case-control study
Even though most people do not think about it in this way, tea is a herbal remedy. We know that it is pleasant, but is it also effective?
This study explored the associations between tea drinking and the incident risk of type 2 diabetes mellitus(T2 DM). A dynamic prospective cohort study among a total of 27 841 diabetes-free permanent adult residents randomly selected from 2, 6, and 7 rural communities between 2006-2008, 2011-2012, and 2013-2014, respectively. Questionnaire survey, physical examination, and laboratory test were carried out among the participants. In 2018, the researchers conducted a follow-up through the electronic health records of residents. Cox regression models were applied to explore the association between tea drinking and the incident risk of T2 DM and estimate the hazard ratio(HR), and its 95%CI.
Among the 27 841 rural community residents in Deqing County, 10 726(39%) were tea drinkers, 8215 (77%) of which were green tea drinkers. A total of 883 new T2 DM incidents were identified until December 31, 2018, and the incidence density was 4.43 per 1000 person-years (PYs). The incidence density was 4.07/1000 PYs in those with tea drinking habits and 4.71/1000 PYs in those without tea drinking habits. The incidence density was 3.79/1000 PYs in those with green tea drinking habits. After controlling for sex, age, education, farming, smoking, alcohol consumption, dietary preference, body mass index, hypertension, impaired fasting glucose, and family history of diabetes, the risk of T2 DM among rural residents with tea drinking habits was 0.79 times higher than that among residents without tea drinking habits(HR=0.79, 95%CI 0.65-0.96), and the risk of T2 DM among residents with green tea drinking habits was 0.72 times higher than that among residents without tea drinking habits(HR=0.72, 95%CI 0.58-0.89). No significant associations were found between other kinds of tea and the risk of T2 DM, nor the amount of green tea-drinking.
The authors concluded that drinking green tea may reduce the risk of T2 DM among adult population in rural China.
Epidemiological studies of this nature resemble big fishing expeditions that can bring up all sorts of rubbish and – if lucky – also some fish. The question thus is whether this study identified an interesting association or just some odd rubbish.
A quick look into Medline seems to suggest great caution. Here are the conclusions from a few further case-control studies:
- In Chinese adults, daily green tea consumption was associated with a lower risk of incident T2D and a lower risk of all-cause mortality in patients with diabetes, but the associations for other types of tea were less clear. In addition, daily tea consumption was associated with a lower risk of diabetic microvascular complications, but not macrovascular complications.
- Green tea drinking was associated with an increased risk of T2D in Chinese adults. The mechanisms underlying the association need to be elucidated.
- Tea consumers had reduced risks of all-cause mortality and partial cause-specific mortality, but not for the risk of death from cancer. On the contrary, daily tea drinkers with smoking habits and excessive alcohol drinking had an increased risk of death from cancer.
Thus the question of whether tea drinking might prevent diabetes remains open, in my view.
Yet, the paper might teach us two important lessons:
- Case-control studies must be taken with a pinch of salt.
- Correlation is not the same as causation.
Ischemic heart disease (IHD) related to cardiovascular or cerebrovascular disease is the leading cause of mortality and an important issue of public health worldwide. The cost of long-term healthcare for IHD patients may result in a huge financial burden. This study analyzed the medical expenditure incurred for and survival of IHD patients treated with Chinese herbal medicine (CHM) and Western medicine.
Subjects were randomly selected from the National Health Insurance Research Database in Taiwan. The Cox proportional hazards regression model, Kaplan–Meier estimator, logrank test, chi-square test, and analysis of variance were applied. Landmark analysis was used to assess the cumulative incidence of death in IHD patients.
A total of 11,527 users were identified as CHM combined with Western medicine and 11,527 non-CHM users. CHM users incurred a higher medical expenditure for outpatient care within 1 (24,529 NTD versus 18,464 NTD, value <0.0001) and 5 years (95,345 NTD versus 60,367 NTD, value <0.0001). However, CHM users had shorter hospitalizations and lower inpatient medical expenditure (7 days/43,394 NTD in 1 year; 11 days/83,141 NTD in 5 years) than non-CHM users (11 days/72,939 NTD in 1 year; 14 days/107,436 NTD in 5 years).
The CHM group’s adjusted hazard ratio for mortality was 0.41 lower than that of the non-CHM group by Cox proportional hazard models with time-dependent exposure covariates. Danshen, Huang qi, Niu xi, Da huang, and Fu zi were the most commonly prescribed Chinese single herbs; Zhi-Gan-Cao-Tang, Xue-Fu-Zhu-Yu-Tang, Tian-Wang-Bu-Xin-Dan, Sheng-Mai-San, and Yang-Xin-Tang were the five most frequently prescribed herbal formulas in Taiwan.
The authors concluded that combining Chinese and Western medicine can reduce hospital expenditure and improve survival for IHD patients.
Why, you will ask, do I think that this study deserves to be in the ‘worst paper cometition’?
It is not so bad!
It is an epidemiological case-control study with a large sample size that generates interesting findings.
Agreed!
But, as a case-control study, it cannot establish a causal link between CHM and the outcomes. You might argue that the conclusions avoid doing this – “can … improve survival” is not the same as “does improve survival”. This may be true, yet the title of the article leaves little doubt about the interpretation of the authors:
Chinese Herbal Medicine as an Adjunctive Therapy Improves the Survival Rate of Patients with Ischemic Heart Disease: A Nationwide Population-Based Cohort Study
I find it difficult not to view this as a deliberate attempt of the authors, editors, and reviewers to mislead the public.
Looking at the details of the study, it is easy to see that the two groups were different in a whole range of parameters that were measured. More importantly, they most likely differ in a range of variables that were not measured and had significant influence on IHD survival. It stands to reason, for instance, that patients who elected to use CHM in addition to their standard care were more health conscious. They would thus have followed a healthier diet and lifestyle. It would be foolish to claim that such factors do not influence IHD survival.
The fact that the authors fail even to mention this possibility, interpret an association as a causal link, and thus try to mislead us all makes this paper, in my view, a strong contender for my
WORST PAPER OF 2022 COMPETITION
This cohort study was designed as undertaken to evaluate the protective effect of Arsenicum album 30C against COVID-19.
Participants were enrolled in a homeopathy intervention (HI) cohort (who received Arsenicum album) or in a non-intervention (NI) cohort (who received no systematic intervention) from COVID-19 containment areas of Delhi. Individuals of age 5 years or above were given four medicated pills of Arsenicum album 30C, while those from 1 to 5 years old were given two medicated pills in each dose.
The analysis included 10,180 individuals residing in 11 COVID-19 containment areas in Delhi, out of which 6,590 individuals were in the HI cohort and 3,590 individuals were in the NI cohort. The overall protective effect of Arsenicum album 30C was 83% (95% confidence interval [CI], 76.77 to 88.17): 45 cases per 6,590 (8.34 per 10,000 person-weeks) in the Arsenicum album 30C group versus 143 cases per 3,590 (45.01 per 10,000 person-weeks) in the NI cohort. The protective effect of Arsenicum album 30C against laboratory-confirmed COVID-19 was 74% (95% CI, 55.08 to 85.41): 18 cases per 6,590 (3.32 per 10,000 person-weeks) in the Arsenicum album 30C group versus 38 cases per 3,590 (11.85 per 10,000 person-weeks) in the NI cohort.
The authors concluded that the use of Arsenicum album 30C was associated with some protection against probable and laboratory-confirmed COVID-19 in a containment-zone setting. Randomized controlled trials are needed to confirm or refute these results.
It is remarkable, I feel, that the authors conclude Arsenicum album 30C was associated with some protection. All too often enthusiasts of homeopathy claim a causal link where there is none – but not this time, and I wonder why.
Unfortunately, I was unable to read the full text of the paper (it’s behind a paywall and I would be grateful for anyone to make it available). Thus, I cannot comment on one of the most crucial questions related to the study: how were the patients divided into the two groups?
It is clear that it was not by randomization. Yet only randomization would have created two fully comparable groups. The most likely explanation for the findings of this trial is therefore that the two groups differed in terms of one or more prognostic factors. This would explain why a group of patients receiving a placebo (Arsenicum album C30 is a dilution of Arsenic at a ratio of 1: 1000000000000000000000000000000000000000000000000000000000000 and therefore is a pure placebo [unless, of course, one believes in homeopathic magic) experience different outcomes from those receiving nothing.
As I said, the answer can only be found by studying the precise selection criteria used in this study. Until this is cleared up, I can only say three things for sure:
- A causal link between the treatment and the result is highly unlikely.
- It is regrettable that researchers do not use randomization for potentially important trials.
- It seems unethical to encourage placebo use for the prevention of a serious illness.
_______________________
UPDATE
I just received the full text from one of the authors. This is what they say about the allocation of the participants:
“Participants were enrolled in two cohorts: the homeopathy intervention (HI) cohort and the non-intervention (NI) cohort. Recruitment to the cohorts was at cluster level (containment area): the clusters were allotted to the HI cohort or the NI cohort as per convenience.”
I am afraid, this tells me very little, and my concerns noted above still apply.
A few other points are of relevance:
- The study was conducted between April and August 2020. This begs the question of why it took 2 years to publish the findings.
- The outcomes were verified via telephone. This means that social desirability might have influenced the results.
- The paper also confirms that there were many important differences between the groups that might have prognostic significance.
- The conclusion at the end of the paper does imply causality in stronger terms than the abstract: “The use of Arsenicum album 30C may help protect against COVID-19 infection. Randomized controlled trials are needed
to confirm or refute our findings.
An epidemiological study from the US just published in the BMJ concluded that “the mortality gap in Republican voting counties compared with Democratic voting counties has grown over time, especially for white populations, and that gap began to widen after 2008.”
In a BMJ editorial, Steven Woolf comments on the study and provides further evidence on how politics influence health in the US. Here are his concluding two paragraphs:
Political influence on US mortality rates became overt during the covid-19 pandemic, when public health policies, controlled by states, were heavily influenced by party affiliation. Republican politicians, often seeking to appeal to President Trump and his supporters, challenged scientific evidence and opposed enforcement of vaccinations and safety measures such as masking. A macabre natural experiment occurred in 2021, a year marked by the convergence of vaccine availability and contagious variants that threatened unvaccinated populations: states led by governors who promoted vaccination and mandated pandemic control measures experienced much lower death rates than the “control” group, consisting of conservative states with lax policies and large unvaccinated populations. This behavior could explain why US mortality rates associated with covid-19 were so catastrophic, vastly exceeding losses in other high income countries.
Observers of health trends in the US should keep their eye on state governments, where tectonic shifts in policy are occurring. While gridlock in Washington, DC incapacitates the federal government, Republican leaders in dozens of state capitols are passing laws to undermine health and safety regulations, ban abortion, limit LGBT+ rights, and implement more conservative policies on voting, school curriculums, and climate policy. To understand the implications for population health, researchers must break with custom; although scientific literature has traditionally avoided discussing politics, the growing influence of partisan affiliation on policies affecting health makes this covariate an increasingly important subject of study.
_____________________
What has this to do with so-called alternative medicine (SCAM)?
Not a lot.
Except, of course, that Trump has been quite sympathetic to both quackery and quacks (see, for instance, here and here). Moreover, the embarrassing Dr. Oz, America’s charlatan-in-chief, is now a Republican candidate for the US senate. And the creation of the NHI office for alternative medicine, currently called NCCIH, was the idea of the Republican senator, Tom Harkin.
I think we get the drift: on the US political level, SCAM seems to be a right-wing thing.
Am I claiming that SCAM is the cause of the higher mortality in Republican counties?
No.
Do I feel that both are related to irresponsible attitudes towards healthcare issues?
Yes.
There are many patients in general practice with health complaints that cannot be medically explained. Some of these patients attribute their problems to dental amalgam.
This study examined the cost-effectiveness of the removal of amalgam fillings in patients with medically unexplained physical symptoms (MUPS) attributed to amalgam compared to usual care, based on a prospective cohort study in Norway.
Costs were determined using a micro-costing approach at the individual level. Health outcomes were documented at baseline and approximately two years later for both the intervention and the usual care using EQ-5D-5L. Quality-adjusted life year (QALY) was used as the main outcome measure. A decision analytical model was developed to estimate the incremental cost-effectiveness of the intervention. Both probabilistic and one-way sensitivity analyses were conducted to assess the impact of uncertainty on costs and effectiveness.
In patients who attributed health complaints to dental amalgam and fulfilled the inclusion and exclusion criteria, amalgam removal was associated with a modest increase in costs at the societal level as well as improved health outcomes. In the base-case analysis, the mean incremental cost per patient in the amalgam group was NOK 19 416 compared to the MUPS group, while the mean incremental QALY was 0.119 with a time horizon of two years. Thus, the incremental costs per QALY of the intervention were NOK 162 680, which is usually considered to be cost-effective in Norway. The estimated incremental cost per QALY decreased with increasing time horizons, and amalgam removal was found to be cost-saving over both 5 and 10 years.
The authors concluded that this study provides insight into the costs and health outcomes associated with the removal of amalgam restorations in patients who attribute health complaints to dental amalgam fillings, which are appropriate instruments to inform health care priorities.
The group sizes were 32 and 28 respectively. This study was thus almost laughably small and therefore cannot lead to firm conclusions of any type. In this contest, a recent systematic review might be relevant; it concluded as follows:
On the basis of the available RCTs, amalgam restorations, if compared with resin-based fillings, do not show an increased risk for systemic diseases. There is still insufficient evidence to exclude or demonstrate any direct influence on general health. The removal of old amalgam restorations and their substitution with more modern adhesive restorations should be performed only when clinically necessary and not just for material concerns. In order to better evaluate the safety of dental amalgam compared to other more modern restorative materials, further RCTs that consider important parameters such as long and uniform follow up periods, number of restorations per patient, and sample populations representative of chronic or degenerative diseases are needed.
Similarly, a review of the evidence might be informative:
Since more than 100 years amalgam is successfully used for the functional restoration of decayed teeth. During the early 1990s the use of amalgam has been discredited by a not very objective discussion about small amounts of quicksilver that can evaporate from the material. Recent studies and reviews, however, found little to no correlation between systemic or local diseases and amalgam restorations in man. Allergic reactions are extremely rare. Most quicksilver evaporates during placement and removal of amalgam restorations. Hence it is not recommended to make extensive rehabilitations with amalgam in pregnant or nursing women. To date, there is no dental material, which can fully substitute amalgam as a restorative material. According to present scientific evidence the use of amalgam is not a health hazard.
Furthermore, there is evidence that the removal of amalgam fillings is not such a good idea. One study, for instance, showed that the mercury released by the physical action of the drill, the replacement material and especially the final destination of the amalgam waste can increase contamination levels that can be a risk for human and environment health.
As dental amalgam removal does not seem risk-free, it is perhaps unwise to remove these fillings at all. Patients who are convinced that their amalgam fillings make them ill might simply benefit from assurance. After all, we also do not re-lay electric cables because some people feel they are the cause of their ill-health.
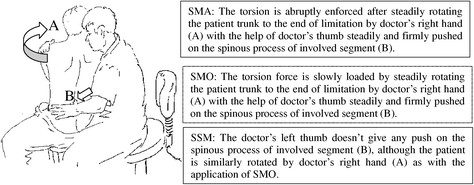
This study explored the curative effects of remote home management combined with ‘Feng’s spinal manipulation’ on the treatment of elderly patients with lumbar disc herniation (LDH). (LDH is understood by the investigators to be a condition where lumbar disc degeneration or trauma causes the nucleus pulposus and annulus fibrosus to protrude towards the spinal canal and to constrict the spinal cord or nerve root.)
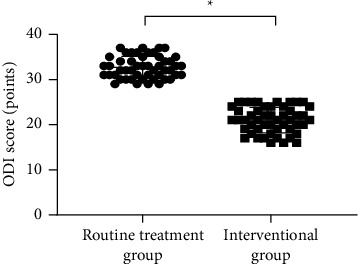
The clinical data of 100 patients with LDH were retrospectively reviewed. The 100 patients were equally divided into a routine treatment group and an interventional group according to the order of admission. The routine treatment group received conventional rehabilitation training, and the interventional group received remote home management combined with Feng’s spinal manipulation. The Oswestry disability index (ODI) and straight leg raising test were adopted for the assessment of the degrees of dysfunction and straight leg raising angles of the two groups after intervention. The curative effects of the two rehabilitation programs were evaluated.
Compared TO the routine treatment group, the interventional group had a remarkably higher excellent and good rate (P < 0.05), a significantly lower average ODI score after intervention (P < 0.001), notably higher straight leg raising angle, surface AEMG (average electromyogram) during stretching and tenderness threshold after intervention (P < 0.001), markedly lower muscular tension, surface AEMG during buckling, and flexion-extension relaxation ratio (FRR; (P < 0.001)), and much higher quality of life scores after intervention (P < 0.001).
The authors concluded that remote home management combined with Feng’s spinal manipulation, as a reliable method to improve the quality of life and the back muscular strength of the elderly patients with LDH, can substantially increase the straight leg raising angle and reduce the degree of dysfunction. Further study is conducive to establishing a better solution for the patients with LDH.
The authors state that “Feng’s spinal manipulation adopts spinal fixed-point rotation reduction to correct the vertebral displacement, and its curative effects have been confirmed in the treatment of sequestered LDH.” This is an odd statement: firstly, there is no vertebral displacement in LDH; secondly, if the treatment had been confirmed to be curative, why conduct this study?
Moreover, I don’t quite understand how the authors conducted a retrospective chart review and equally divide the 100 patients into two groups treated differently. What I do understand, however, is this:
- a retrospective review does not lend itself to conclusions about the effectiveness of any therapy;
- no type of spinal manipulation can hope to cure a lumbar disc degeneration or trauma that causes a herniation of the nucleus pulposus and annulus fibrosus.
Thus, I recommend we take this study with a sizable pinch of salt.
Today is the start of chiropractic awareness week 2022. On this occasion the BCA states most categorically: First and foremost, chiropractic is a statutorily regulated healthcare profession, supported by evidence, which offers a safe form of treatment for patients with a range of conditions. Here I am tempted to cite my friend Simon Singh:
THEY HAPPILY PROMOTE BOGUS TREATMENTS
I am, of course, particularly impressed by the BCA’s assurance of safety. In my view, the safety issue needs to be addressed more urgently than any other in the realm of chiropractic. So, to make a meaningful contribution to the current chiropractic awareness week, I conducted a few Medline searches to identify all publications of 2022 on chiropractic/spinal manipulation risks.
This is what I found:
Objective: Patients can be at risk of carotid artery dissection and ischemic stroke after cervical chiropractic manipulation. However, such risks are rarely reported and raising awareness can increase the safety of chiropractic manipulations.
Case report: We present two middle-aged patients with carotid artery dissection leading to ischemic stroke after receiving chiropractic manipulation in Foshan, Guangdong Province, China. Both patients had new-onset pain in their necks after receiving chiropractic manipulations. Excess physical force during chiropractic manipulation may present a risk to patients. Patient was administered with recombinant tissue plasminogen activator after radiological diagnoses. They were prescribed 100 mg and clopidogrel 75 mg daily for 3 months as dual antiplatelet therapy. There were no complications over the follow-up period.
Conclusion: These cases suggest that dissection of the carotid artery can occur as the result of chiropractic manipulations. Patients should be diagnosed and treated early to achieve positive outcomes. The safety of chiropractic manipulations should be increased by raising awareness about the potential risks.
Spontaneous intracranial hypotension (SIH) still remains an underdiagnosed etiology of new-onset headache. Important risk factors include chiropractic manipulation (CM). We present a case of a 36-year-old Filipino woman who presented with severe bifrontal and postural headache associated with dizziness, vomiting, and doubling of vision. A cranial computed tomography scan was done which showed an acute subdural hematoma (SDH) at the interhemispheric area. Pain medications were given which afforded minimal relief. On history, the headaches occurred 2 weeks after cervical CM. Cranial and cervical magnetic resonance imaging revealed findings supportive of intracranial hypotension and neck trauma, respectively. The patient improved with conservative management. We found 12 articles on SIH and CM after a systematic review of literature. Eleven patients (90.9%) initially presented with orthostatic headache. Eight patients (66.7%) were initially treated conservatively but only 5 (62.5%) had complete recovery. Recovery was achieved within 14 days from start of supportive therapy. Among the 3 patients who failed conservative treatment, 2 underwent non-directed epidural blood patch and one required neurosurgical intervention. This report highlights that a thorough history is warranted in patients with new onset headache. A history of CM must be actively sought. The limited evidence from the case reports showed that patients with SIH and SDH but with normal neurologic examination and minor spinal pathology can be managed conservatively for less than 2 weeks. This review showed that conservative treatment in a closely monitored environment may be an appropriate first line treatment.
Introduction: Cranio-cervical artery dissection (CeAD) is a common cause of cerebrovascular events in young subjects with no clear treatment strategy established. We evaluated the incidence of major adverse cardiovascular events (MACE) in CeAD patients treated with and without stent placement.
Methods: COMParative effectiveness of treatment options in cervical Artery diSSection (COMPASS) is a single high-volume center observational, retrospective longitudinal registry that enrolled consecutive CeAD patients over a 2-year period. Patients were ≥ 18 years of age with confirmed extra- or intracranial CeAD on imaging. Enrolled participants were followed for 1 year evaluating MACE as the primary endpoint.
Results: One-hundred ten patients were enrolled (age 53 ± 15.9, 56% Caucasian, and 50% male, BMI 28.9 ± 9.2). Grade I, II, III, and IV blunt vascular injury was noted in 16%, 33%, 19%, and 32%, respectively. Predisposing factors were noted in the majority (78%), including sneezing, carrying heavy load, chiropractic manipulation. Stent was placed in 10 (10%) subjects (extracranial carotid n = 9; intracranial carotid n = 1; extracranial vertebral n = 1) at the physician’s discretion along with medical management. Reasons for stent placement were early development of high-grade stenosis or expanding pseudoaneurysm. Stented patients experienced no procedural or in-hospital complications and no MACE between discharge and 1 year follow up. CeAD patients treated with medical management only had 14% MACE at 1 year.
Conclusion: In this single high-volume center cohort of CeAD patients, stenting was found to be beneficial, particularly with development of high-grade stenosis or expanding pseudoaneurysm. These results warrant confirmation by a randomized clinical trial.
Background: Manipulation and mobilisation for low back pain are presented in an evidence-based manner with regard to mechanisms of action, indications, efficacy, cost-effectiveness ratio, user criteria and adverse effects. Terms such as non-specific or specific are replaced by the introduction of “entities” related to possible different low back pain forms.
Efficacy: MM is effective for acute and chronic low back pain in terms of pain relief, recovery of function and relapse prevention. It is equally effective but less risky compared to other recommended therapies. MM can be used alone in acute cases and not only in the case of chronic low back pain where it is always and necessarily part of a multimodal therapy programme, especially in combination with activating measures. The users of MM should exclusively be physician specialists trained according to the criteria of the German Medical Association (Bundesärztekammer) with an additional competence in manual medicine or appropriately trained certified therapists. The application of MM follows all rules of Good Clinical Practice.
Adverse effects: Significant adverse effects of MM for low back pain are reported in the international literature with a frequency of 1 per 50,000 to 1 per 3.7 million applications, i.e. MM for low back pain is practically risk-free and safe if performed according to the rules of the European Training Requirements of the UEMS.
Studies have reported that mild adverse events (AEs) are common after manual therapy and that there is a risk of serious injury. We aimed to assess the safety of Chuna manipulation therapy (CMT), a traditional manual Korean therapy, by analysing AEs in patients who underwent this treatment. Patients who received at least one session of CMT between December 2009 and March 2019 at 14 Korean medicine hospitals were included. Electronic patient charts and internal audit data obtained from situation report logs were retrospectively analysed. All data were reviewed by two researchers. The inter-rater agreement was assessed using the Cohen’s kappa coefficient, and reliability analysis among hospitals was assessed using Cronbach’s Alpha coefficient. In total, 2,682,258 CMT procedures were performed in 289,953 patients during the study period. There were 50 AEs, including worsened pain (n = 29), rib fracture (n = 11), falls during treatment (n = 6), chest pain (n = 2), dizziness (n = 1), and unpleasant feeling (n = 1). The incidence of mild to moderate AEs was 1.83 (95% confidence interval [CI] 1.36-2.39) per 100,000 treatment sessions, and that of severe AEs was 0.04 (95% CI 0.00-0.16) per 100,000 treatment sessions. Thus, AEs of any level of severity were very rare after CMT. Moreover, there were no instances of carotid artery dissection or spinal cord injury, which are the most severe AEs associated with manual therapy in other countries.
_______________________________
This is not too bad after all!
Five papers are clearly better than nothing.
What conclusions might be drawn from my mini-review?
I think it might be safe to say:
- There is not much but at least some research going on in this area.
- The risks of chiropractic/spinal manipulation are real and are being recognized.
- BUT NOT BY CHIROPRACTORS! The most remarkable feature of the 5 papers, I think, is that none originates from a chiropractic team.
Thus, allow me to make a suggestion to chiropractors worldwide: Instead of continuing with HAPPILY PROMOTING BOGUS TREATMENTS, what about using the ‘chiropractic awareness week’ to raise awareness of the urgent necessity to research the safety of your treatments?
The associations between so-called alternative medicine (SCAM) and negative attitudes to vaccinations are, as discussed repeatedly on this blog, strong and undeniable. A new paper sheds more light on these issues.
By far the most common strategy used in the attempt to modify negative attitudes toward vaccination is to appeal to evidence-based reasoning. However, focusing on science comprehension is inconsistent with one of the key facts of cognitive psychology: Humans are biased information processors and often engage in motivated reasoning. On this basis, it is hypothesized that negative attitudes can be explained primarily by factors unrelated to the empirical evidence for vaccination; including some shared attitudes that also attract people to SCAM.
This study tested psychosocial factors associated with SCAM endorsement in past research; including aspects of spirituality, intuitive (vs analytic) thinking styles, and the personality trait of openness to experience. These relationships were tested in a cross-sectional, stratified CATI survey (N = 1256, 624 Females).
Questions regarding SCAM were derived from a previously validated instrument, designed to standardize the measurement of SCAM utilization, and distinguish between those that use a particular SCAM from those that do not. Each SCAM item provided an indication of whether the respondent had utilized each of the following therapeutic or self-treatment activities within the last 12 months:
- herbal and homeopathic remedies,
- energy-based and body therapies (including therapeutic massage),
- vitamins, yoga, meditation, prayer, body therapies, hypnosis, spiritual healing,
- and chiropractic or osteopathic treatments.
The results show that educational level and thinking style did not predict vaccination rejection. Psychosocial factors such as
- preferring SCAM to conventional medicine (OR .49, 95% CI .36-.66),
- endorsement of spirituality as a source of knowledge (OR .83, 95% CI .71-.96),
- openness (OR .86, 95% CI .74-.99),
all predicted negative attitudes to vaccination. Furthermore, for 9 of the 12 SCAMs surveyed, utilisation in the last 12 months was associated with lower levels of vaccination endorsement. Additionally, the rank-order correlation between the number of different alternative therapies used in the last 12 months and vaccination attitude score was significant. Finally, analytical thinking style was negatively related to all forms of CAM, with this relationship significant in three cases:
- herbal remedies ρ = −.08, p = .0014,
- homeopathy, ρ = −.06, p = .0236,
- prayer for the purpose of healing, ρ = −.15, p < .0001.
The authors concluded that vaccination scepticism appears to be the outcome of a particular cultural and psychological orientation leading to unwillingness to engage with the scientific evidence. Vaccination compliance might be increased either by building general confidence and understanding of evidence-based medicine, or by appealing to features usually associated with SCAM, e.g. ‘strengthening your natural resistance to disease’.
In the discussion section of their paper, the authors argue that these results describe a vaccine sceptic as viewing themselves as anti-authoritarian and unconventional, with a preference for unorthodox treatments with spiritual or ‘life-affirming’ features. The significant effect for personality, but not for cognitive style, is congruent with the notion that it is a reluctance to engage with the evidence, rather than a lack of capacity to appropriately process the evidence, that predicts vaccination scepticism…
SCAM endorsement and vaccination scepticism are components of a common attitudinal stance, with some shared psychosocial determinants. The results of the present study indicate that vaccination rejection is related to psychosocial factors: a general preference for complementary over conventional medicines, valuing diverse and unconventional alternatives, and a spiritual orientation to attitude formation. The null findings with regard to cognitive style and educational level suggest that factors unrelated to the actual empirical evidence for vaccination – i.e. a particular personality and attitudinal mindset are most instrumental in determining vaccination attitudes. Efforts to counter vaccination concerns should be mindful that negative vaccination views appear to form part of a broader attitudinal system that does not necessarily trust empirical or positivist evidence from authoritative sources. Vaccination promotion efforts may benefit from targeting groups associated with SCAM and building general confidence in scientific medicine, rather than targeting specific misunderstandings regarding vaccination.
Bioresonance is an alternative therapeutic and diagnostic method employing a device developed in Germany by Scientology member Franz Morell in 1977. The bioresonance machine was further developed and marketed by Morell’s son-in-law Erich Rasche and is also known as ‘MORA’ therapy (MOrell + RAsche). Bioresonance is based on the notion that one can diagnose and treat illness with electromagnetic waves and that, via resonance, such waves can influence disease on a cellular level.
On this blog, we have discussed the idiocy bioresonance several times (for instance, here and here). My favorite study of bioresonance is the one where German investigators showed that the device cannot even differentiate between living and non-living materials. Despite the lack of plausibility and proof of efficacy, research into bioresonance continues.
The aim of this study was to evaluate if bioresonance therapy can offer quantifiable results in patients with recurrent major depressive disorder and with mild, moderate, or severe depressive episodes.
The study included 140 patients suffering from depression, divided into three groups.
- The first group (40 patients) received solely bioresonance therapy.
- The second group (40 patients) received pharmacological treatment with antidepressants combined with bioresonance therapy.
- The third group (60 patients) received solely pharmacological treatment with antidepressants.
The assessment of depression was made using the Hamilton Depression Rating Scale, with 17 items, at the beginning of the bioresonance treatment and the end of the five weeks of treatment.
The results showed a statistically significant difference for the treatment methods applied to the analyzed groups (p=0.0001). The authors also found that the therapy accelerates the healing process in patients with depressive disorders. Improvement was observed for the analyzed groups, with a decrease of the mean values between the initial and final phase of the level of depression, of delta for Hamilton score of 3.1, 3.8 and 2.3, respectively.
The authors concluded that the bioresonance therapy could be useful in the treatment of recurrent major depressive disorder with moderate depressive episodes independently or as a complementary therapy to antidepressants.
One could almost think that this is a reasonably sound study. But why did it generate such a surprising result?
When reading the full paper, the first thing one notices is that it is poorly presented and badly written. Thus there is much confusion and little clarity. The questions keep coming until one comes across this unexpected remark: the study was a retrospective study…
This explains some of the confusion and it certainly explains the surprising results. It remains unclear how the patients were selected/recruited but it is obvious that the groups were not comparable in several ways. It also becomes very clear that with the methodology used, one can make any nonsense look effective.
In the end, I am left with the impression that mutton is being presented as lamb, even worse: I think someone here is misleading us by trying to convince us that an utterly bogus therapy is effective. In my view, this study is as clear an example of scientific misconduct as I have seen for a long time.
Enthusiasts of so-called alternative medicine (SCAM) seem remarkably often those who deny the evidence related to the dire consequences of a COVID-19 infection. Consequently, they also deny the value of COVID vaccinations. Because on this blog we have had so many examples of this phenomenon, let me today show an interesting study that might give them food for thought.
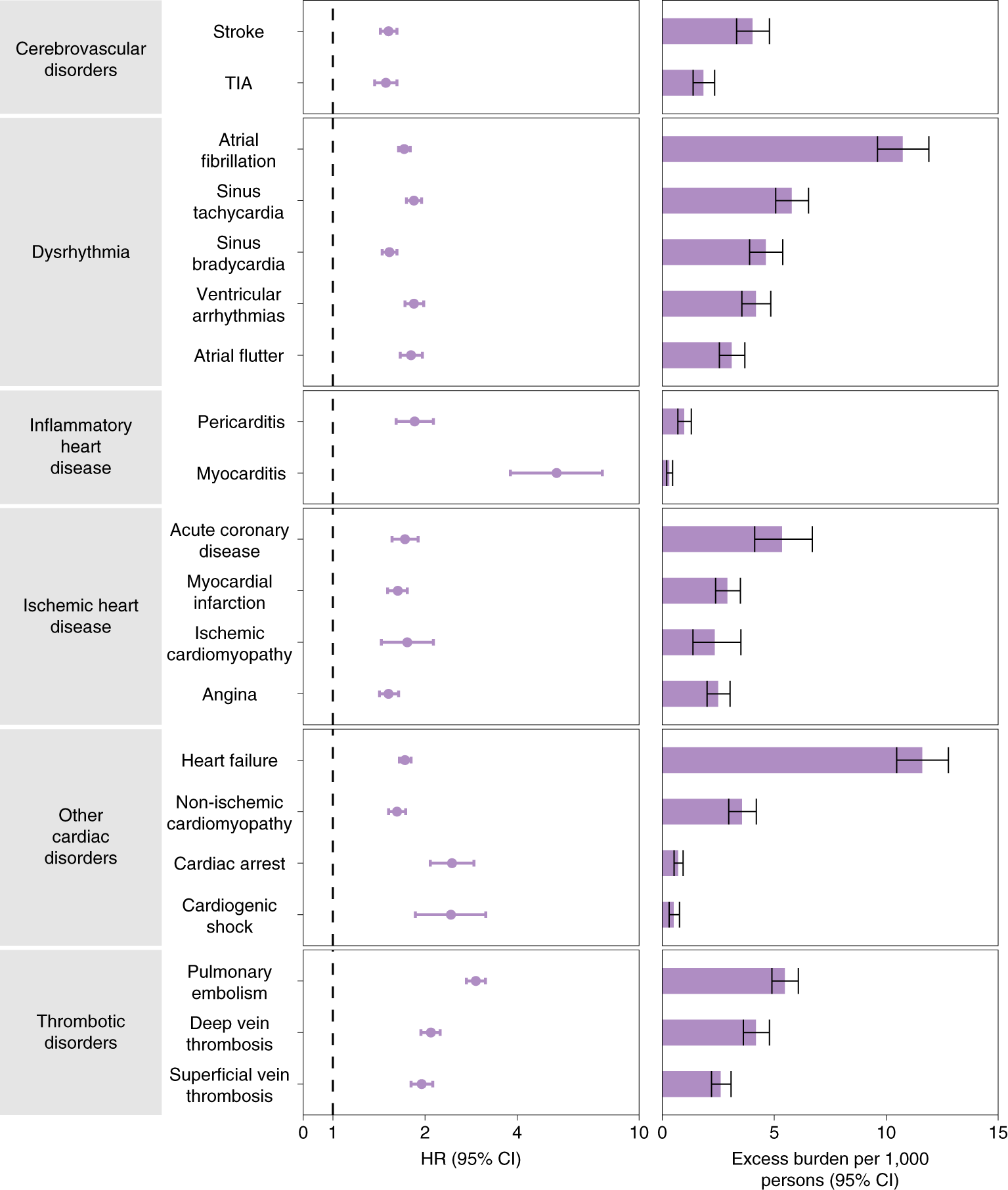
The cardiovascular complications of acute coronavirus disease 2019 (COVID-19) are well described, but the post-acute cardiovascular manifestations of COVID-19 have not yet been comprehensively characterized. The authors of this study used national healthcare databases from the US Department of Veterans Affairs to build a cohort of 153,760 individuals with COVID-19, as well as two sets of control cohorts with 5,637,647 (contemporary controls) and 5,859,411 (historical controls) individuals, to estimate risks and 1-year burdens of a set of pre-specified incident cardiovascular outcomes.
The results show that beyond the first 30 d after infection, individuals with COVID-19 are at increased risk of incident cardiovascular disease spanning several categories, including cerebrovascular disorders, dysrhythmias, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure, and thromboembolic disease. These risks and burdens were evident even among individuals who were not hospitalized during the acute phase of the infection and increased in a graded fashion according to the care setting during the acute phase (non-hospitalized, hospitalized, and admitted to intensive care).
Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes compared with the contemporary control cohort.
Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 153,760) and contemporary control cohort (n = 5,637,647). Adjusted HRs and 95% CIs are presented. The length of the bar represents the excess burden per 1,000 persons at 12 months, and associated 95% CIs are also shown.
The authors concluded that the results provide evidence that the risk and 1-year burden of cardiovascular disease in survivors of acute COVID-19 are substantial. Care pathways of those surviving the acute episode of COVID-19 should include attention to cardiovascular health and disease.
I know, this is a case-control study and correlation is not causation. But to investigate the possibility of a causal link further, the authors also tested the robustness of results in several sensitivity analyses involving the outcomes of MACE and any cardiovascular outcome. The sensitivity analyses were performed in comparisons involving COVID-19 versus the contemporary control and COVID-19 versus the historical control and, additionally, COVID-19 by care setting versus both controls.
(1) To test whether the inclusion of additional algorithmically selected covariates would challenge the robustness of study results, they selected and used 300 high-dimensional variables (instead of the 100 used in the primary analyses) to construct the inverse probability weighting.
(2) They then also tested the results in models specified to include only pre-defined covariates (that is, without the inclusion of algorithmically selected covariates) to build the inverse probability weighting.
(3) They changed the analytic approach by using the doubly robust method (instead of the inverse weighting method used in primary analyses) to estimate the magnitude of the associations between COVID-19 exposure and the pre-specified outcomes.
All sensitivity analyses yielded results consistent with those produced using the primary approach. This means that it is likely that the cause of the outcomes was the COVID-19 exposure.
How often have we seen advocates of SCAM argue against vaccination by pointing to the risk of myocarditis and other cardiovascular conditions, no matter how minuscule that risk truly is? This study quantifies the relative risk of several different cardiovascular outcomes after COVID-19 infection and the risk of myocarditis clearly stands out. I hope that the findings of this important study will make the COVID deniers reconsider their attitude.