osteopathy
When I first saw this, I was expecting something like If Homeopathy Beats Science (Mitchell and Webb) – YouTube : videos (reddit.com). But no, “Acute Care Homeopathy for Medical Professionals” is not a masterpiece by gifted satirists. It is much better; it is for real! In fact, it is a collaboration between the “Academy of Homeopathy Education” (AHE) and the American Institute of Homeopathy (AIH). Together, they published the following announcement:
Education” (AHE) and the American Institute of Homeopathy (AIH). Together, they published the following announcement:
AHE and AIH are pleased to present a customized educational program designed for busy medical professionals interested in enhancing their practice and expanding the treatment tools available with Homeopathy. Grounded in the original theory and philosophy of Homeopathy, AHE’s quality curriculum empowers practitioners and the material’s inspirational delivery encourages further study towards the mastery of Homeopathy for chronic care.
This course is open to all licensed healthcare providers— medical, osteopathic, naturopathic, dentists, chiropractors, veterinarians, nurse practitioners, nurses, physician assistants, pharmacologists and pharmacists.
Acute-care homeopathy addresses the challenges of 21st-century medical practice.
Among many things, you’ll learn safe and effective ways to manage pain and mitigate antibiotic overuse with FDA-regulated and approved Homeopathic remedies. AHE delivers an integrated learning experience that combines online real-time classroom experiences culminating in a telehealth based clinical internship allowing participants to study from anywhere in the world.
AHE’s team of Homeopathy experts have taught thousands of students around the globe and are known for unparalleled academic rigor, comprehensive clinical training, and robust research initiatives. AHE ensures that every graduate develops the necessary critical thinking skills in homeopathy case taking, analysis, and prescribing to succeed in practice with confidence and competence.
- Smart and savvy tech support team helps to on-board and train even the most reticent digital participants
- Academic support professionals provide an educational safety-net
- Stellar faculty to inspire confidence and encourage students to achieve their best work
- “Fireside Chats,” forums, and social gatherings build community
- Tried and true administrative systems keep things running smoothly so you can focus on learning Homeopathy.
All AHE students receive Radar Opus, the leading software package used by professional homeopaths worldwide.
Upon completion of the didactic program, practitioners begin an Acute Care Internship through AHE and the Homeopathy Help Network’s Acute Care Telehealth Clinic “Homeopathy Help Now” (HHN) which sees thousands of cases each year. Upon successful completion of the internship, practitioners will be invited to participate in ongoing supervised practice through HHN.
AHE is part of a larger vision to shape the future of Homeopathy: HOHM Foundation and the Homeopathy Help NetworkAll clinical services are delivered in an education and research-driven model. HOHM’s Office of Research has multiple peer-reviewed publications focused on education, practice, and clinical outcomes. HOHM is committed to funding Homeopathy study and research at every level.
The Academy of Homeopathy Education (AHE) operates in conjunction with HOHM Foundation, a 501c3 initiative committed to education, advocacy, and access. The Homeopathy Help Network is a telehealth clinic providing fee-for-service chronic care as well as donation-based acute care through Homeopathy Help Now.
____________________________
I suspect you simply cannot wait to enroll. To learn more about “Acute Care Homeopathy for Medical Professionals” please fill out the form.
… and don’t forget to pay the fee of US$ 5 500.
No, it’s not expensive, if you think about it. After all, acute-care homeopathy addresses the challenges of 21st-century medical practice.
Naprapathy is an odd variation of chiropractic. To be precise, it has been defined as a system of specific examination, diagnostics, manual treatment, and rehabilitation of pain and dysfunction in the neuromusculoskeletal system. It is aimed at restoring the function of the connective tissue, muscle- and neural tissues within or surrounding the spine and other joints. The evidence that it works is wafer-thin. Therefore rigorous studies are of interest.
The aim of this study was to evaluate the cost-effectiveness of manual therapy compared with advice to stay active for working-age persons with nonspecific back and/or neck pain.
The two interventions were:
- a maximum of 6 manual therapy sessions within 6 weeks, including spinal manipulation/mobilization, massage, and stretching, performed by a naprapath (index group),
- information from a physician on the importance to stay active and on how to cope with pain, according to evidence-based advice, on 2 occasions within 3 weeks (control group).
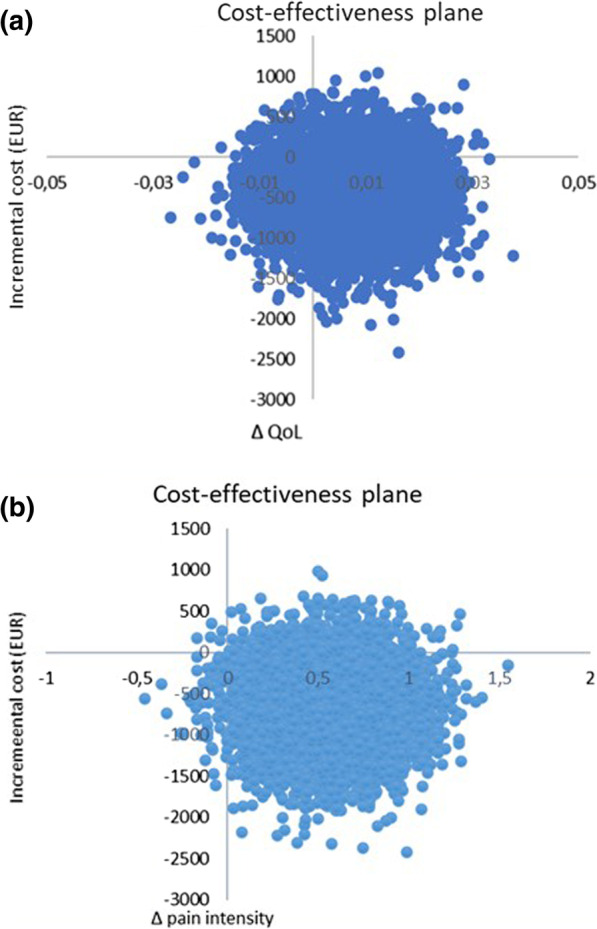
A cost-effectiveness analysis with a societal perspective was performed alongside a randomized controlled trial including 409 persons followed for one year, in 2005. The outcomes were health-related Quality of Life (QoL) encoded from the SF-36 and pain intensity. Direct and indirect costs were calculated based on intervention and medication costs and sickness absence data. An incremental cost per health-related QoL was calculated, and sensitivity analyses were performed.
The difference in QoL gains was 0.007 (95% CI – 0.010 to 0.023) and the mean improvement in pain intensity was 0.6 (95% CI 0.068-1.065) in favor of manual therapy after one year. Concerning the QoL outcome, the differences in mean cost per person were estimated at – 437 EUR (95% CI – 1302 to 371) and for the pain outcome the difference was – 635 EUR (95% CI – 1587 to 246) in favor of manual therapy. The results indicate that manual therapy achieves better outcomes at lower costs compared with advice to stay active. The sensitivity analyses were consistent with the main results.
Cost-effectiveness plane using bootstrapped incremental cost-effectiveness ratios for QoL and pain intensity outcomes
The authors concluded that these results indicate that manual therapy for nonspecific back and/or neck pain is slightly less costly and more beneficial than advice to stay active for this sample of working age persons. Since manual therapy treatment is at least as cost-effective as evidence-based advice from a physician, it may be recommended for neck and low back pain. Further health economic studies that may confirm those findings are warranted.
This is an interesting and well-conducted study. The differences between the groups seem small and of doubtful relevance. The authors acknowledge this fact by stating: “together with the clinical results from previously published studies on the same population the results suggest that manual therapy may be as cost-effective a treatment as evidence-based advice from a physician, for back and neck pain”. Moreover, the data do not convince me that the treatment per se was effective; it might have been the non-specific effects of touch and attention.
I have said it before: there is currently no optimal treatment for neck and back pain. Therefore, the findings even of rigorous cost-effectiveness studies will only generate lukewarm results.
This study used a US nationally representative 11-year sample of office-based visits to physicians from the National Ambulatory Medical Care Survey (NAMCS), to examine a comprehensive list of factors believed to be associated with visits where complementary health approaches were recommended or provided.
NAMCS is a national health care survey designed to collect data on the provision and use of ambulatory medical care services provided by office-based physicians in the United States. Patient medical records were abstracted from a random sample of office-based physician visits. The investigators examined several visit characteristics, including patient demographics, physician specialty, documented health conditions, and reasons for a health visit. They ran chi-square analyses to test bivariate associations between visit factors and whether complementary health approaches were recommended or provided to guide the development of logistic regression models.
Of the 550,114 office visits abstracted, 4.43% contained a report that complementary health approaches were ordered, supplied, administered, or continued. Among complementary health visits, 87% of patient charts mentioned nonvitamin nonmineral dietary supplements. The prevalence of complementary health visits significantly increased from 2% in 2005 to almost 8% in 2015. Returning patient status, survey year, physician specialty and degree, menopause, cardiovascular, and musculoskeletal diagnoses were significantly associated with complementary health visits, as was seeking preventative care or care for a chronic problem.
The authors concluded that these data confirm the growing popularity of complementary health approaches in the United States, provide a baseline for further studies, and inform subsequent investigations of integrative health care.
The authors used the same dataset for a 2nd paper which examined the reasons why office-based physicians do or do not recommend four selected complementary health approaches to their patients in the context of the Andersen Behavioral Model. Descriptive estimates were employed of physician-level data from the 2012 National Ambulatory Medical Care Survey (NAMCS) Physician Induction Interview, a nationally representative survey of office-based physicians (N = 5622, weighted response rate = 59.7%). The endpoints were the reasons for the recommendation or lack thereof to patients for:
- herbs,
- other non-vitamin supplements,
- chiropractic/osteopathic manipulation,
- acupuncture,
- mind-body therapies (including meditation, guided imagery, and progressive relaxation).
Differences by physician sex and medical specialty were described.
For each of the four complementary health approaches, more than half of the physicians who made recommendations indicated that they were influenced by scientific evidence in peer-reviewed journals (ranging from 52.0% for chiropractic/osteopathic manipulation [95% confidence interval, CI = 47.6-56.3] to 71.3% for herbs and other non-vitamin supplements [95% CI = 66.9-75.4]). More than 60% of all physicians recommended each of the four complementary health approaches because of patient requests. A higher percentage of female physicians reported evidence in peer-reviewed journals as a rationale for recommending herbs and non-vitamin supplements or chiropractic/osteopathic manipulation when compared with male physicians (herbs and non-vitamin supplements: 78.8% [95% CI = 72.4-84.3] vs. 66.6% [95% CI = 60.8-72.2]; chiropractic/osteopathic manipulation: 62.3% [95% CI = 54.7-69.4] vs. 47.5% [95% CI = 42.3-52.7]).
For each of the four complementary health approaches, a lack of perceived benefit was the most frequently reported reason by both sexes for not recommending. Lack of information sources was reported more often by female versus male physicians as a reason to not recommend herbs and non-vitamin supplements (31.4% [95% CI = 26.8-36.3] vs. 23.4% [95% CI = 21.0-25.9]).
The authors concluded that there are limited nationally representative data on the reasons as to why office-based physicians decide to recommend complementary health approaches to patients. Developing a more nuanced understanding of influencing factors in physicians’ decision making regarding complementary health approaches may better inform researchers and educators, and aid physicians in making evidence-based recommendations for patients.
I am not sure what these papers really offer in terms of information that is not obvious or that makes a meaningful contribution to progress. It almost seems that, because the data of such surveys are available, such analyses get done and published. The far better reason for doing research is, of course, the desire to answer a burning and relevant research question.
A problem then arises when researchers, who perceive the use of so-called alternative medicine (SCAM) as a fundamentally good thing, write a paper that smells more of SCAM promotion than meaningful science. Having said that, I find it encouraging to read in the two papers that
- the prevalence of SCAM remains quite low,
- more than 60% of all physicians recommended SCAM not because they were convinced of its value but because of patient requests,
- the lack of perceived benefit was the most frequently reported reason for not recommending it.
Osteopathic visceral manipulation (VM) is a bizarre so-called alternative medicine (SCAM) that has been featured on this blog with some regularity, e.g.:
- Osteopathic visceral manipulation: a new study fails to convince anyone
- Visceral manipulation…you couldn’t make it up
- Intravaginal manipulations by (German) osteopaths: a new low point for clinical research into alternative medicine?
- Visceral osteopathy is implausible and does not work … SO, LET’S FORGET ABOUT IT ONCE AND FOR ALL
Rigorous trials fail to show that it works for anything. So, the obvious solution to this dilemma is to conduct dodgy trials!
This study tested the effects of VM on dysmenorrhea, irregular, delayed, and/or absent menses, and premenstrual symptoms in PCOS patients.
Thirty Egyptian women with polycystic ovary syndrome (PCOS), with menstruation-related complaints and free from systematic diseases and/or adrenal gland abnormalities, participated in a single-blinded, randomized controlled trial. They were recruited from the women’s health outpatient clinic in the faculty of physical therapy at Cairo University, with an age of 20-34 years, and a body mass index (BMI) ≥25, <30 kg/m2. Patients were randomly allocated into two equal groups (15 patients); the control group received a low-calorie diet for 3 months, and the study group that received the same hypocaloric diet added to VM to the pelvic organs and their related structures for eight sessions over 3 months. Evaluations for body weight, BMI, and menstrual problems were done by weight-height scale, and menstruation-domain of Polycystic Ovary Syndrome Health-Related Quality of Life Questionnaire (PCOSQ), respectively, at baseline and after 3 months from interventions. Data were described as mean, standard deviation, range, and percentage whenever applicable.
Of 60 Egyptian women with PCOS, 30 patients were included, with baseline mean age, weight, BMI, and a menstruation domain score of 27.5 ± 2.2 years, 77.7 ± 4.3 kg, 28.6 ± 0.7 kg/m2, and 3.4 ± 1.0, respectively, for the control group, and 26.2 ± 4.7 years, 74.6 ± 3.5 kg, 28.2 ± 1.1 kg/m2, and 2.9 ± 1.0, respectively, for the study group. Out of the 15 patients in the study group, uterine adhesions were found in 14 patients (93.3%), followed by restricted uterine mobility in 13 patients (86.7%), restricted ovarian/broad ligament mobility (9, 60%), and restricted motility (6, 40%). At baseline, there was no significant difference (p>0.05) in any of the demographics (age, height), or dependent variables (weight, BMI, menstruation domain score) among both groups. Post-study, there was a statistically significant reduction (p=0.000) in weight, and BMI mean values for the diet group (71.2 ± 4.2 kg, and 26.4 ± 0.8 kg/m2, respectively) and the diet + VM group (69.2 ± 3.7 kg; 26.1 ± 0.9 kg/m2, respectively). For the improvement in the menstrual complaints, a significant increase (p<0.05) in the menstruation domain mean score was shown in the diet group (3.9 ± 1.0), and the diet + VM group (4.6 ± 0.5). On comparing both groups post-study, there was a statistically significant improvement (p=0.024) in the severity of menstruation-related problems in favor of the diet + VM group.
The authors concluded that VM yielded greater improvement in menstrual pain, irregularities, and premenstrual symptoms in PCOS patients when added to caloric restriction than utilizing the low-calorie diet alone in treating that condition.
WHERE TO START?
- Tiny sample size.
- A trail design (A+B vs B) which will inevitably generate a positive result.
- Questionable ethics.
VM is a relatively invasive and potentially embarrassing intervention for any woman; I imagine that this is all the more true in Egypt. In such circumstances, it is mandatory to ask whether a planned study is ethically justifiable. I would answer this question related to an implausible treatment like VM with a straight NO!
I realize that there may be people who disagree with me. But even those guys should accept that, at the very minimum, such a study must be designed such that it leads to a clear answer – is VM effective or not? The present trial merely suggests that the placebo effect associated with VM is powerful (which is hardly surprising for a therapy like VM).
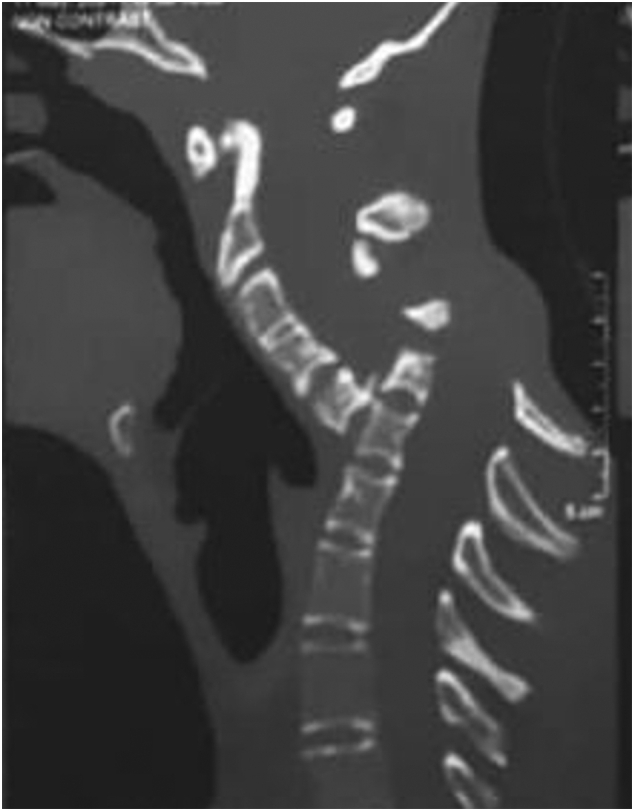
Spondyloptosis is a grade V spondylolisthesis – a vertebra having slipped so far with respect to the vertebra below that the two endplates are no longer congruent. It is usually seen in the lower lumbar spine but rarely can be seen in other spinal regions as well. Spondyloptosis is most commonly caused by trauma. It is defined as the dislocation of the spinal column in which the spondyloptotic vertebral body is either anteriorly or posteriorly displaced (>100%) on the adjacent vertebral body. Only a few cases of cervical spondyloptosis have been reported. The cervical cord injury in most patients is complete and irreversible. In most cases of cervical spondyloptosis, regardless of whether there is a neurologic deficit or not, reduction and stabilization of the fracture-dislocation is the management of choice
The case of a 16-year-old boy was reported who had been diagnosed with spondyloptosis of the cervical spine at the C5-6 level with a neurologic deficit following cervical manipulation by a traditional massage therapist. He could not move his upper and lower extremities, but the sensory and autonomic function was spared. The pre-operative American Spinal Cord Injury Association (ASIA) Score was B with SF-36 at 25%, and Karnofsky’s score was 40%. The patient was disabled and required special care and assistance.
The surgeons performed anterior decompression, cervical corpectomy at the level of C6 and lower part of C5, deformity correction, cage insertion, bone grafting, and stabilization with an anterior cervical plate. The patient’s objective functional score had increased after six months of follow-up and assessed objectively with the ASIA Impairment Scale (AIS) E or (excellent), an SF-36 score of 94%, and a Karnofsky score of 90%. The patient could carry on his regular activity with only minor signs or symptoms of the condition.
The authors concluded that this case report highlights severe complications following cervical manipulation, a summary of the clinical presentation, surgical treatment choices, and a review of the relevant literature. In addition, the sequential improvement of the patient’s functional outcome after surgical correction will be discussed.
This is a dramatic and interesting case. Looking at the above pre-operative CT scan, I am not sure how the patient could have survived. I am also not aware of previous similar cases. This does, however, not mean they don’t exist. Perhaps most affected patients simply died without being diagnosed. So, do we need to add spondyloptosis to the (hopefully) rare but severe complications of spinal manipulation?
During the last two years, I have written more often than I care to remember about the numerous links between so-called alternative medicine (SCAM) and COVID-19 vaccination hesitancy. For instance:
- A Professor for Integrative and Anthroposophical Medicine claims that severe adverse effects of COVID vaccinations are 40 times more frequent than officially recognized
- What are the reasons for opposing COVID vaccinations?
- A naturopath promoting fake news about COVID vaccinations
- COVID-19 vaccinations: Prof Walach wants to “dampen the enthusiasm by sober facts”
- A change in diet protects us from severe COVID symptoms – REALLY?
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- Upper Bavaria is struggling with COVID-19, not least due to so-called alternative medicine
- The International Chiropractors Association’s Statement on Vaccination
- Parents’ Willingness to Vaccinate with a COVID-19 Vaccine: strongly influenced by homeopathy
- “The uncensored truth” about COVID-19 vaccines” … as told by some chiro loons
- Ex-doctor Andrew Wakefield: “Better to die as a free man than live as a slave” (and get vaccinated against Covid-19)
- Is this the crown of the Corona-idiocy? Nosodes In Prevention And Management Of COVID -19
- The rejection of so-called alternative medicine is associated with a higher willingness to get vaccinated
Whenever I publish a post on these subjects, some enthusiasts of SCAM argue that, despite all this evidence, they are not really against COVID vaccinations. But who is correct? What proportions of SCAM practitioners are pro or contra? One way to find out is to check how they themselves behave. Do they get vaccinated or not?
Here are some recent data from Canada that seem to provide an answer.
A breakdown of vaccination rates among Canadian healthcare professions has been released, based on data gathered from 17 of B.C.’s 18 regulated colleges. The findings are most revealing:
- dieticians, physicians, and surgeons lead the way, with vaccination rates of 98%,
- occupational therapists were at 97%,
- Chinese medicine practitioners and acupuncturists were at 79%,
- chiropractors at 78%
- naturopaths at 69%.
The provincial health officer Dr. Bonnie Henry said the province is still working with the colleges on how to notify patients about their practitioner’s vaccination status. “We are working with each college on how to build it into professional standards. The overriding principle is patient status,” she told a news conference. “It may be things like when you call to book, you are asked whether you would prefer to see a vaccinated or unvaccinated professional. We are trying to protect privacy and provide agency to make the decision.”
______________________
As far as I am aware, these are unique data. It would be interesting to see additional evidence. If anyone knows about vaccination rates in other countries of acupuncturists, herbalists, homeopaths, osteopaths, Heilpraktiker, etc. I would love to learn more.
I just stumbled over a paper we published way back in 1997. It reports a questionnaire survey of all primary care physicians working in the health service in Devon and Cornwall. Here is an excerpt:
Replies were received from 461 GPs, a response rate of 47%. A total of 314 GPs (68%, range 32-85%) had been involved in complementary medicine in some way during the previous week. One or other form of complementary medicine was practised by 74 of the respondents (16%), the two most common being homoeopathy (5.9%) and acupuncture (4.3%). In addition, 115 of the respondents (25%) had referred at least one patient to a complementary therapist in the previous week, and 253 (55%) had endorsed or recommended treatment with complementary medicine. Chiropractic, acupuncture and osteopathy were rated as the three most effective therapies, and the majority of respondents believed that these three therapies should be funded by the health service. A total of 176 (38%) respondents reported adverse effects, most commonly after manipulation.
What I found particularly interesting (and had totally forgotten about) were the details of these adverse effects: Serious adverse effects of spinal manipulation included the following:
- paraplegia,
- spinal cord transection,
- fractured vertebra,
- unspecified bone fractures,
- fractured neck of femur,
- severe pain for years after manipulation.
Adverse effects not related to manipulation included:
- death after a coffee enema,
- liver toxicity,
- anaphylaxis,
- 17 cases of delay of adequate medical attention,
- 11 cases of adverse psychological effects,
- 14 cases of feeling to have wasted money.
If I remember correctly, none of the adverse effects had been reported anywhere which would make the incidence of underreporting 100% (exactly the same as in a survey we published in 2001 of adverse effects after spinal manipulations).
Today is WORLD ASTHMA DAY, a good opportunity perhaps to revisit a few of our own evaluations of so-called alternative medicine (SCAM) for asthma. Here are the abstracts of some of our systematic reviews on the subject:
Objective: The objective of this systematic review was to assess the effectiveness of yoga as a treatment option for asthma.
Method: Seven databases were searched from their inception to October 2010. Randomized clinical trials (RCTs) and non-randomized clinical trials (NRCTs) were considered, if they investigated any type of yoga in patients with asthma. The selection of studies, data extraction, and validation were performed independently by two reviewers.
Results: Six RCTs and one NRCT met the inclusion criteria. Their methodological quality was mostly poor. Three RCTs and one NRCT suggested that yoga leads to a significantly greater reduction in spirometric measures, airway hyperresponsivity, dose of histamine needed to provoke a 20% reduction in forced expiratory volume in the first second, weekly number of asthma attacks, and need for drug treatment. Three RCTs showed no positive effects compared to various control interventions.
Conclusions: The belief that yoga alleviates asthma is not supported by sound evidence. Further, more rigorous trials are warranted.
Some clinicians believe that spinal manipulation is an effective treatment for asthma. The aim of this systematic review was to critically evaluate the evidence for or against this claim. Four electronic databases were searched without language restrictions from their inceptions to September 2008. Bibliographies and departmental files were hand-searched. The methodological quality of all included studies was assessed with the Jadad score. Only randomised clinical trials of spinal manipulation as a treatment of asthma were included. Three studies met these criteria. All of them were of excellent methodological quality (Jadad score 5) and all used sham-manipulation as the control intervention. None of the studies showed that real manipulation was more effective than sham-manipulation in improving lung function or subjective symptoms. It is concluded that, according to the evidence of the most rigorous studies available to date, spinal manipulation is not an effective treatment for asthma.
Contradictory results from randomised controlled trials of acupuncture in asthma suggest both a beneficial and detrimental effect. The authors conducted a formal systematic review and meta-analysis of all randomised clinical trials in the published literature that have compared acupuncture at real and placebo points in asthma patients. The authors searched for trials published in the period 1970-2000. Trials had to measure at least one of the following objective outcomes: peak expiratory flow rate, forced expiratory volume in one second (FEV1) and forced vital capacity. Estimates of the standarised mean difference, between acupuncture and placebo were computed for each trial and combined to estimate the overall effect. Hetereogeneity was investigated in terms of the characteristics of the individual studies. Twelve trials met the inclusion criteria but data from one could not be obtained. Individual patient data were available in only three. Standardised differences between means ranging from 0.071 to 0.133, in favour of acupuncture, were obtained. The overall effect was not conventionally significant and it corresponds to an approximate difference in FEV1 means of 1.7. After exploring hetereogenenity, it was found that studies where bronchoconstriction was induced during the experiment showed a conventionally significant effect. This meta-analysis did not find evidence of an effect of acupuncture in reducing asthma. However, the meta-analysis was limited by shortcomings of the individual trials, in terms of sample size, missing information, adjustment of baseline characteristics and a possible bias against acupuncture introduced by the use of placebo points that may not be completely inactive. There was a suggestion of preferential publication of trials in favour of acupuncture. There is an obvious need to conduct a full-scale randomised clinical trial addressing these limitations and the prognostic value of the aetiology of the disease.
Background: Emotional stress can either precipitate or exacerbate both acute and chronic asthma. There is a large body of literature available on the use of relaxation techniques for the treatment of asthma symptoms. The aim of this systematic review was to determine if there is any evidence for or against the clinical efficacy of such interventions.
Methods: Four independent literature searches were performed on Medline, Cochrane Library, CISCOM, and Embase. Only randomised clinical trials (RCTs) were included. There were no restrictions on the language of publication. The data from trials that statistically compared the treatment group with that of the control were extracted in a standardised predefined manner and assessed critically by two independent reviewers.
Results: Fifteen trials were identified, of which nine compared the treatment group with the control group appropriately. Five RCTs tested progressive muscle relaxation or mental and muscular relaxation, two of which showed significant effects of therapy. One RCT investigating hypnotherapy, one of autogenic training, and two of biofeedback techniques revealed no therapeutic effects. Overall, the methodological quality of the studies was poor.
Conclusions: There is a lack of evidence for the efficacy of relaxation therapies in the management of asthma. This deficiency is due to the poor methodology of the studies as well as the inherent problems of conducting such trials. There is some evidence that muscular relaxation improves lung function of patients with asthma but no evidence for any other relaxation technique.
Background: Asthma is one of the most common chronic diseases in modern society and there is increasing evidence to suggest that its incidence and severity are increasing. There is a high prevalence of usage of complementary medicine for asthma. Herbal preparations have been cited as the third most popular complementary treatment modality by British asthma sufferers. This study was undertaken to determine if there is any evidence for the clinical efficacy of herbal preparations for the treatment of asthma symptoms.
Methods: Four independent literature searches were performed on Medline, Pubmed, Cochrane Library, and Embase. Only randomised clinical trials were included. There were no restrictions on the language of publication. The data were extracted in a standardised, predefined manner and assessed critically.
Results: Seventeen randomised clinical trials were found, six of which concerned the use of traditional Chinese herbal medicine and eight described traditional Indian medicine, of which five investigated Tylophora indica. Three other randomised trials tested a Japanese Kampo medicine, marihuana, and dried ivy leaf extract. Nine of the 17 trials reported a clinically relevant improvement in lung function and/or symptom scores.
Conclusions: No definitive evidence for any of the herbal preparations emerged. Considering the popularity of herbal medicine with asthma patients, there is urgent need for stringently designed clinically relevant randomised clinical trials for herbal preparations in the treatment of asthma.
Breathing techniques are used by a large proportion of asthma sufferers. This systematic review was aimed at determining whether or not these interventions are effective. Four independent literature searches identified six randomized controlled trials. The results of these studies are not uniform. Collectively the data imply that physiotherapeutic breathing techniques may have some potential in benefiting patients with asthma. The safety issue has so far not been addressed satisfactorily. It is concluded that too few studies have been carried out to warrant firm judgements. Further rigorous trials should be carried out in order to redress this situation.
__________________________________
So, if you suffer from asthma, my advice is to stay away from SCAM. This might be easier said than done because SCAM practitioners are only too willing to lure asthma patients into their cult. In 2003, we have demonstrated this phenomenon by conducting a survey with chiropractors. Here is our short paper in full:
Classic chiropractic theory claims that vertebral subluxation blocks the flow of ‘‘innate intelligence’’ which, in turn, affects the health of asthma patients (1). Chiropractictors often use spinal manipulation (SM) to correct such malalignments and treat asthma (2). Several clinical trials of chiropractic SM exist, but the most rigorous ones are clearly negative (3,4). Chronic medication with corticosteroids can lead to osteoporosis, a condition, which is a contra-indication to chiropractic SM (5). Given this background, we aimed to determine whether chiropractors would advise an asthma patient on long-term corticosteroids (5 years) to try chiropractic as a treatment for this condition.
All 350 e-mail addresses listed at www.interadcom.com/chiro/html were randomised into two groups. A (deceptive) letter from a (fictitious) patient was sent to group A while group B was asked for advice on chiropractic treatment for asthma as part of a research project. Thus, groups A and B were asked the same question in di¡erent contexts: is chiropractic safe and e¡ective for an asthma patient on long-term steroids. After data collection, respondents from group A were informed that the e-mail had been part of a research project.
Of 97 e-mails in group A, we received 31 responses (response rate = 32% (95% CI, 0.23^ 0.41)). Seventy-four per cent (23 respondents) recommended visiting a chiropractor (95% CI, 0.59^ 0.89). Thirty-five per cent (11 respondents) mentioned minimal or no adverse effects of SM (95% CI, 0.18 ^ 0.52). Three chiropractors responded that some adverse e¡ects exist, e.g. risk of bone fracture, or stroke. Two respondents noted that other investigations (X-rays, spinal and neurological examination) were required before chiropractic treatment. Three respondents suggested additional treatments and one warned about a possible connection between asthma and the measles vaccine. Of 77 e-mails sent to group B, we received 16 responses (response rate = 21% (95% CI, 0.17^ 0.25)). Eleven respondents (69%) recommended visiting a chiropractor (95% CI, 0.46 ^ 0.91). Ten respondents mentioned minimal or no adverse effects of SM (95% CI, 0.39^ 0.87). Five chiropractors responded that adverse effects of SM exist (e.g. bone fracture). Five respondents suggested pre-testing the patient to check bone density, allergy, diet, exercise level, hydration and blood. Additional treatments were recommended by three respondents. The pooled results of groups A and B suggested that the majority of chiropractors recommend chiropractic treatment for asthma and the minority mention any adverse effects.
Our results demonstrate that chiropractic advice on asthma therapy is as readily available over the Internet as it is likely to be misleading. The majority of respondents from both groups (72%) recommended chiropractic treatment. This usually entails SM, a treatment modality which has been demonstrated to be ineffective in rigorous clinical trials (3,4,6). The advice may also be dangerous: the minority of the respondents of both groups (17%) caution of the risk of bone fracture. Our findings also suggest that, for the research question asked, a degree of deception is necessary. The response rate in group B was 12% lower than that of group A, and the answers received differed considerably between groups. In group A, 10% acknowledged the possibility of adverse e¡ects, this figure was 33% in group B. In conclusion, chiropractors readily provide advice regarding asthma treatment, which is often not evidence-based and has the potential to put patients at risk.
__________________________
As I stated above: if you suffer from asthma, my advice is to
stay away from SCAM.
The objective of this study was to compare chronic low back pain patients’ perspectives on the use of spinal manipulative therapy (SMT) compared to prescription drug therapy (PDT) with regard to health-related quality of life (HRQoL), patient beliefs, and satisfaction with treatment.
Four cohorts of Medicare beneficiaries were assembled according to previous treatment received as evidenced in claims data:
- The SMT group began long-term management with SMT but no prescribed drugs.
- The PDT group began long-term management with prescription drug therapy but no spinal manipulation.
- This group employed SMT for chronic back pain, followed by initiation of long-term management with PDT in the same year.
- This group used PDT for chronic back pain followed by initiation of long-term management with SMT in the same year.
A total of 1986 surveys were sent out and 195 participants completed the survey. The respondents were predominantly female and white, with a mean age of approx. 77-78 years. Outcome measures used were a 0-to-10 numeric rating scale to measure satisfaction, the Low Back Pain Treatment Beliefs Questionnaire to measure patient beliefs, and the 12-item Short-Form Health Survey to measure HRQoL.
Recipients of SMT were more likely to be very satisfied with their care (84%) than recipients of PDT (50%; P = .002). The SMT cohort self-reported significantly higher HRQoL compared to the PDT cohort; mean differences in physical and mental health scores on the 12-item Short Form Health Survey were 12.85 and 9.92, respectively. The SMT cohort had a lower degree of concern regarding chiropractic care for their back pain compared to the PDT cohort’s reported concern about PDT (P = .03).
The authors concluded that among older Medicare beneficiaries with chronic low back pain, long-term recipients of SMT had higher self-reported rates of HRQoL and greater satisfaction with their modality of care than long-term recipients of PDT. Participants who had longer-term management of care were more likely to have positive attitudes and beliefs toward the mode of care they received.
The main issue here is that the ‘study’ was a mere survey which by definition cannot establish cause and effect. The groups were different in many respects which rendered them not comparable. For instance, participants who received SMT had higher self-reported physical and mental health on average than those who received PDT. Differences also existed between the SMT and the PDT groups for agreement with the notion that “spinal manipulation for LBP makes a lot of sense”; 96% of the SMT group and 35% of the PDT group agreed with it. Compare this with another statement, “taking /having prescription drug therapy for LBP makes a lot of sense” and we find that only 13% of the SMT cohort agreed with, 95% of the PDT cohort agreed. Thus, a powerful bias exists toward the type of therapy that each person had chosen. Another determinant of the outcome is the fact that SMT means hands-on treatments with time, compassion, and empathy given to the patient, whereas PDT does not necessarily include such features. Add to these limitations the dismal response rate, recall bias, and numerous potential confounders and you have a survey that is hardly worth the paper it is printed on. In fact, it is little more than a marketing exercise for chiropractic.
In summary, the findings of this survey are influenced by a whole range of known and unknown factors other than the SMT. The authors are clever to avoid causal inferences in their conclusions. I doubt, however, that many chiropractors reading the paper think critically enough to do the same.
This study describes the use of so-called alternative medicine (SCAM) among older adults who report being hampered in daily activities due to musculoskeletal pain. The characteristics of older adults with debilitating musculoskeletal pain who report SCAM use is also examined. For this purpose, the cross-sectional European Social Survey Round 7 from 21 countries was employed. It examined participants aged 55 years and older, who reported musculoskeletal pain that hampered daily activities in the past 12 months.
Of the 4950 older adult participants, the majority (63.5%) were from the West of Europe, reported secondary education or less (78.2%), and reported at least one other health-related problem (74.6%). In total, 1657 (33.5%) reported using at least one SCAM treatment in the previous year.
The most commonly used SCAMs were:
- manual body-based therapies (MBBTs) including massage therapy (17.9%),
- osteopathy (7.0%),
- homeopathy (6.5%)
- herbal treatments (5.3%).
SCAM use was positively associated with:
- younger age,
- physiotherapy use,
- female gender,
- higher levels of education,
- being in employment,
- living in West Europe,
- multiple health problems.
(Many years ago, I have summarized the most consistent determinants of SCAM use with the acronym ‘FAME‘ [female, affluent, middle-aged, educated])
The authors concluded that a third of older Europeans with musculoskeletal pain report SCAM use in the previous 12 months. Certain subgroups with higher rates of SCAM use could be identified. Clinicians should comprehensively and routinely assess SCAM use among older adults with musculoskeletal pain.
I often mutter about the plethora of SCAM surveys that report nothing meaningful. This one is better than most. Yet, much of what it shows has been demonstrated before.
I think what this survey confirms foremost is the fact that the popularity of a particular SCAM and the evidence that it is effective are two factors that are largely unrelated. In my view, this means that more, much more, needs to be done to inform the public responsibly. This would entail making it much clearer:
- which forms of SCAM are effective for which condition or symptom,
- which are not effective,
- which are dangerous,
- and which treatment (SCAM or conventional) has the best risk/benefit balance.
Such information could help prevent unnecessary suffering (the use of ineffective SCAMs must inevitably lead to fewer symptoms being optimally treated) as well as reduce the evidently huge waste of money spent on useless SCAMs.