risk
The U.S. Department of Health and Human Services alleges that Jason James of the James Healthcare & Associates clinic in Iowa, USA — along with his wife, Deanna James, the clinic’s co-owner and office manager — filed dozens of claims with Medicare for a disposable acupuncture device, which is not covered by Medicare, as if it were a surgically implanted device for which Medicare can be billed. According to the lawsuit, more than 180 such claims were filed. Beginning in 2016, the lawsuit alleges, the clinic began offering an electro-acupuncture device referred to as a “P-Stim.” When used as designed, the P-Stim device is affixed behind a patient’s ear using an adhesive. The device delivers intermittent electrical pulses through a single-use, battery-powered attachment for several days until the battery runs out and the device is thrown away.
Because Medicare does not reimburse medical providers for the use of such devices, DHHS alleges that some doctors and clinics have billed Medicare for the P-Stim device using a code number that only applies to a surgically implanted neurostimulator. The use of an actual neurostimulator is reimbursed by Medicare at approximately $6,000 per claim, while P-Stim devices were purchased by the Keokuk clinic for just $667, DHHS alleges. The department alleges James knew his billings were fraudulent as the P-Stim device is “nowhere close to even resembling genuine implantable neurostimulators” and does not require surgery.
The lawsuit alleges that on June 15, 2016, when Jason James was contemplating the use of P-Stim devices at the Keokuk clinic, he sent a text message to P-Stim sales representative Mark Kaiser, asking, “Is there a limit on how many Neurostims can be done on one day? Don’t wanna do so many that gives Medicare a red flag on first day. Thanks.” After realizing the “large profit windfall” that could result from the billing practice, DHHS’s lawsuit alleges, James “told Mark Kaiser not to mention the Medicare reimbursement rate to his nurse practitioner or staff – only his office manager and biller needed that information.” James then pressured clinic employees to heavily market the P-Stim devices to patients, even if those patients were not agreeable or, after trying it, were reluctant to continue the treatment, the lawsuit claims.
In October 2016, the clinic’s supplier of P-Stim devices sent the clinic an email stating the company had “no position on what the proper coding might be for this device if billed to a third-party payer” such as an insurer or Medicare, according to the lawsuit. The company advised the clinic to “consult a certified biller/coder and/or attorney to ensure compliance.” According to the lawsuit, James then sent Kaiser a text message asking, “Should we be concerned?”
DHHS alleges the clinic’s initial reimbursement claims were submitted to Medicare through a nurse practitioner and were denied for payment due to the lack of a trained physician’s involvement. In response, the clinic hired Dr. Robert Schneider, an Iowa-licensed physician, to work at the clinic for the sole purpose of enabling James Healthcare & Associates to bill Medicare for the P-Stim devices, the lawsuit claims. James then informed Kaiser he had a goal of billing Medicare for 20 devices per month, which would generate roughly $125,573 of monthly income, the lawsuit alleges. The lawsuit also alleges Dr. Schneider rarely saw clinic patients in person, consulting with them instead through Facebook Live.
In April 2017, Medicare allegedly initiated a review of the clinic’s medical records, triggering additional communications between James and Kaiser. At one point, James allegedly wrote to Kaiser and said he had figured out why Medicare was auditing the clinic. “Anything over $7,500 is automatically audited for my area,” he wrote, according to the lawsuit. “We are now charging $7,450 to remove the audit.”
The clinic ultimately submitted 188 false claims to Medicare seeking reimbursement for the P-Stim devices, DHHS alleges, with Medicare paying out $4,100 and $6,300 per claim, for a total loss of $1,028,800. DHHS is suing the clinic under the federal False Claims Act and is seeking trebled damages of more than $3 million, plus a civil penalty of up to $4.2 million.
An attorney for the clinic, Michael Khouri, said Wednesday he believe the federal government’s lawsuit was filed in error because a settlement in the case had already been reached. However, the assistant U.S. attorney handling the case said no settlement in the case had been finalized and the lawsuit was not filed in error.
Previous legal cases
In 2015, the Iowa Board of Chiropractic charged Jason James with knowingly making fraudulent or untrue representations in connection with his practice, engaging in conduct that was harmful or detrimental to the public, and making untruthful statements in advertising. The board alleged James told patients they would be able to stop taking diabetes medication through the use of a diet and nutrition program, and that he had claimed to be providing extensive laboratory tests when not all of the tests for which he billed were ever conducted. The board also claimed James referred patients to a medical professional who was not licensed to practice in Iowa. The case was resolved with a settlement agreement in which James agreed to pay a $500 penalty and complete 10 hours of education in marketing and ethics.
In 2019, Schneider sued the clinic for failing to comply with the terms of his employment agreement. Court exhibits indicate the agreement stipulated that Schneider was to work no more than two days per month and would collect $2,000 for each day worked, plus $250 per month for consulting, plus “$250 per device over six per calendar month.” In March 2020, a jury ruled in favor of the clinic and found that it had not breached its employment agreement with Schneider.
_________________________
Before some chiropractors now claim that such cases represent just a few rotten apples in a big basket of essentially honest chiropractors, let me remind them of a few previous posts:
- A $2.6M Insurance Fraud by Chiropractors and Doctors?
- Fraud and sex offences by chiropractors
- Chiropractic therapy for gastrointestinal diseases. Evidence of scientific misconduct?
- Twenty Things Most Chiropractors Won’t Tell You
- The Dark Side of Chiropractic Care
- Chiropractic subluxation: the myth must be kept alive
- CHIROPRACTIC: an early and delightful critique
- Students of chiropractic condemn the ‘unacceptable behaviour’ of some chiropractors and their professional organisations
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Chiropractor is in the dock for not wearing a mask
- “The uncensored truth” about COVID-19 vaccines” … as told by some chiro loons
To put it bluntly: chiropractic was founded by a crook on a bunch of lies and unethical behavior, so it is hardly surprising that today the profession has a problem with ethics and honesty.
It been reported that the German HEILPRAKTIKER, Holger G. has been sentenced to serve a total of 4 years and three months behind bars. He made himself a pair of glasses out of aluminum foil and appeared at the start of his trial wearing a Corona protective mask. The accusations against him were fierce: He was accused of having issued false Corona vaccination certificates en masse in Munich and of having given medication to patients. A woman, who had contracted Corona and had been treated by Holger G. with vitamin solutions, had died last year.
According to the verdict, Holger G. had violated the German Medicines Act. The court announced he was also convicted of 96 counts of dangerous bodily harm and 102 counts of unauthorized trading in prescription drugs. In addition, the court ordered the HEILPRAKTIKER to be placed in a rehab facility.
The 71-year-old MAN had issued Corona vaccination cards since April 2021, without actually vaccinating the people concerned. For the forged vaccination cards, he charged several tens of thousands of Euros. In addition, the former HEILPRAKTIKER illegally sold prescription drugs. The judgment is so severe because Holger G. has form. He also ordered to bear the costs of the proceedings.
___________________________
I have long criticized the German HEILPRAKTIKER. In my recent book on the subject, I make the following points:
– Today, no one can provide reliable data on the number of HEILPRAKTIKER in Germany.
– The training of HEILPRAKTIKER is woefully inadequate.
– The far-reaching rights of the HEILPRAKTIKER are out of proportion to their overt lack of competence.
– This disproportion poses a serious danger to patients.
– This danger is further increased by the fact that there is no effective control of the activity of the HEILPRAKTIKER does not take place.
– Existing laws are almost never applied to the HEILPRAKTIKER.
– Most HEILPRAKTIKER mislead the public unhindered with untenable therapeutic claims.
– The federal government seems to put off over and over again any serious discussion of the HEILPRAKTIKER.
Cases like the one above show that it is high time for reform – or, should that prove impossible, the discontinuation of this utterly obsolete and highly dangerous profession.
“We are hugely concerned about the welfare of doctors and healthcare workers with long COVID”. These are the first words of a comprehensive survey of UK doctors with post-acute COVID health complications. It reveals that these doctors experience symptoms such as:
- fatigue,
- headaches,
- muscular pain,
- nerve damage,
- joint pain,
- respiratory problems.
Around 60% of doctors said that post-acute COVID ill health has affected their ability to carry out day-to-day activities on a regular basis. 18% reported that they were now unable to work due to their post-acute COVID ill-health, and only 31% said they were working full-time, compared with more than half before the onset of their illness.
The report demands financial support for doctors and healthcare staff with post-acute COVID, post-acute COVID to be recognized as an occupational disease in healthcare workers, with a definition that covers all of the debilitating disease’s symptoms and for improved access to physical and mental health services to aid comprehensive assessment, appropriate investigations and treatment. The report also calls for greater workplace protection for healthcare staff risking their lives for others and better support for post-acute COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
In November 2021, an online survey investigating the emotional states of depression, anxiety, stress, compassion satisfaction, and compassion fatigue was administered to 78 Italian healthcare workers (HCWs). Between 5 and 20% of the cohort showed the effects of the adverse psychological impact of the pandemic and more than half of them experienced medium levels of compassion fatigue as well as a medium level of compassion satisfaction. The results also show that those with fewer years of clinical practice might be at greater risk of burnout, anxiety, and stress symptoms and might develop a lower level of compassion satisfaction. Moreover, the factors that potentially contribute to poor mental health, compassion fatigue, and compassion satisfaction seem to differ between residents and specialist physicians.
A cross-sectional study was conducted from September 2021 to April 2022 and targeted all physicians working at King Fahd Hospital of the University, Al Khobar, Saudi Arabia. Patient Health Questionnaire-9 and General Anxiety Disorder-7 were used to elicit self-reported data regarding depression and anxiety, respectively. In addition, sociodemographic and job-related data were collected. A total of 438 physicians responded, of which 200 (45.7%) reported symptoms of depression and 190 (43.4%) of anxiety. Being aged 25-30 years, female, resident, and reporting a reduction in work quality were factors significantly associated with both anxiety and depression. Female gender (AOR = 3.570; 95% CI = 2.283-5.582; P < 0.001), working an average 9-11 hours/day (AOR = 2.130; 95% CI = 1.009-4.495; P < 0.047), and self-perceived reduction in work quality (AOR = 3.139; 95% CI = 2.047-4.813; P < 0.001) were significant independent predictors of anxiety. Female gender (AOR = 2.929; 95% CI = 1.845-4.649; P < 0.001) and self-perceived reduction in work quality (AOR = 3.141; 95% CI = 2.053-4.804; P < 0.001) were significant independent predictors of depression.
An observational, multicenter cross-sectional study was conducted at eight tertiary care centers in India. The consenting participants were HCWs between 12 and 52 weeks post-discharge after COVID-19 infection. The mean age of the 679 eligible participants was 31.49 ± 9.54 years. The overall prevalence of COVID sequelae was 30.34%, with fatigue (11.5%) being the most common followed by insomnia (8.5%), difficulty in breathing during activity (6%), and pain in joints (5%). The odds of having any sequelae were significantly higher among participants who had moderate to severe COVID-19 (OR 6.51; 95% CI 3.46-12.23) and lower among males (OR 0.55; 95% CI 0.39-0.76). Besides these, other predictors for having sequelae were age (≥45 years), presence of any comorbidity (especially hypertension and asthma), category of HCW (non-doctors vs doctors), and hospitalization due to COVID-19.
Such data are scary. Not only will we have a tsunami of long-Covid patients from the general public, and not only do we currently lack effective causal treatments for the condition, but also is the number of HCWs who are supposed to deal with all this drastically reduced.
Most if not all countries are going to be affected by these issues. But the UK public might suffer the most, I fear. The reasons are obvious if you read a previous post of mine: in the UK, we have significantly fewer doctors, nurses, hospital beds, and funding (as well as politicians who care and would be able to do something about the problem) than in other comparable countries. To me, this looks like the emergence of a perfect storm.
An impressive article by John Mac Ghlionn caught my attention. Allow me to quote a few passages from it:
The U.S. House of Representatives and the U.S. Senate recently reintroduced legislation to increase access to Medicare-covered services provided by chiropractors. Last year, the US chiropractic market size was worth $13.13 Billion. By the end of the decade, it will be worth over $18 billion. Each year, a whopping 35 million Americans seek chiropractic care.
But why? It’s a questionable science full of questionable characters.
Last year, a Georgia woman was left paralyzed and unable to speak after receiving a neck adjustment from a chiropractor. She’s not the first person to have had her life utterly ruined by a chiropractor, and chances are she won’t be the last. Many patients who visit chiropractors suffer severe side effects; some lose their lives…
As Dr. Steven Novella has noted, what used to be fraud is now known as holistic medicine. Dr. Edzard Ernst, a retired British-German physician and researcher, has expertly demonstrated the many ways in which chiropractic treatments are rooted not in science, but in mystical concepts…
Spinal adjustments, also known as “subluxations,” are also common. A dangerous practice that has been heavily criticized, spinal manipulations are associated with a number of adverse effects, including the risk of stroke. As Dr. Ernst has noted, the cost-effectiveness of this particular treatment “has not been demonstrated beyond reasonable doubt.”
Not content with spinal and neck manipulations, some chiropractors offer to treat other conditions — like diabetes, for example. They are not trained to treat diabetes. Other chiropractors appear to take joy in torturing infants. In August of 2018, a chiropractor made headlines for all the wrong reasons when a video emerged showing him hanging a two-week-old newborn upside down by the ankles…
Finally, as I alluded to earlier, the chiropractic community is full of fraudsters. In 2019, in the US, 15 chiropractors were charged in an insurance fraud and illegal kickback operation. More recently, in February of this year, a New York federal judge sentenced Patrick Khaziran to 30 months in prison after he pleaded guilty to being part of a widespread scheme that defrauded the NBA out of at least $5 million. In recent times, the chiropractic community has come under scrutiny for abusive care and illegal billing practices. When it comes to instances of healthcare fraud, chiropractic medicine is unrivaled.
None of this should come as a surprise. After all, the entire chiropractic community was constructed on a foundation of lies. As the aforementioned Dr. Ernst told me, we should be skeptical of what chiropractors are offering, largely because the whole practice was founded “by a deluded charlatan, who insisted that all human diseases are due to subluxations of the spine. Today, we know that chiropractic subluxations are mere figments of Palmer’s imagination. Yet, the chiropractic profession is unable to separate itself from the myth. It is easy to see why: without it, they would at best become poorly trained physiotherapists without any raison d’etre.”
… Dr. William T. Jarvis famously referred to chiropractic as “the most significant nonscientific health-care delivery system in the United States.” Comparing the chiropractic community to a cult, Dr. Jarvis wondered, somewhat incredulously, why chiropractors are licensed to practice in all 50 US states. The entire profession, he warned, “should be viewed as a societal problem, not simply as a competitor of regular health-care.”
___________________________
In my view, this is an impressive article, not least because it is refreshingly devoid of the phenomenon known as ‘false balance, e.g. a chiropractor being invited to add his self-interested views at the end of the paper claiming, for instance, “we have years of experience and cause far less harm than real doctors”.
Cervical artery dissection (CeAD), which includes both vertebral artery dissection (VAD) and carotid artery dissection (CAD), is the most serious safety concern associated with cervical spinal manipulation (CSM). This study evaluated the association between CSM and CeAD among US adults.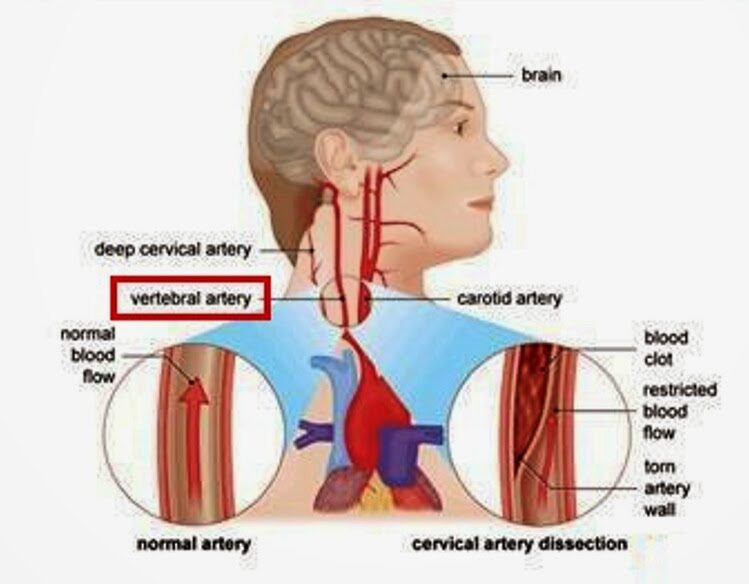
Through analysis of health claims data, the researchers employed a case-control study with matched controls, a case-control design in which controls were diagnosed with ischemic stroke, and a case-crossover design in which recent exposures were compared to exposures in the same case that occurred 6-7 months earlier. The researchers evaluated the association between CeAD and the 3-level exposure, CSM versus office visit for medical evaluation and management (E&M) versus neither, with E&M set as the referent group.
2337 VAD cases and 2916 CAD cases were identified. Compared to population controls, VAD cases were 0.17 (95% CI 0.09 to 0.32) times as likely to have received CSM in the previous week as compared to E&M. In other words, E&M was about 5 times more likely than CSM in the previous week in cases, relative to controls. CSM was 2.53 (95% CI 1.71 to 3.68) times as likely as E&M in the previous week among individuals with VAD than among individuals experiencing a stroke without CeAD. In the case-crossover study, CSM was 0.38 (95% CI 0.15 to 0.91) times as likely as E&M in the week before a VAD, relative to 6 months earlier. In other words, E&M was approximately 3 times more likely than CSM in the previous week in cases, relative to controls. Results for the 14-day and 30-day timeframes were similar to those at one week.
The authors concluded that, among privately insured US adults, the overall risk of CeAD is very low. Prior receipt of CSM was more likely than E&M among VAD patients as compared to stroke patients. However, for CAD patients as compared to stroke patients, as well as for both VAD and CAD patients in comparison with population controls and in case-crossover analysis, prior receipt of E&M was more likely than CSM.
What seems fairly clear from this and a previous similar analysis by the same authors is, I think, this: retrospective studies of this type can unfortunately not provide us with much reliable information about the risks of spinal manipulation. The reasons for this are manyfold, e.g.: less than exact classifications in patients’ records, or the fact that multiple types of spinal manipulations exist of which only some might be dangerous.
Guest post by Ken McLeod
Readers will have no trouble recalling that crank ‘naturopath’ Barbara O’Neill has graced these pages several times. She is subject to a Permanent Prohibition Order by the New South Wales Health Care Complaints Commission. It goes like this:
“The Commission is satisfied that Mrs O’Neill poses a risk to the health and safety of members of the public and therefore makes the following prohibition order:
“Mrs O’Neill is permanently prohibited from providing any health services, as defined in s4 Of the Health Care Complaints Act 1993, whether in a paid or voluntary capacity.’ 1
Evidently Ms O’Neill has scrambled her chakras or muddled her meridians because she continues to forget the Order. For example;
O’Neill did a video interview concerning the Prohibition Order and that has been posted online at YouTube.2 The video was posted ‘1 year ago,’ has had 323,000 views and had 1,598 comments. She goes into great detail what she regards as the appalling treatment at the hands of the HCCC.
In the video she admits that she has continued to travel the world spreading her lies and misrepresentations. Some of the lies are that she is a naturopath, and was a nurse, and ‘I used to work in the Operating Theatre as a psychiatric nurse….’
In the video at 53:20 in the video she refers to an aboriginal man ‘Dan’ who works at her Misty Mountain Lifestyle Retreat, (note the present tense), who is in his 50s was obese and recently had a heart attack, ‘was on a lot of medications,’ ‘was a bit scared of coming off medications,’ ‘I said Dan, I think it’s time to stop your blood pressure medications, you’re going too low, you’re a 100 over 60,’ ‘three days later his blood pressure was 100 over 75,….’ 3
Call me a cynic, but that strikes me as rather dangerous advice, worthy of an investigation by the HCCC. Meanwhile, there is no sign of ‘Dan ‘ in Misty Mountain’s ‘About page.’ Dan’s brother Dave appears, but no Dan.4 Could it be that O’Neill’s advice led to some incapacity? Tips are welcome.
Meanwhile, readers could learn much more about Barbara O’Neill at Wikipedia.5
This article first appeared in the June issue of the Australian Skeptic Magazine,6 reprinted with kind permission.
REFERENCES
1 https://www.hccc.nsw.gov.au/decisions-orders/public-statements-and-warnings/public-statement-and-statement-of-decision-in-relation-to-in-relation-to-mrs-barbara-o-neill
2 https://www.youtube.com/watch?v=tsbK5TLdAPo
3 This was dangerous and reckless advice. The full transcript is here
4 https://www.mmh.com.au/our-story
5 https://en.wikipedia.org/wiki/Barbara_O%27Neill
6 https://www.skeptics.com.au/magazine/
It has been reported that a GP has been erased from the medical register after a disciplinary tribunal concluded yesterday that her statements on vaccines amounted to misconduct.
Dr Jayne Donegan, who no longer works as an NHS GP, was found by the tribunal to have ‘encouraged parents to mislead healthcare professionals about their children’s diet or immunization history’. The UK General Medical Council (GMC) brought several allegations against Dr Donegan, about statements made between 2019 and 2020, however, the determination of impaired fitness to practise (FTP) and subsequent erasure was based solely on her suggestions to parents.
The tribunal determined that her misconduct ‘posed an ongoing risk to patient safety given her lack of insight and lack of remediation’ and that ‘public confidence would be undermined’ if such a doctor was allowed to remain in practice. An immediate order of suspension was imposed, which the tribunal determined necessary for the ‘protection of the public’. Other GMC allegations, such as Dr. Donegan’s statements failing to ‘give balanced information on the risks and benefits of immunization’, were proved true by the tribunal but were not determined to be serious misconduct.
Dr. Donegan works as a homeopathic and naturopathic practitioner and has been ‘researching disease ecology and vaccination since 1994’, according to her website. The tribunal considered statements made by Dr. Donegan in a consultation with an undercover reporter and during her lectures on vaccination. She had said that the historical decline in deaths from whooping cough was because of sanitation and surgeons, not vaccinations. She had also suggested to audiences at her lectures that they could avoid answering questions from healthcare professionals about their child’s immunization history. When asked by an audience member about this, Dr. Donegan had said: ‘I thought what am I going to do because if I were you, I could just forge something but I can’t do that because I am a doctor and I would get struck off and I really would get struck off. What can I do? I thought maybe I can do something homeopathic because they are not having it. In the meantime, I wrote “Yes, I’ll get it done” thinking what will I do and they never came back to me, so when the next one went I just said “yes. The main thing is, don’t stick your head above the parapet because you make it difficult for them. If you say they are not vaccinated, they say they can’t go on the trip or they say “They could but the insurers won’t insure us”, so just keep saying “yes” but don’t say I said that.’
The tribunal concluded that comments like this made it clear Dr. Donegan was aware this was a ‘serious matter that could result in her being struck off’, despite her defense that she was simply ‘making people laugh’. The MPTS tribunal chair Mr Julian Weinberg said: ‘The Tribunal considered that honest and accurate communication of an individual’s medical history forms an essential part of ongoing patient healthcare and that any attempt to undermine this risks the safety of patients. It noted that whilst no dishonesty was found against Dr. Donegan, the Tribunal has found that she encouraged parents to be dishonest with healthcare professionals by, for example, forging medical documents/records, thereby undermined this essential quality of the doctor/patient relationship.’ Mr Weinberg highlighted that the tribunal’s findings did not concern ‘the rights or wrongs of her views on immunization’ but rather her encouragement to parents to mislead healthcare professionals.
Dr. Donegan said in response to the decision: ‘I boycotted the GMC’s political show trial against me which ended today. Serious irregularities include bogus dishonesty charges and bogus accusations that I put newborns at risk of serious harm.’ She added: ‘Being struck off by a corrupt GMC is a small price to pay for taking a lawful ethical stand for the safety of British children.’
Apparently, Dr. Donegan even claimed that she is delighted to be struck off the register of medical practitioners – and so, I presume, are many of us reading this post!
A German paper reported the following horrific story about a Heilpraktiker, an alternative practitioner without a medical degree:
Starting July 7, Torben K. (46) from Solingen will have to answer to the Wuppertal Regional Court. The Heilpraktiker is said to have injected silicone oil into the penis and testicles of a man († 32) at his request. Shortly thereafter, the patient developed health problems and later died.
The prosecution accuses the Heilpraktiker from Solingen of bodily injury resulting in death and violation of the Heilpraktikergesetz.
According to the report, the victim had traveled to Solingen in June 2019, where the defendant had given him the injection in his apartment.
Back home, the 32-year-old patient suddenly developed shortness of breath, had to be hospitalized, then transferred to the university hospital in Giessen. Seven months after the injection, he is dead. According to the indictment, the patient suffered multiple organ failure as a result of blood poisoning.
Three days of trial are scheduled. The defendant faces up to 15 years in prison.
_________________________
I had never heard of intra-testicular injections. So, I did a Medline search and found just two papers of the procedure in human patients:
Blunt trauma is the most common mechanism of injury to the scrotum and testicle. Surgical exploration with primary repair, hematoma evacuation, and de-torsion are common surgical interventions. A 20-year-old male with no previous medical history presented after a high-speed motor vehicle collision. Ultrasonography demonstrated heterogeneous changes of the tunica albuginea and decreased arterial flow to bilateral testicles. He was subsequently taken to the operating room for surgical exploration, which revealed bilateral mottled testes with questionable viability. Papaverine was injected into each testicle, which resulted in visibly increased perfusion and subsequent preservation of the testicles. Conclusion: Current evidence on the use of papaverine is isolated to testicular torsion. Additional research should be conducted on the use of papaverine in blunt testicular trauma. Papaverine injection may be a valuable treatment option when inadequate perfusion is observed intra-operatively.
No 2:
Purpose: We describe a simple technique to deliver local anaesthetic for percutaneous testis biopsies.
Materials and methods: With the testis held firmly, a 25 gage needle is used to inject lidocaine, without epinephrine, into the skin and dartos superficial to the testis, then the needle is advanced through the tunica albuginea and 0.5 mL to 1.0 mL of lidocaine is injected directly into the testis. The testis becomes slightly more turgid with the injection. A percutaneous biopsy is then immediately performed.
Results: Intra-testicular lidocaine, (without the need of a cord block or any sedation) was used on a total of 45 consecutive patients having percutaneous testicular biopsies. Procedure time was short (averages less than 5 minutes) and anaesthesia was profound. There was no change in the number of seminiferous tubules for evaluation compared to biopsies on men using a cord block. Only 1/45 men had a post-procedure testicular hematoma (this resolved in 4 weeks).
Conclusions: Intra-testicular lidocaine appears to be a simple, rapid and safe method to provide anaesthesia for a percutaneous testis biopsy.
All the other papers on intra-testicular injections were about animal experiments, mostly for exploring means of castration. This renders the above case even more unusual. The Heilpraktiker’s defense might stress that the patient wanted the treatment. That may be so but is it a valid excuse? No, of course not. In my view – and I am just a medic, not a lawyer – the Heilpraktiker is responsible for the treatment regardless of how much the patient insisted on it.
I missed this paper when it first came out in 2022. Yet, it seems potentially quite important and I, therefore, feel like discussing it here:
President of the UNESCO Committee on Bioethics Stefan Semplici called on the governments of all countries to ensure free and wider access of their citizens to alternative medicine and pay for this therapy through health insurance. Alternative medicine based on tradition – traditional medicine, in many poor countries is the only treatment option for the population. In developed countries, and especially in China and India, it enjoys well-deserved prestige (for example, acupuncture and herbal medicine) and is often integrated into the public health system.
The International Committee on Bioethics of UNESCO announced the recognition of these alternative therapies as an option for medical practice and, at the same time, as part of the identity of the cultural traditions of various nations. The UNESCO Universal Declaration on Bioethics and Human Rights includes the right to the highest attainable standard of health (Article 14), the right to respect for pluralism and cultural diversity (Article 12) and traditional knowledge (Article 17). The purpose of this document is to establish criteria for the respect and acceptability of different types of medicine without compromising the assurance of quality and patient safety that is essential in all treatments.
In order to adapt the traditions of traditional therapies to advances in medicine, this international organization calls on governments and the scientific community to collaborate with practitioners of alternative therapies to evaluate their effectiveness and safety and develop therapeutic standards and protocols for integrating traditional medicine into healthcare system. The UNESCO International Bioethics Committee believes that these methods should be seen as complementary to modern medicine, and not just an alternative to it.
_________________________
The United Nations Educational, Scientific and Cultural Organization (UNESCO) is an agency of the United Nations aimed at promoting world peace and security through international cooperation in education, arts, sciences, and culture. UNESCO’s International Bioethics Committee (IBC) is a body of 36 independent experts that follows progress in the life sciences and its applications in order to ensure respect for human dignity and freedom.
I have to say that I rarely have seen an announcement in so-called alternative medicine (SCAM) that is more confusing and less well thought through. The UNESCO Committee on Bioethics wants:
- alternative therapies as an option for medical practice,
- the highest attainable standard of health,
- to collaborate with practitioners of alternative therapies to evaluate their effectiveness and safety.
When I first read these lines, I asked myself: who on earth wrote such nonsense? It was certainly not written by someone who understands healthcare, SCAM, and evidence-based medicine.
As discussed almost permanently on this blog, most forms of SCAM have not been shown to generate more good than harm. This means that employing them ‘as an option in medical practice’ cannot possibly produce ‘the highest attainable standards of health’. In fact, the UNESCO plan would lead to lower not higher standards. How can a committee on bioethics not realize that this is profoundly unethical?
Collaboration with practitioners of alternative therapies to evaluate SCAM’s effectiveness and safety sounds a bit more reasonable. It ignores, however, that tons of evidence already exist but fail to be positive. Why do these experts in bioethics not advocate to first make a sober assessment of the published literature?
I must say that the initiative of the UNESCO Committee on Bioethics puzzles me a lot and disturbs me even more.
I’d be keen to learn what you think of it.
The current secondary analysis based on the WHO database (VigiBase) of individual case safety reports (ICSRs) focuses on the suspected cutaneous adverse drug reactions (ADRs) linked to traditional medicines (TMs).
All the ICSRs reported between 1st January 2016 and 30th June 2021 from the UN Asia region in VigiBase where at least one TM was suspected to cause cutaneous ADRs were included in the study. Data regarding demographic details, suspected drug, adverse reaction as per MedDRA term, the seriousness of the reaction, de-challenge, re-challenge, and clinical outcome for suspected cutaneous ADRs associated with TM were obtained from VigiBase and analyzed for frequency of reported events and suspected medicines.
A total of 3,523 ICSRs with 5,761 ADRs related to “skin and subcutaneous tissue disorders” were included in the analysis. Amongst these, 6.8% of ICSRs were reported as serious.
The most common ADRs were:
- pruritus (29.6%),
- rash (20.3%),
- urticaria (18.9%),
- hyperhidrosis (3.3%).
Artemisia argyi H.Lév. and Vaniot. (14.9%), Ginkgo biloba L. (5.1%), Vitis vinifera L. (4%), Vitex agnus-castus L. (3.8%), Silybum marianum (L.), Gaertn (3.5%), and Viscus album L. (2.7%) were some commonly suspected TMs for cutaneous ADRs. There were 46 cases of Stevens-Johnson syndrome and toxic epidermal necrolysis reported with TMs during the study period. Death was reported in 5 ICSRs.
The authors concluded that TMs are linked with various cutaneous ADRS ranging from pruritus to toxic epidermal necrolysis which may have serious consequences. TMs listed as suspected offending agents in this analysis, should be kept in mind while dealing with suspected cutaneous ADRs. Clinicians should be more vigilant in detecting and reporting events associated with TMs.
Herbal remedies have a reputation for being time-tested, gentle, harmless, and benign. Reports such as this one might make us doubt this cliche. More importantly, they should force us to ask whether the remedy we are tempted to try truly does generate more good than harm. In most instances, I fear, the answer is not positive.


