case-control study
The purpose of this recent investigation was to evaluate the association between chiropractic utilization and use of prescription opioids among older adults with spinal pain … at least this is what the abstract says. The actual paper tells us something a little different: The objective of this investigation was to evaluate the impact of chiropractic utilization upon the use of prescription opioids among Medicare beneficiaries aged 65 plus. That sounds to me much more like trying to find a CAUSAL relationship than an association.
Anyway, the authors conducted a retrospective observational study in which they examined a nationally representative multi-year sample of Medicare claims data, 2012–2016. The study sample included 55,949 Medicare beneficiaries diagnosed with spinal pain, of whom 9,356 were recipients of chiropractic care and 46,593 were non-recipients. They measured the adjusted risk of filling a prescription for an opioid analgesic for up to 365 days following the diagnosis of spinal pain. Using Cox proportional hazards modeling and inverse weighted propensity scoring to account for selection bias, they compared recipients of both primary care and chiropractic to recipients of primary care alone regarding the risk of filling a prescription.
The adjusted risk of filling an opioid prescription within 365 days of initial visit was 56% lower among recipients of chiropractic care as compared to non-recipients (hazard ratio 0.44; 95% confidence interval 0.40–0.49).
The authors concluded that, among older Medicare beneficiaries with spinal pain, use of chiropractic care is associated with significantly lower risk of filling an opioid prescription.
The way this conclusion is formulated is well in accordance with the data. However, throughout the paper, the authors imply that chiropractic care is the cause of fewer opioid prescriptions. For instance: The observed advantage of early chiropractic care mirrors the results of a prior study on a population of adults aged 18–84. The suggestion is that chiropractic saves patients from taking opioids.
It does not need a lot of fantasy to guess why some people might want to create this impression. I am sure that chiropractors would be delighted if the US public felt that their manipulations were the solution to the opioid crisis. For many months, they have been trying hard enough to pretend this is true. Yet, I know of no convincing data to demonstrate it.
The new investigation thus turns out to be a lamentable piece of pseudo research. Retrospective case-control studies can obviously not establish cause and effect, particularly if they do not even account for the severity of the symptoms or the outcomes of the treatment.
Fish and omega-3 polyunsaturated fatty acids (PUFA) have been suggested to play a role in improving cancer prognosis. However, results from epidemiological studies remain inconsistent. A new systematic review was aimed at creating clarity by assessing the association between dietary fish and/or omega-3 PUFAs intake and cancer prognosis. For this purpose, the authors conducted a meta-analysis of observational studies.
A systematic search of related publications was performed using PubMed and Web of Science databases. Hazard ratios (HR) and 95% confidence intervals (CI) were extracted and then pooled using a random-effect model. Potential linear and non-linear dose-response relationships were explored using generalized least squares estimation and restricted cubic splines.
As a result, 21 cohort studies were included in the analysis. Compared to the lowest category, the highest category of fish intake was associated with a significant lower mortality in patients with ovarian cancer (n = 1, HR = 0.74, 95% CI: 0.57-0.95) and overall cancer (n = 12, HR = 0.87, 95% CI: 0.81-0.94). Marine omega-3 PUFAs intake rather than total omega-3 PUFAs intake showed significant protective effects on survival of overall cancer (n = 8, HR = 0.81, 95% CI: 0.71-0.94), in particular prostate cancer (n = 2, HR = 0.62, 95% CI: 0.46-0.82).
Yes, correlation is not causation, I know. This is all the more important, as the mechanism of action of PUFAs in relation to cancer seems speculative at present. On the other hand, causality is rendered more likely by a dose-response meta-analysis. It indicated a nonlinear and a linear relationship between fish intake, as well as marine omega-3 PUFAs intake, and overall cancer survival, respectively.
Thus I feel that the conclusion drawn by the authors is reasonable: our analysis demonstrated a protective effect of dietary fish and marine omega-3 PUFAs consumption on cancer survival.
As you know, I am not in the habit of telling personal stories on this blog. Today, allow me to make an exception by taking you back 40 years into my own history.
Back in the 1980s, I spent much of my time doing research in hemorheology (flow properties of blood). At the time, this was a buoyant area of research, and my late friend Arpad Matrai and I were enthusiastically investigating it, first in London under John Dormandy and later at the LMU in Munich. But we were by no means the only team working in hemorheology. Another group at Aachen was much larger, better-funded, and in many ways way ahead of us. One member of that group regularly irritated us; this was Holger Kiesewetter, the ‘hero’ of my story.
Arpad was sure that much of Kiesewetter’s work and even more of his financial dealings were suspect (“How come a junior research can afford driving a Porsche?”, he used to wonder). Something did not seem quite right. Despite our reservations, we did collaborate occasionally. In 1984, we even managed to co-organize a conference and jointly publish its proceedings.
After my friend and co-worker Arpad had died of leukemia, I gradually drifted back into clinical medicine, became a professor of rehab medicine first in Hannover and then in Vienna. This also meant that I completely lost touch with Holger Kiesewetter. I was, therefore, more than a little surprised to one day receive a phone call from him in Vienna. He told me that he had applied for a professorship at my Uni and asked me to support his application. I did not promise to do so and I certainly did not lend my support to his application. Quite simply, I remembered too many instances that gave me reasons to be concerned about my ‘friend’s’ integrity.
Kiesewetter did not get the Vienna post but I later learned that he had become a professor of transfusion medicine at the Charite in Berlin. In the mid-1990s, a chance meeting at an airport occurred when we were both catching flights. He told me that he was doing fine, and he seemed to have his fingers in many pies.
Then I lost sight of him completely.
Until yesterday, that is.
I was doing some searches on herbal remedies when I came across the intriguing subject of ‘BIO VIAGRA‘. A German article reported this:
“In clinical trials, 50 men had much better sex afterward, more fun in bed, and just generally felt better about themselves,” the Sueddeutsche Zeitung daily cited Olaf Schroeder from Berlin’s Charite hospital as saying. “Their libido was even higher than the control group taking Viagra,” he said. The potent cocktail includes tribulus terrestris, a herb already used in alternative medicine, a root vegetable found in the Andes called maca and grape juice extract, newspapers said. The treatment, dubbed “Plantagrar”, is due to be launched in early 2010, the Bild daily said.
Having published a review of maca, I was interested and continued searching.
Another article stated that a certain Mr. Schröder had stated that he had investigated the efficacy of the remedy on 50 test persons. However, the data of the experiment have not been published. In addition, the researchers’ procedure has been massively criticized: 25 men were given the bio-potency drug, 25 others a placebo, i.e. a tablet without active ingredients. Afterward, the test persons were to compare their experiences with those they had had with Viagra. Fritz Sörgel, director of the Nuremberg Institute for Biomedical and Pharmaceutical Research, calls the procedure “completely dubious”. “This is a completely new kind of study that this doctoral student has invented.” The number of test persons is much too low, the comparison with Viagra cannot be taken seriously.
This sounded already quite dodgy, and a third article in the usually reliable German Medical Journal provided more details:
For several months, those involved kept a low profile, but now the affair surrounding the development of a herbal aphrodisiac at Berlin’s Charité University Hospital has consequences: Last week, the head of the Institute for Transfusion Medicine, Prof. Dr.-Ing. Dr. med. Holger Kiesewetter, was given leave of absence. This step was taken “at his own request”, said hospital spokesperson Claudia Peter. The withdrawal came about two weeks after the public prosecutor’s office searched his work and private rooms as well as other locations.
The “Bio-Viagra affair” had caused a furore in mid-March. A doctoral student of Kiesewetter’s had claimed to the Deutsche Presse-Agentur that he had successfully developed an aphrodisiac on a purely herbal basis. Some daily newspapers reported on the remedy, which was called “Plantagrar”. A little later, however, the Charité management denied it. It was “the activity of an employee (. . .) on his own responsibility”. The case also came to the attention of the drug supervisory authority. Erectile dysfunctions are recognised diseases according to the ICD-10 classification system. The “Bio-Viagra” was therefore a drug whose development should have been controlled, the state office for health and social affairs said.
A spokesperson for the Berlin public prosecutor’s office confirmed the presumption of a violation of the German Medicines Act to the Deutsches Ärzteblatt. In addition, Kiesewetter is being investigated for bribery, corruption and breach of trust to the detriment of the Charité. The head of the institute had apparently been promised benefits by private companies.
That sounded very much like the Kiesewetter I remembered. I was unable to find the actual trial or more details about the herbal remedy. The scandal seems to have put an end not only to the university career of the researchers but also to the aphrodisiac.
However, I did find a Wiki page about Kiesewetter that suggests that ‘bio viagra’ was by no means the only escapade from the straight and narrow. But what is he up to today? Did he retire? No, after the debacle at the Charite, he seems to have gone into private practice:
After working as director of the Institute for Transfusion Medicine and Immunohaematology at the Charité and head of the coagulation outpatient clinic at the Charité, he has been providing patient care at the Hämostaseologicum Berlin-Mitte since 2010.
This is also the address he used for his most recent (2020) publication.
Am I worried about my old ‘friend’?
No, I am confident that he is doing just fine … financially, I mean.
THE GUARDIAN published an interesting article about vaccination hesitancy yesterday. Here is a short passage from it:
One major missing piece of the puzzle, currently under consideration, is a strategy that gets to the bottom of why 5 million people remained unvaccinated, especially those in communities with an ingrained distrust of authority.
No 10 even turned to an artificial intelligence (AI) company earlier in the year to determine the causes of vaccine hesitancy, but Whitehall sources acknowledge there is still a lack of understanding about how many of the unvaccinated remain so because of entrenched anti-vax ideology, misconceptions that could be turned around, a lack of time or transport to get to vaccine centres, or just apathy.
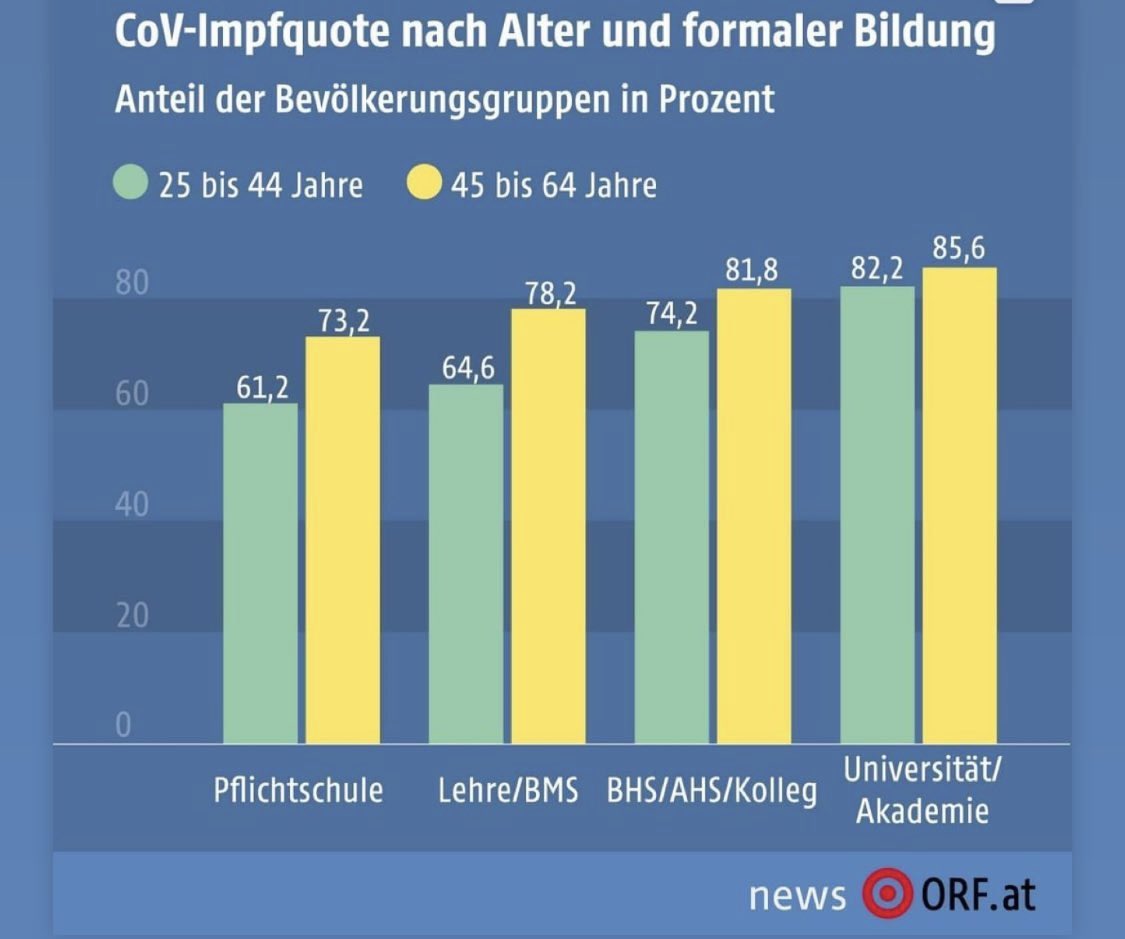
Yesterday, it was also reported in DER STANDARD that the Austrian Science Minister Martin Polaschek has commissioned a study from Statistics Austria, which for the first time was to look at the vaccination status of the population according to socio-economic characteristics.
The study yielded fascinating findings that might shed some light on the phenomenon of ‘entrenched anti-vax ideology’:
- Across all age groups, the proportion of vaccinated persons, including recovered persons, is 67%.
- Slightly less than four percent of the population are only recovered, and about 30% are neither one nor the other.
- There are no marked differences between men and women.
- The willingness to vaccinate is strongly related to the level of education.
- The vaccination rate in the group of 25-64 year-olds with a university degree is about 84% and thus significantly higher than among those who have only basic education (68%).
- In this age group, it also seems important whether someone has a job (76%) or not (69%).
- People employed in the information and communication sector (85%) and public administration (83%) are the most likely to be vaccinated.
- Workers in agriculture and forestry (67%) and construction (65%) are the least likely to accept vaccinations.
- Health and social services personnel have a vaccination rate of 79%.
- More than half of the 600,000 schoolchildren had already been vaccinated, and in the upper secondary school it was even 72%.
- The rate among teachers is also high, at 85%.
- 86% of the approximately 395,000 students at universities had been vaccinated.
- As 92% of all medical students were vaccinated.
- The vaccination rate among Austrian nationals, at about 70%, is clearly higher than that of people without an Austrian passport (52%).
- The difference between those born in Austria and those not born in Austria is only five percentage points.
- The willingness to be vaccinated is higher among people from Turkey (73%) than among those born in Austria (68%).
- Among Germans and Afghans, it is around 72%.
- People from Romania (43%) and the Russian Federation (45%) have the lowest vaccination rates.
- The percentage of vaccinated people is highest among those between 75 and 84 years.
Similar findings have, of course, been reported from other countries. However, what seems new to me here is the finding that vaccination rates are strongly correlated to the level of education: the anti-vax brigade tends to be uneducated and ignorant. If confirmed, this suggests that education might be a way to make them accept vaccinations.
PS
Of course, correlation is not causality. But there seems to be a dose-response relationship between education and willingness to vaccinate. This makes a causal effect more likely.
THOSE WHO KNOW NOTHING MUST BELIEVE EVERYTHING
I came across this article via a German secondary report about it entitled “Scientists discover what else protects from severe symptoms” (Forscher finden heraus, was noch vor schweren Symptomen schützt). The article rightly stressed that vaccination is paramount and then explains that, once you have caught COVID, nutrition can prevent serious symptoms.
Even though I rarely discuss standard nutritional issues on my blog (nutrition belongs to mainstream not so-called alternative medicine [SCAM], in my view), this subject did attract my attention. Here are the essentials of the original scientific paper:
Australian scientists studied the association between habitual frequency of food intake of certain food groups during the COVID-19 pandemic and manifestations of COVID-19 symptoms in adult outpatients with suspected SARS-CoV-2 infection. They included 236 patients who attended an outpatient clinic for suspected COVID-19 evaluation. Severity of symptoms, habitual food intake frequency, demographics and Bristol chart scores were obtained before diagnostic confirmation with real-time reverse transcriptase PCR using nasopharyngeal swab.
The results of the COVID-19 diagnostic tests were positive for 103 patients (44%) and negative for 133 patients (56%). In the SARS-CoV-2-positive group, symptom severity scores had significant negative correlations with the habitual intake frequency of specific food groups. Multivariate binary logistic regression analysis adjusted for age, sex, and occupation confirmed that SARS-CoV-2-positive patients showed a significant negative association between having higher symptom severity and the habitual intake frequency of legumes and grains, bread, and cereals.
The authors concluded that an increase in habitual frequency of intake of ‘legumes’, and ‘grains, bread and cereals’ food groups decreased overall symptom severity in patients with COVID-19. This study provides a framework for designing a protective diet during the COVID-19 pandemic and also establishes a hypothesis of using a diet-based intervention in the management of SARS-CoV-2 infection, which may be explored in future studies.
So, the authors seem to think that they found a causal relationship: A CHANGE IN DIET DECREASES SYMPTOMS. In different sections of the article, they seem to confirm this notion, and they state that they tested the hypothesis of the effect of diet on SARS-CoV-2 infection symptom severity.
Yey, the investigation was merely a correlative study that cannot establish cause and effect. There are many other variables that might be linked to dietary habits which could be the true cause of the observed phenomenon (or contributors to it).
What’s the harm? If the article makes people adopt a healthier diet, all is pukka!
Perhaps, in this case, that might be true (even though one could argue that this paper might support anti-vax notions arguing that vaccination is not important if it is possible to prevent severe symptoms through dietary changes). But the confusion of correlation with causality is both frequent and potentially harmful. And it is unquestionably poor science!
I feel that we need to be concerned about the fact that even reputable journals let such things pass – not least because the above example shows what the popular press subsequently can make of such misleading messages.
Compelling evidence has long shown that diagnostic imaging for low back pain does not improve care in the absence of suspicion of serious pathology. However, the effect of imaging use on clinical outcomes has not been investigated in patients presenting to chiropractors. The aim of this study was to determine if diagnostic imaging affects clinical outcomes in patients with low back pain presenting for chiropractic care.
A matched observational study using prospective longitudinal observational data with a one-year follow-up was performed in primary care chiropractic clinics in Denmark. Data were collected from November 2016 to December 2019. Participants included low back pain patients presenting for chiropractic care, who were either referred or not referred for diagnostic imaging at their initial visit. Patients were excluded if they were younger than 18 years, had a diagnosis of underlying pathology, or had previously had imaging relevant to their current clinical presentation. Coarsened exact matching was used to match participants referred for diagnostic imaging with participants not referred for diagnostic imaging on baseline variables including participant demographics, pain characteristics, and clinical history. Mixed linear and logistic regression models were used to assess the effect of imaging on back pain intensity and disability at two weeks, three months, and one year, and on global perceived effect and satisfaction with care at two weeks.
A total of 2162 patients were included, and 24.1% of them were referred for imaging. Near perfect balance between matched groups was achieved for baseline variables except for age and leg pain. Participants referred for imaging had slightly higher back pain intensity at two weeks (0.4, 95%CI: 0.1, 0.8) and one year (0.4, 95%CI: 0.0, 0.7), and disability at two weeks (5.7, 95%CI: 1.4, 10.0), but these differences are unlikely to be clinically meaningful. No difference between groups was found for the other outcome measures. Similar results were found when a sensitivity analysis, adjusted for age and leg pain intensity, was performed.
The authors concluded that diagnostic imaging did not result in better clinical outcomes in patients with low back pain presenting for chiropractic care. These results support that current guideline recommendations against routine imaging apply equally to chiropractic practice.
This study confirms what most experts suspected all along and what many chiropractors vehemently denied for years. One could still argue that the outcomes do not differ much and therefore imaging does not cause any harm. This argument would, however, be wrong. The harm it causes does not affect the immediate clinical outcomes. Needless imaging is costly and increases the cancer risk.
Conspiracy beliefs are associated with detrimental health attitudes during the coronavirus pandemic. Prior research on these issues was mostly cross-sectional, however, and restricted to attitudes or behavioral intentions. This investigation was designed to examine to what extent conspiracy beliefs predict health behavior and well-being over a longer period of time.
In this multi-wave study on a large (N = 5745) Dutch research panel (weighted to provide nationally representative population estimates), the researchers examined if conspiracy beliefs early in the pandemic (April 2020) would predict a range of concrete health and well-being outcomes eight months later (December 2020).
The results revealed that Covid-19 conspiracy beliefs prospectively predicted a decreased likelihood of getting tested for corona; if tested, an increased likelihood of the test coming out positive; and, an increased likelihood of having violated corona regulations, deteriorated economic outcomes (job loss; reduced income), experiences of social rejection, and decreased overall well-being. Most of these effects generalized to a broader susceptibility to conspiracy theories (i.e. conspiracy mentality).
The authors concluded that conspiracy beliefs are associated with a myriad of negative life outcomes in the long run. Conspiracy beliefs predict how well people have coped with the pandemic over a period of eight months, as reflected in their health behavior, and their economic and social well-being.
These findings tie in with another recent study that investigated whether individual beliefs and personal characteristics differences affect people’s likelihood of contracting COVID-19. In the early months of the pandemic, U.S. participants responded to a variety of individual difference measures as well as questions specific to the pandemic itself. Four months later, 2120 of these participants were asked whether they had contracted COVID-19. Nearly all of the included individual difference measures significantly predicted whether a person reported testing positive for the virus in this four-month period. Additional analyses revealed that all of these relationships were primarily mediated by whether participants held accurate knowledge about COVID-19.
I find it hard not to despair vis a vis such results. Not that they were not to be expected – if you ignore the existence of risk factors exist for heart attacks, it seems plausible that your likelihood of dying of myocardial infarction is increased. What is particularly desolating are two facts:
- This pandemic seems to have rendered the voices of stupidity and ignorance loud and popular, even fashionable.
- Those lunatics who adhere to conspiracy beliefs harm not merely themselves but endanger all of us.
I ask myself how we will ever get past this new age of unreason.
In a recently published study, the willingness to be vaccinated of parents of underage children and persons without underage children was examined. The study was based on a random sample (telephone survey, n = 2014, survey between 12.11.2020 and 10.12.2020).
The results revealed that parents consistently show a lower propensity to vaccinate with a COVID-19 vaccine than respondents without minor children (54.1% vs. 71.1%). Fathers showed a more pronounced own willingness to vaccinate than mothers. Furthermore, men were more willing than women to have their own child vaccinated with a COVID-19 vaccine.
The overall sample also showed that a rejection of so-called alternative medicine (SCAM) was associated with a significantly higher willingness to be vaccinated. There was also a significant correlation between the attitude towards homeopathy and one’s own willingness to be vaccinated. If homeopathy was supported, the willingness to vaccinate was lower. This correlation between the attitude towards homeopathy and willingness to vaccinate was also evident in the sub-sample of parents. Among the parents, it was again the women who significantly more often had a positive attitude towards homeopathy than men, who more often do not think anything of it.
This new evidence ties in neatly with many of my previous posts on the subject of SCAM and vaccination, for instance:
- More information on homeopaths’ and anthroposophic doctors’ attitude towards vaccinations
- The anti-vaccination movement is financed by the dietary supplement industry
- The UK Society of Homeopaths, a hub of anti-vaccination activists?
- HOMEOPATHY = “the complete alternative to vaccination” ?!?!
- Are anthroposophy-enthusiasts for or against vaccinations?
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Andrew Wakefield, Donald Trump, SCAM, and the anti-vaccination cult
- Naturopaths’ counselling against vaccinations could be criminally negligent
- HOMEOPATHS AGAINST VACCINATION: “The decision to vaccinate and how you implement that decision is yours and yours alone”
- Use of alternative medicine is associated with low vaccination rates
- Integrative medicine physicians tend to harbour anti-vaccination views
- Vaccination: chiropractors “espouse views which aren’t evidence based”
- Faith-healing as an alternative to vaccination?
- Learning about homeopathy the hard way: the story of Aaron Rodgers
- Patients consulting chiropractors, homeopaths, or naturopaths are less likely to agree to the flu jab
- Parents’ Willingness to Vaccinate with a COVID-19 Vaccine: strongly influenced by homeopathy
- “The uncensored truth” about COVID-19 vaccines” … as told by some chiro loons
- Beliefs and behaviors of US chiropractors
- Many naturopaths, homeopaths, and chiropractors are a risk to public health
- Homeopaths (and other SCAM practitioners) are peddling dangerous myths
- Misinformation and fraudulent claims about boosting immunity during the pandemic
Collectively, this evidence tells us that:
- the effect has been shown in many different ways,
- it can therefore be assumed to be real,
- it is not confined to COVID vaccinations,
- it is not confined to one particular branch of SCAM,
- it even affects MDs (who surely should know better) dabbling in SCAM,
- it has a long history,
- it is prevalent in many, if not most countries,
- it does real harm.
So, the next time someone tells you that SCAM and SCAM practitioners have a positive influence on public health, tell them to think again.
Muscular dystrophies are a rare, severe, and genetically inherited disorders characterized by progressive loss of muscle fibers, leading to muscle weakness. The current treatment includes the use of steroids to slow muscle deterioration by dampening the inflammatory response. Chinese herbal medicine (CHM) has been offered as adjunctive therapy in Taiwan’s medical healthcare plan, making it possible to track CHM usage in patients with muscular dystrophies. This investigation explored the long-term effects of CHM use on the overall mortality of patients with muscular dystrophies.
A total of 581 patients with muscular dystrophies were identified from the database of Registry for Catastrophic Illness Patients in Taiwan. Among them, 80 and 201 patients were CHM users and non-CHM users, respectively. Compared to non-CHM users, there were more female patients, more comorbidities, including chronic pulmonary disease and peptic ulcer disease in the CHM user group. After adjusting for age, sex, use of CHM, and comorbidities, patients with prednisolone usage exhibited a lower risk of overall mortality than those who did not use prednisolone. CHM users showed a lower risk of overall mortality after adjusting for age, sex, prednisolone use, and comorbidities. The cumulative incidence of the overall survival was significantly higher in CHM users. One main CHM cluster was commonly used to treat patients with muscular dystrophies; it included Yin-Qiao-San, Ban-Xia-Bai-Zhu-Tian-Ma-Tang, Zhi-Ke (Citrus aurantium L.), Yu-Xing-Cao (Houttuynia cordata Thunb.), Che-Qian-Zi (Plantago asiatica L.), and Da-Huang (Rheum palmatum L.).
The authors concluded that the data suggest that adjunctive therapy with CHM may help to reduce the overall mortality among patients with muscular dystrophies. The identification of the CHM cluster allows us to narrow down the key active compounds and may enable future therapeutic developments and clinical trial designs to improve overall survival in these patients.
I disagree!
What the authors have shown is a CORRELATION, and from that, they draw conclusions implying CAUSATION. This is such a fundamental error that one has to wonder why a respected journal let it go past.
A likely causative explanation of the findings is that the CHM group of patients differed in respect to features that the statistical evaluations could not control for. Statisticians can never control for factors that have not been measured and are thus unknown. A possibility in the present case is that these patients had adopted a different lifestyle together with employing CHM which, in turn, resulted in a longer survival.
As discussed regularly on this blog, there is plenty of evidence to show that many chiropractors, homeopaths, and naturopaths discourage their patients from getting vaccinated. Now, a further investigation from the US seems to confirm these findings.
This analysis aims to evaluate differences between categories of so-called alternative medicine (SCAM) regarding vaccination behavior among US adults.
The data from the 2017 National Health Interview Survey (NHIS; n = 26,742; response rate 80.7%) was used for this purpose. Prevalences of flu vaccination, consultations with SCAM practitioners in the past 12 months, and their potential interactions were examined.
A total of 42.7% of participants had received the flu vaccination in the past 12 months, 32.4% had seen one or more SCAM practitioners. Users of any type of SCAM were as likely as non-users to have received a flu vaccination (44.8% users versus 41.7% non-users; p = 0,862; adjusted odds ratio [AOR] = 1.01, 95% confidence interval [CI] = 0.95-1.07).
Regarding specific SCAMs, individuals consulting with
- naturopaths (p < 0.001; AOR = 0.67, 95 %CI = 0.54-0.82),
- homeopaths (p < 0.001; AOR = 0.55; 95 %CI = 0.44-0.69),
- chiropractors (p = 0.016; AOR = 0.9, 95 %CI = 0.83-0.98)
were less likely, while other SCAM approaches showed no significant association with flu vaccination behavior. Independent predictors for a flu shot were prior diabetes, cancer, current asthma, kidney disease, overweight and current pregnancy. As well, higher educational level, age, ethnicity, health insurance coverage, and having seen a general physician or medical specialist in the past 12 months were also associated with a higher vaccination rate.
The authors concluded that SCAM users were equally likely to receive an influenza vaccination compared with non-users. Different complementary therapies showed varied associations with vaccination behavior. Further analyses may be needed to distinguish influencing factors among patients’ vaccination behavior.
This investigation confirms the prevalent anti-vax stance within chiropractic, homeopathy, and naturopathy. The effect is strongest by far with homeopaths. Nothing new! We knew this for a very long time. The question is WHAT ARE WE DOING ABOUT IT? Or more specifically, are the professional organizations of these SCAM professions finally going to take any actions against even the most rabid anti-vaxxers in their midst?
And the answer?
You guessed it: NO!
And the irony of all this must not get lost here: chiropractors, homeopaths, naturopaths, and their respective organizations all pride themselves regularly that they attribute particular importance to disease prevention.