bias
Shiatsu has been mentioned here before (see for instance here, here and here). It is one of those alternative therapies for which a plethora of therapeutic claims are being made in the almost total absence of reliable evidence. This is why I am delighted each time a new study emerges.
This proof of concept study explored the feasibility of ‘hand self-shiatsu’ as an intervention to promote sleep onset and continuity for young adults with SRC. It employed a prospective case-series design, where participants, athletes who have suffered from concussion, act as their own controls. Baseline and follow-up data included standardized self-reported assessment tools and sleep actigraphy. Seven athletes, aged between 18 and 25 years, participated. Although statistically significant improvement in actigraphy sleep scores between baseline and follow-up was not achieved, metrics for sleep quality and daytime fatigue showed significant improvement.
The authors concluded from these data that these findings support the hypothesis that ‘hand self-shiatsu has the potential to improve sleep and reduce daytime fatigue in young postconcussion athletes. This pilot study provides guidance to refine research protocols and lays a foundation for further, large-sample, controlled studies.
How very disappointing! If this was truly meant to be a pilot study, it should not mention findings of clinical improvement at all. I suspect that the authors labelled it ‘a pilot study’ only when they realised that it was wholly inadequate. I also suspect that the study did not yield the result they had hoped for (a significant improvement in actigraphy sleep scores), and thus they included the metrics for sleep quality and daytime fatigue in the abstract.
In any case, even a pilot study of just 7 patients is hardly worth writing home about. And the remark that participants acted as their own controls is a new level of obfuscation: there were no controls, and the results are based on before/after comparisons. Thus none of the outcomes can be attributed to shiatsu; more likely, they are due to the natural history of the condition, placebo effects, concomitant treatments, social desirability etc.
What sort of journal publishes such drivel that can only have the effect of giving a bad name to clinical research? The Journal of Integrative Medicine (JIM) is a peer-reviewed journal sponsored by Shanghai Association of Integrative Medicine and Shanghai Changhai Hospital, China. It is a continuation of the Journal of Chinese Integrative Medicine (JCIM), which was established in 2003 and published in Chinese language. Since 2013, JIM has been published in English language. They state that the editorial board is committed to publishing high-quality papers on integrative medicine... I consider this as a bad joke! More likely, this journal is little more than an organ for popularising TCM propaganda in the West.
And which publisher hosts such a journal?
Elsevier
What a disgrace!
This systematic review was aimed at evaluating the effects of acupuncture on the quality of life of migraineurs. Only randomized controlled trials that were published in Chinese and English were included. In total, 62 trials were included for the final analysis; 50 trials were from China, 3 from Brazil, 3 from Germany, 2 from Italy and the rest came from Iran, Israel, Australia and Sweden.
Acupuncture resulted in lower Visual Analog Scale scores than medication at 1 month after treatment and 1-3 months after treatment. Compared with sham acupuncture, acupuncture resulted in lower Visual Analog Scale scores at 1 month after treatment.
The authors concluded that acupuncture exhibits certain efficacy both in the treatment and prevention of migraines, which is superior to no treatment, sham acupuncture and medication. Further, acupuncture enhanced the quality of life more than did medication.
The authors comment in the discussion section that the overall quality of the evidence for most outcomes was of low to moderate quality. Reasons for diminished quality consist of the following: no mentioned or inadequate allocation concealment, great probability of reporting bias, study heterogeneity, sub-standard sample size, and dropout without analysis.
Further worrisome deficits are that only 14 of the 62 studies reported adverse effects (this means that 48 RCTs violated research ethics!) and that there was a high level of publication bias indicating that negative studies had remained unpublished. However, the most serious concern is the fact that 50 of the 62 trials originated from China, in my view. As I have often pointed out, such studies have to be categorised as highly unreliable.
In view of this multitude of serious problems, I feel that the conclusions of this review must be re-formulated:
Despite the fact that many RCTs have been published, the effect of acupuncture on the quality of life of migraineurs remains unproven.
I only recently came across this review; it was published a few years ago but is still highly relevant. It summarizes the evidence of controlled clinical studies of TCM for cancer.
The authors searched all the controlled clinical studies of TCM therapies for all kinds of cancers published in Chinese in four main Chinese electronic databases from their inception to November 2011. They found a total of 2964 reports (involving 253,434 cancer patients) including 2385 randomized controlled trials and 579 non-randomized controlled studies.
The top seven cancer types treated were lung cancer, liver cancer, stomach cancer, breast cancer, esophagus cancer, colorectal cancer and nasopharyngeal cancer by both study numbers and case numbers. The majority of studies (72%) applied TCM therapy combined with conventional treatment, whilst fewer (28%) applied only TCM therapy in the experimental groups. Herbal medicine was the most frequently applied TCM therapy (2677 studies, 90.32%). The most frequently reported outcome was clinical symptom improvement (1667 studies, 56.24%) followed by biomarker indices (1270 studies, 42.85%), quality of life (1129 studies, 38.09%), chemo/radiotherapy induced side effects (1094 studies, 36.91%), tumour size (869 studies, 29.32%) and safety (547 studies, 18.45%).
The authors concluded that data from controlled clinical studies of TCM therapies in cancer treatment is substantial, and different therapies are applied either as monotherapy or in combination with conventional medicine. Reporting of controlled clinical studies should be improved based on the CONSORT and TREND Statements in future. Further studies should address the most frequently used TCM therapy for common cancers and outcome measures should address survival, relapse/metastasis and quality of life.
This paper is important, in my view, predominantly because it exemplifies the problem with TCM research from China and with uncritical reviews on this subject. If a cancer patient, who does not know the background, reads this paper, (s)he might think that TCM is worth trying. This conclusion could easily shorten his/her life.
The often-shown fact is that TCM studies from China are not reliable. They are almost invariably positive, their methodological quality is low, and they are frequently based on fabricated data. In my view, it is irresponsible to publish a review that omits discussing these facts in detail and issuing a stark warning.
TCM FOR CANCER IS A VERY BAD CHOICE!
The UK media have often disappointed me when reporting about matters related to alternative medicine. Yet, this is ‘small fry’ compared to their coverage of the EU during the last decades. Here I have selected 50 (there are plenty more) headlines from a long list of ‘alternative truths’ and Euromyths of their invented or misleading healthcare-related stories:
- New EU sulphur rules will cause problems with oil-fired Aga’s, Dec 2009
- EU ‘bans boozing’, Feb 2005
- UK diners will face £200m for EU allergen rules, Nov 2014
- False alarm over 999 calls, Dec 2006
- Ambulances turn yellow for Europe, Mar 2002
- EU to force St Johns Ambulances to replace its entire fleet, Apr 2002
- Human medicines to be forbidden for use on animals, Feb/Mar 1995
- Taxpayers money used to rehabilitate Peruvian drug addicts, Jul 2014
- EU bans children from blowing up balloons, Oct 2011
- EU health directive to prevent barmaids from showing cleavage, Nov 2005
- “EU red tape” is denying cancer patients access to new treatments, Jun 2016
- EC rules on levels of listeria threaten British cheeses, Feb 1995
- Sales of cigars to fall due to be sold individually with a health warning, Jan 1994
- Circus performers required to wear hard hats, Jul 2003
- EU responsible for your hay fever, May 2015
- Condom dimensions to be harmonised, Mar 2000
- Fishing boats obliged to carry condoms, Nov 1992
- EU to push for standard condom size, Oct 1994
- EU plans to liquify corpses and pour them down the drain, July 2010
- Traditional cricket teas will be subjected to random hygiene checks, Apr 1993
- EC to ban prawn cocktail crisps, Jan 1993
- Smoky bacon crisps to be banned, May 2003
- EU outlaws teeth whitening products, Feb 2003
- EU blocking vital checks on doctors’ qualifications, Apr 2016
- EU doctors in UK a threat to patients, Sep 2016
- UK hospital have to employ people who do not speak English, Apr 2012
- Hundreds of GPs to be forced to acquire additional qualifications, Sep 1994
- 58 hour working week will ground hospitals to a halt, Aug 2004
- UK doctors unable to treat off shore patients at night, Feb 1999
- HGV drivers not permitted to wear glasses, Feb 1996
- Regulators to set maximum heat of electric blankets, leaving pensioners cold, Oct 1993
- Organic farmers ordered by EU to use homeopathic medicine, Apr 2015
- Small inshore fishing boats to be forced to carry extensive medical kits, Dec 1994
- Rare meat to be banned due to “too much bacteria”, Sep 1993
- Street vendors face closure due to an EC food hygiene Directive, Nov 1992
- EC to stop UK citizens taking extra strong multi-vitamin pills, Feb 1993
- EU rights to reside in another member state, EU benefit claimants and NHS treatment entitlement, Feb 2013
- Brussels to ban herbal cures, Mar 1999
- License to be required to sell herbal medicines, Oct 1994
- Update on whether license to be required to sell herbal medicines, Nov 1994
- Horses to no longer receive medicine that would make them unsafe for consumption, Jan 1994
- Hysteria about listeria, Feb 1995
- European Commission approve unsafe high-risk medical devices, Jul 2016
- Medicines to receive Latin labelling, May 1999
- Soya milk indistinguishable from cow milk and thus to be banned, April 1995
- Scotch whisky must be handled as a dangerous chemical, Nov 1995
- EC hygiene rules force closure of abattoirs, Nov 1992
- EU ban on ciggie breaks? Just hot air, Jun 2007
- Brussels to reinstate tobacco subsidies, Feb 2013
- EU to ban vitamin supplements, Mar 2002
_________________________________________________________
Yes, some of this is so nonsensically idiotic that it could be quite funny.
But sadly, it is also very annoying, even infuriating. I am sure these relentless lies are partly the cause why Brexit is currently dividing the UK and threatening to become a monumental exercise in self-destruction.
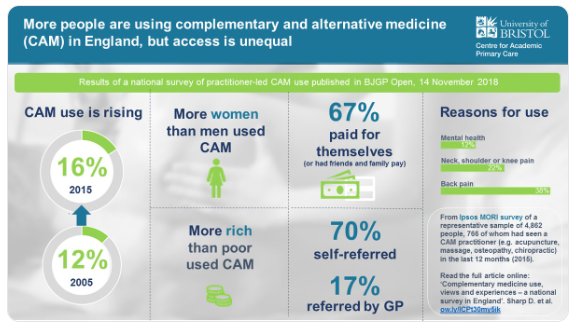
A survey was commissioned in 2015 to obtain general population figures for practitioner-led CAM use in England, and to discover people’s views and experiences regarding access.
Of 4862 adults surveyed, 766 (16%) had seen a CAM practitioner. People most commonly visited CAM practitioners for manual therapies (massage, osteopathy, chiropractic) and acupuncture, as well as yoga, pilates, reflexology, and mindfulness or meditation. Women, people with higher socioeconomic status (SES) and those in south England were more likely to access CAM. Musculoskeletal conditions (mainly back pain) accounted for 68% of use, and mental health 12%. Most was through self-referral (70%) and self-financing. GPs (17%) or NHS professionals (4%) referred and/or recommended CAM to users. These CAM users were more often unemployed, with lower income and social grade, and receiving NHS-funded CAM. Responders were willing to pay varying amounts for CAM; 22% would not pay anything. Almost two in five responders felt NHS funding and GP referral and/or endorsement would increase their CAM use.
The authors concluded that CAM use in England is common for musculoskeletal and mental health problems, but varies by sex, geography, and SES. It is mainly self-referred and self-financed; some is GP-endorsed and/or referred, especially for individuals of lower SES. Researchers, patients, and commissioners should collaborate to research the effectiveness and cost-effectiveness of CAM and consider its availability on the NHS.
The table below shows the percentage figures for specific CAMs (right column).
| Type of CAM practitioner | n | % |
| Massage practitioner | 143 | 19 |
| Osteopath | 91 | 12 |
| Acupuncturist | 88 | 11 |
| Chiropractor | 87 | 11 |
| Yoga teacher | 52 | 7 |
| Physiotherapist-delivered CAM | 41 | 5 |
| Pilates teacher | 28 | 4 |
| Reflexologist | 22 | 3 |
| Meditation and/or mindfulness teacher | 20 | 3 |
| Homeopath | 20 | 3 |
| Reiki practitioner | 17 | 2 |
| Hypnotherapist | 15 | 2 |
| Herbalist | 14 | 2 |
| Chinese herbal medical practitioner | 12 | 2 |
| Other | 74 | 10 |
Our own survey suggested that, in 2005, the 1-year prevalence of CAM-use in England was 26.3 % and the practitioner-led CAM-use was 12.1 %. The two surveys are, however, not comparable because they did use different methodologies; for instance, they included different types of CAM. I therefore think that any conclusion of an increase in practitioner-led CAM-use between 2005 and 2015 is not warranted. It also follows that the graphic below is misleading.
In the discussion, the authors of the new survey make the following point: Ability to pay may be a factor in accessing CAM (indicated by the association of CAM use with higher SES; lower SES responders being more likely to be GP-referred to CAM; and responders stating that they may use more CAM if the NHS provided services, and GPs endorsed and/or referred them). Integration of CAM into the NHS through primary care could promote continuity of care, safety, and balance of power. An integrative medicine approach includes many of the values recently included in UK health policy documents; for example, Five Year Forward View. It is patient-centred, as discussed in 2010, focuses on prevention, and emphasises patient self-management and person- and community-centred approaches to health and wellbeing. Many of these values underpin social prescribing, which is an increasingly popular model of health care. There seems to be significant patient demand for CAM and more holistic approaches, and a view that CAM may improve patient satisfaction.
I have in a previous post commented on prevalence surveys: the argument that is all too often spun around such survey data goes roughly as follows: a large percentage of the population uses alternative medicine; people pay out of their own pocket for these treatments; they are satisfied with them (if not, they would not pay for them). BUT THIS IS GROSSLY UNFAIR! Why should only those individuals who are rich enough to afford alternative medicine benefit from it? ALTERNATIVE MEDICINE SHOULD BE MADE AVAILABLE FOR ALL.
To me, it is obvious that this line of argument is dangerously wrong. It lends itself to the promotion of unproven therapies to the detriment of good healthcare and progress. Sadly, I fear that the new survey is going to be misused in this way.
Yesterday was the 80th anniversary of the Kristallnacht, the infamous start of the Nazi holocaust. For Cristian Becker, a German PR man who is currently spending much of his time promoting homeopathy and attacking critics of homeopathy, it was the occasion to publish this tweet:
 I will try to translate it for you:
I will try to translate it for you:
Today, on 9 November, all fundamentalist GWUP-sceptics such as Natalie Grams and Edzard Ernst reflect on what hate can bring about. First, one hates homeopathy, then advocates of homeopathy, and then it can seem as though one tolerates violence.
I struggle to respond to such vitriolic stupidity.
What makes this even more shocking is the fact that, as far as I see, none of the professional bodies of German homeopathy have distanced themselves for it.
I know Dr Grams a little, and can honestly say that neither of us ‘hates’ homeopathy nor homeopaths. And crucially, we both detest violence.
If such pseudo-arguments are now being used by the defenders of homeopathy, it mainly shows, I think, two things:
- They clearly have run out of real arguments which, in turn, suggests that the end of publicly funded homeopathy is imminent.
- Homeopathic remedies are not an effective therapy against feeble-mindedness.
The Clinic for Complementary Medicine and Diet in Oncology was opened, in collaboration with the oncology department, at the Hospital of Lucca (Italy) in 2013. It uses a range of alternative therapies aimed at reducing the adverse effects of conventional oncology treatments.
Their latest paper presents the results of complementary medicine (CM) treatment targeted toward reducing the adverse effects of anticancer therapy and cancer symptoms, and improving patient quality of life. Dietary advice was aimed at the reduction of foods that promote inflammation in favour of those with antioxidant and anti-inflammatory properties.
This is a retrospective observational study on 357 patients consecutively visited from September 2013 to December 2017. The intensity of symptoms was evaluated according to a grading system from G0 (absent) to G1 (slight), G2 (moderate), and G3 (strong). The severity of radiodermatitis was evaluated with the Radiation Therapy Oncology Group (RTOG) scale. Almost all the patients (91.6%) were receiving or had just finished some form of conventional anticancer therapy.
The main types of cancer were breast (57.1%), colon (7.3%), lung (5.0%), ovary (3.9%), stomach (2.5%), prostate (2.2%), and uterus (2.5%). Comparison of clinical conditions before and after treatment showed a significant amelioration of all symptoms evaluated: nausea, insomnia, depression, anxiety, fatigue, mucositis, hot flashes, joint pain, dysgeusia, neuropathy.
The authors concluded that the integration of evidence-based complementary treatments seems to provide an effective response to cancer patients’ demand for a reduction of the adverse effects of anticancer treatments and the symptoms of cancer itself, thus improving patient’s quality of life and combining safety and equity of access within public healthcare systems. It is, therefore, necessary for physicians (primarily oncologists) and other healthcare professionals in this field to be appropriately informed about the potential benefits of CMs.
Why do I call this ‘wishful thinking’?
I have several reasons:
- A retrospective observational study cannot establish cause and effect. It is likely that the findings were due to a range of factors unrelated to the interventions used, including time, extra attention, placebo, social desirability, etc.
- Some of the treatments in the therapeutic package were not CM, reasonable and evidence-based. Therefore, it is likely that these interventions had positive effects, while CM might have been totally useless.
- To claim that the integration of evidence-based complementary treatments seems to provide an effective response to cancer patients’ is pure fantasy. Firstly, some of the CMs were certainly not evidence-based (the clinic’s prime focus is on homeopathy). Secondly, as already pointed out, the study does not establish cause and effect.
- The notion that it is necessary for physicians (primarily oncologists) and other healthcare professionals in this field to be appropriately informed about the potential benefits of CMs is not what follows from the data. The paper shows, however, that the authors of this study are in need to be appropriately informed about EBM as well as CM.
I stumbled across this paper because a homeopath cited it on Twitter claiming that it proves the effectiveness of homeopathy for cancer patients. This fact highlights why such publications are not just annoyingly useless but acutely dangerous. They mislead many cancer patients to opt for bogus treatments. In turn, this demonstrates why it is important to counterbalance such misinformation, critically evaluate it and minimise the risk of patients getting harmed.
On this blog, I have repeatedly discussed chiropractic research that, on closer examination, turns out to be some deplorable caricature of science. Today, I have another example of what I would call pseudo-research.
This RCT compared short-term treatment (12 weeks) versus long-term management (36 weeks) of back and neck related disability in older adults using spinal manipulative therapy (SMT) combined with supervised rehabilitative exercises (SRE).
Eligible participants were aged 65 and older with back and neck disability for more than 12 weeks. Co-primary outcomes were changes in Oswestry and Neck Disability Index after 36 weeks. An intention to treat approach used linear mixed-model analysis to detect between group differences. Secondary analyses included other self-reported outcomes, adverse events and objective functional measures.
A total of 182 participants were randomized. The short-term and long-term groups demonstrated significant improvements in back and neck disability after 36 weeks, with no difference between groups. The long-term management group experienced greater improvement in neck pain at week 36, self-efficacy at week 36 and 52, functional ability and balance.
The authors concluded that for older adults with chronic back and neck disability, extending management with SMT and SRE from 12 to 36 weeks did not result in any additional important reduction in disability.
What renders this paper particularly fascinating is the fact that its authors include some of the foremost researchers in (and most prominent proponents of) chiropractic today. I therefore find it interesting to critically consider the hypothesis on which this seemingly rigorous study is based.
As far as I can see, it essentially is this:
36 weeks of chiropractic therapy plus exercise leads to better results than 12 weeks of the same treatment.
I find this a most remarkable hypothesis.
Imagine any other form of treatment that is, like SMT, not solidly based on evidence of efficacy. Let’s use a new drug as an example, more precisely a drug for which there is no solid evidence for efficacy or safety. Now let’s assume that the company marketing this drug publishes a trial based on the hypothesis that:
36 weeks of therapy with the new drug plus exercise leads to better results than 12 weeks of the same treatment.
Now let’s assume the authors affiliated with the drug manufacturer concluded from their findings that for patients with chronic back and neck disability, extending drug therapy plus exercise from 12 to 36 weeks did not result in any additional important reduction in disability.
WHAT DO YOU THINK SUCH A TRIAL CAN TELL US?
My answer is ‘next to nothing’.
I think, it merely tells us that
- daft hypotheses lead to daft research,
- even ‘top’ chiropractors have problems with critical thinking,
- SMT might not be the solution to neck and back related disability.
I REST MY CASE.
Homeopathy for depression? A previous review concluded that the evidence for the effectiveness of homeopathy in depression is limited due to lack of clinical trials of high quality. But that was 13 years ago. Perhaps the evidence has changed?
A new review aimed to assess the efficacy, effectiveness and safety of homeopathy in depression. Eighteen studies assessing homeopathy in depression were included. Two double-blind placebo-controlled trials of homeopathic medicinal products (HMPs) for depression were assessed.
- The first trial (N = 91) with high risk of bias found HMPs were non-inferior to fluoxetine at 4 and 8 weeks.
- The second trial (N = 133), with low risk of bias, found HMPs was comparable to fluoxetine and superior to placebo at 6 weeks.
The remaining research had unclear/high risk of bias. A non-placebo-controlled RCT found standardised treatment by homeopaths comparable to fluvoxamine; a cohort study of patients receiving treatment provided by GPs practising homeopathy reported significantly lower consumption of psychotropic drugs and improved depression; and patient-reported outcomes showed at least moderate improvement in 10 of 12 uncontrolled studies. Fourteen trials provided safety data. All adverse events were mild or moderate, and transient. No evidence suggested treatment was unsafe.
The authors concluded that limited evidence from two placebo-controlled double-blinded trials suggests HMPs might be comparable to antidepressants and superior to placebo in depression, and patients treated by homeopaths report improvement in depression. Overall, the evidence gives a potentially promising risk benefit ratio. There is a need for additional high quality studies.
I beg to differ!
What these data really show amounts to far less than the authors imply:
- The two ‘double-blind’ trials are next to meaningless. As equivalence studies they were far too small to produce meaningful results. Any decent review should discuss this fact in full detail. Moreover, these studies cannot have been double-blind, because the typical adverse-effects of anti-depressants would have ‘de-blinded’ the trial participants. Therefore, these results are almost certainly false-positive.
- The other studies are even less rigorous and therefore do also not allow positive conclusions.
This review was authored by known proponents of homeopathy. It is, in my view, an exercise in promotion rather than a piece of research. I very much doubt that a decent journal with a responsible peer-review system would have ever published such a biased paper – it had to appear in the infamous EUROPEAN JOURNAL OF INTEGRATIVE MEDICINE.
So what?
Who cares? No harm done!
Again, I beg to differ.
Why?
The conclusion that homeopathy has a ‘promising risk/benefit profile’ is frightfully dangerous and irresponsible. If seriously depressed patients follow it, many lives might be lost.
Yet again, we see that poor research has the potential to kill vulnerable individuals.
Mini-scalpel acupuncture or acupotomy is a relatively new type of non-invasive acupuncture/ micro surgery using a small needle-scalpel invented by Professor Zhu Hanzhang around 30 years ago in China. It is a slightly thicker and more blunt instrument that gets under the skin and is able to break apart adhesions and muscle knots more effectively than a regular acupuncture needle would.
Sounds weird?
Never mind, the question is does it work!
A systematic review showed that almost all studies reported an effect of acupotomy on joint pain compared to a variety of controls. On reflection, this is hardly surprising:
- all the trials were from China;
- all had major methodological flaws.
This means that we need better studies to decide the efficacy question.
This new study investigated the efficacy and safety of mini-scalpel acupuncture (MA) for knee osteoarthritis (KOA) in an assessor-blinded randomized controlled pilot trial; this would provide information for a large-scale randomized controlled trial.
Participants (n = 24) were recruited and randomly allocated to the MA group (experimental) or acupuncture group (control). The MA group received treatment once a week for 3 weeks (total of 3 treatments), while the acupuncture group received treatment two times per week for 3 weeks (total of 6 treatments). The primary outcome was pain as assessed by a visual analogue scale (VAS). The secondary outcomes (intensity of current pain, stiffness, and physical function) were assessed using the short-form McGill Pain Questionnaire (SF-MPQ) and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC). Assessments were performed at baseline, 1, 2, and 3 during treatment and at week 5 (2 weeks after the end of treatment).
Of the 24 participants, 23 completed the study. Both groups showed significant improvements in VAS, SF-MPQ, and WOMAC. There were no significant differences between the MA and acupuncture groups. No serious adverse event occurred and blood test results were within normal limits.
The authors concluded that although both MA and acupuncture provide similar effects with regard to pain control in patients with KOA, MA may be more effective in providing pain relief because the same relief was obtained with fewer treatments. A large-scale clinical study is warranted to further clarify these findings.
I can recommend this article to anyone who wants a quick introduction into the critical analysis of clinical trials. It is a veritable treasure trove of mistakes, flaws, errors, fallacies etc. Here are just a few:
- The authors aim of investigating the safety of MA is unobtainable. It would require not 24 but probably 24 000 patients.
- The authors aim of investigating the efficacy of MA is equally unobtainable. It would require a much larger sample than 24, a sham control arm, identical treatment schedules, patient-blinding, etc.
- Calling the trial a ‘pilot’ is endearing but, except for the title and the insufficient sample size, this study has none of the characteristics of a pilot study.
- In their ‘introduction’, the authors state that miniscalpel acupuncture (MA) is a new subtype of acupuncture that is effective in treating chronic soft tissue injuries such as adhesions and contractures. This is clearly wrong but discloses their bias very plainly.
- The authors statement that both MA and acupuncture provide similar effects with regard to pain control in patients with KOA is misleading. It implies that both interventions had specific effects. Without a sham control arm, this is pure speculation.
- Similarly their assumption that MA may be more effective in providing pain relief because the same relief was obtained with fewer treatments, is pure fantasy.
- In fact, as MA requires injections of local anaesthetics, any outcome is heavily confounded by this addition.
- In the discussion section, the authors state that because MA is invasive and provides a strong stimulus, some participants complained of stiff and dull pain for few days after treatment. Yet, when reporting adverse effects in the results section, this was not mentioned.
- The way this study was designed, it should have been clear from the start that it would not produce any meaningful findings. Seen from this perspective, running the trial could even be seen as a breach of research ethics.
- According to the aims of a pilot study and the authors hope that their study would provide information for a large-scale randomized controlled trial, all reporting of outcomes is misplaced and should be replaced by information as to how a definitive trial should be conducted.
The following footnote is worth mentioning: This study is supported by a grant from the Ministry of Health & Welfare, Korea. It suggests to me that this ministry should urgently re-think its funding strategy and recruit some reviewers who are capable of critical analysis.
In my view, this is a lousy study which the authors decides to call ‘a pilot’ in order to get it published in a lousy journal.
