclusive trial is a study where homeopathy yields results that are not significantly different from placebo.
Is this silly?
Yes, it is completely bonkers!
Is it dishonest?
Yes, in my view, it is.
Why is it done nonetheless?
Perhaps a glance at the affiliations of the authors provides an answer. And here is the list of the affiliations of the trialists of the present cutaneous wart study:
- 1Department of Repertory, D.N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 2D.N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 3Department of Organon of Medicine and Homoeopathic Philosophy, The Calcutta Homoeopathic Medical College and Hospital, Kolkata, West Bengal, India.
- 4Department of Practice of Medicine, The Calcutta Homoeopathic Medical College and Hospital, Kolkata, West Bengal, India.
- 5Department of Repertory, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Kolkata, West Bengal, India.
- 6Department of Organon of Medicine and Homoeopathic Philosophy, D.N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 7Department of Pediatrics, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 8Department of Organon of Medicine and Homoeopathic Philosophy, State National Homoeopathic Medical College and Hospital, Lucknow, Uttar Pradesh.
- 9Independent Researcher; Champsara, Baidyabati, Hooghly, West Bengal, India.
- 10Independent Researcher, Shibpur, Howrah, West Bengal, India.
And, as before, this paper also contains this statement:
Conflict of interest statement
None declared.
Pre-hypertension, or stage 1 hypertension as it is also called, is usually defined as a systolic pressure reading between 120 mmHg and 139 mmHg, or a diastolic reading between 80 mmHg and 89 mmHg. It remains a significant public health challenge and appropriate intervention is required to stop its progression to hypertension and cardiovascular diseases.
This double-blind, randomized, two parallel arms, placebo-controlled study tested the effects of individualized homeopathic medicines (IH) against placebo in intervening with the progression of pre-hypertension to hypertension.
Ninety-two patients with pre-hypertension were randomized to receive either IH (n = 46) or identical-looking placebo (n = 46). Both IH or placebo were applied in the mutual context of lifestyle modification (LSM) advice including dietary approaches to stop hypertension (DASH) and brisk exercises.
The primary endpoints were systolic and diastolic blood pressures (SBP and DBP); secondary endpoints were Measure Yourself Medical Outcome Profile version 2.0 (MYMOP-2) scores. All endpoints were measured at baseline, and every month, up to 3 months.
After 3 months of intervention, the number of patients having progression from pre-hypertension to hypertension between groups was similar without any significant differences in between the groups. Reduction in BP and MYMOP-2 scores were also not significantly different. Lycopodium clavatum, Thuja occidentalis and Natrum muriaticum were the most frequently prescribed medicines. No serious adverse events were reported from either group.
The authors concluded that there was a small, but non-significant direction of effect favoring homeopathy, which ultimately rendered the trial as inconclusive.
We have come across this terminology before; homeopaths seem to like it. It prevents them from calling a negative trial by its proper name: A NEGATIVE TRIAL. In their view
- a positive trial is a study where homeopathy yields better results than placebo,
- a negative trial is a study where placebo yields better results than homeopathy,
- an inconclusive trial is a study where homeopathy yields results that are not significantly different from placebo.
Is this silly?
Yes, it is completely bonkers!
Is it dishonest?
Yes, in my view, it is.
Why is it done nonetheless?
Perhaps a glance at the affiliations of the authors provides an answer:
- 1Dept. of Organon of Medicine and Homoeopathic Philosophy, D. N. De Homoeopathic Medical College and Hospital, Kolkata, West Bengal, affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India. Electronic address: [email protected].
- 2Dept. of Organon of Medicine and Homoeopathic Philosophy, D. N. De Homoeopathic Medical College and Hospital, Kolkata, West Bengal, affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India.
- 3Principal and Administrator D. N. De Homoeopathic Medical College and Hospital, Kolkata, West Bengal, affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India.
- 4Dept. of Practice of Medicine, D. N. De Homoeopathic Medical College and Hospital, Kolkata, West Bengal, affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India.
- 5Dept. of Practice of Medicine, Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, Howrah, Govt. of West Bengal, affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India.
- 6Dept. of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Block GE, Sector III, Salt Lake, Kolkata 700106, West Bengal, India; affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India.
- 7Dept. of Organon of Medicine and Homoeopathic Philosophy, State National Homoeopathic Medical College and Hospital, Lucknow, Govt. of Uttar Pradesh, affiliated to Dr. Bhimrao Ramji Ambedkar University, Agra, Govt. of Uttar Pradesh), India.
- 8Dept. of Repertory, D. N. De Homoeopathic Medical College and Hospital, Kolkata, West Bengal, affiliated to The West Bengal University of Health Sciences, Govt. of West Bengal, India.
Despite these multiple conflicts of interest, the article carries this note:
“Declaration of Competing Interest: None declared.”
During the last few days, we were entertained by one of the more fanatical specimen of the lunatic fringe. From the outset, ‘ASTRO’ was out to provoke, insult, and foremost state utter nonsense. Within just a few hours ‘ASTRO’ posted dozens of comments, one more hilarious than the next.
As always, I let it pass for a while because this sort of thing usually is very amusing and mildly instructive. Then, when my fun was over, I told him or her that my conversation with him or her was finished, thereafter I sent ‘ASTRO’ my usual hint to indicate that my patience was wearing thin (an overdose of nonsense, fun, and hilarity might be toxic) and now I have blocked ‘ASTRO’.
This little incident is a mere triviality, of course. Yet, it is also a most welcome reminder to demonstrate what is needed to get blocked by me. Here are a few selected ‘bon mots’ posted by ‘ASTRO’ which all contributed to his or her dismissal from this blog:
- Lenny is an intellectual terrorist
- you manipulate data
- you are nobody in the scientific world
- I’m very sorry for your lack of education
- I don’t hate you for lying, I pity you
- With all sincerity, and seeing that you don’t have a single scientific publication, I recommend that mounts a business for atheists resentful and sell cheap products with the face of Carl Sagan or James Randi in a coffe cup or pins, I assure you that the media will make of your business, earn some money and you’ll be able to publish a book trash like Ben Goldacre, with his “Bad science” or the Steven Novella. Poor quality is a typical sign of skeptical pseudoscientists.
- your “letter to the editor” is based on manipulating data and making false accusations, everything
- you only have an opinion based on your belief and denial that may well be a projection of your lack of knowledge
- I’m disappointed that you have very superficial knowledge, no wonder Mathie will ignore you
- Your comments again reflect that you haven’t the slightest idea
- your lack of reading comprehension is evident
- You are very ignorant
- your aggressiveness and lack of empathy tell a lot about your profile of atheist resentful of life
- these” verdicts ” that Ernst quotes in his pamphlets are at best a fraud
- in reality you, Grams and the team of the anti-homeopathy propaganda network have no idea what you’re talking about
- Ernst,” friend, ” you’re still pretty aggressive, maybe you need some joy in your life. Now I understand why the pseudoscientific skeptical atheist community is so childish and so toxic
- anyone who questions Edzar’s sacred dogmas is a troll
- Thank you for confirming that you are a sectarian
- your obsessive behavior borders on harassment
- Magazines like Skepter are very popular with immature gentlemen who believe they are the world or with teenagers who are just out of college who believe that science is done with whims
- don’t be like Lenny and try to grow up
- real science is in the objective pursuit and not in harassment campaigns orchestrated by a few clowns who believe James Randi is unquestionable
- every time I read your entries I feel sorry that your level of logic is so low and lousy
- Your naivety and superficial knowledge in philosophy of science (and that of most of those who follow you) is very pitiful
- you are the example of a pseudo-sceptic, a rude and cowardly skeptic who can’t tolerate criticism
- your friends are a sect, possibly a group based on coertion
- it doesn’t look like “Lenny” has a single scientific article published, not to mention your colleagues in the “About” section that the few who look like scientists are mediocre in their fields, the rest are small-time activists. No wonder, so much envy, so much anger, so much hatred, that’s what leaves fanatical atheism. They’re talibans of science, not scientists
- you with your age presume a lot and I only see you being interviewed by mainstream media that talk nonsense against homeopathy
- You had to control that aggressiveness, you feel more nervous and angry, maybe you’re a relative of the troll Lenny
- The obsessive behavior of Aust trying to refute Frass already looks like that of a stalker, similar of the journalist Christian Kreil who invented a whole string of nonsense in a German public media trying to link Frass to a questionable company, the media does not even mention Frass’s refutation to Kreil
One thing we cannot accuse ‘ASTRO’ of is that he or she was not industrious. You might ask why I did not stop his aggressive stupidity earlier after it had stopped being funny. Perhaps I should have – but, to be honest, these trolls do amuse me a great deal. More importantly, they might teach us important lessons:
- The fun one can have with fanatics is usually short-lasted.
- Some weirdos are very well misinformed, i.e. they read a lot and misunderstand even more.
- The minds of heavily deluded people are beyond productive discussions.
- Any hope to educate them will be disappointed.
- If we allow them to, they swiftly make themselves ridiculous.
- Their pseudo-arguments are strikingly similar.
- Their aggressiveness can be considerable.
And finally, the little ‘ASTRO’ interlude tells you something else:
It really does need a lot to get banned from my blog.
Guest post by Norbert Aust and Viktor Weisshäupl
Imagine you recently published an excellent and rigorous trial providing solid evidence that a certain therapy is able to help patients suffering from some inevitably fatal condition. You proved that your therapy is able to significantly prolong the patients’ lifetime, much longer than with the current state-of-the-art therapeutic approach. But the patients not only live considerably longer, but they also do so with a much better quality of life (QoL) and subjective well-being. In short: this therapy marks some progress that would otherwise take years or decades of scientific effort.
And then someone comes forward and points out your data apparently were manipulated. Essential parameters of this trial were modified sometime after data collection was completed, with the patients’ outcome and first analyses available. Thus the results were biased in a certain direction and the critics show that the results as published in your study show characteristics that such manipulations would evoke. After all, this holds an implication of scientific misconduct that could, if verified, ruin your academic reputation more or less completely.
What would you do?
Ignore the preposterous concerns because you know your methods and performance were rigorous and solid? After all, anytime some real academic criticism arises you are ready to prove your findings are well-founded results of accepted scientific methods. Or would you publish data or documents that your critics were too ignorant to find or to understand, and thus to stop such rumours once and for all? Maybe you could even clarify some of the issues raised by those critics, maybe add some follow-up information or data to ensure no more misunderstandings occur. Or would you try to find some clues for a libel lawsuit?
Well, we thought some of the above would happen after we contacted the authors of the recent study on adjunct homeopathy in non-small cell lung cancer. On that date, we forwarded our detailed analysis to the lead author and all the co-authors.
Of course, we even considered the possibility, not very likely though, that we would receive some explanation for the numerous exclusion criteria while other serious conditions that coincide with advanced age did not preclude enrollment. Or an updated CONSORT diagram accounting for the patients excluded. Or some explanation just why the numerous amendments to the protocol were necessary but not important enough to mention them in the published paper.
But nothing of this happened as yet (July 2021). Instead on June 14 and 16, 2021, not two weeks after our messages to the authors, the registration data at ClinicalTrials were updated once again and a new version of the protocol was uploaded [3]. And this update looks pretty much like it is meant to cover up and blur the former data that we based our analysis on. Of course, these data and the former version of the protocol are available still – just one layer further down, and you have to scroll to the bottom of the page to find the small link “history of changes”. Maybe not many visitors will do that.
In contrast to the versions before, now the uploaded data are in line with the study as published, namely, they include a full list of the exclusion criteria and the reduced observation time for QoL, which was the primary outcome. Note: throughout the trial until the end of data assessment those parameters were set with pregnancy as the only exclusion criterion and two years follow up time, only to be amended in the protocol uploaded two months after data collection was complete and analysis presumably was well underway.
In addition, there is a new version of the study protocol, this one dated Feb. 6, 2014. Of course, this protocol is fairly new, in spite of the date it carries. Why would the older version allegedly from January 2011 be uploaded to the register in September 2019, if this more actual version already had existed and was available?
Contrary to the prior version all the clues are removed that would indicate that this document was finished at a much later point in time than given in its date: References to some future software versions that were released years after the protocol was allegedly compiled are dropped. And this strange literature reference “25” that corresponds to the reference list in the final study as published but is pointless in the protocol without any reference list, is removed too. And of course, again contrary to the prior version, the exclusion criteria are identical with the final study as is the shortened follow-up time for QoL.
New to the protocol is a section “Bringing in the patient’s voice”, where the authors disclose how they want to “systematically research the ethical, legal, socio-political, and science theoretical dimensions of homeopathy as in the case of lung cancer (non-small-cell lung carcinoma) exemplified” in some “integral social scientific study”, where some “focus groups” of 4 to 10 participants together with their relatives, friends and caregivers included should be used to study “interactions between individuals, collectively shared and uncontested assumptions, and the emergence of collective meaning”.
But from all of this more or less meaningless but very sciency sounding socio-speak, not a single word found its way into the study. Nothing. So it is pointless to try to figure out what the content of this part of the investigation is all about.
Why then was this chapter added? This “integral social scientific study” was to start after the “third or fourth homeopathic treatment” (But why should patients not be included in this “research” from the very first beginning?). Is it perhaps to give some rationale why the follow-up time for QoL was to end after the third homeopathic treatment?
So what we see, when we look up the study at ClinicalTrials now, is a perfectly matching set of data and a protocol that corresponds to the study as published and looks as if it was published at a time where the trial was underway and the patients were still blinded. If you do not look very closely everything now appears to be perfect.
And here we would like to forward some critique to the register: The purpose of the study register is to prevent not only publication bias but misleading manipulation from happening as well. They do quite a good job in preserving former versions of data and documents and keeping them available to the public. Many national study registers do not offer this service. But you must be of a suspicious mind and of some persistence to actively search and find and check the history of modifications. Thus, a cover-up like the one we are witnessing here might well prove successful. We, therefore, propose to improve the presentation of the registration: If vital amendments occurred that may affect the outcomes – such as protocol changes, extensions of exclusion criteria, modifications of follow-up time – this should be indicated upfront in the study’s record instead of some small hint to “history of changes” at the very bottom of the page.
In conclusion, there appears to be no proof that the results of the study were produced using rigorous scientific methods. And the issues we raised in our report to the authors remain unresolved.
This multicenter, randomized, sham-controlled trial was aimed at assessing the long-term efficacy of acupuncture for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Men with moderate to severe CP/CPPS were recruited, regardless of prior exposure to acupuncture. They received sessions of acupuncture or sham acupuncture over 8 weeks, with a 24-week follow-up after treatment. Real acupuncture treatment was used to create the typical de qi sensation, whereas the sham acupuncture treatment (the authors state they used the Streitberger needle, but the drawing looks more as though they used our device) does not generate this feeling.
The primary outcome was the proportion of responders, defined as participants who achieved a clinically important reduction of at least 6 points from baseline on the National Institutes of Health Chronic Prostatitis Symptom Index at weeks 8 and 32. Ascertainment of sustained efficacy required the between-group difference to be statistically significant at both time points.
A total of 440 men (220 in each group) were recruited. At week 8, the proportions of responders were:
- 60.6% (95% CI, 53.7% to 67.1%) in the acupuncture group
- 36.8% (CI, 30.4% to 43.7%) in the sham acupuncture group (adjusted difference, 21.6 percentage points [CI, 12.8 to 30.4 percentage points]; adjusted odds ratio, 2.6 [CI, 1.8 to 4.0]; P < 0.001).
At week 32, the proportions were:
- 61.5% (CI, 54.5% to 68.1%) in the acupuncture group
- 38.3% (CI, 31.7% to 45.4%) in the sham acupuncture group (adjusted difference, 21.1 percentage points [CI, 12.2 to 30.1 percentage points]; adjusted odds ratio, 2.6 [CI, 1.7 to 3.9]; P < 0.001).
Twenty (9.1%) and 14 (6.4%) adverse events were reported in the acupuncture and sham acupuncture groups, respectively. No serious adverse events were reported. No significant difference was found in changes in the International Index of Erectile Function 5 score at all assessment time points or in peak and average urinary flow rates at week 8.
The authors concluded that, compared with sham therapy, 20 sessions of acupuncture over 8 weeks resulted in greater improvement in symptoms of moderate to severe CP/CPPS, with durable effects 24 weeks after treatment.
The study was sponsored by the China Academy of Chinese Medical Sciences and the National Administration of Traditional Chinese Medicine. The trialists originate from the following institutions:
- 1Guang’anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China (Y.S., B.L., Z.Q., J.Z., J.W., X.L., W.W., R.P., H.C., X.W., Z.L.).
- 2Key Laboratory of Chinese Internal Medicine of Ministry of Education, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China (Y.L.).
- 3ThedaCare Regional Medical Center – Appleton, Appleton, Wisconsin (K.Z.).
- 4Hengyang Hospital Affiliated to Hunan University of Chinese Medicine, Hengyang, China (Z.Y.).
- 5The First Hospital of Hunan University of Chinese Medicine, Changsha, China (W.Z.).
- 6Guangdong Provincial Hospital of Traditional Chinese Medicine, Guangzhou, China (W.F.).
- 7The First Affiliated Hospital of Anhui University of Chinese Medicine, Hefei, China (J.Y.).
- 8West China Hospital of Sichuan University, Chengdu, China (N.L.).
- 9China Academy of Chinese Medical Sciences, Beijing, China (L.H.).
- 10Yantai Hospital of Traditional Chinese Medicine, Yantai, China (Z.Z.).
- 11Shaanxi Provincial Hospital of Traditional Chinese Medicine, Xi’an, China (T.S.).
- 12The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, China (J.F.).
- 13Beijing Fengtai Hospital of Integrated Traditional and Western Medicine, Beijing, China (Y.D.).
- 14Xi’an TCM Brain Disease Hospital, Xi’an, China (H.S.).
- 15Dongfang Hospital Beijing University of Chinese Medicine, Beijing, China (H.H.).
- 16Luohu District Hospital of Traditional Chinese Medicine, Shenzhen, China (H.Z.).
- 17Guizhou University of Traditional Chinese Medicine, Guiyang, China (Q.M.).
These facts, together with the previously discussed notion that clinical trials from China are notoriously unreliable, do not inspire confidence. Moreover, one might well wonder about the authors’ claim that patients were blinded. As pointed out above, the real and sham acupuncture were fundamentally different: the former did generate de qi, while the latter did not! A slightly pedantic point is my suspicion that the trial did not test the efficacy but the effectiveness of acupuncture, if I am not mistaken. Finally, one might wonder what the rationale of acupuncture as a treatment of CP/CPPS might be. As far as I can see, there is no plausible mechanism (other than placebo) to explain the effects.
So, is the evidence that emerged from the new study convincing?
No, in my view, it is not!
In fact, I am surprised that a journal as reputable as the Annals of Internal Medicine published it.
Weleda, the firm founded by Rudolf Steiner and Ita Wegman originally for producing and selling their anthroposophic remedies, celebrates its 100th anniversary. It is a truly auspicious occasion for which I feel compelled to offer a birthday present.
I hope they like it!
On the Weleda UK website, we find an article entitled ‘ An introduction to Homeopathy‘ which contains the following statements:
- Homeopathy works by stimulating the body’s own natural healing capacity. The remedy triggers the body’s own healing forces and so a remedy is prescribed on a very individual basis.
- If you do experience complex, persistent or worrying symptoms then please seek the advice of a doctor who specialises in homeopathy.
- Today there are four homeopathic hospitals offering treatment under the National Health Service – in London, Glasgow, Liverpool and Bristol.
- It’s still the only alternative medicine incorporated into the NHS.
- Homeopathy can be used to treat the same wide range of illness as conventional medicine, and may even prove successful when all other forms of treatment have failed.
- Over-the-counter homeopathic medicines are made using natural plant, mineral and, occasionally, animal substances
- … active elements are in infinitesimally small quantities.
As I understand a bit about the subject – not as much as my friend Dana Ullman, of course, but evidently more than the Weleda team – I thought I might offer them, as a birthday present, a free correction of these 7 passages. Here we go:
- Homeopathy is claimed to work by stimulating the body’s own natural healing capacity. In fact, it does not work. Yet, believers argue that the remedy triggers the body’s own healing forces and so a remedy is prescribed on a very individual basis.
- If you do experience complex, persistent or worrying symptoms then please seek the advice of a doctor who specializes in something other than homeopathy.
- Today there are no homeopathic hospitals offering treatment under the National Health Service – the ones in London, Glasgow, Liverpool, and Bristol all closed or changed their names.
- It’s no longer incorporated into the NHS.
- Homeopathy cannot be used to treat the same wide range of illnesses as conventional medicine and is not successful when all other forms of treatment have failed.
- Over-the-counter homeopathic medicines are made using any imaginable substance and even non-material stuff like vacuum or X-rays.
- … active elements are absent.
HAPPY BIRTHDAY, WELEDA!