risk
Although the use of so-called alternative medicine (SCAM) is said to be rising among older adults, many do
not discuss these healthcare practices with their primary care practitioners (PCPs). This recent US survey sought to determine the prevalence of SCAM use and to identify factors associated with SCAM disclosure among patients ages 65 and older.
Participants completed an anonymous survey, which evaluated their SCAM use over the past year and disclosure of SCAM to a PCP. Additional questions queried demographics, patient health, and relationships with one’s PCP. Analyses included descriptive statistics, chi-square tests, and logistic regression.
One hundred seventy-three participants answered surveys (response rate=23%). The Main findings were as follows:
- Sixty percent reported the use of at least one form of SCAM in the past year.
- Among those using SCAM, 64% disclosed use to their PCP.
- Patients disclosed supplements/herbal products and naturopathy/homeopathy/acupuncture at a higher rate than bodywork techniques and mind-body practices (71.9% and 66.7% vs. 48% and 50%).
- The only factor significantly associated with disclosure was trust in one’s PCP (odds ratio=2.97; confidence interval=1.01–8.73).
- The most commonly used types of SCAM were herbal products/dietary supplements (37.0%), mind-body therapies (28.9%), bodywork techniques (26.6%), and naturopathy/acupuncture/homeopathy (8.7%).
The authors concluded that clinicians may improve SCAM disclosure rates in older adults by inquiring about all types of SCAM and continuing to invest in their patient relationships, specifically by building trust.
The one-year prevalence of SCAM use – 60% – is extraordinary and considerably higher than in other surveys. How can this be explained?
I think that two factors might have played a role: firstly the survey was tiny, and secondly, its response rate was dismal. People who have no interest in SCAM would probably have not responded. Thus the prevalence figure is way too high and the survey is not representative of any population.
Having said that, I believe that some of the conclusions are still correct. As I have pointed out so often already:
- doctors need to ask their patients about SCAM usage;
- once they have identified a SCAM user, they need to advise him/her responsibly;
- to do that, they need to know about SCAM;
- as most doctors have little knowledge about the subject, they need to learn;
- failing to do that is not ethical behavior.
The ‘American Heart Association News’ recently reported the case of a 33-year-old woman who suffered a stroke after consulting a chiropractor. I take the liberty of reproducing sections of this article:
Kate Adamson liked exercising so much, her goal was to become a fitness trainer. She grew up in New Zealand playing golf and later, living in California, she worked out often while raising her two young daughters. Although she was healthy and ate well, she had occasional migraines. At age 33, they were getting worse and more frequent. One week, she had the worst headache of her life. It went on for days. She wasn’t sleeping well and got up early to take a shower. She felt a wave of dizziness. Her left side seemed to collapse. Adamson made her way down to the edge of the tub to rest. She was able to return to bed, where she woke up her husband, Steven Klugman. “I need help now,” she said.
Her next memory was seeing paramedics rushing into the house while her 3-year-old daughter, Stephanie, was in the arms of a neighbor. Rachel, her other daughter, then 18 months old, was still asleep. When she woke up in the hospital, Adamson found herself surrounded by doctors. Klugman was by her side. She could see them, hear them and understand them. But she could not move or react.
Doctors told Klugman that his wife had experienced a massive brain stem stroke. It was later thought to be related to neck manipulations she had received from a chiropractor for the migraines. The stroke resulted in what’s known as locked-in syndrome, a disorder of the nervous system. She was paralyzed except for the muscles that control eye movement. Adamson realized she could answer yes-or-no questions by blinking her eyes.
Klugman was told that Adamson had a very minimal chance of recovery. She was put on a ventilator to breathe, given nutrition through a feeding tube, and had to use a catheter. She learned to coordinate eye movements to an alphabet chart. This enabled her to make short sentences. “Am I going to die?” she asked one of her doctors. “No, we’re going to get you into rehab,” he said.
Adamson stayed in the ICU on life support for 70 days before being transferred to an acute rehabilitation facility. She could barely move a finger, but that small bit of progress gave her hope. In rehab, she slowly started to regain use of her right side; her left side remained paralyzed. Therapists taught her to swallow and to speak. She had to relearn to blow her nose, use the toilet and tie her shoes.
She was particularly fond of a social worker named Amy who would incorporate therapy exercises into visits with her children, such as bubble blowing to help her breathing. Amy, who Adamson became friends with, also helped the children adjust to seeing their mother in a wheelchair.
Adamson changed her dream job from fitness trainer to hospital social worker. She left rehab three and a half months later, still in a wheelchair but able to breathe, eat and use the toilet on her own. She continued outpatient rehab for another year. She assumed her left side would improve as her right side did. But it remained paralyzed. She would need to use a brace on her left leg to walk and couldn’t use her left arm and hand. Still, two years after the stroke, which happened in 1995, Adamson was able to drive with a few equipment modifications…
In 2018, Adamson reached another milestone. She graduated with a master’s degree in social work; she’d started college in 2011 at age 49. “It wasn’t easy going to school. I just had to take it a day at a time, a semester at a time,” she said. “The stroke has taught me I can walk through anything.” …
Now 60, she works with renal transplant and pulmonary patients, helping coordinate their services and care with the rest of the medical team at Vanderbilt University Medical Center. “Knowing that you’re making a difference in somebody’s life is very satisfying. It takes me back to when I was a patient – I’m always looking at how I would want to be treated,” she said. “I’ve really come full circle.”
Adamson has adapted to doing things one-handed in a two-handed world, such as cooking and tying her shoes. She also walks with a cane. To stay in shape, she works with a trainer doing functional exercises and strength training. She has a special glove that pulls her left hand into a fist, allowing her to use a rowing machine and stationary bike….
Adamson is especially determined when it comes to helping her patients. “I work really hard to be an example to them, to show that we are all capable of going through difficult life challenges while still maintaining a positive attitude and making a difference in the world.”
________________________
What can we learn from this story?
Mainly two things, in my view:
- We probably should avoid chiropractors and certainly not allow them to manipulate our necks. I know, chiros will say that the case proves nothing. I agree, it does not prove anything, but the mere suspicion that the lock-in syndrome was caused by a stroke that, in turn, was due to upper spinal manipulation plus the plethora of cases where causality is much clearer are, I think, enough to issue that caution.
- Having been in rehab medicine for much of my early career, I feel it is good to occasionally point out how important this sector often neglected part of healthcare can be. Rehab medicine has been a sensible form of multidisciplinary, integrative healthcare long before the enthusiasts of so-called alternative medicine jumped on the integrative bandwagon.
A regional court in the Bavarian city of Ingolstadt has sentenced a natural healing practitioner, i.e. Heilpraktiker, and her supplier to jail for fraud. The pair were found to have deceived patients suffering from terminal cancer to put their faith in a remedy that they touted as a miracle cure. The practitioner was jailed for three years for her part in the scam, while the supplier was sentenced to six years and nine months.
The defendants in the case were a 57-year-old Heilpraktiker from the town of Schrobenhausen and a 68-year-old businessman from Ingolstadt who supplied the preparation. Both defendants were said to have promoted the remedy BG-Mun, saying that it could quickly cure cancer without any evidence of this being the case.
The court heard that patients paid up to €6,000 for the remedy. According to the court, the practitioner had boasted of “great successes” with one patient, Sabine H., who had acquired the remedy and stopped her course of chemotherapy at the defendant’s advice. The court was told that the pair would have known at this point that the substance would have no effect. A drug researcher from the University of Bremen had described the defendants’ actions as “profiteering” from the suffering of desperate patients. “Ultimately, it is a hustle against those who really are clutching at straws when it comes to their illness,” he said.
Even after the death of former patients, the defendants continued to promote their bogus remedy, the prosecutor emphasized. The Heilpraktiker advised several patients to rely exclusively on BG-Mun for their treatment and to discontinue the chemotherapy advised by orthodox medicine.
The defense lawyers demanded a comprehensive acquittal for both clients. The central argument: Both the Heilpraktiker and the entrepreneur had tried BG-Mun on themselves, found it helpful and therefore believed in its effect. The two had therefore acted without any intention to deceive. Without an intention to deceive, however, there is no fraud. In addition, BG-Mun had only ever been advertised as a “component in an overall therapy” and never as a sole medicine. According to the defense lawyers, BG-Mun is a means of alternative medicine and “therefore does not belong to evidence-based medicine”. In the opinion of the lawyers, empirical effectiveness, therefore, does not have to be proven. The public prosecutor, on the other hand, quoted experts who say that BG-Mun is a protein solution that has no effect whatsoever against cancer and is also not approved as a medicine.
Elsewhere it had been reported that the court also dealt with the charge of misuse of title, specifically with the fact that the Heilpraktiker used the title of professor orally and also on advertising flyers. The title of professor comes from an educational institution in the USA, which itself is not recognized as a university in the USA. The German Conference of Ministers of Education and Cultural Affairs does not recognize this title in this country and calls it a “decorative certificate”.
____________________
What I find particularly fascinating about this case is that the defense lawyers claimed, that BG-Mun is a means of alternative medicine and “therefore does not belong to evidence-based medicine”. This type of argument crops up regularly when quacks go to trial. I am not a legal expert and can thus only judge it from a medical point of view. Medically speaking, I find it hard to think of an argument that is more ridiculous than this one. To me, it seems like saying: “I am a charlatan and therefore you cannot judge by by the standards of regular healthcare.”
The second argument of the defense is hardy any better: “I was convinced that it worked, therefore, my prescribing it was honest and correct.” Imagine a doctor saying such nonsense! The argument makes a mockery of evidence by replacing it with belief. I am glad that the German court did not fall for such pseudo-arguments.
Enthusiasts of so-called alternative medicine (SCAM) sometimes remind me of the French philosopher, Blaire Pascal, and his famous wager. Blaise Pascal (1623-1662) argued that, because it is impossible to either prove or disprove the existence of God, it would probably be best to wager in favor of his existence. In case one got it wrong, little would be lost; in case one was correct, everything was gained.
Likewise, enthusiasts of SCAM often argue that, because of the lack of evidence for many SCAMs, one cannot be sure whether they work or not. Thus it would probably be best to wager in favor of SCAM and make use of it. In case one got it wrong, little would be lost; in case one was correct, everything was gained.
This line of thinking is common and, at first glance, it seems to be “a safe bet”. However, once we analyze it critically, it quickly falls apart. To explain, it might be best to choose a concrete example. Let’s assume, therefore, that we are talking about a cancer patient who wants to leave no stone unturned to cure her cancer.
So, she goes on the Internet and does her ‘research’. As soon as she has found a SCAM that might suit her, another one crops up, and then another, and then dozens. Which SCAM should she use? There are hundreds of SCAM cancer “cures” being promoted to the unsuspecting and vulnerable. Since one is as unproven as the next, our patient has a hard time deciding which SCAM to try. Applying all simultaneously or consecutively would be “betting on the safe side,” but is not a realistic option. If nothing else, it would be an unaffordable full-time job.
A further flaw in Pascal’s approach to SCAM relates to the fact that we are unable to prove the existence of God, but scientists are entirely capable of finding out about SCAM and its effects on cancer patients. After all, that’s what clinical trials are designed for. If for a particular SCAM, no studies are available (which is often the case), it probably means that it is not worth the effort of testing the claims that are being made for it. SCAM cancer cures are ‘alternatives’ for one main reason: they are implausible, so much so that the chances of them doing more good than harm usually approach zero.
And there is yet another caveat: while accepting the existence of God might be not associated with major harm (I know, some people would dispute this), many SCAMs are by no means free of risks. Therefore it is simply not true to assume that “little is lost” in case they do not work.
Direct harm can occur through the interactions of some form of SCAM with prescription drugs, for instance. But the potential for indirect harm is much more important. Here the risks range from raising false hopes or financial exploitation to undermining rationality in a much more general sense. By far the biggest indirect risk is that SCAM is used as a replacement for effective treatments. Most patients do not approach SCAM to give up conventional medicine entirely. But SCAM practitioners can be most persuasive, and some over-enthusiastic SCAM therapists do try to convince their patients to abandon life-saving treatments.
Pascal’s wager was disputed when it was first published. As a result of the ensuing discussions, significant advances were made, for instance, in the area of probability theory. Applying Pascal’s wager to SCAM, as many enthusiasts do, is however a very different matter. I am afraid, the benefits of doing so might not outweigh the risks.
The COVID-19 pandemic has posed an unprecedented challenge to global health. Classical homeopathy may, according to homeopaths, have a role to play in alleviating this burden. The objective of this study was to curate data on the treatment effect of classical homeopathy for COVID-19 in a real-world scenario to guide future scientific investigations.
Classical homeopaths from the International Academy of Classical Homeopathy (IACH) were asked to provide details on cases they treated by filling out a standardized questionnaire. COVID-19 cases were defined according to World Health Organization (WHO) criteria as suspected/probable/confirmed cases, with intervention provided being either stand-alone classical homeopathy or combined with conventional therapy for COVID-19. Cases were followed up with main outcomes being ‘improved’, ‘not improved’, or ‘progressed’ post-treatment. Details of the homeopathic remedies used and the main symptoms at the presentation were gathered. Factors associated with main outcomes were investigated with correlational and regression analyses.
367 patients (male 166, female 201) met eligibility criteria (mean age 42.75 years). The mean follow-up period was 6.5 (standard deviation, SD=5.3) days. 255 were confirmed COVID-19 cases, with 61 probable and 51 suspected cases, respectively. The most used remedy was Arsenicum album. Over 73% of COVID-19 patients (and about 79% of severe cases) improved under classical homeopathic treatment. The number of remedies required per individual was negatively correlated to improvement (P< 0.01). Fever, the most common symptom at presentation (74.4%), was associated with an increased likelihood of improvement (P<0.01). Improvement was negatively associated with advanced age, but not associated with sex (P<0.01).
The authors conclude that this study suggests that classical homeopathy was associated with improvement in COVID-19, including severe cases. Despite limitations from study design and data sources, our findings should prompt further studies on the role of classical homeopathy in the management of COVID-19.
I BEG TO DIFFER!
These cases suggest nothing of the sort. If anything, these highly selected cases suggest that about 27% of the exemplary patients did not improve, perhaps they even died. This implies to me that classical homeopathy worsens the prognosis of patients infected with COVID-19.
The ‘International Academy of Classical Homeopathy‘ is led by the ‘Ueber-Homeopath’, George Vithoulkas. His vision is that this Academy will become a center of real knowledge which will provide an education that will far exceed the technical and strictly “medical” aspect of one’s learning. One might ask what fanatics like he truly want to achieve – is it perhaps the promotion of ‘euthanasia homoeopathica’?
This survey evaluated the attitude of healthcare professionals toward the use of so-called alternative medicine (SCAM) to improve current care. A questionnaire on the current practice and opinions about SCAM use was sent to healthcare professionals in Amsterdam UMC, who work for the department of hematology or oncology. Oncologists, hematologists, residents, (specialized) nurses, dieticians, (hospital)pharmacists, and pharmacy technicians were asked to participate.
Among eligible healthcare professionals, 77 responded to the questionnaire (34%). Overall, 87% of healthcare
professionals indicated it is important to be aware of their patient’s SCAM use, and all find the potential of drug–herb interactions important. However, more than half of the healthcare professionals inquire about the patient’s SCAM use infrequently. In addition, only 15% of the healthcare professionals stated they had sufficient knowledge of SCAM to advise patients on their use of SCAM.
The authors concluded that healthcare professionals are aware of the potential risks of SCAM use in combination with anti-cancer treatment. However, SCAM use is not yet discussed with every patient. This may be due to healthcare professionals’ lack of knowledge about SCAM.
This survey would in itself be fairly irrelevant; it employed only a tiny convenience sample and its findings cannot be generalized. Yet, it produced results that have been shown dozens of times before, and it might therefore be a good idea to remind ourselves of their relevance and implications.
- Patients use SCAM whether we want it or not.
- Contrary to what is often said, SCAM is not harmless.
- Therefore conventional healthcare professionals need to know about their patients’ SCAM use.
- To find out, healthcare professionals need to ask specific questions about SCAM.
- Next, they must advise their patients responsibly (this is an ethical obligation, not a choice).
- In order to do that they need to learn the essentials about SCAM.
- Failing to do this means failing their patients.
I have to admit that I do not regularly read the DMZ, a German paper. In fact, until a minute ago, I did not know it existed. Nor do I know Anton Aeberhard. I saw his DMZ homeopathy article on the Internet and find it excellent; so much so that I translated parts of it for you:
… Because this pseudoscience is considered by some people to be an effective alternative to conventional medicine, it is important to understand the potential dangers and risks of homeopathy…
Homeopathy is based on the principle of the rule of similars and extreme dilution of substances. However, there is no scientific evidence that homeopathic remedies have any therapeutic effect beyond the placebo effect. Most studies that purport to show efficacy are methodologically flawed. Homeopathy contradicts fundamental principles of biology, chemistry, and physics. It is therefore irresponsible to consider this practice a legitimate medical treatment.
One of the greatest and real dangers of homeopathy is that it can cause people to refuse or delay effective medical treatments. By believing in homeopathic remedies, life-threatening conditions such as cancer, heart disease, or infections may not be treated appropriately. This can lead to worsening health conditions and increase the risk of complications or even death…
Conclusion I
Homeopathy is a pseudoscientific practice based on outdated principles and a lack of scientific evidence. The dangers of this practice should not be underestimated. It can cause people to reject or delay effective medical treatments, which can endanger their health and lives. It is important to make informed decisions about health care and to rely on evidence-based medicine to provide the best possible treatment and care.
Conclusion II.
Homeopathy is a joke.
________________________
Thank you Anton Aeberhard!
It is not often that we find a journalist who has the courage to defy the demand for ‘balance’. In the case of clear nonsensical issues, this demand becomes a demand for misleading people, a demand for FALSE balance!
When a journalist writes about the planet, he does not require a representative of the FLAT EARTH SOCIETY to add his views. Similarly, when someone writes about homeopathy, there is no need to interview the chair of a homeopaths’ association saying: “But we have 200 years of experience and we therefore know it works…”
This systematic review was aimed at determining if there has been a change in the reporting of adverse events associated with spinal manipulation in randomized clinical trials (RCTs) since 2016.
Databases were searched from March 2016 to May 2022: MEDLINE (Ovid), Embase, CINAHL, ICL, PEDro, and Cochrane Library. The following search terms and their derivatives were adapted for each platform: spinal manipulation; chiropractic; osteopathy; physiotherapy; naprapathy; medical manipulation and clinical trial.
Domains of interest (pertaining to adverse events) included: completeness and location of reporting; nomenclature and description; spinal location and practitioner delivering manipulation; methodological quality of the studies and details of the publishing journal. Frequencies and proportions of studies reporting on each of these domains were calculated. Univariable and multivariable logistic regression models were fitted to examine the effect of potential predictors on the likelihood of studies reporting on adverse events.
There were 5399 records identified by the electronic searches, of which 154 (2.9%) were included in the analysis. Of these, 94 (61.0%) reported adverse events with only 23.4% providing an explicit description of what constituted an adverse event. Reporting of adverse events in the abstract had increased (n=29, 30.9%) while reporting in the results section had decreased (n=83, 88.3%) over the past 6 years. Spinal manipulation was delivered to 7518 participants in the included studies. No serious adverse events were reported in any of these studies.
The authors concluded that, while the current level of reporting of adverse events associated with spinal manipulation in RCTs has increased since our 2016 publication on the same topic, the level remains low and inconsistent with established standards. As such, it is imperative for authors, journal editors and administrators of clinical trial registries to ensure there is more balanced reporting of both benefits and harms in RCTs involving spinal manipulation.
In fact, it is an ethical imperative to accurately report adverse effects. Not reporting adverse effects amounts to a violation of medical research ethics. Adverse effects of spinal manipulation occur in about 50% of all patients. This means that investigators reporting significantly lower figures are likely guilty of under-reporting. And under-reporting of adverse events is also a breach of ethical standards.
My conclusion thus is that the vast majority of trials of spinal manipulation are unethical and should be discarded.
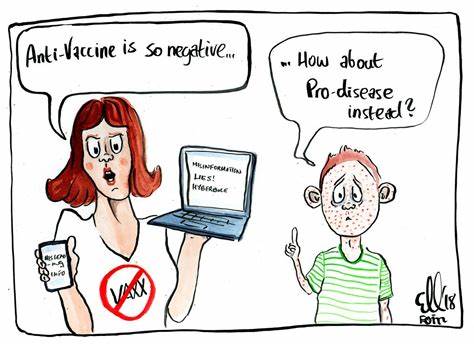
Numerous qualitative studies and a few quantitative studies have linked vaccine hesitancy or refusal with the belief in the efficacy of so-called alternative medicine (SCAM). Yet, large-scale data on this topic are scarce. In this study, the French researchers investigated the factors associated with the coverage rates of seven childhood vaccines or vaccine groups in the ninety-six metropolitan French departments. One of the factors investigated was the local interest in SCAM. In order to assess this interest, they built an Alternative Medicine Index based on departmental internet searches regarding SCAM—internet searches being a reliable indicator of the public’s actual interest in a given topic. They then conducted multiple regression analyses, which showed that this Index is a significant explanatory factor for the departmental variance in vaccination coverage rates, exceeding in importance the effect of other relevant local sociodemographic factors.
A further recent study from France adds to the picture. It presents the results of a survey conducted in July 2021 among a representative sample of the French mainland adult population (n = 3087). Using cluster analysis, the researchers identified five profiles of SCAM attitudes and found that even among the most pro-SCAM group, very few respondents disagreed with the idea that SCAM should only be used as a complement to conventional medicine. They then compared these SCAM attitudes to vaccine attitudes. Attitudes to SCAM had a distinct impact as well as a combined effect on attitudes to different vaccines and vaccines in general. They found that:
- attitudes to SCAM provide a very limited explanation of vaccine hesitancy;
- among the hesitant, pro-SCAM attitudes are often combined with other traits associated with vaccine hesitancy such as distrust of health agencies, radical political preferences, and low income.
Both SCAM endorsement and vaccine hesitancy are more prevalent among the socially disadvantaged. Drawing on these results, the researchers argue that, to better understand the relationship between SCAM and vaccine hesitancy, it is necessary to look at how both can reflect a lack of access and recourse to mainstream medicine and distrust of public institutions.
 The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
- Preference of so-called alternative medicine predicts negative attitudes to vaccination
- What are the reasons for opposing COVID vaccinations?
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- More information on homeopaths’ and anthroposophic doctors’ attitude towards vaccinations
- The anti-vaccination movement is financed by the dietary supplement industry
- Sorry, I was wrong about homeopathy and vaccination
- The UK Society of Homeopaths, a hub of anti-vaccination activists?
- HOMEOPATHY = “the complete alternative to vaccination” ?!?!
- Are anthroposophy-enthusiasts for or against vaccinations?
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Naturopaths’ counselling against vaccinations could be criminally negligent
- HOMEOPATHS AGAINST VACCINATION: “The decision to vaccinate and how you implement that decision is yours and yours alone”
- Use of alternative medicine is associated with low vaccination rates
- Integrative medicine physicians tend to harbour anti-vaccination views
- Vaccination: chiropractors “espouse views which aren’t evidence based”
What seems fairly clear to me is that a cross-correlation exists: an attitude against modern medicine and the ‘scientific establishment’ determines both the enthusiasm for SCAM and the aversion to vaccination. What is, however, far from clear to me is what we could do about it.
Yes, better education seems important – and that’s precisely what I aim at achieving with this blog. Sadly, judging from some of the comments we receive, it does not seem crowned with much success.
Any other ideas?
“The decline of homeopathy, the ‘medicine’ that doesn’t cure anything” is the title of a remarkable article in EL PAIS of which I take the liberty of showing you a few key passages:
In the more than 200 years that have passed since its invention, no one has been able to prove that homeopathy is actually capable of curing anything with its alleged medicines that have no active ingredients…
…EL PAÍS reached out to some of its main promoters, such as the pharmaceutical company Boiron, leader in the sector; the Spanish Association of Homeopathy Pharmacists and the Spanish Society of Homeopathic Doctors. In the absence of a response from all three, the explanations are given by experts who are more critical of the discipline.
Many people who used to consume homeopathy were not even aware that this was the case. Fernando Frías, one of the activists who worked to undermine the discipline’s remaining prestige, recalls that people did not believe them when they were told that compounds with diluted Berlin Wall were sold to overcome the feelings of oppression and anxiety. This was actually commercialized under the premise that “like cures like”: if the Berlin Wall oppressed, a piece of it diluted in water should remedy it. “Many were under the impression that it was just a natural therapy and that we were making things up to attack it,” says Frías…
… There has been a lot of debate about how to regulate an alleged drug whose only effect is, in truth, the placebo effect. In 2001, the European Parliament issued a directive that covered its use in countries with a homeopathic tradition; sources explain that this happened due to the pressure exerted by both the industries and the governments of countries where pseudoscience is deep-rooted, such as France (where Boiron is headquartered) or Germany, where its consumption is much higher than in others, such as Spain.
“Having regard to the particular characteristics of these homeopathic medicinal products, such as the very low level of active principles they contain and the difficulty of applying to them the conventional statistical methods relating to clinical trials, it is desirable to provide a special, simplified registration procedure for those homeopathic medicinal products which are placed on the market without therapeutic indications in a pharmaceutical form and dosage which do not present a risk for the patient,” states the directive.
In its more than two centuries of history, this is not the first time that homeopathy loses ground. Still, Frías warns, it cannot be ruled out that at some point something will come up that will make it fashionable again. “Look at the example of chemtrails [the condensation trails left by airplanes that some conspiracy theorists believe are a way of poisoning the population from the air]. It seemed that no one remembered them anymore, but now they’re back,” he says. Frías cites the astrophysicist and disseminator Javier Armentia, who states that beliefs are like a rubber duck: no matter how much they sink, they always resurface. “Especially if there is money behind,” he adds.
______________________
As reported previously, homeopathy and other forms of so-called alternative medicine (SCAM) have come under fire in Spain. In 2017, ‘HOMEOPATHY PLUS‘ reported that “in a reversal of the 2015 Royal Legislative Decree, the Minister of Health has withdrawn homeopathic remedies and outlawed the practice in Spain’s national health services.” In 2018, more than 400 people signed an open letter triggered by the case of a cancer patient who died after preferring homeopathy to regular treatment. “Let’s be clear: pseudoscience kills,” begins the letter. Since then, the struggle of Spanish rational thinkers to stop misleading information about SCAM in general and homeopathy, in particular, has only intensified.
Spain is thus joining other European countries in opposing misinformation about homeopathy. Contrary to what some have claimed (for instance, in the comments section of this blog), most of the opponents do not want to restrict the public’s choice. People who wish to use homeopathy should be able to do so (but should pay for it themselves). However, the choice must be based on evidence-based information.
