legal action
In a video, Mr.Darkmoore speaks from a hospital bed and says the cause behind his visit to the emergency room stemmed from a chiropractor’s work on him. Three days ago, he had a ringing in his ear due to a long-term condition he knew as tinnitus. Thus, he decided to visit a chiropractor. “I figured $100 to a chiro, let them adjust a few things, if all else fails, I’ll go to a doctor,” explains Darkmoore.
This $100 visit led to several other complications and doctor’s bills worth thousands of dollars. The day after he was treated by the chiropractor, he experienced a headache that eventually led to dizzy spells. He decided to visit the emergency room where a CT scan was ordered which showed that the chiropractor had dissected an artery in his neck.
Next, Darkmoore was put on blood thinners to avoid blood clots that could result in a stroke or worse. Darkmoore explains that he will be on two blood thinners for the next three months to prevent clotting. If the dissection heals partially, he says he will need to take aspirin every day for the rest of his life. If it doesn’t heal, he claims that he will need surgery.
Many viewers of the video claimed they have had the same “chiropractor gone wrong” experience as Darkmoore.
- “Wow. How scary. I had a similar thing happen to me. Extremely bad headache after going one time. Haven’t gone since,” one commenter wrote.
- “I’m so sorry this happened to u,” another user echoed. “My chiropractor also caused an injury which required emergency surgery & I have permanent damage. I’m glad u survived.”
Darkmore captioned his last update video, “I appreciate the thoughts and prayers. Hopefully, I’ll be okay after 3 months of recovery.”
__________________
Let’s hope that he is correct and that he will make a speedy and full recovery.
Of course, chiros will queue up to stress that important details are missing in this case report. To them, I would merely say this:
THERE IS NO GOOD EVIDENCE THAT NECK MANIPULATIONS BRING ANY BENEFIT AND QUITE A BIT OF EVIDENCE THAT THEY CAN CAUSE SERIOUS HARM.
SO, WHY NOT JUST STOP OFFERING THE PROCEDURE?
We have discussed dental amalgam and its risks to human health before. Finally, there is new legislation in sight. The European Commission has revised the EU Mercury Regulation to protect EU citizens and the environment from toxic mercury. Among other things, this will completely ban the use of dental amalgam, for which 40 tons of mercury are currently consumed annually in the EU. The revised mercury ordinance provides for the following:
– No more use of dental amalgam from January 1, 2025; viable mercury-free alternatives are available.
– Ban on the manufacture and export of dental amalgam from the EU from January 1, 2025;
– Ban on the manufacture and export of six mercury-containing lamps from January 1, 2026 and January 1, 2028 (depending on lamp type).
The delegated act adopted under the Mercury Regulation transposes into EU law the decisions taken at the fourth Conference of the Parties (2022) to the Minamata Convention by introducing a ban on the production, import, and export of eight additional mercury-containing products, including mercury-containing lamps and non-electrical equipment.
The Minamata Convention is the main international legal framework for the protection of human health and the environment from anthropogenic emissions and releases of mercury to air, water, and soil. Like the Mercury Regulation, it addresses the entire life cycle of mercury, from primary mercury mining to mercury waste management.
The revised Mercury Regulation must now be approved by the European Parliament and the Council under the ordinary legislative procedure. The delegated act will be sent to the European Parliament and the Council for consideration.
Mercury is a highly toxic chemical that poses a threat to both human health and the environment. When released into the environment, it enters the food chain where it accumulates (mainly in fish). High mercury exposure can damage the brain, lungs, kidneys, and immune system.
Historically, mercury has been used in a wide range of applications, including gold mining, batteries, fluorescent tubes, thermometers, and barometers. Over the last twenty years, the EU has developed a comprehensive body of legislation, in particular the Mercury Regulation, which protects human health and the environment from anthropogenic emissions and releases of mercury, taking into account the entire life cycle of mercury from primary mercury mining to final disposal of mercury waste. It also includes measures on trade in mercury-containing products and mercury pollution.
The Minamata Convention entered into force on August 16, 2017, and has so far been ratified by the European Union and 143 countries, including all EU Member States. The fifth session of the Conference of the Parties to the Minamata Convention on Mercury (COP-5) will be held in Geneva, Switzerland, from October 30 to November 3, 2023.
_____________________________
The U.S. Department of Health and Human Services alleges that Jason James of the James Healthcare & Associates clinic in Iowa, USA — along with his wife, Deanna James, the clinic’s co-owner and office manager — filed dozens of claims with Medicare for a disposable acupuncture device, which is not covered by Medicare, as if it were a surgically implanted device for which Medicare can be billed. According to the lawsuit, more than 180 such claims were filed. Beginning in 2016, the lawsuit alleges, the clinic began offering an electro-acupuncture device referred to as a “P-Stim.” When used as designed, the P-Stim device is affixed behind a patient’s ear using an adhesive. The device delivers intermittent electrical pulses through a single-use, battery-powered attachment for several days until the battery runs out and the device is thrown away.
Because Medicare does not reimburse medical providers for the use of such devices, DHHS alleges that some doctors and clinics have billed Medicare for the P-Stim device using a code number that only applies to a surgically implanted neurostimulator. The use of an actual neurostimulator is reimbursed by Medicare at approximately $6,000 per claim, while P-Stim devices were purchased by the Keokuk clinic for just $667, DHHS alleges. The department alleges James knew his billings were fraudulent as the P-Stim device is “nowhere close to even resembling genuine implantable neurostimulators” and does not require surgery.
The lawsuit alleges that on June 15, 2016, when Jason James was contemplating the use of P-Stim devices at the Keokuk clinic, he sent a text message to P-Stim sales representative Mark Kaiser, asking, “Is there a limit on how many Neurostims can be done on one day? Don’t wanna do so many that gives Medicare a red flag on first day. Thanks.” After realizing the “large profit windfall” that could result from the billing practice, DHHS’s lawsuit alleges, James “told Mark Kaiser not to mention the Medicare reimbursement rate to his nurse practitioner or staff – only his office manager and biller needed that information.” James then pressured clinic employees to heavily market the P-Stim devices to patients, even if those patients were not agreeable or, after trying it, were reluctant to continue the treatment, the lawsuit claims.
In October 2016, the clinic’s supplier of P-Stim devices sent the clinic an email stating the company had “no position on what the proper coding might be for this device if billed to a third-party payer” such as an insurer or Medicare, according to the lawsuit. The company advised the clinic to “consult a certified biller/coder and/or attorney to ensure compliance.” According to the lawsuit, James then sent Kaiser a text message asking, “Should we be concerned?”
DHHS alleges the clinic’s initial reimbursement claims were submitted to Medicare through a nurse practitioner and were denied for payment due to the lack of a trained physician’s involvement. In response, the clinic hired Dr. Robert Schneider, an Iowa-licensed physician, to work at the clinic for the sole purpose of enabling James Healthcare & Associates to bill Medicare for the P-Stim devices, the lawsuit claims. James then informed Kaiser he had a goal of billing Medicare for 20 devices per month, which would generate roughly $125,573 of monthly income, the lawsuit alleges. The lawsuit also alleges Dr. Schneider rarely saw clinic patients in person, consulting with them instead through Facebook Live.
In April 2017, Medicare allegedly initiated a review of the clinic’s medical records, triggering additional communications between James and Kaiser. At one point, James allegedly wrote to Kaiser and said he had figured out why Medicare was auditing the clinic. “Anything over $7,500 is automatically audited for my area,” he wrote, according to the lawsuit. “We are now charging $7,450 to remove the audit.”
The clinic ultimately submitted 188 false claims to Medicare seeking reimbursement for the P-Stim devices, DHHS alleges, with Medicare paying out $4,100 and $6,300 per claim, for a total loss of $1,028,800. DHHS is suing the clinic under the federal False Claims Act and is seeking trebled damages of more than $3 million, plus a civil penalty of up to $4.2 million.
An attorney for the clinic, Michael Khouri, said Wednesday he believe the federal government’s lawsuit was filed in error because a settlement in the case had already been reached. However, the assistant U.S. attorney handling the case said no settlement in the case had been finalized and the lawsuit was not filed in error.
Previous legal cases
In 2015, the Iowa Board of Chiropractic charged Jason James with knowingly making fraudulent or untrue representations in connection with his practice, engaging in conduct that was harmful or detrimental to the public, and making untruthful statements in advertising. The board alleged James told patients they would be able to stop taking diabetes medication through the use of a diet and nutrition program, and that he had claimed to be providing extensive laboratory tests when not all of the tests for which he billed were ever conducted. The board also claimed James referred patients to a medical professional who was not licensed to practice in Iowa. The case was resolved with a settlement agreement in which James agreed to pay a $500 penalty and complete 10 hours of education in marketing and ethics.
In 2019, Schneider sued the clinic for failing to comply with the terms of his employment agreement. Court exhibits indicate the agreement stipulated that Schneider was to work no more than two days per month and would collect $2,000 for each day worked, plus $250 per month for consulting, plus “$250 per device over six per calendar month.” In March 2020, a jury ruled in favor of the clinic and found that it had not breached its employment agreement with Schneider.
_________________________
Before some chiropractors now claim that such cases represent just a few rotten apples in a big basket of essentially honest chiropractors, let me remind them of a few previous posts:
- A $2.6M Insurance Fraud by Chiropractors and Doctors?
- Fraud and sex offences by chiropractors
- Chiropractic therapy for gastrointestinal diseases. Evidence of scientific misconduct?
- Twenty Things Most Chiropractors Won’t Tell You
- The Dark Side of Chiropractic Care
- Chiropractic subluxation: the myth must be kept alive
- CHIROPRACTIC: an early and delightful critique
- Students of chiropractic condemn the ‘unacceptable behaviour’ of some chiropractors and their professional organisations
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Chiropractor is in the dock for not wearing a mask
- “The uncensored truth” about COVID-19 vaccines” … as told by some chiro loons
To put it bluntly: chiropractic was founded by a crook on a bunch of lies and unethical behavior, so it is hardly surprising that today the profession has a problem with ethics and honesty.
It been reported that the German HEILPRAKTIKER, Holger G. has been sentenced to serve a total of 4 years and three months behind bars. He made himself a pair of glasses out of aluminum foil and appeared at the start of his trial wearing a Corona protective mask. The accusations against him were fierce: He was accused of having issued false Corona vaccination certificates en masse in Munich and of having given medication to patients. A woman, who had contracted Corona and had been treated by Holger G. with vitamin solutions, had died last year.
According to the verdict, Holger G. had violated the German Medicines Act. The court announced he was also convicted of 96 counts of dangerous bodily harm and 102 counts of unauthorized trading in prescription drugs. In addition, the court ordered the HEILPRAKTIKER to be placed in a rehab facility.
The 71-year-old MAN had issued Corona vaccination cards since April 2021, without actually vaccinating the people concerned. For the forged vaccination cards, he charged several tens of thousands of Euros. In addition, the former HEILPRAKTIKER illegally sold prescription drugs. The judgment is so severe because Holger G. has form. He also ordered to bear the costs of the proceedings.
___________________________
I have long criticized the German HEILPRAKTIKER. In my recent book on the subject, I make the following points:
– Today, no one can provide reliable data on the number of HEILPRAKTIKER in Germany.
– The training of HEILPRAKTIKER is woefully inadequate.
– The far-reaching rights of the HEILPRAKTIKER are out of proportion to their overt lack of competence.
– This disproportion poses a serious danger to patients.
– This danger is further increased by the fact that there is no effective control of the activity of the HEILPRAKTIKER does not take place.
– Existing laws are almost never applied to the HEILPRAKTIKER.
– Most HEILPRAKTIKER mislead the public unhindered with untenable therapeutic claims.
– The federal government seems to put off over and over again any serious discussion of the HEILPRAKTIKER.
Cases like the one above show that it is high time for reform – or, should that prove impossible, the discontinuation of this utterly obsolete and highly dangerous profession.
Guest post by Ken McLeod
Readers will have no trouble recalling that crank ‘naturopath’ Barbara O’Neill has graced these pages several times. She is subject to a Permanent Prohibition Order by the New South Wales Health Care Complaints Commission. It goes like this:
“The Commission is satisfied that Mrs O’Neill poses a risk to the health and safety of members of the public and therefore makes the following prohibition order:
“Mrs O’Neill is permanently prohibited from providing any health services, as defined in s4 Of the Health Care Complaints Act 1993, whether in a paid or voluntary capacity.’ 1
Evidently Ms O’Neill has scrambled her chakras or muddled her meridians because she continues to forget the Order. For example;
O’Neill did a video interview concerning the Prohibition Order and that has been posted online at YouTube.2 The video was posted ‘1 year ago,’ has had 323,000 views and had 1,598 comments. She goes into great detail what she regards as the appalling treatment at the hands of the HCCC.
In the video she admits that she has continued to travel the world spreading her lies and misrepresentations. Some of the lies are that she is a naturopath, and was a nurse, and ‘I used to work in the Operating Theatre as a psychiatric nurse….’
In the video at 53:20 in the video she refers to an aboriginal man ‘Dan’ who works at her Misty Mountain Lifestyle Retreat, (note the present tense), who is in his 50s was obese and recently had a heart attack, ‘was on a lot of medications,’ ‘was a bit scared of coming off medications,’ ‘I said Dan, I think it’s time to stop your blood pressure medications, you’re going too low, you’re a 100 over 60,’ ‘three days later his blood pressure was 100 over 75,….’ 3
Call me a cynic, but that strikes me as rather dangerous advice, worthy of an investigation by the HCCC. Meanwhile, there is no sign of ‘Dan ‘ in Misty Mountain’s ‘About page.’ Dan’s brother Dave appears, but no Dan.4 Could it be that O’Neill’s advice led to some incapacity? Tips are welcome.
Meanwhile, readers could learn much more about Barbara O’Neill at Wikipedia.5
This article first appeared in the June issue of the Australian Skeptic Magazine,6 reprinted with kind permission.
REFERENCES
1 https://www.hccc.nsw.gov.au/decisions-orders/public-statements-and-warnings/public-statement-and-statement-of-decision-in-relation-to-in-relation-to-mrs-barbara-o-neill
2 https://www.youtube.com/watch?v=tsbK5TLdAPo
3 This was dangerous and reckless advice. The full transcript is here
4 https://www.mmh.com.au/our-story
5 https://en.wikipedia.org/wiki/Barbara_O%27Neill
6 https://www.skeptics.com.au/magazine/
A German paper reported the following horrific story about a Heilpraktiker, an alternative practitioner without a medical degree:
Starting July 7, Torben K. (46) from Solingen will have to answer to the Wuppertal Regional Court. The Heilpraktiker is said to have injected silicone oil into the penis and testicles of a man († 32) at his request. Shortly thereafter, the patient developed health problems and later died.
The prosecution accuses the Heilpraktiker from Solingen of bodily injury resulting in death and violation of the Heilpraktikergesetz.
According to the report, the victim had traveled to Solingen in June 2019, where the defendant had given him the injection in his apartment.
Back home, the 32-year-old patient suddenly developed shortness of breath, had to be hospitalized, then transferred to the university hospital in Giessen. Seven months after the injection, he is dead. According to the indictment, the patient suffered multiple organ failure as a result of blood poisoning.
Three days of trial are scheduled. The defendant faces up to 15 years in prison.
_________________________
I had never heard of intra-testicular injections. So, I did a Medline search and found just two papers of the procedure in human patients:
Blunt trauma is the most common mechanism of injury to the scrotum and testicle. Surgical exploration with primary repair, hematoma evacuation, and de-torsion are common surgical interventions. A 20-year-old male with no previous medical history presented after a high-speed motor vehicle collision. Ultrasonography demonstrated heterogeneous changes of the tunica albuginea and decreased arterial flow to bilateral testicles. He was subsequently taken to the operating room for surgical exploration, which revealed bilateral mottled testes with questionable viability. Papaverine was injected into each testicle, which resulted in visibly increased perfusion and subsequent preservation of the testicles. Conclusion: Current evidence on the use of papaverine is isolated to testicular torsion. Additional research should be conducted on the use of papaverine in blunt testicular trauma. Papaverine injection may be a valuable treatment option when inadequate perfusion is observed intra-operatively.
No 2:
Purpose: We describe a simple technique to deliver local anaesthetic for percutaneous testis biopsies.
Materials and methods: With the testis held firmly, a 25 gage needle is used to inject lidocaine, without epinephrine, into the skin and dartos superficial to the testis, then the needle is advanced through the tunica albuginea and 0.5 mL to 1.0 mL of lidocaine is injected directly into the testis. The testis becomes slightly more turgid with the injection. A percutaneous biopsy is then immediately performed.
Results: Intra-testicular lidocaine, (without the need of a cord block or any sedation) was used on a total of 45 consecutive patients having percutaneous testicular biopsies. Procedure time was short (averages less than 5 minutes) and anaesthesia was profound. There was no change in the number of seminiferous tubules for evaluation compared to biopsies on men using a cord block. Only 1/45 men had a post-procedure testicular hematoma (this resolved in 4 weeks).
Conclusions: Intra-testicular lidocaine appears to be a simple, rapid and safe method to provide anaesthesia for a percutaneous testis biopsy.
All the other papers on intra-testicular injections were about animal experiments, mostly for exploring means of castration. This renders the above case even more unusual. The Heilpraktiker’s defense might stress that the patient wanted the treatment. That may be so but is it a valid excuse? No, of course not. In my view – and I am just a medic, not a lawyer – the Heilpraktiker is responsible for the treatment regardless of how much the patient insisted on it.
An article in the German publication T-online is, I think, relevant to us here on this blog. I translated part of it for you:
The suspicion of particularly serious fraud against a doctor from the German Meißen district has been substantiated. Since the beginning of the pandemic, the 66-year-old physician is said to have issued “certificates of convenience” in the thousands throughout Germany, a spokesman for the public prosecutor’s office said. In return for a payment of 25 euros, the doctor from Moritzburg is said to have issued blanket and unjustified certificates stating that the wearing of mouth and nose protection was not medically justifiable. In other cases, the physician stated an unlimited inoculation prohibition or that Corona quick tests were possible only over saliva.
After an initial search in February, the public prosecutor’s office had assumed to be dealing with merely 162 false vaccination and mask certificates. But the extent of the fraud seems to go far beyond that: The accused is now said to have taken in at least 60,000 euros with the fake certificates.
Based on further investigations, the public prosecutor’s office assumes that the medical practitioner has managed to issue false corona attestations “every minute” with so-called collective appointments. These appointments were arranged in cooperation with Heilpraktiker from all parts of Germany and partly even with funeral homes.
On Tuesday, more than 360 police officers searched 140 homes of exemption certificate holders in nine states – mainly in Bavaria. In the process, 174 incorrect Corona attestations were found. They now must face instigations into using illegal health certificates. In addition, the office of a Bavarian Heilpraktiker, as well as a further commercial area, were searched.
This is not the first time that the Moritzburg doctor has come into conflict with the law. The 66-year-old physician considers herself a ‘Reichsbuerger’ (citizen of the Reich, a right-wing extremist). She was a member of the Moritzburg shooting club, and owned eleven weapons. Because they were not all registered and several hundred rounds of ammunition were found in the house, she stood trial for the first time already in 2014.
A regional court in the Bavarian city of Ingolstadt has sentenced a natural healing practitioner, i.e. Heilpraktiker, and her supplier to jail for fraud. The pair were found to have deceived patients suffering from terminal cancer to put their faith in a remedy that they touted as a miracle cure. The practitioner was jailed for three years for her part in the scam, while the supplier was sentenced to six years and nine months.
The defendants in the case were a 57-year-old Heilpraktiker from the town of Schrobenhausen and a 68-year-old businessman from Ingolstadt who supplied the preparation. Both defendants were said to have promoted the remedy BG-Mun, saying that it could quickly cure cancer without any evidence of this being the case.
The court heard that patients paid up to €6,000 for the remedy. According to the court, the practitioner had boasted of “great successes” with one patient, Sabine H., who had acquired the remedy and stopped her course of chemotherapy at the defendant’s advice. The court was told that the pair would have known at this point that the substance would have no effect. A drug researcher from the University of Bremen had described the defendants’ actions as “profiteering” from the suffering of desperate patients. “Ultimately, it is a hustle against those who really are clutching at straws when it comes to their illness,” he said.
Even after the death of former patients, the defendants continued to promote their bogus remedy, the prosecutor emphasized. The Heilpraktiker advised several patients to rely exclusively on BG-Mun for their treatment and to discontinue the chemotherapy advised by orthodox medicine.
The defense lawyers demanded a comprehensive acquittal for both clients. The central argument: Both the Heilpraktiker and the entrepreneur had tried BG-Mun on themselves, found it helpful and therefore believed in its effect. The two had therefore acted without any intention to deceive. Without an intention to deceive, however, there is no fraud. In addition, BG-Mun had only ever been advertised as a “component in an overall therapy” and never as a sole medicine. According to the defense lawyers, BG-Mun is a means of alternative medicine and “therefore does not belong to evidence-based medicine”. In the opinion of the lawyers, empirical effectiveness, therefore, does not have to be proven. The public prosecutor, on the other hand, quoted experts who say that BG-Mun is a protein solution that has no effect whatsoever against cancer and is also not approved as a medicine.
Elsewhere it had been reported that the court also dealt with the charge of misuse of title, specifically with the fact that the Heilpraktiker used the title of professor orally and also on advertising flyers. The title of professor comes from an educational institution in the USA, which itself is not recognized as a university in the USA. The German Conference of Ministers of Education and Cultural Affairs does not recognize this title in this country and calls it a “decorative certificate”.
____________________
What I find particularly fascinating about this case is that the defense lawyers claimed, that BG-Mun is a means of alternative medicine and “therefore does not belong to evidence-based medicine”. This type of argument crops up regularly when quacks go to trial. I am not a legal expert and can thus only judge it from a medical point of view. Medically speaking, I find it hard to think of an argument that is more ridiculous than this one. To me, it seems like saying: “I am a charlatan and therefore you cannot judge by by the standards of regular healthcare.”
The second argument of the defense is hardy any better: “I was convinced that it worked, therefore, my prescribing it was honest and correct.” Imagine a doctor saying such nonsense! The argument makes a mockery of evidence by replacing it with belief. I am glad that the German court did not fall for such pseudo-arguments.
This analysis was aimed at quantifying how many studies registered on the Open Science Framework (OSF) up to November 2017 are performed but not shared after at least 4 years. Examining a sample of 315 registrations, of which 169 were research studies, the researchers found that 104 (62%) were published. They estimated that 5550 out of 9544 (58%) registered studies on the OSF are published.
Researchers use registries to make unpublished studies public, and the OSF policy to open registrations after a four-year embargo substantially increases the number of studies that become known to the scientific community. In responses to emails asking researchers why studies remained unpublished logistical issues (e.g., lack of time, researchers changing jobs) were the most common cause, followed by null results, and rejections during peer review.
The authors concluded that their study shows that a substantial amount of studies researchers perform remain unpublished.
I find this truly shocking!
Researchers are able to do research only because they receive financial and other support from elsewhere. Therefore they have an ethical obligation to publish it. The reasons frequently given for not publishing research are nothing well and truly invalid:
- Lack of time is a mere excuse; if researchers had the time to get the grants, permissions, etc. they simply must have the time to finish the job properly.
- Researchers changing jobs is an equally flawed excuse; if someone changes position, he/she is obliged to finish the job they were doing. A surgeon can also not leave mid-surgery because he has a better offer.
- ‘Null results’ is even worse as a reason. Null results are just as important as positive findings – occasionally they are even more important. If researchers fail to realize this, they simply disqualify themselves as researchers.
- ‘Rejections during peer review’ is complete nonsense. Everyone who submits papers for publication gets rejected once in a while. In this case, one learns from the peer-review comments, improves the paper in question, and re-submits it to another journal.
I have seen many studies of so-called alternative medicine (SCAM) that, for this or that reason, never were published. And I feel strongly that this is a serious violation of research ethics – so much so that I would ban researchers who are guilty of this crime from conducting research in the future. I also feel that, in order to receive the necessary support (financial and other), researchers should sign that they will publish their findings within a given time after finishing their study. Failing to comply could then incur a penalty such as paying back part of the funds wasted. I think such measures would very quickly clear up the current intolerable situation.
It has recently been reported that a 39-year-old woman (a mother-of-three died) died after immersing herself in a river as part of a cold water therapy session. The woman died after paramedics were called to attend a riverside in Derbyshire. The session was run by Kevin O’Neill of ‘Breatheolution’, whose previous clients include Coleen Rooney and actor Stephen Graham. The woman, who was visiting with two friends after paying up to £200 for a two-hour cold water therapy session, was rushed to hospital where she died.
Mr. O’Neill commented: “I am heartbroken. I’ve not slept and I’m finding it hard to process. I cannot stop thinking about her family. It’s tragic.” An inquest is expected to be opened into the woman’s death. East Midlands Ambulance Service said they were called to Bankside, in Bridgemont. “The caller reported a medical emergency,” a spokesperson said. “We sent a paramedic in a fast response car and a double-crewed ambulance. The air ambulance was also in attendance.”
Derbyshire Fire and Rescue Service, which was called to assist the paramedics, has warned people about the dangers of entering open water. “While we cannot and will not comment or speculate on the circumstances and cause of this tragic death, we would like to remind people of the dangers of entering open water and cold water shock,” said group manager Lee Williams.
_____________________
Breatheolution’ has a website where a whole page is dedicated to its leader Kevin O’Neill. I wondered what qualifications Kevin has, but all it tells us about him is this: “I struggled for so long with alcohol and other substance abuse that something had to give, I lost my sister Yvonne in 2019 and I think it was enough trauma to make me think a lot more about my own life”
The website also explains what the cold water sessions are about:
1-2-1 Breath Coaching, practice & Cold water session (river or tank)
2 hours @ £110.00
These sessions are proving popular with those who are not keen on group sessions or just prefer to have a more personal experience. The 2-3 hour sessions will be tailored to you and your breathing and will include potentially life-changing tools and methods to allow you to witness your breathing and physiology differently in the future, its all about feeling and awareness.
Another section of the site is dedicated to celebrities who Kevin seems to have treated. And then there is a video of the treatment. What I did not find anywhere, however, are the conditions that Kevin claims to treat with his cold water therapy.
In any case, it would have been wise for Kevin to read up about the risks of cold water immersion (CWI) before going into business. Perhaps this review would have helped:
In 2012, an estimated 372,000 people (42 per hour) died from immersion, assumed to be drowning. Immersion is the third leading cause of unintentional injury-related death, accounting for 7% of all such deaths (World Health Organization, 2014). These figures are underestimations owing to poor reporting in many Third World countries that have a high number of deaths. The data also do not include life-long morbidity caused by immersion-related injuries, estimated to be a much bigger numerical problem.
There is no strict definition of ‘cold water’. Given that some of the hazardous responses to cold water appear to peak on immersion somewhere between 15 and 10°C, it is reasonable to say that cold water is water <15°C (Tipton et al. 1991). However, the thermoneutral water temperature for a resting naked individual is ∼35°C, so it is possible for individuals to become very cold, with time, on immersion in water below this temperature. The corresponding temperature for those exercising (including shivering) is ∼25°C (Tipton & Golden, 1998).
Historically, the threat associated with CWI was regarded in terms of hypothermia or a reduction in deep body temperature below 35°C. This belief was established as a result of the Titanic disaster and supported by data obtained during maritime conflicts of World War II. However, more recently, a significant body of statistical, anecdotal and experimental evidence has pointed towards other causes of death on immersion. For example, in 1977 a Home Office Report revealed that ∼55% of the annual open water deaths in the UK occurred within 3 m of a safe refuge (42% within 2 m), and two-thirds of those who died were regarded as ‘good swimmers’. This evidence suggests more rapid incapacitation than can occur with whole-body cooling and consequent hypothermia.
The following four stages of immersion have been associated with particular risks (Golden & Hervey, 1981; Golden et al. 1991); the duration of these stages and the magnitude of the responses evoked within them vary significantly, depending on several factors, not least of which is water temperature:
- Initial immersion (first 3 min), skin cooling;
- Short-term immersion (3 min plus), superficial neuromuscular cooling;
- Long-term immersion (30 min plus), deep tissue cooling (hypothermia); and
- Circum-rescue collapse: immediately before, during or soon after rescue.
As a result of laboratory-based research, the initial responses to immersion, or ‘cold shock’, were identified as particularly hazardous (Tipton, 1989), accounting for the majority of immersion deaths (Tipton et al. 2014). These deaths have most often been ascribed to drowning, with the physiological responses of a gasp and uncontrollable hyperventilation, initiated by the dynamic response of the cutaneous cold receptors, resulting in the aspiration of the small volume of water necessary to initiate the drowning process (Bierens et al. 2016). Relatively little is known about the minimal rates of change of cold receptor temperature necessary to cause cold shock. The response has been reported to begin in water as warm as 25°C but is easy to suppress consciously at that temperature. In laboratory conditions, the respiratory frequency response (an indication of respiratory drive) peaks on naked immersion in a water temperature between 15 and 10°C, and is no greater on immersion in water at 5°C (Tipton et al. 1991). The corresponding average rates of change of chest skin temperature over the first 20 s of these immersions was 0.42 (water temperature 15°C), 0.56 (water temperature 10°C) and 0.68°C s−1 (water temperature 5°C). This suggests that an average rate of change in chest skin temperature between 0.42 and 0.56°C s−1 on the first 20 s of immersion is sufficient to evoke a maximal respiratory cold shock response.
More recently, it has been suggested (Shattock & Tipton, 2012) that a larger number of deaths than once thought may be attributable to arrhythmias initiated on immersion by the coincidental activation of the sympathetic and parasympathetic division of the autonomic nervous system by stimulation of cutaneous cold receptors around the body [sympathetic activation (cold shock)] and in the oronasal region on submersion or with wave splash [vagal stimulation (diving response)]. This ‘autonomic conflict’ is a very effective way of producing dysrhythmias and arrhythmias even in otherwise young and healthy individuals, particularly, but not necessarily, if a prolonged breath hold is involved in the immersion (Tipton et al. 1994). It seems that predisposing factors, such as long QT syndrome, ischaemic heart disease or myocardial hypertrophy, are necessary for fatal arrhythmias to evolve (Shattock & Tipton, 2012); many of these factors, including drug-induced long QT syndrome, are acquired. Non-fatal arrhythmias could still indirectly lead to death if they cause incapacitation and thereby drowning (Tipton, 2013). The hazardous responses associated with the cold shock response are presented in Fig. 2.
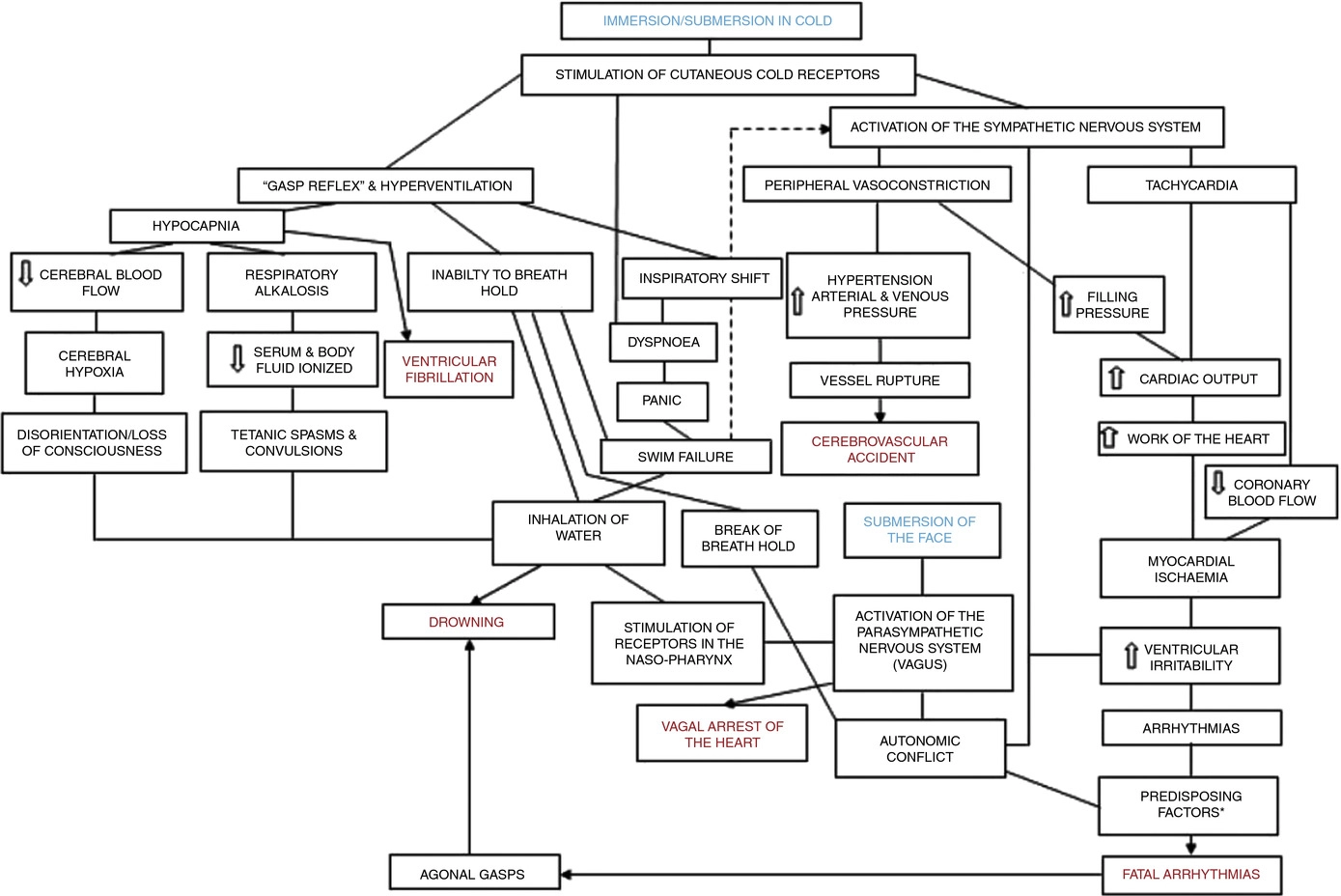
Figure 2. A contemporary view of the initial responses to immersion and submersion in cold water (‘cold shock’)
The problems encountered in short-term immersions are primarily related to physical incapacitation caused by neuromuscular cooling (Castellani & Tipton, 2015). The arms are particularly susceptible because of their high surface area to mass ratio. Low muscle temperatures affect chemical and physical processes at the cellular level. This includes metabolic rate, enzymatic activity, calcium and acetylcholine release and diffusion rate, as well as the series elastic components of connective tissues (Vincent & Tipton, 1988). Maximal dynamic strength, power output, jumping and sprinting performance are related to muscle temperature, with reductions ranging from 4 to 6% per degree Celsius reduction in muscle temperature down to 30°C (Bergh & Ekblom, 1979). At nerve temperatures below ∼20°C, nerve conduction is slowed and action potential amplitude is decreased (Douglas & Malcolm, 1955). Nerve block may occur after exposure to a local temperature of between 5 and 15°C for 1–15 min. This can lead to dysfunction that is equivalent to peripheral paralysis and can, again, result in drowning owing to the inability to keep the airway clear of the water (Clarke et al. 1958; Basbaum, 1973; Golden & Tipton, 2002; Fig. 3).
Figure 3. The ‘physiological pathways to drowning’ after immersion or submersion in cold water, with possible interventions for partial mitigation (dashed)
Abbreviations: EBA, emergency breathing aid; IS, immersion suit; and LJ, lifejacket. Reproduced with permission, from Tipton (2016b).
Even in ice-cold water, the possibility of hypothermia does not arise for at least 30 min in adults. Hypothermia affects cellular metabolism, blood flow and neural function. In severe hypothermia, the patient will be deeply unconscious. The progressive signs and symptoms (approximate deep body temperature) are shivering (36°C), confusion, disorientation, introversion (35°C), amnesia (34°C), cardiac arrhythmias (33°C), clouding of consciousness (33–30°C), loss of consciousness (30°C), ventricular fibrillation (28°C) and death (25°C) (Bierens et al. 2016). There is great variability between deep body temperature and the signs and symptoms of hypothermia. For example, although the deep body temperature associated with death is often quoted as 25°C, the lowest temperature recorded to date after accidental exposure to cold (air) and with full recovery was 12.7°C in a 28-month-old child (Associated Press, 2014). The coldest adult survivor of CWI followed by submersion had a body temperature of 13.7°C (Gilbert et al. 2000). There is also a large amount of variation in the rate at which people cool on immersion in cold water, owing to a combination of thermal factors (including water temperature and water movement, internal and external insulation) and non-thermal factors (including body size and composition, blood glucose, motion illness, racial and sex differences; Haight & Keatinge, 1973; Gale et al. 1981; White et al. 1992; Mekjavic et al. 2001; Golden & Tipton, 2002).
The most significant practical consequence of hypothermia in water is loss of consciousness; this prevents individuals from undertaking physical activity to maintain a clear airway and avoid drowning. Thus, once again, drowning is often the end-point (Fig. 3).
About 17% of those who die as a result of immersion die immediately before, during or after rescue (Golden et al. 1991). The deaths immediately before rescue are intriguing and probably related to behavioural changes at this time or the relief and psychophysiological alterations associated with imminent rescue, including a reduction in circulating stress hormone concentration and an increase in vagal tone. Death during rescue is most commonly associated with a collapse in arterial pressure when lifted vertical from the water and kept in that position for some time (Golden et al. 1991).
_____________________________
The tragic death of the woman should perhaps remind us that
- there is no SCAM or wellness treatment that is entirely harmless,
- and there are only few ‘would-be gurus’ who know what they are doing.



