methodology
The ‘keto diet’ is a currently popular high-fat, low-carbohydrate diet; it limits the intake of glucose which results in the production of ketones by the liver and their uptake as an alternative energy source by the brain. It is said to be an effective treatment for intractable epilepsy. In addition, it is being promoted as a so-called alternative medicine (SCAM) for a wide range of conditions, including:
- weight loss,
- cognitive and memory enhancement,
- type II diabetes,
- cancer,
- neurological and psychiatric disorders.
Now, it has been reported that the ‘keto diet’ may be linked to higher levels of cholesterol and double the risk of cardiovascular events. In the study, researchers defined a low-carb, high-fat (LCHF) diet as 45% of total daily calories coming from fat and 25% coming from carbohydrates. The study, which has so far not been peer-reviewed, was presented Sunday at the American College of Cardiology’s Annual Scientific Session Together With the World Congress of Cardiology.
“Our study rationale came from the fact that we would see patients in our cardiovascular prevention clinic with severe hypercholesterolemia following this diet,” said Dr. Iulia Iatan from the Healthy Heart Program Prevention Clinic, St. Paul’s Hospital, and University of British Columbia’s Centre for Heart Lung Innovation in Vancouver, Canada, during a presentation at the session. “This led us to wonder about the relationship between these low-carb, high-fat diets, lipid levels, and cardiovascular disease. And so, despite this, there’s limited data on this relationship.”
The researchers compared the diets of 305 people eating an LCHF diet with about 1,200 people eating a standard diet, using health information from the United Kingdom database UK Biobank, which followed people for at least a decade. They found that people on the LCHF diet had higher levels of low-density lipoprotein and apolipoprotein B. Apolipoprotein B is a protein that coats LDL cholesterol proteins and can predict heart disease better than elevated levels of LDL cholesterol can. The researchers also noticed that the LCHF diet participants’ total fat intake was higher in saturated fat and had double the consumption of animal sources (33%) compared to those in the control group (16%). “After an average of 11.8 years of follow-up – and after adjustment for other risk factors for heart disease, such as diabetes, high blood pressure, obesity, and smoking – people on an LCHF diet had more than two times higher risk of having several major cardiovascular events, such as blockages in the arteries that needed to be opened with stenting procedures, heart attack, stroke, and peripheral arterial disease.” Their press release also cautioned that their study “can only show an association between the diet and an increased risk for major cardiac events, not a causal relationship,” because it was an observational study, but their findings are worth further investigation, “especially when approximately 1 in 5 Americans report being on a low-carb, keto-like or full keto diet.”
I have to say that I find these findings not in the slightest bit surprising and would fully expect the relationship to be causal. The current craze for this diet is concerning and we need to warn consumers that they might be doing themselves considerable harm.
Other authors have recently pointed out that, within the first 6-12 months of initiating the keto diet, transient decreases in blood pressure, triglycerides, and glycosylated hemoglobin, as well as increases in HDL and weight loss may be observed. However, the aforementioned effects are generally not seen after 12 months of therapy. Despite the diet’s favorable effect on HDL-C, the concomitant increases in LDL-C and very-low-density lipoproteins (VLDL) may lead to increased cardiovascular risks. And another team of researchers has warned that “given often-temporary improvements, unfavorable effects on dietary intake, and inadequate data demonstrating long-term safety, for most individuals, the risks of ketogenic diets may outweigh the benefits.”
In this retrospective matched-cohort study, Chinese researchers investigated the association of acupuncture treatment for insomnia with the risk of dementia. They collected data from the National Health Insurance Research Database (NHIRD) of Taiwan to analyze the incidence of dementia in patients with insomnia who received acupuncture treatment.
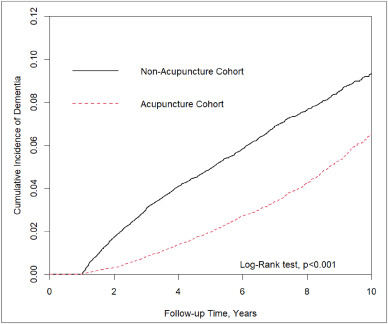
The study included 152,585 patients, selected from the NHIRD, who were newly diagnosed with insomnia between 2000 and 2010. The follow-up period ranged from the index date to the date of dementia diagnosis, date of withdrawal from the insurance program, or December 31, 2013. A 1:1 propensity score method was used to match an equal number of patients (N = 18,782) in the acupuncture and non-acupuncture cohorts. The researchers employed Cox proportional hazards models to evaluate the risk of dementia. The cumulative incidence of dementia in both cohorts was estimated using the Kaplan–Meier method, and the difference between them was assessed through a log-rank test.
Patients with insomnia who received acupuncture treatment were observed to have a lower risk of dementia (adjusted hazard ratio = 0.54, 95% confidence interval = 0.50–0.60) than those who did not undergo acupuncture treatment. The cumulative incidence of dementia was significantly lower in the acupuncture cohort than in the non-acupuncture cohort (log-rank test, p < 0.001).
The researchers concluded that acupuncture treatment significantly reduced or slowed the development of dementia in patients with insomnia.
They could be correct, of course. But, then again, they might not be. Nobody can tell!
As many who are reading these lines know: CORRELATION IS NOT CAUSATION.
But if acupuncture was not the cause for the observed differences, what could it be? After all, the authors used clever statistics to make sure the two groups were comparable!
The problem here is, of course, that they can only make the groups comparable for variables that were measured. These were about 20 parameters mostly related to medication intake and concomitant diseases. This leaves a few hundred potentially relevant variables that were not quantified and could thus not be accounted for.
My bet would be lifestyle: it is conceivable that the acupuncture group had acupuncture because they were generally more health-conscious. Living a relatively healthy life might reduce the dementia risk entirely unrelated to acupuncture. According to Occam’s razor, this explanation is miles more likely that the one about acupuncture.
So, what this study really demonstrates or implies is, I think, this:
- The propensity score method can never be perfect in generating completely comparable groups.
- The JTCM publishes rubbish.
- Correlation is not causation.
- To establish causation in clinical medicine, RCTs are usually the best option.
- Occam’s razor can be useful when interpreting research findings.
I had all but forgotten about these trials until a comment by ‘Mojo’ (thanks Mojo!) reminded me of this article in the JRSM by M.E. Dean. It reviewed these early trials of homeopathy back in 2006. Here are the crucial excerpts:
The homeopath in both trials was a Dr Herrmann, who received a 1-year contract in February 1829 to test homeopathy with the Russian military.3 The first study took place at the Military Hospital in the market town of Tulzyn, in the province of Podolya, Ukraine.4 At the end of 3 months, 164 patients had been admitted, 123 pronounced cured, 18 were convalescing, 18 still sick, and six had died. The homeopathic ward received many gravely ill patients, and the small number of deaths was shown at autopsy to be due to advanced gross pathologies. The results were interesting enough for the Russian government to order Herrmann to the Regional Military Hospital at St Petersburg to take part in a larger trial, supervised by a Dr Gigler. Patients were admitted to an experimental homeopathic ward, for treatment by Herrmann, and comparisons were made with the success rate in the allopathic wards, as happened in Tulzyn. The novelty was Gigler’s inclusion of a ‘no treatment’ ward where patients were not subject to conventional drugging and bleeding, or homeopathic dosing. The untreated patients benefited from baths, tisanes, good nutrition and rest, but also:
‘During this period, the patients were additionally subjects of an innocent deception. In order to deflect the suspicion that they were not being given any medicine, they were prescribed pills made of white breadcrumbs or cocoa, lactose powder or salep infusions, as happened in the homeopathic ward.’3 (page 415)
The ‘no treatment’ patients, in fact, did better than those in both the allopathic and homeopathic wards. The trial had important implications not just for homeopathy but also for the excessive allopathic drugging and bleeding that was prevalent. As a result of the report, homeopathy was banned in Russia for some years, although allopathy was not.
… A well-known opponent of homeopathy, Carl von Seidlitz, witnessed the St Petersburg trial and wrote a hostile report.5 He then conducted a homeopathic drug test in February 1834 at the Naval Hospital in the same city in which healthy nursing staff received homeopathically-prepared vegetable charcoal or placebo in a single-blind cross-over design.6 Within a few months, Armand Trousseau and colleagues were giving placebo pills to their Parisian patients; perhaps in the belief that they were testing homeopathy, and fully aware they were testing a placebo response.7,8 A placebo-controlled homeopathic proving took place in Nuremberg in 1835 and even included a primitive form of random assignment—identical vials of active and placebo treatment were shuffled before distribution.9 Around the same time in England, Sir John Forbes treated a diarrhoea outbreak after dividing his patients into two groups: half received allopathic ‘treatment as usual’ and half got bread pills. He saw no difference in outcome, and when he reported the experiment in 1846 he added that the placebos could just as easily have been homeopathic tablets.10 In 1861, a French doctor gave placebo pills to patients with neurotic symptoms, and his attitude is representative: he called the placebo ‘orthodox homeopathy’, because, as he said, ‘Bread pills or globules of Aconitum 30c or 40c amount to the same thing’.11
References:
A recent article in ‘The Lancet Regional Health‘ emphasized the “need for reimagining India’s health system and the importance of an inclusive approach for Universal Health Coverage” by employing traditional medicine, including homeopathy. This prompted a response by Siddhesh Zadey that I consider worthy of reproducing here in abbreviated form:
… Since the first trial conducted in 1835 that questioned homeopathy’s efficacy, multiple randomized controlled trials (RCTs) and other studies compiled in several systematic reviews and meta-analyses have shown that there is no reliable and clinically significant effect of non-individualized or individualized homeopathic treatments across disease conditions ranging from irritable bowel syndrome in adults to acute respiratory tract infections in children when compared to placebo or other treatments. Even reviews that support homeopathy’s efficacy consistently caution about low quality of evidence and raise questions on its clinical use. The most recent analysis of reporting bias in homeopathic trials depicted problematic trial conduction practices that further obscure reliability and validity of evidence. Homeopathic treatments have also been linked to aggravations and non-fatal and fatal adverse events.
The Lancet has previously published on another kind of harm that uptake of homeopathy encourages in India: delay to evidence-based clinical care that can lead to fatality. Authors have pointed out that evidence for some of the alternative systems of medicine may not come from RCTs. I agree that more appropriate study designs and analytical techniques are needed for carefully studying individualized treatment paradigms. However, the need for agreement on some consistent form of evidence synthesis and empirical testing across diverse disciplines cannot be discounted. Several other disciplines including psychology, economics, community health, implementation science, and public policy have adopted RCTs and related study designs and have passed the empirical tests of efficacy. Moreover, the ideas around mechanism of action in case of homeopathy still remain controversial and lack evidence after over a century. On the contrary, biochemical, molecular, and physiological mechanistic evidence supporting allopathic treatments has grown abundantly in the same period.
Owing to lack of evidence on its efficacy and safety, the World Health Organization had previously warned against the use of homeopathic treatments for severe diseases. Additionally, multiple countries, including Germany where the practice originated, have initiated mechanisms that discourage uptake of homeopathy while others are considering banning it. Homeopathy doesn’t work, could be harmful, and is not a part of Indian traditional medicine. While we should welcome pluralistic approaches towards UHC, we need to drop homeopathy.
(for references, see original text)
___________________
Yes, in the name of progress and in the interest of patients, “we need to drop homeopathy” (not just in India but everywhere). I quite agree!
This systematic review and meta-analysis aimed to evaluate the effectiveness and safety of Chinese herbal medicine (CHM) combined with Western medicine (WM) in comparison with WM in reducing systolic and diastolic blood pressure for patients with primary hypertension (PHTN).
Various literature searches located a total of 29 studies that included 2623 patients. The results showed that the clinical effectiveness in the treatment of hypertension with CHM+WM was considerably higher than that with WM alone, clinical effective (RR 1.23, 95% CI [1.17, 1.30], P < 0.00001), and markedly effective (ME) in the patients (RR 1.66, 95% CI [1.52, 1.80], and P < 0.00001). Random effect in SBP (MD 7.91 mmHg,[6.00, 983], P < 0.00001) and DBP (MD 5.46 mmHg, [3.88, 6.43], P < 0.00001), a subgroup analysis was carried out based on the type of intervention, duration of treatment, and CHM formulas that showed significance. Furthermore, no severe side effects were reported, and no patients stopped treatment or withdrawal due to any severe adverse events.
The authors concluded that compared to WM alone, the therapeutic effectiveness of CHM combined with WM is significantly improved in the treatment of hypertension. Additionally, CHM with WM may safely and efficiently lower systolic blood pressure (SBP) and diastolic blood pressure (DBP) in individuals with PHTN. However, rigorous randomized controlled trials with a large sample, high quality, long duration of treatment, and follow-up are recommended to strengthen this clinical evidence.
The authors can boast of an impressive list of affiliations:
- 1Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China; School of Pharmacy, Lebanese International University, 18644, Sana’a, Yemen.
- 2Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China.
- 3Key Laboratory of Chinese Materia Medica, Ministry of Education of Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China.
- 4Department of Urology, Affiliated Hospital of Qingdao Binhai University, Qingdao, Shandong, China.
- 5Department of Respiratory Diseases, Shandong Second Provincial General Hospital, Shandong University, Shandong, China.
- 6Heilongjiang University of Chinese Medicine, Harbin, 150040, Heilongjiang, China. Electronic address: [email protected].
Impressive in the sense of being impressively prone to bias, particularly knowing that ~80% of Chinese research findings have been shown to be fabricated and considering that Chinese authors as good as never publish anything negative about TCM.
But perhaps you still believe that the results reported here are 100% true? In this case, I might even agree with you. The reason is that the authors demonstrate in exemplary fashion what I have been saying so often before:
Blood pressure is one of the many endpoints that are highly prone to placebo effects. Therefore, even the addition of an ineffective CHM to WM would lower blood pressure more effectively than WM alone.
But there is a third way of explaining the findings of this review: some herbal remedies might actually have a hypotensive effect. The trouble is that this review does come not even close to telling us which.
Remember the Bavarian Homeopathy Study? I reported about it only a few days ago. Now the ‘German Homeopathic Doctors Association’ has published an interview with someone who allegedly knows more about it. Here is my translation:
Dr. Springer, what does it actually mean politically that this study came about at all?
First of all, it means that the work of several years was worthwhile and that we were able to convince those responsible with a carefully elaborated study design. It also shows how enormously important it is to have solid political contacts with parties, MPs, parliamentary groups, and spokespersons in health committees. In addition to persuasion, personal credibility and professional competence are indispensable for the growth of such contacts. This is also shown by the fact that LIMed (List of Integrative Medicine) in Bavaria (as in some other federal states) has succeeded in sending committed colleagues to the representations of the State Medical Association and the Medical District and County Association.
What is special about this study?
As far as I know, it is the first study worldwide to be carried out with hand-shaken high potencies (C 200 and C 1000). If the results were positive, the mechanism of action of homeopathy would not be clarified, but it would be proven that highly potentised medicinal substances have a healing effect that can be objectified scientifically.
Who is the sponsor of this study?
The Bavarian Parliament voted with an absolute majority to scientifically investigate the role of complementary medicine in the fight against increasing antibiotic resistance. Several study designs were submitted on this question, and our study approach won the bid in the end. The Bavarian State Ministry of Health and Care is financing the study and has won the Technical University of Munich as a partner – after all, it is one of Germany’s universities of excellence. This removes all doubts about the correct scientific conduct of the study.
What is to be investigated in the study?
It relates to a diagnosis with great relevance to healthcare: Women often suffer from recurrent urinary tract infections, which are often treated with antibiotics. This is always associated with the risk of causative bacteria developing resistance to antibiotics. As homeopathically qualified doctors, we know from decades of experience that we can reduce and even end the frequency of recurrent urinary tract infections and their occurrence with our homeopathic remedies. We want to put this experience to the test scientifically with this study.
How do you see the chances for a positive study result?
As doctors, we know what we do and what we can do. We will do everything in our power to show that we can do it! I would also like to take this opportunity to thank all those who have made this study possible and who are providing us with professional and scientific support!-
The interview was conducted by Ulf Riker, MD.
___________________________
The interview raises several questions:
- Dr. Springer confirms that the existence of the study and its financial support is mostly due to political influence. Is this how good science should be generated?
- Is it true that the study is the first to investigate potency homeopathy? Considering that the bestselling homeopathic, Oscillococcinum, is sold in the C200 potency, this seems to be a very questionable statement.
- If the results were to come out positive, would we really re-write the textbooks of physics and chemistry which state that the absence of an active molecule cannot have an effect?
- Does the involvement of the Technical University truly remove all doubts about the correct scientific conduct of the study?
- If the homeopathically qualified doctors conducting the study already claim to know from decades of experience that they can reduce and even end the frequency of recurrent urinary tract infections with homeopathic remedies, are they not going to be too biased in conducting such a study?
- If the trialists are determined to do everything in their power to show that homeopathy works, will the study generate a reliable result?
- My last question is, how reliable is Dr. Springer? I found another interview of him dated 2021. In it he stated about the homeopathic treatment of COVID patients: ” [There is a} group of Covid-19 patients … [to] whose successful treatment we as homeopathic physicians can certainly contribute. The symptomatology of these patients is considerable, sometimes severe, but not life-threatening. They suffer from headaches and pain in the limbs, dizziness, fever, have the often-quoted “dry cough”, sweat, and usually feel very weak. But they have not yet developed clinical symptoms of pneumonia. These patients – and they are by no means few – can be helped by medical homeopathy, I am firmly convinced, curatively. Provided, of course, that a very precise, individual homeopathic anamnesis is carried out, the patient is closely followed, the course of the disease is closely observed and the remedy administered is adjusted if necessary. By preventing an acute condition and hospitalization in these patients homeopathy could make a not inconsiderable contribution to overcoming these greatest health and social challenges in one hundred years.” That, I think might answer my question.
As I pointed out before, the study design looks rigorous. After reading this interview, I have my doubts that its execution will be rigorous as well.
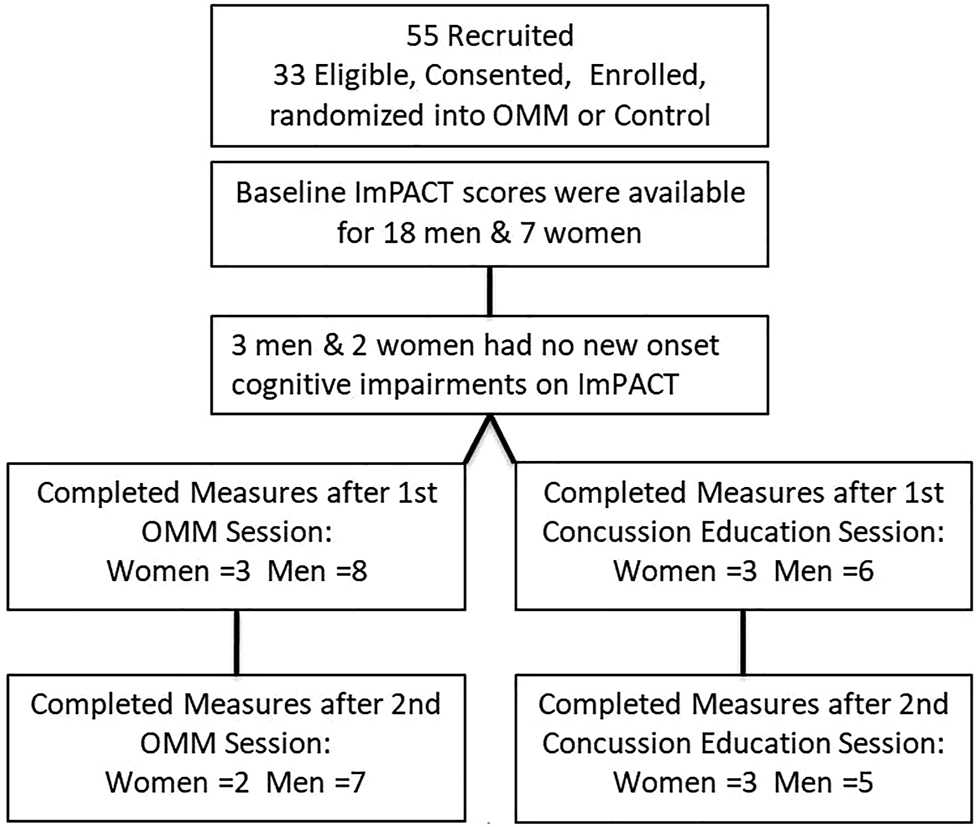
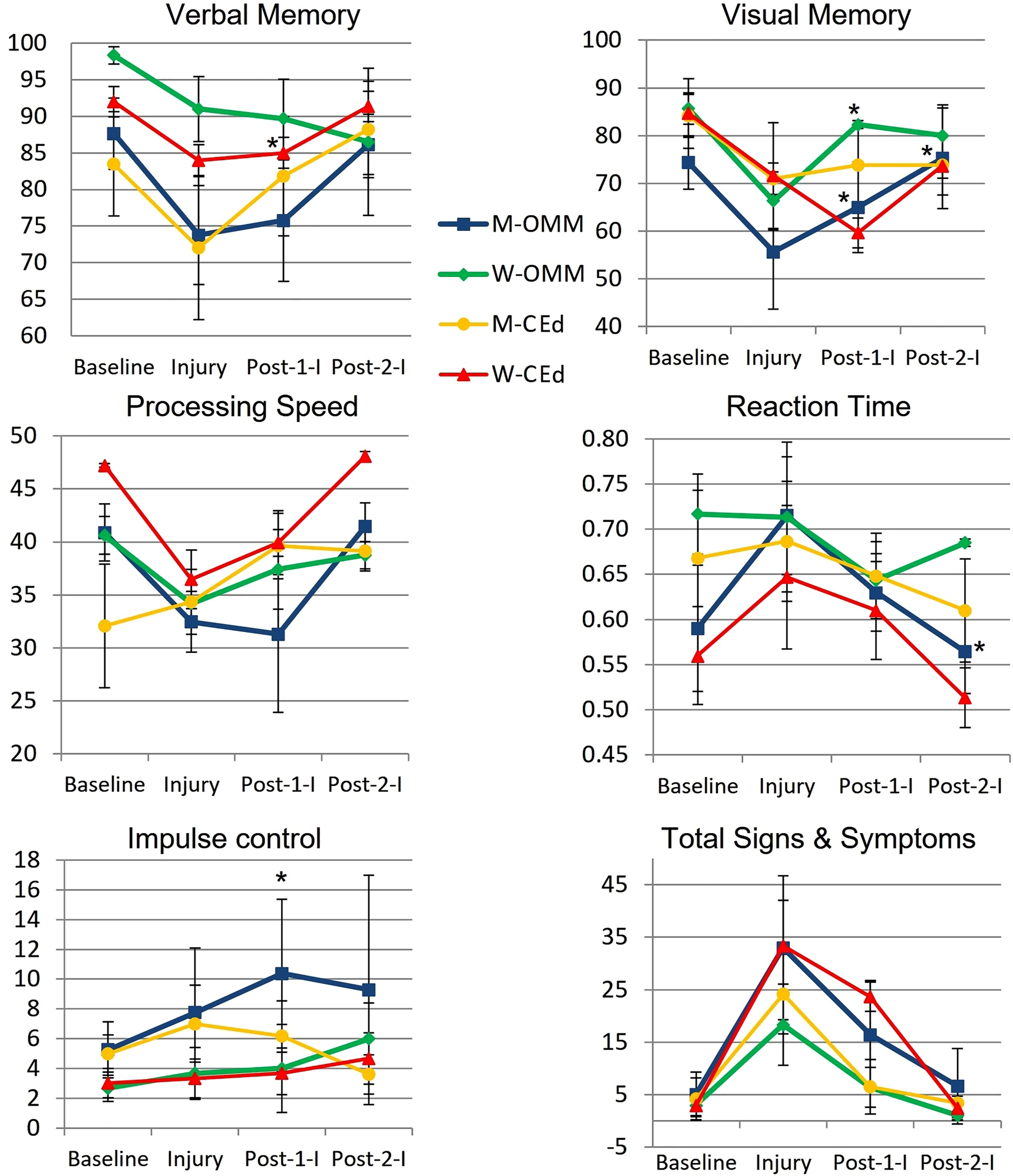
This study from the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine tested whether new-onset impairments (NOI) of neurological functions identified by Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) will improve more so after osteopathic manipulative medicine (OMM) than after concussion-education.
College athletes presenting to the outpatient academic healthcare center (AHCC) with concussion due to head injury within the preceding 2 weeks were recruited for this IRB-approved, randomized, single-blinded trial. Consented men and women were randomized into two groups:
- the verum group received two OMM treatments;
- the control group received two concussion-education sessions.
Preseason, Baseline, ImPACT was compared to Post-Injury scores to determine NOI. Baseline, Post-Injury, and Post-Interventions ImPACTs were compared by analysis of variance (ANOVA, α≤0.05). Post-Injury correlations and mean changes in King-Devick (KD) scores were analyzed.
Post-Injury NOI were found in 77.8% (14/18) men and 85.7% (6/7) women, including ImPACT subscore indices for verbal and visual memory, processing speed (PS), and reaction time (RT). Of those with NOI, mean visual memory recovered by 50.0% following one and by 104.9% (p=0.032) following two OMM treatments in men and by 82.8% (p=0.046) following one treatment in women. Following two interventions, the mean RT in men receiving OMM improved by 0.10 more than education (p=0.0496). The effect sizes of OMM were large (Cohen’s d=1.33) on visual memory and small (Cohen’s d=0.31) on RT.
The authors concluded that NOI in visual memory and RT following concussion significantly improved in the OMM group compared to the education group. Integrating OMM utilizing physical exam and this treatment was a safe individualized approach in athletes with acute uncomplicated concussions. Further research is warranted to improve the utilization of OMM for individuals with concussion.
What the abstract does not tell you is that the two groups were extremely small and that they became even smaller, as some patients were lost to follow-up.
In addition, the results were all over the place.
Furthermore, it is noteworthy that neither the therapists nor the patients were blinded and the observation period was short. Finally, the authors state in their conclusions that OMM is safe. Considering the sample size and the attrition rate (perhaps all those patients lost to follow-up died?), this is of course ridiculously wishful thinking.
So, what can we conclude from this study? I don’t know about you, but I conclude that the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine could do with a good science teacher.
Konjac glucomannan (KGM), also just called ‘glucomannan’, is a dietary fiber hydro colloidal polysaccharide isolated from the tubers of Amorphophallus konjac. It is used as a food, a food additive, as well as a dietary supplement in many countries. KGM is claimed to reduce the levels of glucose, cholesterol, triglycerides, and blood pressure.
The objective of this study was to evaluate the effect of the consumption of gummy candy enriched with KGM on appetite and to evaluate anthropometric data, biochemical, and oxidative stress markers in overweight individuals. Forty-two participants aged 18 to 45 years completed this randomized, double-blind, placebo-controlled clinical trial. Participants were randomly assigned to consume for 14 days, 2 candies per day, containing 250 mg of KGM or identical-looking placebo candy with 250 mg of flaxseed meal, shortly after breakfast and dinner. As a result, we observed that there was a reduction in waist circumference and in the intensity of hunger of the participants who consumed KGM. The authors believe that a longer consumption time as well as an increased dose of KGM would contribute to even more satisfactory body results.
These findings seem promising, yet somehow I am not convinced. The study was small and short-term; moreover, the authors seem uncritical and, instead of a conclusion, they offer speculations.
Our own review of 2014 included 9 clinical studies. There was a variation in the reporting quality of the included RCTs. A meta-analysis (random effect model) of 8 RCTs revealed no significant difference in weight loss between glucomannan and placebo (mean difference [MD]: -0.22 kg; 95% confidence interval [CI], -0.62, 0.19; I(2) = 65%). Adverse events included abdominal discomfort, diarrhea, and constipation. We concluded that the evidence from available RCTs does not show that glucomannan intake generates statistically significant weight loss. Future trials should be more rigorous and better reported.
Rigorous trials are required to change my mind, and I am not sure that the new study falls into this category.
If you think that scanning through dozens of new scientific articles every week is a dry and often somewhat tedious exercise, you are probably correct. But every now and then, this task is turned into prime entertainment by some pseudoscientists trying to pretend to be scientists. Take, for instance, the latest homeopathy study by Indian researchers with no less than 9 seemingly impressive affiliations:
- 1Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 2Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE, Sector III, Salt Lake, Kolkata, West Bengal, India.
- 3Department of Homoeopathy, State Homoeopathic Dispensary, Karaila, Pratapgarh, Uttar Pradesh, India.
- 4Department of Homoeopathy, State Homoeopathic Dispensary, Tulsipur, Shrawasti, Uttar Pradesh, India.
- 5Department of Materia Medica, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 6State Homoeopathic Dispensary, Mangalbari Rural Hospital, Matiali Block, Jalpaiguri, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 7Department of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 8Department of Homoeopathy, East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre, Village and Post Office: Gouripur (South), Police Station Bishnupur, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 9Department of Repertory, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
Now that I have whetted your appetite, here is their study:
Lumbar spondylosis (LS) is a degenerative disorder of the lumbar spine. Despite substantial research efforts, no gold-standard treatment for LS has been identified. The efficacy of individualized homeopathic medicines (IHMs) in lumbar spondylosis (LS) is unknown. In this double-blind, randomized, placebo-controlled trial, the efficacy of IHMs was compared with identical-looking placebos in the treatment of low back pain associated with LS. It was conducted at the National Institute of Homoeopathy, West Bengal, India.
Patients were randomized to receive IHMs or placebos; standardized concomitant care was administered in both groups. The Oswestry low back pain and disability questionnaire (ODQ) was used as the primary outcome measure; the Roland-Morris questionnaire (RMQ) and the short form of the McGill pain questionnaire (SF-MPQ) served as secondary outcome measures. They were measured at baseline and every month for 3 months. Intention-to-treat analyses (ITT) were used to detect any inter-group differences using two-way repeated measures analysis of variance models overall and by unpaired t-tests at different time points.
Enrolment was stopped prematurely because of time restrictions; 55 patients had been randomized (verum: 28; control: 27); 49 could be analyzed by ITT (verum: 26; control: 23).
The results are as follows:
- Inter-group differences in ODQ (F 1, 47 = 0.001, p = 0.977), RMQ (F 1, 47 = 0.190, p = 0.665) and SF-MPQ total score (F 1, 47 = 3.183, p = 0.081) at 3 months were not statistically significant.
- SF-MPQ total score after 2 months (p = 0.030) revealed an inter-group statistical significance, favoring IHMs against placebos.
- Some of the SF-MPQ sub-scales at different time points were also statistically significant: e.g., the SF-MPQ average pain score after 2 months (p = 0.002) and 3 months (p = 0.007).
- Rhus Toxicodendron, Sulphur, and Pulsatilla nigricans were the most frequently indicated medicines.
The authors concluded that owing to failure in detecting a statistically significant effect for the primary outcome and in recruiting a sufficient number of participants, our trial remained inconclusive.
Now that I (and hopefully you too) have recovered from laughing out loud, let me point out why this paper had me in stitches:
- The trial was aborted not because of a “time limit” but because of slow recruitment, I presume. The question is why were not more patients volunteering? Low back pain with LS is extremely common. Could it be that patients know only too well that homeopathy does not help with low back pain?
- If a trial gets aborted because of very low patient numbers, it is probably best not to publish it or at least not to evaluate its results at all.
- If the researchers insist on publishing it, their paper should focus on the reason why it did not succeed so that others can learn from their experience by avoiding their mistakes.
- However, once the researchers do run statistical tests, they should be honest and conclude clearly that, because the primary outcome measure showed no inter-group difference, the study failed to demonstrate that the treatment is effective.
- The trial did not “remain inconclusive”; it was squarely negative.
- The editor of the journal HOMEOPATHY should know better than to publish such nonsense.
A final thought: is it perhaps the ultimate proof of homeopathy’s ‘like cures like’ assumption to use sound science (i.e. an RCT), submit it to the homeopathic process of endless dilutions and succussions, and – BINGO – generate utter nonsense?
This prospective study aimed to identify an optimal lifestyle profile to protect against memory loss in older individuals from areas representative of the north, south, and west of China. Individuals aged 60 years or older who had normal cognition and underwent apolipoprotein E (APOE) genotyping at baseline in 2009 were included. Participants were followed up until death, discontinuation, or 26 December 2019.
Six lifestyle factors were assessed:
- a healthy diet (adherence to the recommended intake of at least 7 of 12 eligible food items),
- regular physical exercise (≥150 min of moderate intensity or ≥75 min of vigorous intensity, per week),
- active social contact (≥twice per week),
- active cognitive activity (≥twice per week),
- never or previously smoked,
- never drinking alcohol.
Participants were categorised into the favourable group if they had 4-6 healthy lifestyle factors, into the average group for two to three factors, and into the unfavourable group for zero to one factor.
Memory function was assessed using the World Health Organization/University of California-Los Angeles Auditory Verbal Learning Test, and global cognition was assessed via the Mini-Mental State Examination. Linear mixed models were used to explore the impact of lifestyle factors on memory in the study sample.
A total of 29 072 participants were included (mean age of 72.23 years; 48.54% (n=14 113) were women; and 20.43% (n=5939) were APOE ε4 carriers). Over the 10-year follow-up period (2009-19), participants in the favourable group had slower memory decline than those in the unfavourable group (by 0.028 points/year, 95% confidence interval 0.023 to 0.032, P<0.001). APOE ε4 carriers with favourable (0.027, 95% confidence interval 0.023 to 0.031) and average (0.014, 0.010 to 0.019) lifestyles exhibited a slower memory decline than those with unfavourable lifestyles. Among people who were not carriers of APOE ε4, similar results were observed among participants in the favourable (0.029 points/year, 95% confidence interval 0.019 to 0.039) and average (0.019, 0.011 to 0.027) groups compared with those in the unfavourable group. APOE ε4 status and lifestyle profiles did not show a significant interaction effect on memory decline (P=0.52).
The authors concluded that a healthy lifestyle is associated with slower memory decline, even in the presence of the APOE ε4 allele. This study might offer important information to protect older adults against memory decline.
This is an important and meticulously reported study. It is the first large-scale investigation that assesses the effects of different lifestyle profiles, APOE ε4 status, and their interactions on longitudinal memory trajectories over a 10-year follow-up period. The results show that lifestyle is associated with the rate of memory decline in cognitively normal older individuals, including in people who are genetically susceptible to memory decline. The authors are rightly careful to avoid causal inferences between lifestyle and memory decline. To demonstrate causality beyond doubt, we would need different study designs.
The authors also discuss several weaknesses of the study:
- Firstly, the assessments of lifestyle factors were based on self-reports and are, therefore, prone to measurement errors.
- Secondly, several participants were excluded due to missing data or not returning for follow-up evaluations, which might have led to selection bias.
- Thirdly, the proportion of individuals with an unhealthy lifestyle might have been underestimated in the study because people with poor health were less likely to have participated in the study.
- Fourthly, given the nature of the study design, it could not assess whether maintaining a healthy lifestyle had already started influencing memory by the time of enrolment in the study.
- Fifthly, the evaluation of memory using a single neuropsychological test that does not comprehensively reflect overall memory function. However, the Auditory Verbal Learning Test is an effective instrument for memory assessment, and a composite score was used based on four Auditory Verbal Learning Test subscales to represent memory conditions to the greatest extent possible.
- Sixthly, as participants might become familiar with repeated cognitive testing, a learning effect could have influenced the results.
- Finally, memory decline was studied solely among older adults; however, memory problems commonly affect young individuals as well.
The authors, therefore, state that further studies should be conducted to facilitate a more extensive investigation into the effects of a healthy lifestyle on memory decline across the lifespan. This approach would help to elucidate the crucial age window during which a healthy lifestyle can exert the most favourable effect.