test of time
The BBC stands for reliable information, at least that’s what I used to believe. After reading a recent article published on the BBC website, I have my doubts, however. See for yourself; here are a few excerpts:
On a holiday to Kerala on India’s south-western Malabar Coast, Shilpa Iyer decided to visit Kotakkal, a town that became famous after the establishment of Arya Vaidya Sala, Kerala’s best-known centre for the practice of Ayurveda, in 1902. Seven days later, she left the historical treatment centre after completeing panchakarma, a cleansing and rejuvenating programme for the body, mind and consciousness.
“There was nothing really wrong, but I was always busy with the demands of modern life and plagued with continual aches and pains. So, I decided to focus on my own health,” Iyer says.
Panchakarma, a holistic Ayurvedic therapy, involves a series of detoxifying procedures. It integrates herbal medicines, cleansing therapies, personalised diet plans and wellness activities to eliminate the root cause of disease, revive and rejuvenate the body, and ensure health and longevity.
Iyer says she left “feeling lighter, healthier and better than ever before”. She isn’t the only one who signed up for an Ayurvedic treatment in Kerala; the holistic system of medicine is a way of life in this coastal paradise.
… Ayurveda translates to “knowledge of life” and originated in India more than 3,000 years ago. It is based on the ideology that health and wellness depend on a delicate balance between the mind, body, spirit and environment, and places great emphasis on preventive strategies rather than curative ones. The ancient system of medicine is centred on the idea of universal interconnectedness between prakriti (the body’s constitution) and doshas (life forces). Varied combinations of the five elements — aakash (sky), jal (water), prithvi (earth), agni (fire) and vayu (air) – create the three doshas.

Dr Gaurang Paneri, an Ayurveda practitioner, explains every person has the three doshas, vata, pitta and kapha, in varying strength and magnitude. “The predominant dosha determines their prakriti. Diseases arise when doshas are affected because of an external or internal stimulus (typically linked to eating habits, lifestyle or physical exercise). Ayurveda works to ensure harmony between the three,” he says…
The small state has more than 100 Ayurvedic government-run hospitals, 800 Ayurvedic pharmaceutical factories and 800 Ayurvedic medicine dispensaries. As many as 120 holiday resorts and private wellness centres offer specialised treatments such as kasti vvasti, an oil-based treatment for back pain and inflammation in the lumbosacral region; elakkizhi, a treatment with heated herbal poultices to tackles aches, pains and muskoskeletal trauma; njavara kizhi, a massage therapy for arthritis or chronic musculoskeletal discomfort; and shirodhara, a restorative therapy to ease stress and anxiety and that involves pouring warm, medicated oil over the forehead.
Most treatment centres offer therapies and treatments for a range of health issues, including immunity, mental health, anxiety, pain management, weight loss, skin and health care, sleep issues, psoriasis, eczema, eye care, arthritis, sciatica, gastric problems and paralysis. The treatments typically include dietary changes, herbal medicines, massage therapies, poultices, meditation and breath exercises…
___________________________
I find such advertisements disguised as journalism disturbing:
- No mention that the treatments in question lack conclusive evidence of effectiveness.
- Not a word about the fact that many can be outright dangerous.
- No mention of the often exorbitant fees visitors are asked to pay.
Please do better next time you report about health matters, BBC!
It has been reported that 5 people who took a Japanese health supplement have died and more than 100 have been hospitalized as of Friday, a week after a pharmaceutical company issued a recall of the products, officials said. Osaka-based Kobayashi Pharmaceutical Co. came under fire for not going public quickly with problems known internally as early as January. Yet the first public announcement came only on 22 March. Company officials said 114 people were being treated in hospitals after taking products — including Benikoji Choleste Help meant to lower cholesterol — that contain an ingredient called benikoji, a red species of mold. Some people developed kidney problems after taking the supplements, but the exact cause was still under investigation in cooperation with government laboratories, according to the manufacturer.
“We apologize deeply,” President Akihiro Kobayashi told reporters last Friday, bowing for a long time to emphasize the apology alongside three other top company officials. He expressed remorse to those who have died and have been taken ill and to their families. He also apologized for the troubles caused to the entire health food industry and the medical profession, adding that the company was working to prevent further damage and improve crisis management.
The company’s products have been recalled — as have dozens of other products that contain benikoji, including miso paste, crackers, and a vinegar dressing. Japan’s health ministry put up a list on its official site of all the recalled products, including some that use benikoji for food coloring. The ministry warned the deaths could keep growing. The supplements could be bought at drug stores without a prescription from a doctor, and some may have been purchased or exported before the recall, including by tourists who may not be aware of the health risks.
Kobayashi Pharmaceutical had been selling benikoji products for years, with a million packages sold over the past 3 fiscal years, but a problem crept up with the supplements produced in 2023. Kobayashi Pharmaceutical said it produced 18.5 tons of benikoji last year. Some analysts blame the recent deregulation initiatives, which simplified and sped up approval for health products to spur economic growth.
________________________
Anouther source reported that Japanese authorities on Saturday raided a drug factory after a pharmaceutical company reported at least five deaths and 114 hospitalizations possibly linked to a health supplement. About a dozen Japanese health officials walked into the Osaka plant of the Kobayashi Pharmaceutical Co., as seen in footage of the raid widely telecasted on Japanese news. The health supplement in question is a pink pill called Benikoji Choleste Help. It is said to help lower cholesterol levels. A key ingredient is benikoji, a type of red mold. The company has said it knows little about the cause of the sickness, which can include kidney failure. It is currently investigating the effects in cooperation with Japan’s government.
___________________________
More recent reports update the figure of affected individuals: Japanese dietary supplements at the center of an expanding health scare have now been linked to at least 157 hospitalizations, a health ministry official said Tuesday.The figure reflects an increase from the 114 hospitalization cases that Kobayashi Pharmaceutical said on Friday were linked to its products containing red yeast rice, or beni kōji.
A Kobayashi Pharmaceutical spokeswoman confirmed the latest hospitalization cases without elaborating further.
Benikoji is widely sold and used; not just in Japan. It comes under a range of different names:
- red yeast rice,
- red fermented rice,
- red kojic rice,
- red koji rice,
- anka,
- angkak,
- Ben Cao Gang Mu.
It is a bright reddish purple fermented rice which acquires its color from being cultivated with the mold Monascus purpureus. Red yeast rice is used as food and as a medicine in Asian cultures, such as Kampo and TCM.
It contains lovastatin which, of course, became patented and is marketed as the prescription drug, Mevacor. Red yeast rice went on to become a non-prescription dietary supplement in the United States and other countries. In 1998, the U.S. FDA banned a dietary supplement containing red yeast rice extract, stating that red yeast rice products containing monacolin K are identical to a prescription drug, and thus subject to regulation as a drug.
Whenever a journalist wants to discuss the subject of acupuncture with me, he or she will inevitably ask one question:
DOES ACUPUNCTURE WORK?
It seems a legitimate, obvious and simple question, particularly during ‘Acupuncture Awareness Week‘, and I have heard it hundreds of times. Why then do I hesitate to answer it?
Journalists – like most of us – would like a straight answer, like YES or NO. But straight answers are in short supply, particularly when we are talking about acupuncture.
Let me explain.
Acupuncture is part of ‘Traditional Chinese Medicine’ (TCM). It is said to re-balance the life forces that determine our health. As such it is seen as a panacea, a treatment for all ills. Therefore, the question, does it work?, ought to be more specific: does it work for pain, obesity, fatigue, hair-loss, addiction, anxiety, ADHA, depression, asthma, old age, etc.etc. As we are dealing with virtually thousands of ills, the question, does it work?, quickly explodes into thousands of more specific questions.
But that’s not all!
The question, does acupuncture work?, assumes that we are talking about one therapy. Yet, there are dozens of different acupuncture traditions and sites:
- body acupuncture,
- ear acupuncture,
- tongue acupuncture,
- scalp acupuncture,
- etc., etc.
Then there are dozens of different ways to stimulate acupuncture points:
- needle acupuncture,
- electroacupuncture,
- acupressure,
- moxibustion,
- ultrasound acupuncture,
- laser acupuncture,
- etc., etc.
And then there are, of course, different acupuncture ‘philosophies’ or cultures:
- TCM,
- ‘Western’ acupuncture,
- Korean acupuncture,
- Japanese acupuncture,
- etc., etc.
If we multiply these different options, we surely arrive at thousands of different variations of acupuncture being used for thousands of different conditions.
But this is still not all!
To answer the question, does it work?, we today have easily around 10 000 clinical trials. One might therefore think that, despite the mentioned complexity, we might find several conclusive answers for the more specific questions. But there are very significant obstacles that are in our way:
- most acupuncture trials are of lousy quality;
- most were conducted by lousy researchers who merely aim at showing that acupuncture works rather that testing whether it is effective;
- most originate from China and are published in Chinese which means that most of us cannot access them;
- they get nevertheless included in many of the systematic reviews that are currently being published without non-Chinese speakers ever being able to scrutinise them;
- TCM is a hugely important export article for China which means that political influence is abundant;
- several investigators have noted that virtually 100% of Chinese acupuncture trials report positive results regardless of the condition that is being targeted;
- it has been reported that about 80% of studies emerging from China are fabricated.
Now, I think you understand why I hesitate every time a journalist asks me:
DOES ACUPUNCTURE WORK?
Most journalists do not have the patience to listen to all the complexity this question evokes. Many do not have the intellectual capacity to comprehend an exhaustive reply. But all want to hear a simple and conclusive answer.
So, what do I say in this situation?
Usually, I respond that the answer would depend on who one asks. An acupuncturist is likely to say: YES, OF COURSE, IT DOES! An less biased expert might reply:
IT’S COMPLEX, BUT THE MOST RELIABLE EVIDENCE IS FAR FROM CONVINCING.
The Amercian Medical Association (AMA) recently published a lengthy article on naturopathy in the US. Here are some excerpts:
There are three types of health professionals who offer naturopathic treatment:
- Naturopathic doctors. These nonphysicians graduate from a four-year, professional-level program at an accredited naturopathic medical school, earning either the doctor of naturopathy (ND) degree or the doctor of naturopathic medicine (NMD) degree.
- Traditional naturopaths, who have obtained education through some combination of a mentorship program with another professional or at an alternative clinic, distance-learning program or classroom schooling on natural health, or other holistic studies.
- Other health professionals such as chiropractors, massage therapists, dentists, nurses, nutritionists, or physicians who practice under a professional license but include some naturopathic methods in their practice and who may have studied on their own or taken courses on naturopathic methods.
At least 24 states and the District of Columbia regulate the practice of naturopathy. In order to be licensed, naturopaths in these states must earn an ND or NMD from an accredited naturopathic program and pass the Naturopathic Physicians Licensing Exam. Three states—Florida, South Carolina and Tennessee—prohibit the practice of naturopathy. In states that neither license nor prohibit the practice of naturopathy, traditional naturopaths and NDs alike may practice without being subject to state regulation.
Postgraduate training is neither common nor required of graduates of naturopathic schools, except in Utah … less than 10% of naturopaths participate in an approved residency, and such residencies last only a year and lack a high degree of standardization.
… naturopaths are required to get at least 1,200 hours of direct patient contact, physicians get 12,000–16,000 hours of clinical training…
ND programs emphasize naturopathic principes—for example, the healing power of nature—and naturopathic therapeutics such as botanical medicine, homeopoathy and hydrotherapy. Coursework in naturopathic therapeutics is combined with, and taught alongside, coursework in sciences. But there are no specifications around the number of hours required in each area … naturopathic students may lack exposure to key clinical scenarios in the course of their training … naturopathic students’ clinical experience is typically gained through outpatient health care clinics, as naturopathic medical schools typically do not have significant hospital affiliation. This means there is no guarantee that a naturopathic student completing a clinical rotation will see patients who are actually sick or hospitalized, and they may not be exposed to infants, children, adolescents or the elderly. It has been said that naturopaths tend to treat the “worried well.”
… Naturopaths claim they are trained as primary care providers and, as such, are educated and trained to diagnose, manage and treat many conditions, including bloodstream infections, heart disease and autoimmune disorders. Yet their education and training falls several years and thousands of hours short of what physicians get.
…The AMA believes it is the responsibility of policymakers to ensure that naturopaths’ claims that they can treat a broad range of conditions are backed by facts—facts that include the specific education and training necessary to ensure patient safety.
________________
The AMA is clearly cautious here. A less polite statement might simply stress that naturopaths are taught a lot of nonsense which they later tend to administer to their unsuspecting patients. On this blog, we have repeatedly discussed the danger naturopaths present to public health in the US and elsewhere, e.g.:
- How reliable are the claims made by naturopathic influencers?
- Naturopath jailed for selling fraudulent vaccination documents
- Naturopath fined for misdiagnosing and treating a rectal tumor for hemorrhoids
- Naturopaths are ‘not bound by science,’ lawyer argues
- Vaccination rates of Canadian healthcare professionals: those of chiropractors and naturopaths are at the lowest
- Is veterinary naturopathy animal abuse?
- Naturopathic ‘cancer specialist’ using coffee enemas found guilty
- Patients consulting chiropractors, homeopaths, or naturopaths are less likely to agree to the flu jab
- A naturopath responsible for the death of two cancer patients was sentenced to two years
- A naturopath in court after two of his cancer patients died
- Many naturopaths, homeopaths, and chiropractors are a risk to public health
- Naturopath treats autism with fecal transplants
- A naturopath promoting fake news about COVID vaccinations
- Naturopathy (according to the WNF) = quackery steeped in obsolete fantasies
- Canadian naturopaths may no longer call themselves ‘medically trained’
- Naturopaths’ counselling against vaccinations could be criminally negligent
- Naturopathy for cancer … claims that have the potential to be lethal
- Severe liver injury due to naturopaths’ prescription of Epsom salt
- Naturopaths should not treat children
- Some naturopaths are clearly a danger to public health
- Death of a child through naturopathy
Claims that naturopaths are a viable alternative to evidence-based medicine are wrong, irresponsible and dangerous. Regulators must be reminded that they have the duty to protect the public from charlatans and should therefore ensure that no false therapeutic or diagnostic claims can be made by naturopaths.
An alarming story of research fraud in the area of so-called alternative medicine (SCAM) is unfolding: Bharat B. Aggarwal, the Indian-American biochemist who worked at MD Anderson Cancer Center, focused his research on curcumin, a compound found in turmeric, and authored more than 125 Medline-listed articles about it. They reported that curcumin had therapeutic potential for a variety of diseases, including various cancers, Alzheimer’s disease and, more recently, COVID-19.
The last of these papers, entitled “Curcumin, inflammation, and neurological disorders: How are they linked?”, was publiched only a few months ago. Here is its abstract:
Background: Despite the extensive research in recent years, the current treatment modalities for neurological disorders are suboptimal. Curcumin, a polyphenol found in Curcuma genus, has been shown to mitigate the pathophysiology and clinical sequalae involved in neuroinflammation and neurodegenerative diseases.
Methods: We searched PubMed database for relevant publications on curcumin and its uses in treating neurological diseases. We also reviewed relevant clinical trials which appeared on searching PubMed database using ‘Curcumin and clinical trials’.
Results: This review details the pleiotropic immunomodulatory functions and neuroprotective properties of curcumin, its derivatives and formulations in various preclinical and clinical investigations. The effects of curcumin on neurodegenerative diseases such as Alzheimer’s disease (AD), amyotrophic lateral sclerosis (ALS), brain tumors, epilepsy, Huntington’s disorder (HD), ischemia, Parkinson’s disease (PD), multiple sclerosis (MS), and traumatic brain injury (TBI) with a major focus on associated signalling pathways have been thoroughly discussed.
Conclusion: This review demonstrates curcumin can suppress spinal neuroinflammation by modulating diverse astroglia mediated cascades, ensuring the treatment of neurological disorders.
The Anderson Cancer Center initially appeared to approve of Aggarwal’s work. However, in 2012, following concerns about image manipulation raised by pseudonymous sleuth Juuichi Jigen, MD Anderson Cancer Center launched a research fraud probe against Aggarwal which eventually led to 30 of Aggarwal’s articles being retracted. Moreover, PubPeer commenters have noted irregularities in many publications beyond the 30 that have already been retracted. Aggarwal thus retired from M.D. Anderson in 2015.
Curcumin doesn’t work well as a therapeutic agent for any disease – see, for instance, the summary from Nelson et al. 2017:
“[No] form of curcumin, or its closely related analogues, appears to possess the properties required for a good drug candidate (chemical stability, high water solubility, potent and selective target activity, high bioavailability, broad tissue distribution, stable metabolism, and low toxicity). The in vitro interference properties of curcumin do, however, offer many traps that can trick unprepared researchers into misinterpreting the results of their investigations.”
Despite curcumin’s apparent lack of therapeutic promise, the volume of research produced on curcumin grows each year. More than 2,000 studies involving the compound are now published annually. Many of these studies bear signs of fraud and involvement of paper mills. As of 2020, the United States National Institutes of Health (NIH) has spent more than 150 million USD funding projects related to curcumin.
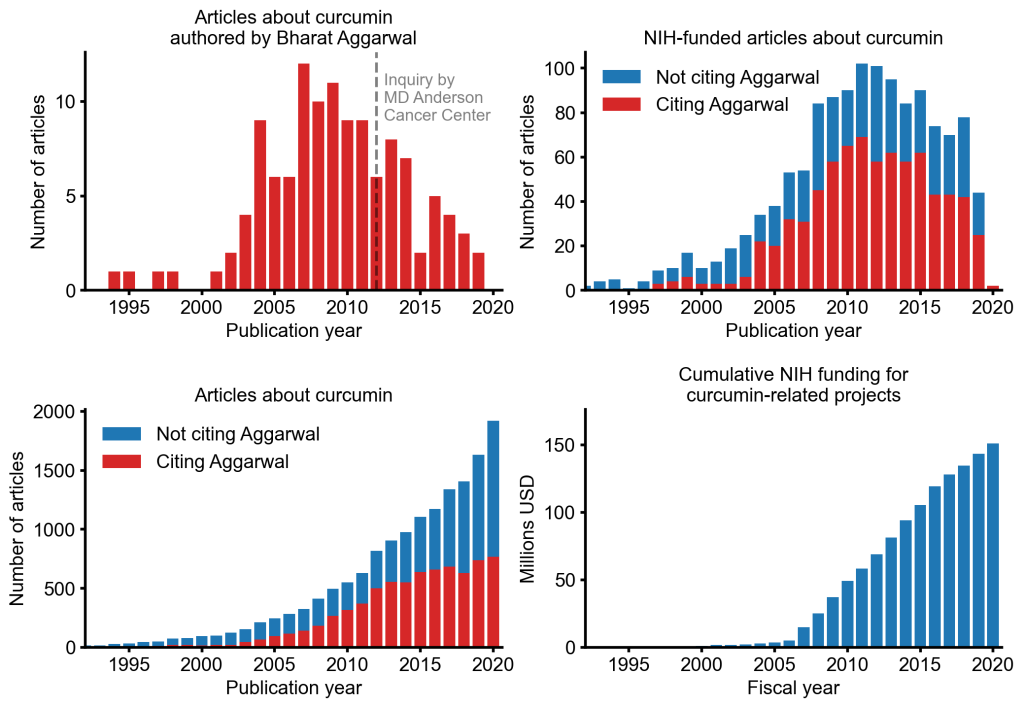
This proliferation of research has fueled curcumin’s popularity as a dietary supplement. It is estimated that the global market for curcumin as a supplement is around 30 million USD in 2020.
The damage done by this epic fraud is huge and far-reaching. Hundreds of millions of taxpayer dollars, countless hours spent toiling by junior scientists, thousands of laboratory animals sacrificed, thousands of cancer patients enrolled in clinical trials for ineffective treatments, and countless people who have eschewed effective cancer treatment in favor of curcumin, were encouraged by research steeped in lies.
Dragons’ Den is a British reality television business programme, presented by Evan Davis and based upon the original Japanese series. The show allows several entrepreneurs an opportunity to present their varying business ideas to a panel of five wealthy investors, the “Dragons” of the show’s title, and pitch for financial investment while offering a stake of the company in return.
It has been reported that Giselle Boxer began selling needle-free acupuncture kits for ears after being diagnosed with myalgic encephalomyelitis (ME). She said the technique had helped improve her own health. Ms Boxer worked for advertising agency before starting her business. A researcher on the show had contacted her to ask if she would like to take part.
Entrepreneur and former footballer Gary Neville was so impressed with her pitch he made her an offer in full before the Dragons had a chance to begin asking questions. She said the impact on the business since the show aired had been “bonkers”. “It’s just been a complete whirlwind,” she said.

The tiny beads are a needle-free form of auriculotherapy, designed to stimulate specific points of the ear to address physical and emotional health concerns. “It completely transformed my life alongside lots and lots of other things like diet, lifestyle changes, meditation, breathwork and movement,” said Ms Boxer. She has since had a child and claimed she was fully healed within a year. “It was like a full overhaul of my life,” Ms Boxer said. Her business, Acu Seeds, sells kits for people to use at home and made a £64,000 profit in its first year, she added.
On the Acu Seed website, we learn the following:
Ear seeds are a form of auriculotherapy, which is the stimulation of specific points of the ear to support physical and emotional health concerns. They are a needle-free form of acupuncture that have been used in Traditional Chinese Medicine (TCM) for thousands of years. TCM teaches that the ear is a microsystem of the whole body, where certain points on the ear correspond to different organs or body parts. Energy pathways (or ‘qi’ or vital life energy) pass through the ear and ear seeds stimulate specific points which send an abundant flow of energy to the related organ or area that needs attention. Think of it like reflexology, but for the ears instead of feet.
Ear seeds also create continual, gentle pressure on nerve impulses in the ear which send messages to the brain that certain organs or systems need support. The brain will then send signals and chemicals to the rest of the body to support whatever ailments you’re experiencing, releasing endorphins into the bloodstream, relaxing the nervous system, and naturally soothing pain and discomfort. Some people use ear seeds alongside acupuncture treatments as they may help the effects of acupuncture last longer between sessions.
I am impressed by the lingo used here:
- support physical and emotional health concerns – the seeds support the concerns but not the health?
- a needle-free form of acupuncture – sorry, the seeds don’t puncture anything; they exert pressure; therefore it’s called acuPRESSURE.
- have been used in Traditional Chinese Medicine (TCM) for thousands of years – no, it was invented just a few decades ago by Paul Nogier.
- TCM teaches that the ear is a microsystem of the whole body – TCM teaches plenty of nonsense but not this one.
- Energy pathways (or ‘qi’ or vital life energy) pass through the ear –Qi is nothing more than a figment of the imagination of TCM advocates.
- send an abundant flow of energy to the related organ or area – only if you believe in your own fictional form of physiology.
- Think of it like reflexology – which btw is also nonsense.
- nerve impulses in the ear send messages to the brain that certain organs or systems need support – only if you believe in your own fictional form of physiology.
- The brain will then send signals and chemicals to the rest of the body – only if you believe in your own fictional form of physiology.
- help the effects of acupuncture last longer – help the non-existing effects of acupuncture last longer?
One the website, we also learn what for which conditions the treatment is effective:
Ear seeds may support a broad spectrum of health concerns including anxiety, stress, headaches, digestion, immunity, focus, sleep and fatigue. Our ear seed kits include the protocol ear maps for these eight health concerns and each protocol uses between 3 to 5 ear seeds. Ear seeds have also been found to support with women’s health issues like menstrual issues, libido, fertility, postpartum issues, inflammation, menopause and weight loss. The ear maps for these issues are given in our women’s health ear seed kit bundles. The specific combination of seed placements will support your chosen health concern. Further issues that they may support with are addiction, pain, tinnitus, vertigo, thyroid health and more.
Here, I am afraid, we might have a major problem:
THERE IS NO GOOD EVIDENCE TO SUPPORT ANY OF THESE CLAIMS!
I thus do wonder whether the venture of Giselle Boxer might be a case for the Advertising Standards Authority.
It has been reported that King Charles’ charity, formerly the Prince’s Foundation, is compelled to return £110,000 to the Indian government. The funds were earmarked for an NHS alternative medicine clinic championed by Charles, which never materialised. The proposed clinic was aimed at integrating Indian traditional medicine into the UK’s healthcare system.
But why did the plan fail?
The answer is simple: the National Health Service (NHS) did not approve it.
The history of the UK ‘Ayurvedic Centre of Excellence’ goes back several years. Here is an excerpt of my book ‘CHARLES, THE ALTERNATIVE KING‘ where I discuss it as one of Charles’ many pipe dreams in the realm of so-called alternative medicine (SCAM):
In 2018, India’s prime minister Narendra Modi paid a visit to the Science Museum in London where he inspected the ‘5000 Years of Science and Innovation’ exhibition. The event was hosted by Charles and included the announcement of new ‘Ayurvedic Centres of Excellence’, allegedly a ‘first-of-its-kind’ global network for evidence-based research on yoga and Ayurveda. The first centre was said to open in 2018 in London. Funding was to come partly from the Indian government and partly from private donors. The central remit of the new initiative was reported to be researching the effects of Ayurvedic medicine.
Dr Michael Dixon (yes, you may have met him several times before, e.g. here, here, or here) commented: “This is going to be the first Ayurvedic centre of excellence in the UK. We will be providing, on the NHS, patients with yoga, with demonstrations and education on healthy eating, Ayurvedic diets, and massage including reflexology and Indian head massage. And all this will be subject to a research project led by Westminster University, to find out whether the English population will take to yoga and these sorts of treatments. Whether they will be helped by it and finally whether it will reduce the call on NHS resources leading to less GP consultations, hospital admissions and operations.”
On its website, the College of Medicine and Integrated Health announced that a memorandum of understanding with India’s Ministry of Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy (AYUSH) had been signed “to create centres of excellence in the UK … Dr Michael Dixon agreed the joint venture to provide the UK centres, which will offer and research traditional Indian medicine… The Indian government will match private UK donations to fund the AYUSH centres in the UK”. In November 2019, the following press release by the president of India offered more details:
The Prince of Wales called on the President of India, Shri Ram Nath Kovind, at Rashtrapati Bhavan today (November 13, 2019).
Welcoming the Prince to India, the President congratulated him on his election as the head of the Commonwealth. He said that India considers the Commonwealth as an important grouping that voices the concerns of a large number of countries, including the Small Island Developing States.
The President said that India and the United Kingdom are natural partners bound by historical ties and shared values of democracy, rule of law and respect for multi-cultural society. As the world’s pre-eminent democracies, our two countries have much to contribute together to effectively address the many challenges faced by the world today.
The Prince planted a Champa sapling – plant native to the subcontinent which has several uses in Ayurveda – in the Herbal Garden of Rashtrapati Bhavan. He was taken around the garden and shown different plants that have medicinal properties. The Prince showed a keen interest in India’s alternative model of healthcare.
The President thanked the Prince of Wales for his support for Ayurveda research. The Prince of Wales Charitable Foundation and the All India Institute of Ayurveda signed an MOU during the visit of Prime Minister Narendra Modi to the UK in April 2018. Under the MOU, the All India Institute of Ayurveda and the College of Medicine, UK will be conducting clinical research on Depression, Anxiety and Fibromyalgia. They will also be undertaking training programme for the development of Standard Operating Protocol on “AYURYOGA” for UK Health professionals.
_________________________
END OF EXCERPT
Charles’ initiative, encompassing Ayurveda, yoga, naturopathy, and homeopathy, was intended to be a landmark project, with the Indian government contributing £110,000 to the King’s Foundation for its implementation. However, the NHS, responsible for St Charles Hospital, never endorsed the project. Despite initial talks, the proposed collaboration did not progress, and the clinic failed to materialise. According to the west London clinical commissioning group (CCG), which oversaw the hospital at the time, there was no official involvement, and discussions ceased in 2020.
Under charity law, funds designated for a specific project cannot be diverted without donor permission and regulatory approval. The King’s Foundation has acknowledged the need to return the remaining budget to the Indian government but has not disclosed when this decision was made or why the funds were not promptly returned.
The initiative faced opposition from the NHS, as a year before the clinic’s launch, NHS England’s CEO Simon Stevens had issued guidance discouraging the prescription of homeopathy and herbal remedies, citing their limited efficacy and misuse of NHS funds.
Despite the failed project, connections between key figures persist. Dr Michael Dixon played a significant role in finalising agreements with the Indian government. The King’s Foundation defended its actions, stating that due to the Covid-19 pandemic, the project shifted online, resulting in reduced costs. They claim to have contacted the Indian government for the return of unused funds, emphasising that the money remains in a restricted account.
As the controversy unfolds, questions arise about the intersections between alternative medicine advocacy, royal endorsements, and international collaborations within the context of public healthcare.
An article in the Daily Mail reported that the original plan proposed that Ayush treatments would be provided to patients, who would be referred by local GPs, at St Charles Hospital in Kensington. Isaac Mathai, who runs Soukya, a homeopathic yoga retreat in Bangalore which Charles and Camilla have visited, was an adviser to the project at St Charles Hospital.
The Indian government made a payment from the budget of the Ayush Ministry, which Mr Modi has used as a tool of diplomacy to promote Indian medicine and culture worldwide, to the King’s Foundation. It was proposed the charity would use its expertise to help set up the clinic. But the NHS at no point agreed to the plans.
A spokesman of the west London clinical commissioning group (CCG), which administered St Charles Hospital at the time, said: ‘Provision of homeopathy and herbal treatments were not considered as part of the project by the CCG. The aim of the project was to test the use of yoga and massage to support the overall health and wellbeing of patients with long-term conditions.’ A King’s Foundation spokesman added that the initial intention had been to deliver Indian traditional medicine at St Charles Hospital.
Certain aspects of yoga can be used as a non-pharmacological conservative therapeutic approach to the management of chronic low back pain (CLBP). This overview summarized and evaluated data from current systematic reviews (SRs) on the use of yoga for CLBP.
The researchers searched SRs on the use of yoga for CLBP in nine electronic databases from inception to September 2023. The methodological quality was evaluated using the Assessment of Multiple Systematic Review Scale-2 (AMSTAR-2). The reporting quality of the included SRs was evaluated using the Preferred Reporting Item for Systematic Review and Meta-Analysis-2020 (PRISMA-2020), and the quality of data was graded using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE). Two independent researchers performed the screening, data extraction, and quality assessment process of SRs.
A total of 13 SRs were included. The results of the AMSTAR-2 indicated that the methodological quality of the included studies was relatively low. The PRISMA-2020 checklist evaluation results indicated that methodological limitations in reporting, especially regarding data processing and presentation, were the main weaknesses. The GRADE assessment indicated that 30 outcomes were rated moderate, 42 were rated low level, and 20 were rated very low level. Downgrading factors were mainly due to the limitations of the included studies.
The authors concluded that yoga appears to be an effective and safe non-pharmacological therapeutic modality for the Management of CLBP. Currently, it may exhibit better efficacy in improving pain and functional disability associated with CLBP. However, the methodological quality and quality of evidence for SRs/MAs in the included studies were generally low, and these results should be interpreted cautiously.
Sorry, but I beg to differ!
- The safety of a therapy cannot be ascertained on the basis of such small sample sizes.
- The effectiveness of yoga has not been demonstrated by these data.
- All that has been shown with this review is that the quality of the research in this area is too poor for drawing conclusions.
Congratulations to Joseph Prahlow, MD, who is the winner of the Excellence in Homeopathy Award! Here are the conclusions of his winning essay. Special thanks to Hermeet Singh and Boiron for their prize donation.
Despite the many obstacles and challenges which face homeopathy in the 21st century, the homeopathic community should be emboldened and encouraged by the fact that there are also many opportunities for the advancement of homeopathy as an alternative choice in health care.
Proclaim the Truth: Homeopathy Actually Works
Notwithstanding the challenges involved (especially for a student) in arriving at the correct simillimum for a case, let alone the appropriate follow-up and case management, the truth of the matter is that homeopathy does, in fact, work! Those of us who have been the beneficiaries of homeopathic care, or who have seen the benefits in others, know with no doubt whatsoever that homeopathy represents a truly amazing form of alternative medicine that is able to successfully treat patients having a wide range of health concerns, including some very ill individuals. And it’s not just based on “experience” or “perception,” although such evidence should not be discounted. Numerous studies show the effectiveness of homeopathy.6-9 The fact that homeopathy actually works represents one of the biggest and most important opportunities for homeopathy. The corresponding challenge relates to “getting the word out” into the general community as well as the medical community. Instead of homeopathy being the “last resort,” it should increasingly become the “first choice” amongst patients. Only by “spreading the word” of its success can this become a reality.
What intrigued me here was the evidence that an award-winning homeopath believes might justify the claim that
“Numerous studies show the effectiveness of homeopathy”
6. Mathie RT, Lloyd SM, Legg LA, et al. Randomised placebo-controlled trials of individualized homeopathic treatment: systematic review and meta-analysis. Syst Rev. 2014 Dec 6;3:142. doi: 10.1186/2046-4053-3-142.
As we have discussed previously that meta-analysis is phoney and created a false-positive result by omitting at least two negative studies.
7. Taylor JA, Jacobs J. Homeopathic ear drops as an adjunct in reducing antibiotic usage in children with otitis media. Glob Pediatr Health 2014 Nov 21;1:2333794X14559395. doi: 10.1177/2333794X14559395.
This study had the notorious A+B versus B design and thus was unable to test for specific effects of homeopathy. Moreover, the lead author, Dr Jennifer Jacobs, was a paid consultant to Standard Homeopathic Company.
8. Sorrentino L, Piraneo S, Riggio E, et al. Is there a role for homeopathy in breast cancer surgery? A first randomized clinical trial on treatment with Arnica montana to reduce post-operative seroma and bleeding in patients undergoing total mastectomy. J Intercult Ethnopharmacol 2017 Jan 3;6(1):1-8. doi: 10.5455/jice.20161229055245.
This study showed no significant result in the intention to treat analysis. The positive conclusion seems to be based on data dredging only.
9. Frass M, Lechleitner P, Grundling C, et al. Homeopathic treatment as an add-on therapy may improve quality of life and prolong survival in patients with non-small cell lung cancer: a randomized, placebo-controlled, double-blind, three-arm, multic0-e1955enter study. Oncologist 2020 Dec 25(12):e1930-e1955. doi: 10.1002/onco.13548.
This study is since months under investigation for fraud. The reasons for this have been discussed previously.
Perhaps the award winning author should chance the crucial sentence into something like:
Numerous studies have shown how homeopaths try to mislead the public?
In any case, please do not let this stop you from reading the full paper by the award-winning author. I promise you that it will create much hilarity.
What does homeopathy offer our modern ailing world?
NOTHING!
We have often discussed cupping on this blog, e.g.:
- The ‘WORST PAPER OF 2022 COMPETITION’ entry No 6: “The efficacy and safety of dry cupping in cervical spondylosis with optimization of cup application time – A randomized clinical trial”
- Cupping therapy for non-specific chronic low back pain
- Cupping for Olympic swimmers. Or: why breaking your shoulder is not necessarily good for writing a successful book
- Infant receiving cupping treatment prompts outrage
Yes, generally speaking I have been critical about cupping – not because I don’t like it (I even used the treatment as a young clinician many years ago) but because the evidence tells me to. I was glad to see that the authors of a recent article entitled “Utility of Cupping Therapy in Substance Use Disorder: A Novel Approach or a Bizarre Treatment?” offer even more outspoken words about the therapy. Here are their conclusions:
Established treatment modalities for substance use disorder and its withdrawal symptoms include pharmacotherapy and psychotherapy, but their utilization by the general population remains unsatisfactory. Taboos regarding mental health services and concerns about confidentiality are massive obstacles for patients seeking psychiatric help, and alternative forms of medicine may seem more approachable, even with the associated risks. As displayed in this case, cupping therapy is a traditional therapy with no role in treating polyaddiction and withdrawal symptoms, but it unnecessarily exposes individuals to really uncomfortable and often concealed complications such as bruising, and skin and blood infections, especially when carried out by untrained, incompetent individuals. While one can explore these options in addition to seeking professional mental health care, it is imperative to spread awareness about the roles, scientific soundness, and adverse effects of these alternative health practices. The health promotion and education sectors need reforms to educate the general population, especially the rural population in India, about the dangers of iatrogenesis caused by non-evidence-backed treatments. There needs to be an extensive advertisement of only the most effective and scientific treatment options provided by medical professionals, and the risks of overlooking them in favor of traditional cures propagated by unqualified individuals. With all the scientific advancements in the 21st century ranging from artificial intelligence in healthcare, and robotic surgeries, to extensive clinical trials for novel anti-cancer drugs, we cannot allow the propagation of ancient, scientifically unsound techniques that may cause more harm than benefit to patients.
Why, I am sure you ask yourself, are they so critical? The reason lies in the case they report in the same paper:
A 30-year-old man presented to the psychiatric outpatient department with complaints of nervousness, anxiety, a sense of impending doom, irritability, anger outbursts, headache, and reduced sleep and appetite for the last five days. The patient had a history of daily consumption of 5-10 mg of alprazolam tablets, 200-250 mg of codeine syrup, and about five packets of chewable tobacco over the last seven years; this was a pattern of polyaddiction to a benzodiazepine, opiate, and nicotine. The patient had no history of fever, confusion, or hallucinations. On eliciting the past history, the patient revealed that he went to an alternative medicine practitioner after his family persuaded him to seek help for his substance use disorder. After ceasing the consumption of all three substances for three days, he started developing the symptoms with which he presented to our hospital. He was hesitant to talk about his substance use disorder to medical professionals and concerned about confidentiality, and, hence, went to an alternative medicine practitioner whom he deemed approachable. There he was given wet cupping therapy on the head for four days, which involved the use of rubber pumps to create a suction inside the cups placed on his head. After three to five minutes, the cups were removed and small incisions were made on the cupping sites, following which a second suction caused the oozing out of blood from the incision sites on the scalp (Figure 1). But, this did not improve his symptoms, and hence, he stopped going there two days before coming to our tertiary care hospital.
On examination, the patient had a pulse rate of 76 beats per minute, blood pressure of 128/78 mm Hg, and respiratory rate of 22 per minute. He was well-oriented to time, place, and person. Systemic examination of the cardiovascular system was unremarkable. He denied any other substance use. The skin over his head had distinct cupping marks but no signs of infection or active bleeding, which are some common complications after cupping therapy (Figure 2). On assessment, the patient had a Clinical Opiate Withdrawal Scale (COWS) score of 13 and a Clinical Institute Withdrawal Assessment (CIWA) scale score of 26.
Later, the patient was admitted to the psychiatric ward to manage the withdrawal symptoms, where we initiated pharmacotherapy. Tablet diazepam (20 mg/day), sodium valproate (800 mg/day), tramadol (200 mg/day), thiamine (300 mg/day), paracetamol (500 mg/day) and intravenous fluids were given to the patient. We counseled the patient regarding substance abuse, its harmful effects, and de-addiction. The patient’s symptoms started to improve, and we continued the treatment for four days and discharged him with a COWS score of 4 and a CIWA score of 2. We intended to reassess him after 14 days, but we lost him to follow-up.


