critical thinking
In this study, the impact of a multimodal integrative oncology pre- and intraoperative intervention on pain and anxiety among patients undergoing gynecological oncology surgery was explored.
Study participants were randomized into three groups:
- Group A received preoperative touch/relaxation techniques, followed by intraoperative acupuncture, plus standard care;
- Group B received preoperative touch/relaxation only, plus standard care;
- Group C (the control group) received standard care.
Pain and anxiety were scored before and after surgery using the Measure Yourself Concerns and Wellbeing (MYCAW) and Quality of Recovery (QOR-15) questionnaires, using Part B of the QOR to assess pain, anxiety, and other quality-of-life parameters.
A total of 99 patients participated in the study: 45 in Group A, 25 in Group B, and 29 in Group C. The three groups had similar baseline demographic and surgery-related characteristics. Postoperative QOR-Part B scores were significantly higher in the treatment groups (A and B) when compared with controls (p = .005), including for severe pain (p = .011) and anxiety (p = .007). Between-group improvement for severe pain was observed in Group A compared with controls (p = .011). Within-group improvement for QOR depression subscales was observed in only the intervention groups (p <0.0001). Compared with Group B, Group A had better improvement of MYCAW-reported concerns (p = .025).
The authors concluded that a preoperative touch/relaxation intervention may significantly reduce postoperative anxiety, possibly depression, in patients undergoing gynecological oncology surgery. The addition of intraoperative acupuncture significantly reduced severe pain when compared with controls. Further research is needed to confirm these findings and better understand the impact of intraoperative acupuncture on postoperative pain.
Regular readers of my blog know only too well what I am going to say about this study.
Imagine you have a basket full of apples and your friend has the same plus a basket full of pears. Who do you think has more fruit?
Dumb question, you say?
Correct!
Just as dumb, it seems, as this study: therapy A and therapy B will always generate better outcomes than therapy B alone. But that does not mean that therapy A per se is effective. Because therapy A generates a placebo effect, it might just be that it has no effect beyond placebo. And that acupuncture can generate placebo effects has been known for a very long time; to verify this we need no RCT.
As I have so often pointed out, the A+B versus B study design never generates a negative finding.
This is, I fear, precisely the reason why this design is so popular in so-called alternative medicine (SCAM)! It enables promoters of SCAM (who are not as dumb as the studies they conduct) to pretend they are scientists testing their therapies in rigorous RCTs.
The most disappointing thing about all this is perhaps that more and more top journals play along with this scheme to mislead the public!
The impact of drug-induced liver injury (DILI) on patients with chronic liver disease (CLD) is unclear. There are few reports comparing DILI in CLD and non-CLD patients. In this study, the researchers aimed to determine the incidence and outcomes of DILI in patients with and without CLD.
They collected data on eligible individuals with suspected DILI between 2018 and 2020 who were evaluated systematically for other etiologies, causes, and the severity of DILI. They compared the causative agents, clinical features, and outcomes of DILI among subjects with and without CLD who were enrolled in the Thai Association for the Study of the Liver DILI registry. Subjects with definite, or highly likely DILI were included in the analysis.
The researchers evaluated the causal relationship between the clinical pattern of liver injury and the suspected drugs or SCAM products with the Roussel Uclaf Causality Assessment Method (RUCAM) system. RUCAM is a validated and established tool to quantitatively assess causality in cases of suspected DILI and/or SCAM product-induced liver injury. They also used the Clinical Assessment of Causality Scale to assess the association as definite (>95% likelihood), highly likely (75–95%), probable (50–74%), possible (25–49%) or unlikely (<25%).
A total of 200 subjects diagnosed with DILI were found in the registry. Of those, 41 had CLD and 159 had no evidence of CLD. So-called alternative medicine (SCAM) products were identified as the most common class of DILI agents. Approximately 59% of DILI in the CLD and 40% in non-CLD group were associated with SCAM use. Individuals with pre-existing CLD had similar severity including mortality. Twelve patients (6%) developed adverse outcomes related to DILI including seven (3.5%) deaths and five (2.5%) with liver failure. Mortality was 4.88% in CLD and 3.14% in non-CLD subjects over median periods of 58 (8-106) days and 22 (1-65) days, respectively.
The authors concluded that, in this liver disease registry, the causes, clinical presentation, and outcomes of DILI in subjects with CLD and without CLD patients were not different. Further study is required to confirm our findings.
Consumers often prefer SCAM to conventional medicine because SCAM is viewed as gentle and safe. The notions are that they
- are natural and therefore harmless;
- have been in use for ages and thus have stood the test of time.
Readers of this blog will appreciate that both notions are, in fact, fallacies:
- appeal to nature;
- appeal to tradition.
This new paper is an impressive reminder that SCAM’s reputation as a safe option is not justified, and that SCAM relies more on fallacies than on facts.
Gut microbiota can influence health through the microbiota–gut–brain axis. Meditation can positively impact the regulation of an individual’s physical and mental health. However, few studies have investigated fecal microbiota following long-term (several years) deep meditation. Therefore, this study tested the hypothesis that long-term meditation may regulate gut microbiota homeostasis and, in turn, affect physical and mental health.
To examine the intestinal flora, 16S rRNA gene sequencing was performed on fecal samples of 56 Tibetan Buddhist monks and neighboring residents. Based on the sequencing data, linear discriminant analysis effect size (LEfSe) was employed to identify differential intestinal microbial communities between the two groups. Phylogenetic Investigation of Communities by Reconstruction of Unobserved States (PICRUSt) analysis was used to predict the function of fecal microbiota. In addition, we evaluated biochemical indices in the plasma.
The α-diversity indices of the meditation and control groups differed significantly. At the genus level, Prevotella and Bacteroides were significantly enriched in the meditation group. According to the LEfSe analysis, two beneficial bacterial genera (Megamonas and Faecalibacterium) were significantly enriched in the meditation group. The functional predictive analysis further showed that several pathways—including glycan biosynthesis, metabolism, and lipopolysaccharide biosynthesis—were significantly enriched in the meditation group. Moreover, plasma levels of clinical risk factors were significantly decreased in the meditation group, including total cholesterol and apolipoprotein B.
The Chinese authors concluded that the intestinal microbiota composition was significantly altered in Buddhist monks practicing long-term meditation compared with that in locally recruited control subjects. Bacteria enriched in the meditation group at the genus level had a positive effect on human physical and mental health. This altered intestinal microbiota composition could reduce the risk of anxiety and depression and improve immune function in the body. The biochemical marker profile indicates that meditation may reduce the risk of cardiovascular diseases in psychosomatic medicine. These results suggest that long-term deep meditation may have a beneficial effect on gut microbiota, enabling the body to maintain an optimal state of health. This study provides new clues regarding the role of long-term deep meditation in regulating human intestinal flora, which may play a positive role in psychosomatic conditions and well-being.
This study is being mentioned on the BBC new-bulletins today – so I thought I have a look at it and check how solid it is. The most obvious question to ask is whether the researchers compared comparable samples.
The investigators collected a total of 128 samples. Subsequently, samples whose subjects had taken antibiotics and yogurt or samples of poor quality were excluded, resulting in 56 eligible samples. To achieve mind training, Tibetan Buddhist monks performed meditation practices of Samatha and Vipassana for at least 2 hours a day for 3–30 years (mean (SD) 18.94 (7.56) years). Samatha is the Buddhist practice of calm abiding, which steadies and concentrates the mind by resting the individual’s attention on a single object or mantra. Vipassana is an insightful meditation practice that enables one to enquire into the true nature of all phenomena. Hardly any information about the controls was provided.
This means that dozens of factors other than meditation could very easily be responsible for the observed differences; nutrition and lifestyle factors are obvious prime candidates. The fact that the authors fail to even discuss these possibilities and more than once imply a causal link between meditation and the observed outcomes is more than a little irritating, in my view. In fact, it amounts to very poor science.
I am dismayed that a respected journal published such an obviously flawed study without a critical comment and that the UK media lapped it up so naively.
In case you have categorized Harry Windsor as an ungrateful brat, you are entirely wrong! He did thank a lot of people – Ophra and Gwyneth Paltrow, for instance. No, I did not read Harry’s bestseller ‘SPARE’. But I did, of course, read the odd report about it simply because it is almost impossible to escape the current press hoo-ha about it.
Most of what I learned is of no interest to me. Some of it, I have to admit, made me concerned about Hary’s wellbeing – after all, we know that chronic drug-taking can severely affect one’s mental health! However, one recent article in Newsweek managed to reassure me on that score:
Among the “professionals, medical experts, and coaches” thanked by the prince for “keeping me physically and mentally strong over the years,” is John Amaral, a Los Angeles-based chiropractor, energy practitioner, author and educator. Amaral is known for his self-developed “energy flow formula,” which combines body and energy work to include mindfulness, meditation and breathing.
This sounded sufficiently relevant for me to look up Amaral. This is what we learn from one website:
Dr. John Amaral is a holistic chiropractor that practices Network Spinal (NSA). This technique helps people release stored tension in their muscles and joints through gentle force adjustments, also known as entrainments. Instead of the traditional cracking or popping of bones that you’re used to seeing at chiropractic offices, John Amaral leverages different energetic intelligences to help people heal physically and emotionally.
Another source tells us the following:
John Amaral is a chiropractor, energy healer and educator who works behind the scenes helping celebrities, entrepreneurs, pro athletes and influencers elevate their energy so they feel and perform their best. John has worked with thousands of people from over 50 countries. He is the Founder of Body Centered Leadership… How much do his sessions cost? According to the Wall Street Journal, a healing session with Amaral will run you $2,500.
And a third website informs us that:
Amaral works with what he calls the “subtle energy body”, which is the energy field around the body that can extend around 3 to 8 feet from the physical body. His work is primarily focused on shifting the tension state of the body and help in freeing up bound-up energy that’s held in different parts of the body. He accesses the energy around the body to achieve this.
In case you have not yet got the drift, take a look at this video; impressive isn’t it?
Yes, Amaral is not cheap but he must be worth it! And because he is such a genial healer, I am confident that we can all relax now knowing that Harry’s health is in such good hands. Personally, I am thrilled by Harry’s hint that there might be a second book in the offing – one with the really dirty linen. I think I might actually buy that one, now that I know how badly he needs the money for keeping healthy.
Yesterday, Harriet’s many friends received the sad news of her unexpected death on 11 January. Harriet was not just a good and loyal friend, she was a tirelessly working, determined, and effective skeptic. Her work focussed on so-called alternative medicine (SCAM), and thus the two of us were on the same wavelength. 
Harriet’s husband, Kirk, posted this short note about her death on social media:
I know Harriet’s work was followed and admired by many of you. It is with great sadness that I must tell you my beloved wife passed away quietly and unexpectedly in her sleep last night. At this moment, she would probably simply ask you to have a kind thought for her, be kind to each other and continue to support her belief in the truth.
I feel that, without intending to, Kirk described Harriet’s character very well. She was a quiet and kind person. Yet she inspired many, and her influence was considerable. Harriet Hall had been the founding member of skeptic organizations, author of books and countless articles, recipient of awards, author of many brilliant lectures, and much more.
Harriet and I have met in person only 2 or 3 times. But we did keep in contact and exchanged many emails. Most generously, she published reviews of most of my books and was often immeasurably supportive of my work.
Harriet Hall will be remembered by skeptics around the world for her quiet enthusiasm, her kindness, and her honesty. I will always remember her for coining an absolutely perfect term for the pseudo-research that plagues the field of SCAM:
TOOTH FAIRY SCIENCE
I lost a friend; the world lost a great skeptic.
We will all miss you, Harriet!
We have discussed the UK conservative MP and arch-Brexiteer, Andrew Bridgen, and his anti-vax stance before. Yesterday, it has been reported that he lost the Tory whip, i.e. he was expelled from the Tory party. The reason for this step is that he had taken to social media and claimed the Covid vaccine to be the “biggest crime against humanity since the holocaust”.
The North West Leicestershire MP has been vocal in remarks questioning the coronavirus vaccine.
On Wednesday he shared an article on vaccines on Twitter, adding: “As one consultant cardiologist said to me, this is the biggest crime against humanity since the Holocaust.”
Renouncing Bridgen’s right to sit as a Tory MP in Parliament, Conservative chief whip Simon Hart said: “Andrew Bridgen has crossed a line, causing great offence in the process. “As a nation, we should be very proud of what has been achieved through the vaccine programme. The vaccine is the best defence against Covid that we have.  “Misinformation about the vaccine causes harm and costs lives. I am therefore removing the whip from Andrew Bridgen with immediate effect, pending a formal investigation.”
“Misinformation about the vaccine causes harm and costs lives. I am therefore removing the whip from Andrew Bridgen with immediate effect, pending a formal investigation.”
Earlier, former Cabinet minister Simon Clarke had condemned his colleague’s tweet referencing the Holocaust, calling it “disgraceful”.
Bridgen is currently already suspended from the Commons after he was found to have displayed a “very cavalier” attitude to the rules in a series of lobbying breaches. MPs agreed on Monday to suspend the North West Leicestershire MP for five sitting days from Tuesday.
Comments from different sources are not flattering for Bridgen:
- Karen Pollock, the chief executive of the Holocaust Educational Trust, said Bridgen’s tweet was “highly irresponsible, wholly inappropriate and an elected politician should know better”.
- Anneliese Dodds, the Labour chair, said: “Andrew Bridgen has been spreading dangerous misinformation on Covid vaccines for some time now. He could have been disciplined weeks ago. “To invoke the Holocaust, as he did today, is utterly shameful, but it should never have reached this point.”
- Andrew Percy, the Conservative MP who is vice-chair of the all-party group against antisemitism, called the comment “disgusting”. Asked by Times Radio if Bridgen should be allowed to stand again, Percy said: “I don’t think anybody who believes this kind of crap should, but that’s a matter for the whips not for me.”
- John Mann, the former Labour MP who is now a non-affiliated peer and the government’s independent adviser on antisemitism, said Bridgen should not be allowed to stand again as a Tory. “There is no possibility that Bridgen can be allowed to stand at the next election,” he said. “He cannot claim that he didn’t realise the level of offence that his remarks cause.”
____________________________
To the best of my knowledge, this is the first time that a UK politician has been punished in this way. But it may well be also the first time that a sitting UK politician has uttered such insane stupidity. Bridgen’s chronic ineptitude is all the more significant as he really should know better. He studied genetics and behaviour at the University of Nottingham and graduated with a degree in biological sciences!
Here are some reactions from people commenting on Twitter about the twit:
- Tory MP, Andrew Bridgen highlights… – Lies in court over family dispute and ordered by judge to pay £800k – Suspended for breaching MP lobbying rules – Thought all Brits entitled to Irish passport after Brexit – Likens vaccines to holocaust What a guy.
- Spreads a dangerous, baseless smear his party colluded in a vaccine Holocaust and at the same time manages to insults victims of a grotesque wartime Holocaust. Conspiracy theorist Andrew Bridgen’s lost the plot. See no way back for the Tory MP now.
- Grubby and despicable: Tory MP Andrew Bridgen loses whip over ‘dangerous’ Covid vaccine claims
- To be fair, Bridgen kept the whip after saying the MI5 knew about the pandemic six months early, then colluded with shadowy elites to impose needless restrictions for their own nefarious ends. So the bar is high.
- Politicians like Andrew Bridgen have succeeded in bringing conspiracy theories into the mainstream. They need to be called out, their arguments dismantled and their political influence cast out to the fringes where it belongs.
- A Holocaust survivor has condemned a Tory MP’s “mind-boggling ignorance” after he compared the mass genocide of Jewish people during World War II to the COVID vaccine rollout
- Many congratulations to Andrew Bridgen on his imminent selection as the Reform Party candidate for North West Leicestershire in the 2024 election
- Andrew Bridgen. Perjury, bullying, misuse of money, months of anti-vaccine garbage, finally loses whip after comparing vaccination to the Holocaust. Scum.
- Six million Jews were murdered in the Holocaust. COVID vaccines have saved millions. The false and outrageous comparisons must end.
- Andrew Bridgen suspended as Tory MP he said: “As one consultant cardiologist said to me, this is the biggest crime against humanity since the Holocaust.” Crucially a cardiologist saying this too. Who are they? Should GMC act in same way as Whips Office?
The prime candidate for the cardiologist in question must, of course, be Aseem Malhotra who also appeared on September 27, 2022, in a press conference with the World Council for Health — a group that has previously spread vaccine misinformation — to call for the “immediate and complete suspension of Covid-19 vaccine.”
Who was it that coined the bon mot: We were all born ignorant but to remain so requires hard work
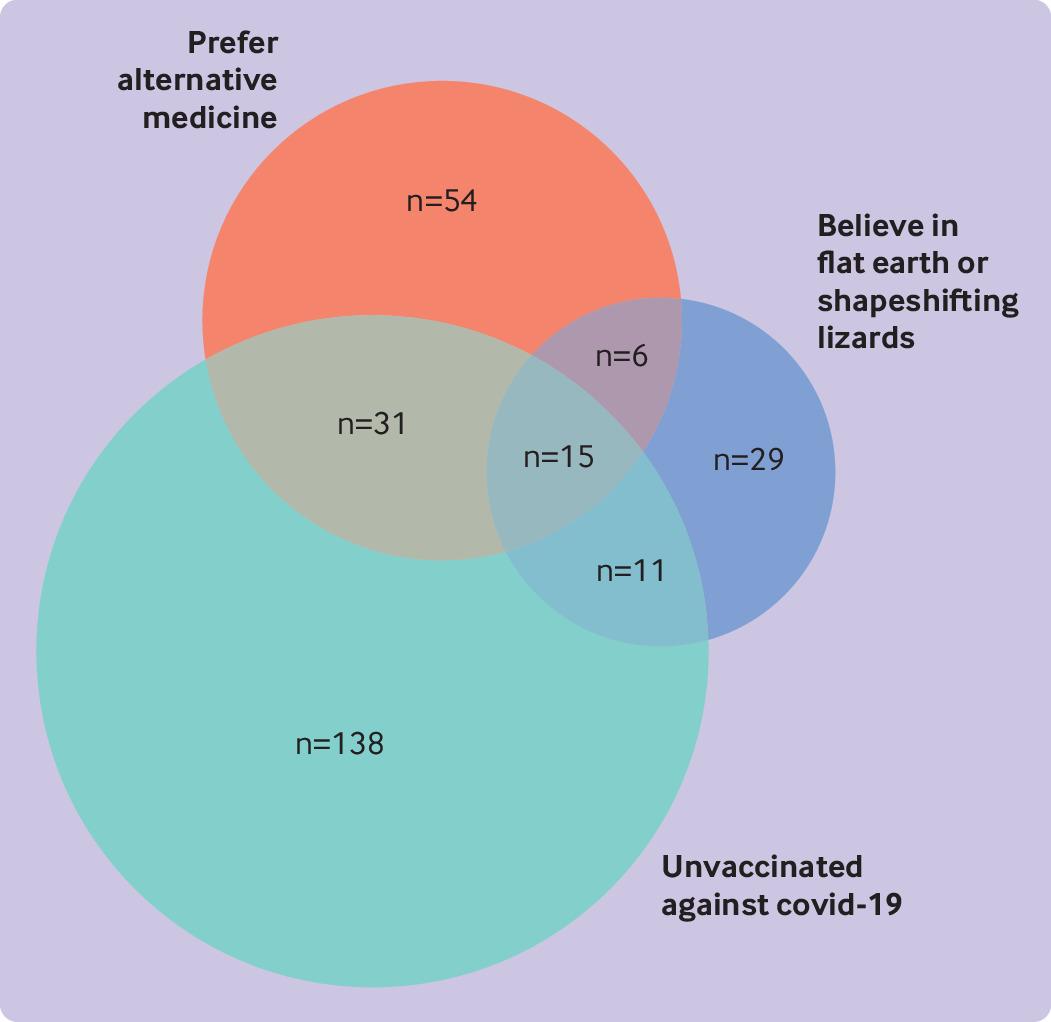
The objective of this cross-sectional survey was to evaluate the beliefs about and attitudes toward cancer prevention of people professing vaccination skepticism or conspiracy theories. Data were collected mainly from a well-known Spanish forum and other platforms, including Reddit (English), 4Chan (English), HispaChan (Spanish), and a Spanish-language website for cancer prevention (mejorsincancer.org) from January to March 2022.
Among 1494 responders, 209 were unvaccinated against covid-19, 112 preferred so-called alternative rather than conventional medicine, and 62 reported flat earth or reptilian beliefs. Cancer beliefs were assessed using the Cancer Awareness Measure (CAM) and Cancer Awareness Measure Mythical Causes Scale (CAM-MYCS), both validated tools.
Awareness of the actual causes of cancer was greater (median CAM score 63.6%) than that of mythical causes (41.7%). The most endorsed mythical causes of cancer were:
- eating food containing additives or sweeteners,
- feeling stressed,
- eating genetically modified food.
Awareness of the actual and mythical causes of cancer among the unvaccinated, alternative medicine, and conspiracy groups was lower than among their counterparts. A median of 54.5% of the actual causes was accurately identified among each of the unvaccinated, alternative medicine, and conspiracy groups, and a median of 63.6% was identified in each of the three corresponding counterparts (P=0.13, 0.04, and 0.003, respectively). For mythical causes, medians of 25.0%, 16.7%, and 16.7% were accurately identified in the unvaccinated, alternative medicine, and conspiracy groups, respectively; a median of 41.7% was identified in each of the three corresponding counterparts (P<0.001 in adjusted models for all comparisons).
In total, 673 (45.0%) participants agreed with the statement “It seems like everything causes cancer.” No significant differences were observed among the unvaccinated (44.0%), conspiracist (41.9%), or alternative medicine groups (35.7%), compared with their counterparts (45.2%, 45.7%, and 45.8%, respectively).
The authors’ conclusions were as follows: we evaluated the patterns of beliefs about cancer among people who believed in conspiracies, rejected the covid-19 vaccine, or preferred alternative medicine. We observed that the participants who belonged to these groups were more likely to endorse mythical causes of cancer than were their counterparts but were less likely to endorse the actual causes of cancer. Almost half of the participants, whether
conspiracists or not, agreed with the statement “It seems like everything causes cancer,” which highlights the difficulty that society encounters in differentiating actual causes of cancer from mythical causes owing to mass (veridical or not) information. This suggests a direct connection between digital misinformation and consequent potential erroneous health decisions, which may represent a further preventable fraction of cancer. Cultivating oriented medical education and scientific literacy, improving online ranking algorithms, building trust, and using effective health communication and social marketing campaigns may be possible ways to tackle this complex public health threat.
This is yet another study showing that so-called alternative medicine (SCAM) usage is linked to misinformation and conspiratorial thinking in other areas. We have discussed similar findings all too often. They are hardly surprising, in my view. As I have repeatedly been trying to point out:
- SCAM use is based mainly on misinformation
- And, to a large extent, SCAM is little more than a conspiracy theory in disguise.
The best way to prevent harm must therefore be to educate the public responsibly (which, of course, is one of the main aims of this blog.
I have tried!
Honestly!
But at present, it is simply not possible to escape the revelations and accusations by Harry Windsor.
So, eventually, I gave in and had a look at the therapy he often refers to. He claims that he is deeply traumatized by what he had to go through and, to help him survive the ordeal, Harry has been reported to use EMDR.
Eye Movement Desensitization and Reprocessing (EMDR) is a fringe psychotherapy that was developed to alleviate the distress associated with traumatic memories. It is supposed to facilitate the accessing and processing of traumatic memories and other adverse life experiences with a view of bringing these to an adaptive resolution. The claim is that, after successful treatment with EMDR therapy, affective distress is relieved, negative beliefs are reformulated, and physiological arousal is reduced.
During EMDR therapy the patient must attend to emotionally disturbing material in brief sequential doses while simultaneously focusing on an external stimulus. Therapist-directed lateral eye movements are commonly used as external stimulus but a variety of other stimuli including hand-tapping and audio stimulation can also be employed.
Francine Shapiro, the psychologist who invented EMDR claims to have serendipitously discovered this technique by experiencing spontaneous saccadic eye movements in response to disturbing thoughts during a walk in the woods. Yet, as GM Rosen explains, this explanation is difficult to accept because normal saccadic eye movements appear to be physiologically undetectable and are typically triggered by external stimuli.
Shapiro hypothesizes that EMDR therapy facilitates the access to the traumatic memory network, so that information processing is enhanced, with new associations forged between the traumatic memory and more adaptive memories or information. These new associations are alleged to result in complete information processing, new learning, elimination of emotional distress, and development of cognitive insights.
EMDR therapy uses a three-pronged protocol:
- (1) the past events that have laid the groundwork for dysfunction are processed, forging new associative links with adaptive information;
- (2) the current circumstances that elicit distress are targeted, and internal and external triggers are desensitized;
- (3) imaginal templates of future events are incorporated, to assist the client in acquiring the skills needed for adaptive functioning.
The question I ask myself is, of course: Does EMDR work?
The evidence is mixed and generally flimsy. A systematic review showed that “limitations to the current evidence exist, and much current evidence relies on small sample sizes and provides limited follow-up data”.
What might be particularly interesting in relation to Harry Windsor is that EMDR techniques have been associated with memory-undermining effects and may undermine the accuracy of memory, which can be risky if patients, later on, serve as witnesses in legal proceedings.
Personally, I think that Harry’s outbursts lend support to the hypothesis that EMDR is not effective. In the interest of the royal family, we should perhaps see whether so-called alternative medicine (SCAM) does offer an effective treatment against navel gazing?
It has been reported that a German consumer association, the ‘Verbraucherzentrale NRW’, has first cautioned the manufacturer MEDICE Arzneimittel Pütter GmbH & Co. and then sued them for misleading advertising statements. The advertisement in question gave the wrong impression that their homeopathic remedy MEDITONSIN would:
- for certain generate a health improvement,
- have no side effects,
- be superior to “chemical-synthetic drugs”.
The study used by the manufacturer in support of such claims was not convincing according to the Regional Court of Dortmund. The results of a “large-scale study with more than 1,000 patients” presented a pie chart indicating that 90% of the patients were satisfied or very satisfied with the effect of Meditonsin. However, this was only based on a “pharmacy-based observational study” with little scientific validity, as pointed out by the consumer association. Despite the lack of evidence, the manufacturer claimed that their study “once again impressively confirms the good efficacy and tolerability of Meditonsin® Drops”. The Regional Court of Dortmund disagreed with the manufacturer and agreed with the reasoning of the consumer association.
“It is not permitted to advertise with statements that give the false impression that a successful treatment can be expected with certainty, as suggested by the advertising for Meditonsin Drops,” emphasizes Gesa Schölgens, head of “Faktencheck Gesundheitswerbung,” a joint project of the consumer centers of North Rhine-Westphalia and Rhineland-Palatinate. According to German law, this is prohibited. In addition, the Regional Court of Dortmund considered consumers to be misled by the advertising because the false impression was created that no harmful side effects are to be expected when Meditonsin Drops are taken. The package insert of the drug lists several side effects, according to which there could even be an initial worsening of symptoms after taking the drug.
The claim of advantages of the “natural remedy” represented by the manufacturer in comparison with “chemical-synthetic medicaments, which merely suppress the symptoms”, was also deemed to be inadmissible. Such comparative advertising is inadmissible.
__________________________________
This ruling is, I think, interesting in several ways. The marketing claims of so-called alternative medicine (SCAM) products seem all too often not within the limits of the laws. One can therefore hope that this case might inspire many more legal cases against the inadmissible advertising of SCAMs.
You, the readers of this blog, have spoken!
The WORST PAPER OF 2022 competition has concluded with a fairly clear winner.
To fill in those new to all this: over the last year, I selected articles that struck me as being of particularly poor quality. I then published them with my comments on this blog. In this way, we ended up with 10 papers, and you had the chance to nominate the one that, in your view, stood out as the worst. Votes came in via comments to my last post about the competition and via emails directly to me. A simple count identified the winner.
It is PAUL VARNAS, DC, a graduate of the National College of Chiropractic, US. He is the author of several books and has taught nutrition at the National University of Health Sciences. His award-winning paper is entitled “What is the goal of science? ‘Scientific’ has been co-opted, but science is on the side of chiropractic“. In my view, it is a worthy winner of the award (the runner-up was entry No 10). Here are a few memorable quotes directly from Paul’s article:
- Most of what chiropractors do in natural health care is scientific; it just has not been proven in a laboratory at the level we would like.
- In many ways we are more scientific than traditional medicine because we keep an open mind and study our observations.
- Traditional medicine fails to be scientific because it ignores clinical observations out of hand.
- When you think about it, in natural health care we are much better at utilizing the scientific process than traditional medicine.
But I am surely doing Paul an injustice. To appreciate his article, please read his article in full.
I am especially pleased that this award goes to a chiropractor who informs us about the value of science and research. The two research questions that undoubtedly need answering more urgently than any other in the realm of chiropractic relate to the therapeutic effectiveness and risks of chiropractic. I just had a quick look in Medline and found an almost complete absence of research from 2022 into these two issues. This, I believe, makes the award for the WORST PAPER OF 2022 all the more meaningful.
PS
Yesterday, I wrote to Paul informing him about the good news (as yet, no reply). Once he provides me with a postal address, I will send him a copy of my recent book on chiropractic as his well-earned prize. I have also invited him to contribute a guest post to this blog. Watch this space!