holistic
We all need cheering up a bit, I’m sure.
Luckily, I found just the thing.
The New York Post reported that a former Versace model, Tom Casey, is crediting his youthful looks to drinking his own urine, and to perineum sunning (exposing your butt hole to sunshine). “I drink my own urine every morning — I call it hair of the dog!” Casey proclaimed, “the feeling is electric.” The ex-model also flushes his urine into his rectum and applies it to his skin as a moisturizer. 
“It wasn’t as bad as the mental barrier in my own mind,” the ex-catwalk star reminisced. “I felt a cool buzz. Intuitively, it just felt good. I drank my urine on and off for a while from there.”
Casey began drinking his own urine on a daily basis back in 2008 and hasn’t looked back. He has even completed a “seven-day urine fast,” drinking nothing but his own urine for an entire week. He also bottles his pee, lets it “ferment” and uses it in an enema. “I would cultivate my own urine and ferment it in a sealed Mason jar for two weeks before transferring it into my rectum,” he explained. “Aged urine enemas are so powerful for your health and I got my six-pack abs after doing them. It flushed out my gut and that’s when I got really ripped.”
Casey uses his urine also as a moisturizer, which he believes helps maintain his appearance. “What it did for my mood and muscle building was amazing. I put it on my skin, especially when I’m on the beach, and it’s so electrifying and strengthening,” he cooed. “It’s a big psychological leap for people to use their own urine as a moisturizer but it’s so euphoric and anti-aging. Uric acid is used in high-end skin care products.”
“I’m 55 years old and most people don’t look and feel like I do at my age. No one can deny that I’m ripped, and that’s down to the fact that I love being extremely healthy and practicing natural healing methods.”
Casey claims Big Pharma is terrified of people learning that the secret to their health lies within themselves.
“What so many pharmaceutical companies don’t want to tell you is that we as humans are the secret to health. That’s what I try to teach people in everything I do,” he stated.
“People should be scared if they’re eating s–tty food and doing pharmaceutical drugs. Why should they be scared to try their own urine?”
____________________________
Personally, I feel that Casey believes the sun might be shining out of his arse. In any case, it is hard to deny that the former Versace model is suffering from proctophasia and/or is taking the piss.
This review summarized the available evidence on so-called alternative medicine (SCAM) used with radiotherapy. Systematic literature searches identified studies on the use of SCAM during radiotherapy. Inclusion required the following criteria: the study was interventional, SCAM was for human patients with cancer, and SCAM was administered concurrently with radiotherapy. Data points of interest were collected from included studies. A subset was identified as high-quality using the Jadad scale. Fisher’s exact test was used to assess the association between study results, outcome measured, and type of SCAM.
Overall, 163 articles met inclusion. Of these, 68 (41.7%) were considered high-quality trials. Articles published per year increased over time. Frequently identified therapies were biologically based therapies (47.9%), mind-body therapies (23.3%), and alternative medical systems (13.5%). Within the subset of high-quality trials, 60.0% of studies reported a favorable change with SCAM while 40.0% reported no change. No studies reported an unfavorable change. Commonly assessed outcome types were patient-reported (41.1%) and provider-reported (21.5%). The rate of favorable change did not differ based on the type of SCAM or outcome measured.
The authors concluded that concurrent SCAM may reduce radiotherapy-induced toxicities and improve quality of life, suggesting that physicians should discuss SCAM with patients receiving radiotherapy. This review provides a broad overview of investigations on SCAM use during radiotherapy and can inform how radiation oncologists advise their patients about SCAM.
In my recent book, I have reviewed the somewhat broader issue of SCAM for palliative and supportive care. My conclusions are broadly in agreement with the above review:
… some forms of SCAM—by no means all— benefit cancer patients in multiple ways… four important points:
• The volume of the evidence for SCAM in palliative and supportive cancer care is currently by no means large.
• The primary studies are often methodologically weak and their findings are contradictory.
• Several forms of SCAM have the potential to be useful in palliative and supportive cancer care.
• Therefore, generalisations are problematic, and it is wise to go by the current best evidence …
One particular finding of the new review struck me as intriguing: The rate of favorable change did not differ based on the type of SCAM. Combined with the fact that most studies are less than rigorous and fail to control for non-specific effects, this indicates to me that, in cancer palliation (and perhaps in other areas as well), SCAM works mostly via non-specific effects. In other words, patients feel better not because the treatment per se was effective but because they needed the extra care, attention, and empathy.
If this is true, it carries an important reminder for oncology: cancer patients are very vulnerable and need all the empathy and compassion they can get. Seen from this perspective, the popularity of SCAM would be a criticism of conventional medicine for not providing enough of it.
What on earth is ‘reincarnation therapy’?
Here is a website that explains it quite well:
The concept of reincarnation is that our souls can experience many lifetimes directly thru centuries, perhaps even thousands of years. Life gives more meaning when you have a deeper understanding of the bigger picture. Earlier life regression has been recognized as a legal form of spiritual healing. No matter what religion you follow or not, you get the feeling that you are more than a physical body. You meet the essence of your soul, connected to a greater universal energy, perhaps for the first time in your life. For those who experience this, they get inner peace…
Reincarnation therapy is a technique that has been and has been used successfully for many years, and is a comprehensive therapy for body, mind and soul based on cause and effect (karma). Reincarnation can help people cure emotional trauma or an injury that you have transferred from a past life or in this life. The technique has not only been used by monks and theologians for many years, but has been more embraced by today’s psychologists, psychiatrists and science. If reincarnation is not a true phenomenon, but just an indefinite theory, how is it that the technique is so successful in healing?
The concept of reincarnation has been present in almost any culture since ancient times. Egyptians, Greeks and Romans, and all believed in the “transfer of souls” from one body to another after death. Although reincarnation is not part of official Christianity, many Christians believe in it or at least accept the opportunity. No matter what we know about this awareness, there is still so much we do not know. The most important thing we can say about previous reincarnation therapy is that it is a method that provides deep and permanent healing in a short time. You do not have to believe in reincarnation to receive healing from this amazing technique.
Reincarnation therapy can change your life! It will help you find your potential, create more compassion and love, gain access to wisdom, peace and guidance for you and others. It can reveal the purpose of life and the reason for incarnation, strengthen the clarity of the spiritual nature of the spirit and help you overcome fear of death. After several regression sessions, many clients report after the regression, about a greater sense of inner peace and love when they understand their choice of living conditions and what they need to learn.
Another website offers more concrete explanations:
Everyone can do reincarnation therapy, but it is especially important for people who experience recurring experiences in current life. Such as, for example, health problems or recurring relationship problems, fears, phobias, family problems, mental disorders, etc. Through the therapy, the problems can suddenly disappear by gaining insight into the cause. It is also interesting for people who are just curious what they have been in the past life. A person can experience the most special experiences. You may remember people or places where you have never been before in current life. There are cases that people suddenly spoke a language they could never speak before. The main purpose for experiencing of Reincarnation Therapy is to confirm for yourself and to know that there is always life even after death. This will change your way of thinking and give you more insight about life.
… Reincarnation therapy takes +/- 3 hours. You wil get into a trance, through which you feel, see, smell, taste everything, etc. We do not work with Hypnosis. Hypnosis is not good for the subconscious mind and many people don’t remember anything after that either. We want you to really experience everything and to experience this as a development.
So, reincarnation therapy is similar to or even identical with past life regression therapy, a so-called alternative medicine (SCAM) that we have recently discussed. 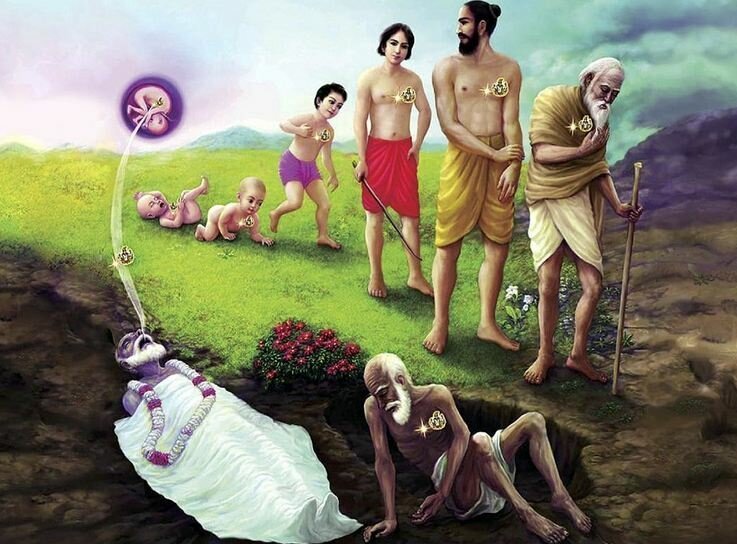
What conditions does it treat or cure? Yet another website provides the answer to this question:
- all kinds of phobias;
- relationship problems;
- depression;
- addictions;
- chronic pain;
- panic attacks;
- insomnia;
- headache,
- etc.
The ‘etcetera’ presumably means that reincarnation therapy is a panacea. That sounds most encouraging! There is just one tiny little problem: there is not a jot of evidence. Yet, I am sure that reincarnation therapy can change your life: in case you are gullible enough to believe all the BS, pay through your nose for an endless series of sessions and thus end up poor.
The 13th European Congress for Integrative Medicine is about to take place online between 4 and 7 November 2021. It will host 125+ speakers presenting from around the world. The programme will cover the following topics.
- Anthroposophic Medicine
- Arts in Healthcare
- Acupuncture
- Antimicrobial Resistance
- Ayurveda
- Covid Research
- Diabetes
- Homeopathy
- Immunology
- Integrative Oncology
- Lifestyle Medicine
- Medical Education
- Mental Health & Stress Management
- Mind and Body Connection
- Mistletoe Therapy
- Nutrition, Gut Health & Microbiome
- Pain Management
- Patient Activation & Self-Management
- Planetary & Environmental Health
- Research and Evaluation
- Social Prescribing
- Traditional Health
- Yoga
Even looking at the more detailed list of lectures, I did not find a single contribution on conventional medicine (“Integrative medicine combines conventional medicine with…” [see below]) or a lecture that is remotely critical of integrative medicine. The definition of INTEGRATED MEDICINE (IM) adopted here seems similar to the US definition we recently discussed. Here is the European definition:
Integrative medicine combines conventional medicine with evidence-informed complementary medicine and therapies to achieve the optimum health and wellbeing of the patient. Focusing on a holistic, patient-centred approach to healthcare, it takes into consideration the patient’s physical and psychological wellbeing and treats the whole person rather than just the disease.
Allow me to do a quick analysis of this definition by looking at its key elements:
- Evidence-informed: While proper medicine is BASED on evidence, IM is merely INFORMED by it. The difference is fundamental. It allows IM clinicians to use any un- or disproven so-called alternative medicine (SCAM) they can think of or invent. The evidence for homeopathy fails to show that it is effective? Never mind, IM does not need to be evidence-based, it is evidence-informed. IM physicians know homeopathy is a placebo therapy (if not they would be ill-informed which would make them unethical), but they nevertheless use homeopathy (try to find an IM clinic that does not offer homeopathy!), because IM is not EBM. IM is evidence-informed!
- Therapies that achieve optimum health and wellbeing. This is odd because the website also states that “therapies can include anything from acupuncture, yoga, massage, aromatherapy, herbal medicine, nutrition, exercise along with many more approaches, tailored to the needs of the individual” indicating that virtually anything can be included. Anyway, “optimum health and wellbeing” seems a strange and unachievable criterion. In fact, it is nothing but a ‘bait and switch‘ salesmen’s trick.
- Holistic: This is a little trick that IM proponents love. With it, they imply that normal medicine is not holistic. However, this implication is demonstrably wrong. Any good medicine is holistic, and if a sector of healthcare fails to account for the whole person, we need to reform it. (Here are the conclusions of an editorial I published in 2007 entitled ‘Holistic heath care?‘: good health care is likely to be holistic but holistic health care, as it is marketed at present, is not necessarily good. The term ‘holistic’ may even be a ‘red herring’ which misleads patients. What matters most is whether or not any given approach optimally benefits the patient. This goal is best achieved with effective and safe interventions administered humanely — regardless of what label we put on them.) Creating a branch of medicine that, like IM, pretends to have a monopoly on holism is grossly misleading and can only hinder this process.
- Patient-centred: This is the same mean little trick in a different guise. They imply that conventional medicine is not patient-centred. Yet, all good medicine is, of course, patient-centred. To imply otherwise is just daft.
- Consideration of the patient’s physical and psychological wellbeing and treating the whole person rather than just the disease: Same trick yet again! The implication is that physical and psychological wellbeing and the whole person are not all that relevant in conventional medicine where only disease labels are being treated.
Altogether, this definition of IM is unworthy of anyone with the slightest ability to think critically. I find it much worse than the latest US definition (which already is fairly awful). In fact, it turns out to be a poorly disguised bonanza of strawman fallacies combined with ‘bait and switch’ deception.
How can this be?
How can a professional organisation engage in such mean trickery?
Perhaps a look at the list of speakers will go some way towards answering the question. Have a good look, you might recognize many individuals as members of our ALTERNATIVE MEDICINE HALL OF FAME.
PS
Registration costs £ 249 (standard rate)
PPS
Perhaps I should also mention at least 4 of the many commercial sponsors of the conference:
- Boiron
- Helixor
- Iscador
- Weleda
Some used to think that Deepak Chopra is amongst the biggest charlatans on the planet. Well, they were wrong! And his new venture proves it beyond doubt.
The Lovetuner is a revolutionary approach to reduce stress, relieve anxiety and arrive in the present moment, connecting your exhale with the power of the 528hz frequency. That’s what the ad says, and Dr. Deepak Chopra agrees!
The website contains a short video which is a ‘MUST WATCH’. Please do have a look at it. Deepak will show you how to use the ‘LOVETUNER’. I promise you, it is impressive! In the video, Deepak also states that he is enthusiastic about the LOVETUNER and promises that:
- the LOVETUNER creates the frequency of love;
- the LOVETUNER can replace meditation;
- the LOVETUNER is inviting love into your life;
- the LOVETUNER increases your lung capacity;
- the LOVETUNER increases the coherence of your biofield;
- the LOVETUNER changes the biofield of the surroundings.
I am sure all these claims are based on the most solid of evidence. The fact that none of it has been published should not disturb us; on the contrary, it means that the evidence is so important that BIG PHARMA does not allow it to be published through the usual peer-reviewed channels – hence the video.
For those who are still not convinced, Deepak adds a written text:
“We want the world to be a more loving, peaceful, harmonious, happier and healthier place, right? First, we need to start with ourselves and be the change we want to see in this world. With the Lovetuner this is an easy and fun way to connect with ourselves and the world around us. The Lovetuner is more than just a meditation device – it is a mindset and a global peace and love movement. The Lovetuner teaches you the breath that spiritual gurus across the globe are going to recommend to you. It’s what you’ll find at your yoga retreat, sound bath, and guided meditation, but with the Lovetuner you can be your own guru.”
So, how does the LOVETUNER work? The website provides a most plausible explanation:
The Lovetuner is a revolutionary mindfulness tool that aligns you with the 528hz frequency, the vibration of love. In music, tuning means adjusting the pitch of a tone. In humans, it means adjusting your emotional and physical state to align with your environment – literally “tuning in” and harmonizing with yourself and what is around you. The Lovetuner has a profound effect on the body, mind and spirit.
Our entire universe is comprised of light and sound, frequency and vibration. The connections between music, cosmos and nature have been known since ancient times. In 1978 Hans Cousto, a Swiss mathematician and musicologist, compared the frequencies in planetary orbits, in architectural works, in old and modern measuring systems, in the human body, in music and in medicine and “discovered” their connection. John Lennon used the 528hz frequency for his song “Imagine.” In music, the 528Hz frequency refers to the note “Mi” and is traced back to the expression “Mi-ra gestorum” on the scale, which in Latin means “miracle”.
The 528hz frequency has a healing and health-promoting effect on our body, mind, and soul. Our cells and organs resonate with this frequency. The vibration is transferred to our entire organism where it can unfold its positive effect. It activates and strengthens our natural self-healing powers.
The 528hz frequency has a very special physical and biological importance.
The medical pioneer Dr. Royal Raymond Rife, who researched at the beginning of the 20th century, used many frequencies in his practice of radionics or electromagnetic therapy, but he specifically referred to 528 because of its ability to repair DNA. Dr. Rife used this frequency among hundreds of others for use with his Rife Machine – “Radionics.” He referred to 528 as “DNA repair.”
Molecular genetic investigations have shown that this frequency can be used to repair defective DNA strands or to restore human DNA to its original state. Scientific studies further showed that it increases the UV light absorption in DNA and can cure DNA by removing impurities that cause disease.
Today, the use of non-pharmacological and non-invasive agents is quite common. Sound waves, which are classified as non-invasive means for stimulating auditory cells, also affect non-auditory cells. Since the frequency of 528hz is related to the musical note Mi, effects such as an increase in the ability to repair DNA are observed.
I know, you are dying to know how much the LOVETUNER costs. For just $ 62, it can be yours! I do think that this is a bargain and am deeply thankful to Deepak for alerting me to this life-changing device. Yes, some used to think that Deepak Chopra is amongst the biggest charlatans on the planet. I am sure that his support for the LOVETUNER will make these people change their minds.
While working on yesterday’s post, I discovered another recent and remarkable article co-authored by Prof Harald Walach. It would surely be unforgivable not to show you the abstract: 
The aim of this study is to explore experiences and perceived effects of the Rosary on issues around health and well-being, as well as on spirituality and religiosity. A qualitative study was conducted interviewing ten Roman Catholic German adults who regularly practiced the Rosary prayer. As a result of using a tangible prayer cord and from the rhythmic repetition of prayers, the participants described experiencing stability, peace and a contemplative connection with the Divine, with Mary as a guide and mediator before God. Praying the Rosary was described as helpful in coping with critical life events and in fostering an attitude of acceptance, humbleness and devotion.
The article impressed me so much that it prompted me to design a virtual study for which I borrowed Walach’s abstract. Here it is:
The aim of this study is to explore experiences and perceived effects of train-spotting on issues around health and well-being, as well as on spirituality. A qualitative study was conducted interviewing ten British adults who regularly practiced the art of train-spotting. As a result of using a tangible train-spotter diary and from the rhythmic repetition of the passing trains, the participants described experiencing stability, peace, and a contemplative connection with the Divine, with Mary as a guide and mediator before the almighty train-spotter in the sky. Train-spotting was described as helpful in coping with critical life events and in fostering an attitude of acceptance, humbleness, and devotion.
These virtual results are encouraging and encourage me to propose the hypothesis that Rosary use and train-spotting might be combined to create a new wellness program generating a maximum holistic effect. We are grateful to Walach et al for the inspiration and are currently applying for research funds to test our hypothesis in a controlled clinical trial.
The integration of so-called alternative medicine (SCAM) into cancer care may reduce the adverse effects of anti-neoplastic treatment but also cause new problems and non-adherence to conventional treatment. Therefore, its net benefit is questionable.
The aim of this randomized controlled study was to investigate the impact of integrative open dialogue about SCAM on cancer patients’ health and quality of life (QoL).
Patients undergoing curative or palliative anti-neoplastic treatment were randomly assigned to standard care (SC) plus SCAM or SC alone. A nurse specialist facilitated SCAM in one or two sessions. The primary endpoint was the
frequency of grade 3–4 adverse events (AE) eight weeks after enrollment. Secondary endpoints were the frequency of grade 1–4 AE and patient-reported QoL, psychological distress, perceived information, attitude towards and use of SCAM 12 and 24 weeks after enrollment. Survival was analyzed post-hoc.
Fifty-seven patients were randomized to SCAM and 55 to SC. No significant differences were found in terms of AEs of cancer patients. A trend towards better QoL, improved survival, and a lower level of anxiety was found in the SCAM group.
The authors concluded that integration of SCAM into daily oncology care is feasible. IOD-CAM was not superior to SC in reducing the frequency of grade 3-4 AEs, but it did not compromise patient safety. Implementation of SCAM
may improve the QoL, anxiety, and emotional well-being of the patients by reducing the level of nausea, vomiting and diarrhea. Finally, SCAM potentially improves the patients’ self-care, which contributes to
increased treatment adherence and improved survival.
This is an interesting paper with a very odd conclusion. The positive trends found failed to be statistically significant. Why employ statistics only to ignore them in our interpretation of the findings?
I can well imagine that the integration of effective treatments into cancer care improves the outcome. I have no problem with this at all – except it is not called INTEGRATIVE MEDICINE but EVIDENCE-BASED MEDICINE!!! If we integrate dubious treatments into cancer care, it’s called INTEGRATIVE MEDICINE, and it’s unlikely to do any good.
In my view, this small study showed just one thing:
Integrative medicine does not reduce adverse effects in cancer patients.
Prince Charles has claimed that people struggling to return to full health after having the coronavirus should practice yoga. This is what the GUARDIAN reported about it on Friday:
In a video statement on Friday to the virtual yoga and healthcare symposium Wellness After Covid, the heir apparent said doctors should work together with “complementary healthcare specialists” to “build a roadmap to hope and healing” after Covid. “This pandemic has emphasised the importance of preparedness, resilience and the need for an approach which addresses the health and welfare of the whole person as part of society, and which does not merely focus on the symptoms alone,” Charles said. “As part of that approach, therapeutic, evidenced-informed yoga can contribute to health and healing. By its very nature, yoga is an accessible practice which provides practitioners with ways to manage stress, build resilience and promote healing…”
… Charles, who has previously espoused the benefits of yoga, is not the only fan in the royal family. His wife, the Duchess of Cornwall, has said “it makes you less stiff” and “more supple”, while Prince William has also been pictured doing yogic poses. In 2019, the Prince of Wales said yoga had “proven beneficial effects on both body and mind”, and delivered “tremendous social benefits” that help build “discipline, self-reliance and self-care”.
__________________
END OF QUOTE
Yoga is a complex subject because it entails a host of different techniques, attitudes, and life-styles. There have been numerous clinical trials of various yoga techniques. They tend to suffer from poor study design as well as incomplete reporting and are thus no always reliable. Several systematic reviews have summarised the findings of these studies. A 2010 overview included 21 systematic reviews relating to a wide range of conditions. Nine systematic reviews arrived at positive conclusions, but many were associated with a high risk of bias. Unanimously positive evidence emerged only for depression and cardiovascular risk reduction.[1] There is no evidence that yoga speeds the recovery after COVID-19 or any other severe infectious disease, as Charles suggested.
Yoga is generally considered to be safe. However, a large-scale survey found that approximately 30% of yoga class attendees had experienced some type of adverse event. Although the majority had mild symptoms, the survey results indicated that patients with chronic diseases were more likely to experience adverse events.[2] It, therefore, seems unlikely that yoga is suited for many patients recovering from a COVID-19 infection.
The warning by the Vatican’s chief exorcist that yoga leads to ‘demonic possession’[3] might not be taken seriously by rational thinkers. Yet, experts have long warned that many yoga teachers try to recruit their clients into the more cult-like aspects of yoga.[4]
Perhaps the most remarkable expression in Charles’ quotes is the term ‘EVIDENCE-INFORMED‘. It crops up regularly when Charles (or his advisor Dr. Michael Dixon) speaks or writes about so-called alternative medicine (SCAM). It is a clever term that sounds almost like ‘evidence-based’ but means something entirely different. If a SCAM is not evidence-based, it can still be legitimately put under the umbrella of ‘evidence-informed’: we know the evidence is not positive, we were well-informed of this fact, we nevertheless conclude that yoga (or any other SCAM) might be a good idea!
In my view, the regular use of the term ‘evidence-informed’ in the realm of SCAM discloses a lack of clarity that suits all snake-oil salesmen very well.
[1] Ernst E, Lee MS: Focus on Alternative and Complementary Therapies Volume 15(4) December 2010 274–27
[2] Matsushita T, Oka T. A large-scale survey of adverse events experienced in yoga classes. Biopsychosoc Med. 2015 Mar 18;9:9. doi: 10.1186/s13030-015-0037-1. PMID: 25844090; PMCID: PMC4384376.
[3] https://www.social-consciousness.com/2017/06/vaticans-chief-exorcist-warns-that-yoga-causes-demonic-possession.html
[4] https://www.theguardian.com/lifeandstyle/2020/jun/26/experience-my-yoga-class-turned-out-to-be-a-cult
After yesterday’s post entitled ‘What does a holistic doctor do that a traditional doctor doesn’t?‘, I thought it would only be fair to turn the question around and ask: What does a proper doctor do that a holistic healer doesn’t? The answers will upset a lot of practitioners of alternative medicine (SCAM), but so be it.
So, what does a proper doctor do that a holistic healer doesn’t?
I suggest several answers and hope that the readers of this blog will contribute to further points. Many of them center around safeguarding the public:
- Proper doctors avoid confusing or misleading the public with titles they do not have.
- They do have rigorous education and training.
- They avoid making false therapeutic claims.
- They adhere to the ethical standards of their profession.
- They resist the temptation to advertise their services to the consumer.
- They do their best to identify the cause of their patient’s symptoms.
- They treat the causes of disease whenever possible.
- They avoid pretending that they always have all the answers.
- They abide by the rules of evidence-based medicine.
- They are aware that almost any effective treatment comes with adverse effects.
- They try to keep abreast with the rapid advances in medicine.
- They know that a patient is more than a diagnostic label.
- They try to treat patients holistically.
At this stage, I can hear some readers shout in anger:
- Ahh, but that is rubbish!
- I know doctors who are not at all like that!
- You are idealizing your profession!
- This is little more than wishful thinking!
Yes, I know that many patients are disappointed and have had a bad experience with conventional medicine. That is one of the reasons many try SCAM. I know that many doctors occasionally fail to live up to the ideal that I depicted above. And I fear that some do so more often than just occasionally.
This is regrettable and occasionally it is unacceptable. Medicine is populated not by perfect people; it is run by humans like you and me. Humans are fallible. Doctors have bad days just like you and me. If that happens regularly, we need to address the problems that may the cause of the deficit. If necessary, the case has to go before a disciplinary hearing. There are thousands of experts who are dedicated to improving healthcare in the hope of generating progress.
The point I was trying to make is that there is such a thing as an ideal physician. It relies on:
- rigorous training,
- ethical codes,
- post-graduate education,
- supervision,
- governance,
- swift disciplinary procedures,
- advances brought about through colossal research efforts,
- etc., etc.
Do ‘holistic healers’ offer all of these safeguards?
The sad answer is no.
For those who disagree, let’s briefly look at a recent example.
John Lawler died in 2017 after being treated by a chiropractor (as discussed on this blog before).
- Mr. Lawler died because of a tear and dislocation of the C4/C5 intervertebral disc caused by a considerable external force.
- The pathologist’s report also showed that the deceased’s ligaments holding the vertebrae of the upper spine in place were ossified.
- This is a common abnormality in elderly patients and limits the range of movement of the neck.
- There was no adequately informed consent by Mr. Lawler.
- Mr. Lawler seemed to have been under the impression that the chiropractor, who used the ‘Dr’ title, was a medical doctor.
- There is no reason to assume that the treatment of Mr. Lawler’s neck would be effective for his pain located in his leg.
- The chiropractor used an ‘activator’ that applies only little and well-controlled force. However, she also employed a ‘drop table’ which applies a larger and not well-controlled force.
As far as I can see, most of the safeguards and standards that apply to conventional medicine were not in place to safeguard Mr. Lawler. And that includes a timely disciplinary hearing of the case. Mr. Lawler died in 2017! The CCG has been dragging its feet ever since, and, as far as I know, the chiropractor was meanwhile allowed to practise. The HEARING BEFORE THE PROFESSIONAL CONDUCT COMMITTEE OF THE GENERAL CHIROPRACTIC COUNCIL has now been scheduled to commence on 19 April 2021.
I know, it’s just an example. But it should make us think.
Holistic medicine is based on several core values:
- good health is a combination of physical, emotional, mental, spiritual, and social wellness
- prevention first, treatment second
- disease is caused by a problem with the whole body, rather than a single event or body part
- the goal of treatment is to fix the underlying cause of disease, instead of just improving the symptoms
- treatment involves a wide range of options, including education, self-care, CAM, and traditional medicine
- a person is not defined by their condition
- the relationship between a doctor and the person being treated determines the treatment outcome
Generally, traditional doctors treat symptoms. They provide medical solutions to alleviate a disease.
A holistic doctor treats the body as one. They aim to find the cause behind the disease, instead of just fixing the symptoms. This could require multiple therapies.
For example, if you have eczema, a medical doctor may give you a prescription cream. But a holistic doctor may suggest dietary and lifestyle changes. The holistic doctor might also recommend using the cream, plus natural home remedies like oatmeal baths.
So, now we know!
This could, of course, be just laughable if it were not perpetuating such common misconceptions. And as this sort of BS is so common, I feel obliged to carry on exposing it. Let me, therefore, correct the main errors in the short paragraph:
- ‘Traditional doctors’ are just doctors, proper doctors; holistic healers often give themselves the title ‘doctor’ but, unless they have been to medical school, they are not doctors.
- ‘Doctors treat symptoms’; yes, they do. But whenever possible, they treat the cause too. Therefore they do what is possible to identify the cause. And during the last 150 years or so, they have become reasonably good at this task.
- ‘A holistic doctor treats the body as one.’ That’s what they claim. But in reality, they are often not trained to do so. The body is mighty complex, and many holistic practitioners are simply not trained for coping with this complexity.
- ‘They aim to find the cause behind the disease’. They might well aim at that, but if they are not fully trained doctors, this is an impossible aim, and they merely end up finding what they have been taught about the cause of disease. An imbalance of Yin and Yang is the imagined cause of disease in TCM, and for many chiropractors, a subluxation is the cause of disease. But such assumptions are not facts; it is merely wishful thinking which get in the way of finding true causes of disease.
- Eczema happens to be a superb example (thank you ‘helpline’). The oatmeal bath of the holistic practitioner is at best a symptomatic treatment. This is why a proper doctor aims to find the cause of eczema which could be an allergy, for instance. Having identified it, the doctor would then advise how to avoid the allergen. If that is possible, further treatment might not be even necessary.
When practitioners are elaborating on their concept of holism, one often only needs to read on to find that those who pride themselves on holism are, in fact, the victims of multiple errors (or perhaps they use the holism gimmick only as a sales strategy, because consumers fall easily for this ‘bait and switch’). And those doctors who are accused of lacking holism are, in fact, more likely to be holistic than the so-called holists.


