holistic
For some time now, I have been using the umbrella term ‘so-called alternative medicine’ (SCAM). As I explain below, I think it is relatively well-suited. But this is not to say that it is the only name for it. Many other umbrella terms have been used in the past.
Is there perhaps one that you prefer?
- Fringe medicine is rarely used today. It denotes the fact that the treatments under this umbrella are not in the mainstream of healthcare. Some advocates seem to find the word derogatory, and therefore it is now all but abandoned.
- Unorthodox medicine is a fairly neutral term describing the fact that medical orthodoxy tends to shun most of the treatments in question. Strictly speaking, the word is also incorrect; the correct term would be ‘heterodox medicine’.
- Unconventional is also a neutral term but it is open to misunderstandings: any new innovation in medicine might initially be called unconventional. It is therefore less than ideal.
- Traditional medicine describes the fact that most of the modalities in question have been around for centuries and thus have a long tradition of usage. However, as the term is sometimes also used for conventional medicine, it is confusing and far from ideal.
- Alternative medicine is the term everyone seems to know and which is most commonly employed in non-scientific contexts. In the late 1980s, some experts pointed out that the word could give the wrong impression: most of the treatments in question are not used as a replacement but as an adjunct to conventional medicine.
- Complementary medicine became subsequently popular based on the above consideration. It accounts for the fact that the treatments tend to be used by patients in parallel with conventional medicine.
- Complementary and alternative medicine (CAM) describes the phenomenon that many of the treatments can be employed either as a replacement of or as an adjunct to conventional medicine.
- Holistic medicine denotes the fact that practitioners often pride themselves to look after the whole patient – body, mind, and spirit. This could lead to the erroneous impression that conventional clinicians do not aim to practice holistically. As I have tried to explain repeatedly, any good healthcare always has been holistic. Therefore, the term is misleading, in my view.
- Natural medicine describes the notion that many of the methods in question are natural. The term seems attractive and is therefore good for business. However, any critical analysis will show that many of the treatments in question are not truly natural. Therefore this term too is misleading.
- Integrated medicine is currently popular and much used by Prince Charles and other enthusiasts. As we have discussed repeatedly on this blog, the term is nevertheless highly problematic.
- Integrative medicine is the word used in the US for integrated medicine.
- CAIM (complementary/alternative/integrative medicine) is a term that some US authors recently invented. I find this attempt to catch all the various terms in one just silly.
- So-called alternative medicine (SCAM) is the term I tend to use. It accounts for two important facts: 1) if a treatment does not work, it cannot possibly serve as an adequate alternative; 2) if a therapy does work, it should be part of conventional medicine. Thus, there cannot be an ‘alternative medicine’, as much as there cannot be an alternative chemistry or an alternative physics.
Yet,some advocates find ‘SCAM’ derogatory. Intriguingly, my decision to use this term was inspired by Prince Charles, arguably the world’s greatest champion of this sector of healthcare. In his book ‘HARMONY’, he repeatedly speaks of ‘so-called alternative treatments’.
You don’t believe me?
Fair enough!
In this case – and in order to save you the expense of buying Charles’ book for checking – let me provide you with a direct quote: “Some so-called alternative treatments seek to work with these functions to aid recovery…” (page 225).
And who would argue that Charles is dismissive about alternative medicine?
Osteopathy is hugely popular in France. Despite the fact that osteopathy has never been conclusively shown to generate more good than harm, French osteopaths have somehow managed to get a reputation as trustworthy, evidence-based healthcare practitioners. They tend to treat musculoskeletal and many other issues. Visceral manipulation is oddly popular amongst French osteopaths. Now the trust of the French in osteopathy seems to have received a serious setback.
‘LE PARISIEN‘ has just published an article about the alleged sexual misconduct of one of the most prominent French osteopaths and director of one of the foremost schools of osteopathy in France. Here are some excerpts from the article that I translated for readers who don’t speak French:
The public prosecutor’s office of Grasse (Alpes-Maritimes) has opened a judicial investigation against Marc Bozzetto, the director and founder of the school of osteopathy in Valbonne, accused of rape and sexual assault.
In total, “four victims are targeted by the introductory indictment,” said the prosecutor’s office, stating that Marc Bozzetto had already been placed in police custody since the beginning of the proceedings. The daily paper ‘Nice-Matin’ has listed six complaints and published the testimony of a seventh alleged victim.
This victim claims to have been sexually assaulted in 2013, alleging that, during a professional appointment, Bozzetto had massaged her breasts and her intimate area. “He told me that everything went through my vagina and clitoris, that I had to spread my legs and let the energy flow through my clitoris. That I had to learn how to give myself pleasure on my own,” she told Nice-Matin. The newspaper also recorded the testimonies of a former employee, a top-level sportswoman, an employee from the world of culture, and a former student.
“I take note that a judicial inquiry is open. To date, he has neither been summoned nor indicted,” said Karine Benadava, the Parisian lawyer of the 80-year-old Bozzetto. Her client had already responded following initial accusations from students: “This is a normal feeling for women, but if all the women who work on the pelvis complain, you can’t get away with it and you have to stop working as a pelvic osteopath,” replied Bozzetto. In another interview, he had declared himself “furious” and unable to understand the reaction of these two students.
The school of osteopathy trains about 300 students each five years and presents itself as the first holistic osteopathy campus in France.
______________________________
Such stories of sexual misconduct of practitioners of so-called alternative medicine (SCAM) are sadly no rarety, particularly those working in the area of manual therapy. They remind me of a case against a Devon SCAM practitioner in which I served as an expert witness many years ago. Numerous women gave witness that he ended up having his fingers in their vagina during therapy. He did not deny the fact but tried to defend himself by claiming that he was merely massaging lymph-nodes in this area. It was my task to elaborate on the plausibility of this claim. The SCAM practitioner in question was eventually sentenced to two years in prison.
It stands to reason that SCAM practitioners working in the pelvic area are at particularly high risk of going atray. The above case might be a good occasion to have a public debate in France and ask: IS VISCERAL OSTEOPATHY EVIDENCE-BASED? The answer is very clearly NO! Surely, this is a message worth noting in view of the current popularity of this ridiculous, costly, and dangerous charlatanry.
And how does one minimize the risk of sexual misconduct of SCAM professionals? The most obvious answer would be, by proper education during their training. In the case mentioned above, this might have been a problem: if the director is into sexual misconduct, what can you expect of the rest of the school? In many other cases, the problem is even greater: many SCAM practitioners have had no training at all, or no training in healthcare ethics to speak of.
I was alerted to an article in which some US doctors, including the famous Andrew Weil, promote the idea that so-called alternative medicine (SCAM) has a lot to offer for people recovering from Covid-19 infections. There would be a lot to argue about their recommendations, but today I will not go into this (I find it just too predictable how SCAM proponents try to promote SCAM on the basis of flimsy evidence; perhaps I am suffering from ‘BS for Covid fatigue’?). What did, however, strike me in their paper was a definition of INTEGRATIVE MEDICINE (IM) that I had not yet come across:
Integrative medicine is defined as healing-oriented medicine that takes account of the whole person, including all aspects of lifestyle. It emphasizes the therapeutic relationship between practitioner and patient, is informed by evidence, and makes use of all appropriate therapies.
Ever since the term IM became fashionable, there have been dozens of definitions of the term (almost as though IM proponents were not quite sure themselves what they were promoting). And ever since I first heard about IM, I felt it was a thinly disguised attempt to smuggle unproven treatments into the routine of evidence-based medicine (EBM). In 2002, I published my 1st comment on the subject. In it, I warned that IM must not become an excuse for using every conceivable untested treatment under the banner of holism. Nineteen years on, this is exactly what has happened, and one definition of IM after the next is soaked in platitudes, falsehoods and misunderstandings.
So, let’s see how reasonable this new definition is. I will try to do this by briefly discussing each element of the two sentences.
- IM is healing-oriented medicine: this is a transparently daft platitude. Does anyone know a medicine that is not oriented towards healing? Healing is the process of becoming well again, especially after a cut or other injury, or of making someone well again. Healing is what medicine has always been and always be aimed at. In other words, it is not something that differentiates IM from other forms of healthcare.
- IM takes account of the whole person: This is the little holistic trick that IM proponents like to adopt. It implies that normal medicine or EBM is not holistic. This implication is wrong. Any good medicine is holistic, and if a sector of healthcare fails to account for the whole person, we need to reform it. (Here are the conclusions of an editorial I published in 2007 entitled ‘Holistic heath care?‘: good health care is likely to be holistic but holistic health care, as it is marketed at present, is not necessarily good. The term ‘holistic’ may even be a ‘red herring’ which misleads patients. What matters most is whether or not any given approach optimally benefits the patient. This goal is best achieved with effective and safe interventions administered humanely — regardless of what label we put on them.) Creating a branch of medicine that, like IM, pretends to have a monopoly on holism can only hinder this process.
- IM includes all aspects of lifestyle: really, all of them? This is nonsense! Good physicians take into account the RELEVANT lifestyles of their patients. If, for instance, my patient with intermittent claudication is a postman, his condition would affect him differently from a patient who is a secretary. But all lifestyles? No! I fear this ‘over the top’ statement merely indicates that those who have conceived it have difficulties differentiating the important from the trivial.
- IM emphasizes the therapeutic relationship: that’s nice! But so do all other physicians (except perhaps pathologists). As medical students, we were taught how to do it, some physicians wrote books about it (remember Balint?), and many of us ran courses on the subject. Some conventional clinicians might even feel insulted by the implication that they do not emphasize the therapeutic relationship. Again, the IM brigade take an essential element of good healthcare as their monopoly. It almost seems to be a nasty habit of theirs to highjack a core element of healthcare and declare it as their invention.
- IM is informed by evidence: that is brilliant, finally there emerges a real difference between IM and EBM! While proper medicine is BASED on evidence, IM is merely INFORMED by it. The difference is fundamental, because it allows IM clinicians to use any un- or disproven SCAM. The evidence for homeopathy fails to show that it is effective? Never mind, IM is not evidence-based, it is evidence-informed. IM physiciance know homeopathy is a placebo therapy (if not they would be ill-informed which would make them unethical), but they nevertheless use homeopathy (try to find an IM clinic that does not offer homeopathy!), because IM is not EBM. IM is evidence-informed!
- IM makes use of all appropriate therapies: and the last point takes the biscuit. Are the IM fanatics honestly suggesting that conventional doctors use inappropriate therapies? Does anyone know a branch of health care where clinicians systematically employ therapies that are not appropriate? Appropriate means suitable or right for a particular situation or occasion. Are IM practitioners the only ones who use therapies that are suitable for a particular situation? This last point really does count on anyone falling for IM not to have the slightest ability to think analytically.
This short analysis confirms yet again that IM is little more than a smokescreen behind which IM advocates try to smuggle nonsense into routine healthcare. The fact that, during the last two decades, the definition constantly changed, while no half decent definition emerged suggests that they themselves don’t quite know what it is. They like moving the goal post but seem unsure in which direction. And their latest attempt to define IM indicates to me that IM advocates might not be the brightest buttons in the drawer.
I often hear that my ambitions to inform the public and inspire critical thinking are hopeless: there are simply too many quacks trumpeting nonsense, and their collective influence is surely bigger than mine. This can be depressing, of course. And because I often feel that I am fighting an unwinnable battle, stories like this are so importand and up-lifting.
Denby Royal was a ‘holistic nutritionist’, then she became a critic of so-called alternative medicine (SCAM). Here is the story about her transformation:
… I had gone to holistic nutrition school. I was running my own nutrition consulting business. And suddenly I didn’t believe in any of it anymore. How did this flip flop come to pass?
… As a holistic nutritionist, I was an active participant in what I now consider alternative medicine tomfoolery, specifically pushing supplements on a clientele of the “worried well” who often mistook wellness enthusiasts like me for medical experts. I want to be clear that I wasn’t knowingly deceiving anyone—I really did believe in the solutions I was offering my clients… To holistic nutrition enthusiasts and people who believe in a certain kind of alt wellness, these “natural” and “holistic” products seem more trustworthy than what mainstream medicine offers. The truth is, they often lack sufficient, peer-reviewed, reliable scientific evidence of their supposed effectiveness.
Did I have rock-solid evidence that these products would do what their labels promised they would do? Not really. Sure, I read studies here and there that found specific health benefits for some of the products. But I rarely mentioned the fine print (if I knew it at all)—that the sample sizes of many of these studies often were so small that the results couldn’t be generalized to a larger population, that the studies’ authors sometimes noted that more research was needed to support any findings on the effects they found, or that systematic reviews later found that many studies were poorly constructed or at risk for bias, making their findings even less compelling than they seemed initially. And in some cases, study authors themselves note that their findings are merely jumping off points, and that more long-term studies are needed in order to draw more solid conclusions…
Was I relying on strong, valid evidence? Nah, not really. But at the time, I thought what I had was better than strong evidence: Faith in a lifestyle and a dogmatic belief that all things traditional and mainstream were unhealthy or harmful, and therefore, that all things unconventional and alternative were curative and would bring about “wellness.”
In an effort to expand my product knowledge I researched a lot of the different supplements available. I was using all the best bias-confirming websites where other homeopathic medicine enthusiasts evangelized their favorite remedies, their enthusiasm and insistence, and anecdotal evidence standing in for what typically shows us that a product is safe and effective—clinical trials and FDA approval.
When their arguments and reasoning started to sink in, I realized that my faith in the healing powers of supplements may have been overzealous at best, unfounded at worst. My world crumbled like a piece of raw gluten-free paleo cheesecake. It started to sink in: Where there was a morsel of convincing medical information blended with enough compelling nonsense and communicated with enough conviction, I believed it, hook, line, and sinker.
When I started to notice the holes in the fabric of holistic nutrition, the fabric looked, well, pretty threadbare. I subsequently disconnected from social media and distanced myself from the entire culture. I took a good look at how I was personally and publicly communicating my relationships with food and wellness. After spending my twenties experimenting with all kinds of specialty diets, I was left feeling exhausted, anxious, underweight, overweight, and fed-up.
And so that last domino fell when I took away the thing that was propping it up for me: social media. Instagram is a playground for wellness influencers, including, at the time, me. My Instagram account was the best way to advertise my nutrition consulting business, so maintaining a certain persona there felt completely crucial to my success, and eventually, my identity. It was a world full of beautifully curated accounts of thin yogis gathering wild herbs in nature or making raw desserts with ingredients that cost more than my entire monthly food budget. I started to feel like the alternative wellness community I was part of—myself included—was an echo chamber, where we stockpiled likes and positive comments to build a wall that would keep out ideas that challenged our status quo. In fact, the more reassurance I received from my online community, the harder I believed in our gospel.
As I was disentangling my beliefs from everything I was learning by looking at the actual evidence, I realized that my education to become a holistic nutritionist hadn’t prepared me to understand health and wellness as completely and comprehensively as I’d once thought. Sure, I’d spent a some time studying the pathology of disease, and a little longer learning about how each bodily system works to get your human suit from point A to point B, but I am only slightly closer to being a medical professional than I am to becoming a professional cricket player. First of all, in total, my entire formal education as a holistic nutritionist was 10 months long. Second of all, that education was intended to complement—not replace—traditional medical treatment. But as soon as I finished the program, I could immediately start taking on clients. And lots of potential clients out there are just like the way I used to be—wishing they looked or felt different and in search of the panacea, willing (if not eager) to defer to an expert.
There may have been many people willing to look to me as an expert, but here’s the thing: in my school, there were no residency or clinical hours required to prepare us for the real world or to take on clients—unlike dietitians here in Canada, who must obtain a bachelor’s degree in Nutritional and Food Sciences, qualify to complete a rigorous post-degree internship program and register with a provincial dietetics organization, or get a master’s degree. We received a certificate, and that was that. It was a credential that wholeheartedly fell short of resembling anything close to making me an authority on the subject of health as it relates to food and diet. But most people in the general public can’t be expected to understand the ins and outs of how experts are credentialed and licensed—many of us assume that someone calling themselves something that we associate with authority is, in fact, an authority we can trust.
The brief education that I received to become a holistic nutritionist did provide me with valuable stepping stones and a general understanding of how the body works. My program discouraged students from saying “treat,” “heal,” “prevent,” or “cure.” Generally speaking holistic nutrition programs don’t provide the training and medical education that registered dietitians receive, which enables them to give sound, ethical medical nutrition advice, nor are they required by law, the way dietitian programs are, to provide it. In fact, in 2015 graduates of the Canadian School of Natural Nutrition were barred from identifying as Registered Holistic Nutritionists, and since then must use the title “Holistic Nutritional Consultant.”
… With what I do have from my classroom education, I can analyze a lifestyle that needs some fine-tuning and provide guidance on how to structure a solid meal plan. That’s about it. After years of self-diagnosis and hashtagging all my fad-diet escapades (for this, I greatly apologize to all those I have alienated with my profuse self-righteousness), I can at least say I have a deep appreciation for those who are actually on the front lines in the fight against unproven medical remedies and the potential damage it may do to those who use it to the exclusion of traditional medicine.
The influence of these remedies is not harmless, and I have seen firsthand in many different examples and situations how it can lure people away from real, evidence-based help in their times of need. I am fortunate enough that within my practice I had enough foresight to turn away individuals who required more guidance than I was capable of giving. But along the way I made many embarrassing and conjectural recommendations. Like I said, I was far from knowingly deceiving anyone. I firmly held the belief that alternative medicine, no matter the cost, was an investment in a healthful future. My own medicine cabinet, an arsenal full of supplements, tincture, and powders, was a personal testament to how deeply I was devoted to holistic nutrition.
This essay is a firm farewell from a world I disconnected from long ago. The person that over years I let myself become through naiveté, not doing my own research, and a misguided desire to be different. So here I am now, officially having left the church of woo, bidding the world of alternative health adieu.
_________________________________
Reading Denby’s account, I was reminded of many themes we have previously discussed on this blog. One issue that perhaps needs more focus is this notion:
“I was far from knowingly deceiving anyone.”
I have not yet met a SCAM practitioner who says:
“I am in the business of deceiving my patients.”
The reasons for this are simple:
- if they knowingly deceive, they would not tell us,
- and if they don’t know that they are deciving their patients, they cannot possibly admit to it.
The way Denby repeatedly assures us that she was far from knowingly deceiving anyone sounds charmingly naive and is, in my experience, very typical for SCAM practitioners. It depicts them as honorable people. Yet, in actual fact, it is neither charming nor honorable. It merely demonstrates the fact that they were perhaps not ruthlessly dishonest but all the more dangerous.
Let me explain this with a deliberately extreme example:
- A man with a chronic condition – say type 2 diabetes – consults a SCAM practitioner who is knowingly deceiving him claiming that her SCAM effectively treats his condition. The patient follows the advice but, since he is not totally convinced (deception is rarely perfect), consults his doctor who puts him straight. This patient will therefore survive.
- The same chap consults a SCAM practitioner who is deeply convinced of the effectiveness of her SCAM and thus not knowingly deceiving her patient when she claims that it is effective for his diabetes. Her conviction is so strong that the patient blindly believes her. Thus he stops his conventional medication and hopes for the best. This patient could easily die.
In a nutshell:
‘Honest’ conviction might render a quack more socially acceptable but also more dangerous to her patients.
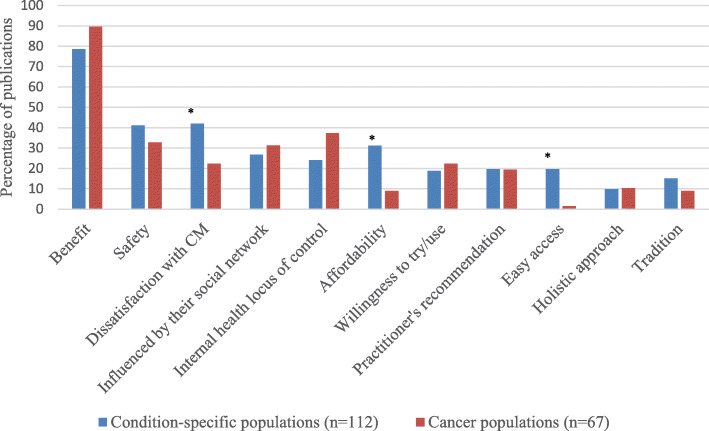
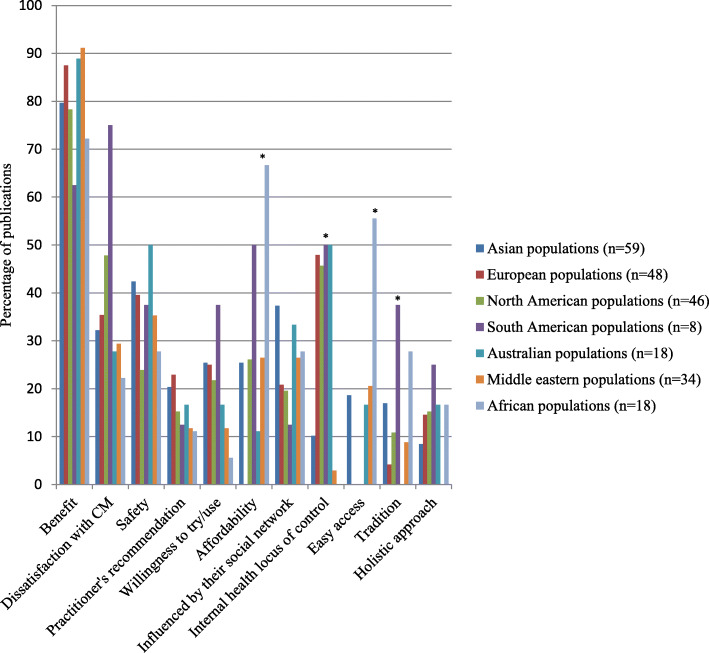
The authors of this review wanted to determine similarities and differences in the reasons for using or not using so-called alternative medicine (SCAM) amongst general and condition-specific populations, and amongst populations in each region of the globe.
Quantitative or qualitative original articles in English, published between 2003 and 2018 were reviewed. Conference proceedings, pilot studies, protocols, letters, and reviews were excluded. Papers were appraised using valid tools and a ‘risk of bias’ assessment was also performed. Thematic analysis was conducted. Reasons were coded in each paper, then codes were grouped into categories. If several categories reported similar reasons, these were combined into a theme. Themes were then analysed using χ2 tests to identify the main factors related to reasons for CAM usage.
A total of 231 publications were included. Reasons for SCAM use amongst general and condition-specific populations were similar. The top three reasons were:
- (1) having an expectation of benefits of SCAM (84% of publications),
- (2) dissatisfaction with conventional medicine (37%),
- (3) the perceived safety of SCAM (37%).
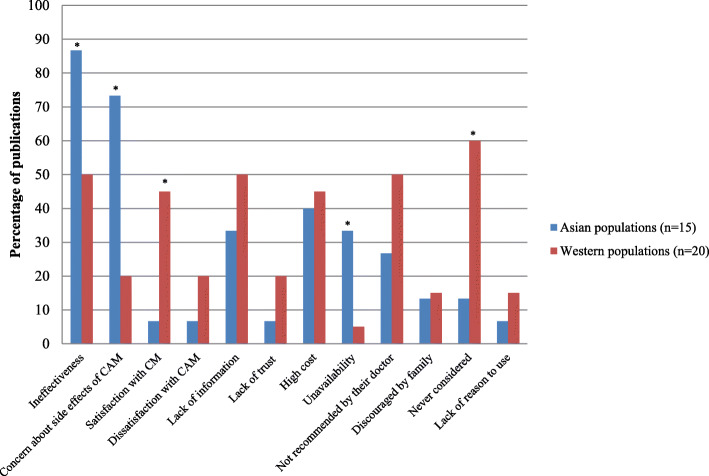
Internal health locus of control as an influencing factor was more likely to be reported in Western populations, whereas the social networks was a common factor amongst Asian populations (p < 0.05). Affordability, easy access to SCAM and tradition were significant factors amongst African populations (p < 0.05). Negative attitudes towards SCAM and satisfaction with conventional medicine were the main reasons for non-use (p < 0.05).
The authors concluded that dissatisfaction with conventional medicine and positive attitudes toward SCAM, motivate people to use SCAM. In contrast, satisfaction with conventional medicine and negative attitudes towards SCAM are the main reasons for non-use.
At this point, I thought: so what? This is all very obvious and does not necessitate an extensive review of the published literature. What it actually shows is that the realm of SCAM is obsessed with conducting largely useless surveys, a phenomenon, I once called ‘survey mania‘. But a closer look at the review does reveal some potentially interesting findings.
In less developed parts of the world, like Africa, SCAM use seems to be determined by affordability, accessibility and tradition. This makes sense and ties in with my impression that consumers in such countries would give up SCAM as soon as they can afford proper medicine.
This notion seems to be further supported by the reasons for not using SCAM. Asian consumers claim overwhelmingly that this is because they consider SCAM ineffective and unsafe.
In our review of 2011 (not cited in the new review), we looked at some of the issues from a slightly different angle and evaluated the expectations of SCAM users. Seventy-three articles met our inclusion criteria of our review. A wide range of expectations emerged. In order of prevalence, they included:
- the hope to influence the natural history of the disease;
- the desire to prevent disease and promote health/general well-being;
- the hope of fewer side effects;
- the wish to be in control over one’s health;
- the hope for symptom relief;
- the ambition to boost the immune system;
- the hope to receive emotional support;
- the wish to receive holistic care;
- the hope to improve quality of life;
- the expectation to relief of side effects of conventional medicine;
- the desire for a good therapeutic relationship;
- the hope to obtain information;
- the hope of coping better with illness;
- the expectation of supporting the natural healing process;
- the availability of SCAM.
All of these aspects, issues and notions might be interesting, even fascinating to some, but we should not forget three important caveats:
- Firstly, SCAM is such a diverse area that any of the above generalisations are highly problematic; the reasons and expectations of someone trying acupuncture may be entirely different from those of someone using homeopathy, for instance.
- Secondly (and more importantly), the ‘survey mania’ of SCAM researchers has not generated the most reliable data; in fact, most of the papers are hardly worth the paper they were printed on.
- Thirdly (and even more importantly, in my view), why should any of this matter? We have known about some of these issues for at least 3 decades. Has this line of research changed anything? Has it prevented consumers getting exploited by scrupulous SCAM entrepreneurs? Has it made consumers, politicians or anyone else more aware of the risks associated with SCAM? Has it saved many lives? I doubt it!
If you think that the papers published on SCAM for humans are bad, you should have a look at those in the veterinary sector. Take for instance this article from the AHVMA (American Holistic Veterinary Medical Association) Journal:
Evidence demonstrates that acupuncture and herbal medicine are useful and effective for the treatment of seizures. In the perspective of Traditional Chinese Veterinary Medicine (TCVM), seizures in dogs and cats can be classified into 6 patterns:
- Obstruction by WindPhlegm,
- Internal Profusion of Phlegm-Fire,
- Stagnation of Blood,
- Liver Blood Deficiency,
- Liver/Kidney Yin Deficiency,
- Yin Deficiency with Blood Deficiency.
This article focuses on how to differentiate and treat these patterns using herbal medicine and acupuncture. An overview of clinical trials is provided, and case examples are also included.
The authors from the ‘Equine Acupuncture Center/University of Florida, USA, concluded that the combination of TCVM and Western medicine (WM) can be an effective therapeutic approach to control seizures and epilepsy. WM is effective for initial control of severe seizures and in identification of the cause of the disease. TCVM can be effectively used for the treatment of milder cases and to help control seizures in those patients that fail to respond to WM.
Having done some research into acupuncture for animals myself, I was particularly interested in this aspect of the paper – interested and disappointed, I have to admit. The sad truth is that, despite the opimistic conclusions of the authors, there is no sound evidence. As no good evidence has emerged since, our own systematic review of 2006 (which was not cited by the authors of the above article) still holds true:
Acupuncture is a popular complementary treatment option in human medicine. Increasingly, owners also seek acupuncture for their animals. The aim of the systematic review reported here was to summarize and assess the clinical evidence for or against the effectiveness of acupuncture in veterinary medicine. Systematic searches were conducted on Medline, Embase, Amed, Cinahl, Japana Centra Revuo Medicina and Chikusan Bunken Kensaku. Hand-searches included conference proceedings, bibliographies, and contact with experts and veterinary acupuncture associations. There were no restrictions regarding the language of publication. All controlled clinical trials testing acupuncture in any condition of domestic animals were included. Studies using laboratory animals were excluded. Titles and abstracts of identified articles were read, and hard copies were obtained. Inclusion and exclusion of studies, data extraction, and validation were performed independently by two reviewers. Methodologic quality was evaluated by means of the Jadad score. Fourteen randomized controlled trials and 17 nonrandomized controlled trials met our criteria and were, therefore, included. The methodologic quality of these trials was variable but, on average, was low. For cutaneous pain and diarrhea, encouraging evidence exists that warrants further investigation in rigorous trials. Single studies reported some positive intergroup differences for spinal cord injury, Cushing’s syndrome, lung function, hepatitis, and rumen acidosis. These trials require independent replication. On the basis of the findings of this systematic review, there is no compelling evidence to recommend or reject acupuncture for any condition in domestic animals. Some encouraging data do exist that warrant further investigation in independent rigorous trials.
The AHVMA-article becomes wholly farcical, once we see the heading the AHVMA-journal has given it:
SCIENTIFIC REVIEW
The AHVMA-journal is the official publication of the American Holistic Veterinary Medical Association, according to their own statement, is the mindful leader elevating the veterinary professional through innovation, education, and advocacy of integrative medicine.
One stated objective of the AHVMA is to advance and educate in the science and art of holistic veterinary medicine. If their new ‘scientific review’ is anything to go by, they seem to have a most bizarre view about science. The question that occurred to me while reading the paper was this: are they not promoting animal abuse, a term defined as any use or treatment of animals that seems unnecessarily cruel, regardless of whether the act is against the law?
I have to admit that the ‘Asian Journal of Pharmaceutical Research and Development‘ did not formerly belong to my reading list. This will have to change, I guess, because any journal capable of publishing such a hilarious spoof ought to be read regularly.
The article in question is entitled ‘An Integrative Medicine Is Prudential Hope for Covid-19 Therapeutics‘ and is authored by Mayank dimri, Rajendra Singh Pawar, Virbal Singh Rajwar, Luv Kush from the SBS University Balawala, Dehradun- Uttarakhand, India. The paper is so unique that I simply could not resist showing you an excerpt. I hope you have as much fun reading it as I had when I was alerted to this masterpiece.
…
Antiviral Astrological Rationality The viral infectivity is governed by Saturn, Rahu and Ketu. COVID-19 is geminian virus, ruled by mercury. It rules lungs / respiratory system and also health/ nutrition house (6th). Antiviral astrological advices are: Stay away from crowds, maintain maximum cleanness and personal hygiene, dietary regimens should be enriched by vitamins, vegetables, nuts and fruits. The foods and drinking water should be warm. The cold and unhealthy environment may be avoided.
The complimentary / alternative integrative medicine conceptualized ethical use of traditional re- medies with
self-responsibility. The concept of herd immunity (epidemological) relates to population. The orthomolecular
medicine10prescribe nutritional supplements for restoration of antiviral immunity. Both have antiviral benefits for fighting global pandemic of COVID-19.
The desirable antiviral activities are anti-replicating to block viral replication, anti-inflammatory for preventing
viral inflammation. Immune stimulatory for strengthening innate immunity and anti-mutagenic for curbing viral mutations.
The ayurvedic herbs have antiviral phytochemicals. Some of them are listed here: Ursolic acid, Apigenin, Rosmarinic acid, Oleanolic acid, Elenoic acid, Hypercin,Liquiritigenin, Acetoside, Glycyrrhizin etc. They have anti RSV activity and possibly prevent viral entry to host cells. The plant extract of Plantago asiatica and Clerodendrum trichotomum proved to be effective antiviral. Fifatrol is an ayurvedic prized medicine against viruses. It is useful in treatment of viral upper respiratory infections and relief from nasal congestion. It is a supportive therapy against COVID-19 virus.
The synergism of vitamins (A, C, D, E) acts as revitaler for fighting against COVID-19. Vitamin C has great potential
as antiviral for respiratory infections. It prevents cytokine induced lung damage and natural immune booster.
Eucalyptus oil has multiple benefits.It is supporter of respiratory system, immune booster and anti-inflammatory. Aromadendrene is an aroma therapeutical, present in oil and moderate antiviral….
I know that the last few months have not been easy for many of us. Therefore, we should be all the more thankful for those who lighten our spirits with some comic relief…
… or did they actually mean what they wrote?
New German Medicine?
German New Medicine?
What on earth is that?
German New Medicine (GNM) is the creation of Ryke Geerd Hamer (1935-2017), a German doctor. The name is reminiscent of the ‘Neue Deutsche Heilkunde’ created by the Nazis during the Third Reich. Hamer received his medical licence in 1963 but was later struck off because of malpractice. He then continued his practice as a ‘Heilpraktiker’. According to proponents, GNM Therapy is a spoken therapy based on the findings and research of the Germanic New Medicine of Dr.Hamer. On the understanding that every disease is triggered by an isolating and shocking event, GNM Therapy assists in finding the DHS (shocking moment) in our lives that preceded the dis-ease and in turn allowing our bodies to complete its natural healing cycle back to full health. Hamer believed to have discovered the ‘5 laws of nature’:
- The Iron Rule of Cancer
- The two-phased development of disease
- Ontogenetic system of tumours and cancer equivalent diseases
- Ontogenetic system of microbes
- Natures biological meaning of a disease
Hamer also postulated that:
- All diseases are caused by psychological conflicts.
- Conventional medicine is a conspiracy of Jews to decimate the non-Jewish population.
- Microbes do not cause diseases.
- AIDS is just an allergy.
- Cancer is the result of a mental shock.
None of Hamer’s ‘discoveries’ and assumptions are plausible or based on facts, and none of his therapeutic approaches have been shown to be effective.
These days, I do not easily get surprised by what I read about so-called alternative medicine (SCAM), but this article entitled ‘Homoeopathy And New German Medicine: Two German Siblings‘ baffled me greatly. Here are a few short excerpts:
… German New Medicine (GNM) like Homoeopathy is one of the gentle healing methods. As siblings, they have some common features as well as their own unique features. So, let’s explore a unique relationship between these two siblings.
1) Holistic aspect:
Both therapeutic methods are believed in holistic concept of body. The disease condition in Homoeopathy and conflict in GNM are very similar in expression as they are reflecting on mental as well as physical level also. In Homoeopathy, Mind, Body and Soul are one of the important trios to understand the Homoeopathic philosophy. While in GNM, Psyche, Brain, Body are important aspect in learning the GNM. Let’s see these trio in their founder’s language,
• Homoeopathy:
Dr. Hahnemann in his oragnon of medicine, 6th edition mentioned about a unity of materialistic body and vital force. Last lines of aphorism 15 are as follows, “…although in thought our mind separates these two unities into distinct conceptions for the sake of easy comprehension.
• German New Medicine:
Dr. Ryke Geerd Hamer, founder of GNM said that, “The differentiation between psyche, brain and the body is purely academic. In reality, they are one.”
2) Disease origin concept:
• Homoeopathy:
In Homoeopathy, disease originates from the dynamic disturbances and followed by functional and pathological changes.
• German New Medicine:
In GNM, morbid condition starts from conflict in the psyche level and later it reflects on body. The common feature is the disturbance is at the all levels of man.
3) Cause of disease:
• Homoeopathy:
In Homoeopathy, among the web of causations, psyche (mind) is also considers as a cause of disease.
• German New Medicine:
So, in GNM, psyche is playing important role in cause of disease. When Conflict starts, its dynamic effect perceived first at mind level.
4) Individuality:
• Homoeopathy:
In Homoeopathy, diathesis is a predisposition for disease condition. i.e. According to the diathesis every individual suffers with their own individual morbid dispositions. Rheumatic diathesis, gouty diathesis, etc. are the examples of diathesis.
• German New Medicine:
In GNM, every individual suffers from the disease condition after the receiving conflict. It is different and depending upon the type of conflict they are receiving. E.g. lung cancer- death fright conflict, cervical cancer –female sexual conflict…
Conclusion:
Some similarities and with some own characteristics, these two healing methods are developing at a good length in medical science. The main aim of these both methods is – “to serve the suffering humanity in gentle way”…
_____________________
Could it be that the author forgot the most striking similarities between GNM and homeopathy? How about these points:
- There is nothing truly gentle about either methods.
- Both are based on bizarre fantasies, far removed from reality.
- Both pretend to be a panacea.
- Both lack proof of efficacy.
- Both have the potential to kill patients (mostly through neglect).
- Both mislead consumers.
- Both are deeply anti-scientific.
- Both dissuade patients from using evidence-based healthcare.
- Both are in conflict with medical ethics.
- Both have cult-like features.
- Both are far from being recognised by proper healthcare.
- Both have been repeatedly in conflict with the law.
- Both were invented by deludes fanatics.
I missed this article by Canadian vascular surgeons when it came out in 2018. It is well-argued, and I think you should read it in full, if you can get access (it’s behind a pay wall). It contains interesting details about the anti-vax attitude of doctors of integrative medicine (something we discussed before), as well as the most dubious things that go on in the ‘Cleveland Clinic’. Here is at least the abstract of the article:
Evidence-based medicine, first described in 1992, offers a clear, systematic, and scientific approach to the practice of medicine. Recently, the non-evidence-based practice of complementary and alternative medicine (CAM) has been increasing in the United States and around the world, particularly at medical institutions known for providing rigorous evidence-based care. The use of CAM may cause harm to patients through interactions with evidence-based medications or if patients choose to forego evidence-based care. CAM may also put financial strain on patients as most CAM expenditures are paid out-of-pocket. Despite these drawbacks, patients continue to use CAM due to media promotion of CAM therapies, dissatisfaction with conventional healthcare, and a desire for more holistic care. Given the increasing demand for CAM, many medical institutions now offer CAM services. Recently, there has been controversy surrounding the leaders of several CAM centres based at a highly respected academic medical institution, as they publicly expressed anti-vaccination views. These controversies demonstrate the non-evidence-based philosophies that run deep within CAM that are contrary to the evidence-based care that academic medical institutions should provide. Although there are financial incentives for institutions to provide CAM, it is important to recognize that this legitimizes CAM and may cause harm to patients. The poor regulation of CAM allows for the continued distribution of products and services that have not been rigorously tested for safety and efficacy. Governments in Australia and England have successfully improved regulation of CAM and can serve as a model to other countries.
Those who have been following this blog a little know how much I agree with these authors. In fact, in the peer-reviewed literature, I have been publishing similar arguments for almost 20 years, e.g:
- Integrative medicine: not a carte blanche for untested nonsense. Ernst E. Arch Intern Med 2002. PMID 12153386
- Disentangling integrative medicine Ernst E. Mayo Clin Proc 2004 – Review. PMID 15065622
- Integrated medicine. Ernst E. J Intern Med 2012. PMID 21682782 Free article.
- Integrative medicine: more than the promotion of unproven treatments? Ernst E. Med J Aust 2016. PMID 26985838
I receive all the energy I need by charging my butthole in the sunlight!
Actually, I don’t, but some people do!
The new so-called alternative medicine (SCAM) of ‘perineum sunning’ has become all the rage. It gives an entirely new meaning to the word ‘holism’. And, like all good SCAMs, it has a long tradition. This article explains:
Butt chugging, or ‘perineum sunning’, is the latest wellness and health trend to take over Instagram, but should you be stripping off?
What if I told you there was a 30-second trick to having a healthier libido, getting deeper sleep, boosting your creativity, super-charging your focus and having more balanced hormone function?
Well, apparently all you need to do is remove your Bonds and let your nether regions soak in some vitamin D. Gird your loins, friends, apparently “butt chugging” is a legitimate wellness trend and we’re completely and utterly perplexed.
Bringing “butt chugging”, or “perineum sunning” if you want to get official about it, into the cultural lexicon is self-proclaimed healer, teacher and micro-influencer Metaphysical Meagan. This week, the superfood lover went veritably viral after preaching about the “profound” benefits of perineum sunning on Instagram. Cue: much laughter, then much confusion.
A fan explained on Instagram:
30 seconds of sunlight on your butthole is the equivalent of a full day of sunlight with your clothes on,” and that it is “an ancient Taoist practice that’s been around for a while!” (Yes, because that is what “ancient” means.) A few weeks after her initial post, presumably because more and more people went to her page to comment after finding various jokes about it online, Metaphysical Meagan posted the photo on Instagram for a second time, now with an outrageously long caption meant to correct any misinformation. She explains that suntanning your asshole is meant to promote the “health & longevity of the physical body,” increase “creativity and creative output” and aid “in a healthy libido & balanced sexual energy.” It is definitely “NOT TO TAN YOUR BUTTHOLE‼️‼️” Also, “sunscreen is not required.
So, perineum sunning is an ancient Taoist practice. That makes sense: rituals and exercises aimed at aligning oneself spiritually with cosmic forces, at undertaking ecstatic spiritual journeys, or at improving physical health are all-important elements of Taoism. And if it’s got such a noble, long tradition, perineum sunning must be good, mustn’t it? No evidence needed!
As I said at the beginning of this post, I have not yet had the pleasure of experiencing this SCAM. But now I am tempted, of course. As soon as the sun is out, I will try it in my garden. I do wonder, however, what the neighbours will think!