The impact of drug-induced liver injury (DILI) on patients with chronic liver disease (CLD) is unclear. There are few reports comparing DILI in CLD and non-CLD patients. In this study, the researchers aimed to determine the incidence and outcomes of DILI in patients with and without CLD.
They collected data on eligible individuals with suspected DILI between 2018 and 2020 who were evaluated systematically for other etiologies, causes, and the severity of DILI. They compared the causative agents, clinical features, and outcomes of DILI among subjects with and without CLD who were enrolled in the Thai Association for the Study of the Liver DILI registry. Subjects with definite, or highly likely DILI were included in the analysis.
The researchers evaluated the causal relationship between the clinical pattern of liver injury and the suspected drugs or SCAM products with the Roussel Uclaf Causality Assessment Method (RUCAM) system. RUCAM is a validated and established tool to quantitatively assess causality in cases of suspected DILI and/or SCAM product-induced liver injury. They also used the Clinical Assessment of Causality Scale to assess the association as definite (>95% likelihood), highly likely (75–95%), probable (50–74%), possible (25–49%) or unlikely (<25%).
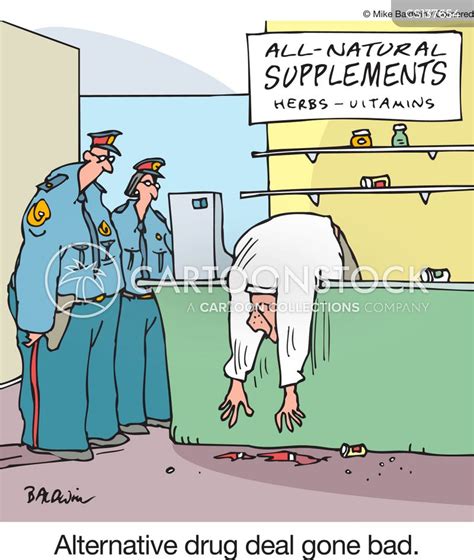
A total of 200 subjects diagnosed with DILI were found in the registry. Of those, 41 had CLD and 159 had no evidence of CLD. So-called alternative medicine (SCAM) products were identified as the most common class of DILI agents. Approximately 59% of DILI in the CLD and 40% in non-CLD group were associated with SCAM use. Individuals with pre-existing CLD had similar severity including mortality. Twelve patients (6%) developed adverse outcomes related to DILI including seven (3.5%) deaths and five (2.5%) with liver failure. Mortality was 4.88% in CLD and 3.14% in non-CLD subjects over median periods of 58 (8-106) days and 22 (1-65) days, respectively.
The authors concluded that, in this liver disease registry, the causes, clinical presentation, and outcomes of DILI in subjects with CLD and without CLD patients were not different. Further study is required to confirm our findings.
Consumers often prefer SCAM to conventional medicine because SCAM is viewed as gentle and safe. The notions are that they
- are natural and therefore harmless;
- have been in use for ages and thus have stood the test of time.
Readers of this blog will appreciate that both notions are, in fact, fallacies:
- appeal to nature;
- appeal to tradition.
This new paper is an impressive reminder that SCAM’s reputation as a safe option is not justified, and that SCAM relies more on fallacies than on facts.

Ashwaganda is a case in point. A friend was taking it for anxiety and over a period of weeks developed severe nausea and exhaustion. On returning to the scammer who prescribed it he was told it was working and to increase the dose! Needless to say he got worse.
It only took me a few minutes research to show him this was a common and potentially dangerous effect carrying the risk of liver damage. He stopped taking it and recovered with a week, hopefully with no long term damage. But even now he still believes in scam, just thinking that this particular one doesn’t suit him.
Withania somnifera (L.) Dunal, commonly known as:
• ashwaganda
• ashwagandha
• winter cherry
See:
https://edzardernst.com/?s=ashwagandha
@Socrates
Strange, as ashwaganda is not normally associated with liver problems, also see https://www.ncbi.nlm.nih.gov/books/NBK548536/
But as the above article already says, it is quite likely that the preparation was adulterated with other, rather more toxic ingredients – especially if those preparations were purchased directly from India as ‘traditional medicine’.
I guess this is one the great advantages of ‘health freedom’ (read: uncontrolled quackery) and the way that herbs and supplements are regulated (as in: not).
If it weren’t so sad, I’d almost laugh at all those gullible people who are scared stiff of even the smallest traces of ‘chemicals’ in their food and water, but don’t think twice when plonking down their hard-earned money for ‘herbal medicines’ containing thousands of times the safe limit of highly toxic substances …
I agree the liver damage risk may be low and possibly due to contaminant. The risk of nausea, stomach upsets and diarrhoea however seems to be quite high and in my friends case quite severe. I saw this first hand when we all went out for dinner and he had to leave the room 3 times during the first course – we didn’t make it to a second. Hard to see how this would help with anxiety.
But the shocking thing was that his ‘therapist’ saw this as the herb working to expel the toxins causing his anxiety and increasing the dose.
@Socrates
Perhaps this was a shock-exposure-style ‘therapy’? Most healthy people would already be mortified by what you describe – so anxiety patients will likely be absolutely overwhelmed by fear and embarrassment in situations like this. So I’d say it’s a typical case of kill or cure …
Ah, yes, if something appears to have an exceedingly strong effect already, up the dose!
To make it abundantly clear that I’m being cynical here: this ‘therapist’ is a danger for society. And then stupid quacks like these even feel insulted when we call them stupid quacks …
This paper describes a potential mechanism by which it causes liver damage:
https://www.sciencedirect.com/science/article/pii/S2666027X21000074
“Withania somnifera, commonly known as Ashwagandha, is a medicinal plant used for thousands of years for various remedies. Extracts of Ashwagandha contain more than 200 metabolites, with withanone (win) being one of the major ones responsible for many of its medicinal properties. Recently, several cases of liver toxicity resulting from commercially available Ashwagandha products have been reported. The first report of Ashwagandha-related liver damage was from Japan, which was quickly resolved after drug-withdrawal. Later, similar cases of liver toxicity due to Ashwagandha consumption were reported from the USA and Iceland. Towards understanding the liver toxicity of Ashwagandha extracts, we studied win, a representative withanolide having toxicophores or structural alerts that are commonly associated with adverse drug reactions. We found that win can form non-labile adducts with the nucleosides dG, dA, and dC. Using various biochemical assays, we showed that win forms adducts in DNA and interfere with its biological property. Win also forms adducts with amines and this process is reversible. Based on the data presented here we concluded that win is detoxified by GSH but under limiting GSH levels it can cause DNA damage. The work presented here provides a potential mechanism for the reported Ashwagandha-mediated liver damage.”