bogus claims
Past life regression therapy (PLRT) is, according to one practitioner, a therapeutic technique for accessing and re-experiencing your past lives directly. A branch of hypnotherapy, past life regression therapy has grown over the last 50 years to be an important addition to the healing arts. This website also informs us that:
Past life regression is an amazing, full-sensory experience. You might experience the memory as a vivid movie, or see only vague flashes of images that prompt the narrative. You might hear gunshots or explosions on a battlefield, or music at a dance. It is possible to recall smells too: smoke from a fire, leather from a saddle, or the sweat of a dirty body.
As the story unfolds, you feel real emotions appropriate to the story. You may cry when you re-experience deep sadness at the death of a beloved child, feel despair in the pit of your stomach as you witness a massacre, or elation at a long-awaited homecoming from war. And just as you can recall strong emotions, you feel the pain of an arrow piercing your body as you are dying, or the heaviness of a load you’re carrying on your back. These physical sensations and emotions are very real in the moment, but pass quickly as you move through the past life story and death.
PLRT is used by some clinicians for anxiety disorders, mood disorders, gender dysphoria, and other conditions. One survey suggested that 22% of European cancer patients use PLRT as a so-called alternative medicine (SCAM) to treat their illness. Some proponents argue that, since the exploration of the event/memory is actually helping the client resolve the challenge, the overall process can have immense therapeutic benefit, provided it is done responsibly and effectively.
So, it is effective because it is effective??? Such assurances make my alarm bells ring loud and clear. And I am not alone. It has been argued that PLRT is unethical:
- First, it is not evidence-based. Past life regression is based on the reincarnation hypothesis, but this hypothesis is not supported by evidence, and in fact, it faces some insurmountable conceptual problems. If patients are not fully informed about these problems, they cannot provide informed consent, and hence, the principle of autonomy is violated.
- Second, past life regression therapy has the great risk of implanting false memories in patients, and thus, causing significant harm. This is a violation of the principle of non-malfeasance, which is surely the most important principle in medical ethics.
I was unable to find convincing evidence that PLRT is effective. Furthermore, PLRT is by no means cheap; a typical session lasts two hours and costs $350. This suggests that PLRT is
- unproven,
- expensive,
- and unsafe.
In other words, it is not a therapeutic option that I would recommend to anyone for any condition.
Mesotherapy is a treatment where fine needles or a high-pressure ‘gun’ are used to inject vitamins, enzymes, hormones, plant extracts, etc. into the skin of a patient. Michel Pistor, a French doctor, developed the therapy in 1952. It was originally used to relieve pain. Today, mesotherapy is also employed for a range of further indications:
- remove fat in areas like the stomach, thighs, buttocks, hips, legs, arms, and face
- reduce cellulite
- fade wrinkles and lines
- tighten loose skin
- recontour the body
- lighten pigmented skin
- treat alopecia, a condition that causes hair loss
Mesotherapy is said to deliver drugs into the middle layer (mesoderm) of the skin. It is claimed to correct underlying issues like poor circulation and inflammation that cause skin damage.
Many different drugs can be used for mesotherapy, including:
- prescription medicines like vasodilators and antibiotics
- hormones such as calcitonin and thyroxin
- enzymes like collagenase and hyaluronidase
- herbal extracts
- homeopathic remedies
- vitamins and minerals
- vaccines
According to the Italian Mesotherapy Society, the mechanisms of action of mesotherapy can be summarised as follows:
But is there at all any sound evidence that mesotherapy works?
It turns out that there are few rigorous studies. The most recent review concluded that mesotherapy proved to be more effective than systemic therapy in the treatment of local pain and functional limitations caused by a variety of musculoskeletal conditions. However, because of the heterogeneity of the analysed studies in terms of injected drugs, administration technique, associated treatments, frequency and total number of sessions, more randomized controlled trials are needed, comparing a standardized mesotherapy protocol with a systemic treatments.
Mesotherapy is not free of serious adverse effects. They include bacterial infections, hair loss, scarring, panniculitis, tissue necrosis, allergic reactions, and other complications.
So, is mesotherapy a treatment that might be recommended?
- Its effectiveness remains unproven.
- It can cause serious adverse effects.
- It is by no means cheap.
I think these facts answer the question fairly well.
I came across a little article by the homeopathy firm Boiron. Normally, I would not mention such promotional literature, but this one is special. Here it is:
These days, leaving home is an exercise in mental fortitude with trying to remember your mask, packing enough hand sanitizer, and taking a host of other precautions. Our daily routines have been upended, leaving us on high alert. As each day brings a new set of challenges — like hybrid learning or work closures — it’s easy for our confidence and self-esteem to take a hit.
If these feelings begin to hold you back, health professionals like Heidi Weinhold, ND, recommend turning to Gelsemium sempervirens. “I think of this remedy whenever I need help facing my fears,” she says.
Dr. Weinhold recommends Gelsemium sempervirens 30C for anyone experiencing nervousness from anticipatory or situational stress. “For college students, that could mean test anxiety before an exam. Some of us are having fears of getting back on a plane or flying, or even going to the grocery store and shopping.”
Gelsemium has a long history as a stress reducer. According to Dr. Weinhold, this remedy was found in Civil War first aid kits where it was used to help give soldiers courage before walking on to the battlefield. Now Gelsemium, too, can help you face your battles and provide you with the strength to persevere through tough times, she says.
Click here to watch this video featuring Dr. Weinhold explaining the uses and benefits of Gelsemium sempervirens.
The short article begs, of course, many questions. What, for instance, is Gelsemium sempervirens? It is a plant sometimes used as a folk remedy for various medical conditions. It looks a bit like honeysuckle but is quite toxic due to the alkaloids that it contains.
Is there any evidence that Gelsemium sempervirens is effective for any condition? No! But that does not matter in the context of homeopathy because a C30 potency would not contain a single molecule of the plant anyway.
And who is Dr. Heidi Weinhold? According to her own website, she
received her Bachelor’s Degree in Biology from Washington & Jefferson College. Dr. Weinhold completed a four-year doctoral program in Naturopathic Medicine from Southwest College of Naturopathic Medicine in Tempe, Arizona. Her studies included drug-herb interactions, homeopathic intakes, dialoguing with physicians, and incorporating natural modalities to enhance conventional treatment. Dr. Weinhold spent 9 months doing supervised clinical rotations through Arizona Pathways, a drug Rehabilitation Community Center, where she provided Naturopathic support to individuals recovering from addiction. In 2013 she received the Alumni Award from Southwest College in recognition of her contribution towards the advancement of Naturopathic Medicine. In 2017, Southwest College further honored Dr. Weinhold by bestowing upon her an honorary Doctorate of Humane Letters.
From 2008-2016, Dr. Weinhold served as the legislative chair for the Pennsylvania Association of Naturopathic Physicians (PANP), working with legislators to promote legislation to license Naturopathic Doctors in Pennsylvania. A giant step towards this effort was achieved with the passage of House Bill 516 in 2016. HB 516 provides title protection and registration for Naturopathic Physicians graduating from accredited Naturopathic Medical Colleges. Full licensure efforts are currently underway. Dr. Weinhold received the 2017 Physician of the Year Award from the Pennsylvania Association of Naturopathic Physicians.
Fascinating! I am particularly interested in her studies of drug-herb interactions, homeopathic intakes, dialoguing with physicians, and incorporating natural modalities to enhance conventional treatment. So I looked her up on Medline: nothing! Heidi has not a single publication in her name.
Now, that’s surprising. It could mean that her studies were too important to be published and the findings are still top secret. Dr. Weinhold has received a prestigious award for advancing naturopathic medicine; it, therefore, stands to reason that we can very soon expect the announcement of a major breakthrough regarding the medicinal powers of homeopathic Gelsemium sempervirens preparations that are devoid of any molecules of Gelsemium sempervirens.
I for one am looking forward to it.
This shocking paper presents 5 cases of patients with moderate to severe COVID-19 infections, 2 of them hospitalized in the intensive care unit, who were successfully treated with homeopathy. All 5 patients responded to homeopathic treatment in an unexpectedly short time span (in fact, it took up to 8 days), improving both physically and mentally.
The authors concluded that the present case series emphasizes the rapidity of response among moderate to severely ill patients to homeopathic treatment, when conventional medical options have been unable to relieve or shorten the disease. The observations described should encourage use of homeopathy in treating patients with COVID-19 during the acute phase of the disease.
If I hear about patients suffering from a cold, or tennis elbow, or otitis, or back pain, or allergy who responded to homeopathic treatment in an unexpectedly short time span, I tend to giggle and usually consider it a waste of time to explain that the observed outcome most likely is not a RESPONSE to homeopathic treatment but a non-causally related by-product. Correlation is not causation! What caused the outcome was, in fact, the natural history of the condition which would have improved even without homeopathy. To make this even clearer, I sometimes ask the homeopath: HOW DO YOU KNOW THAT THE PATIENT WOULD NOT HAVE IMPROVED EVEN FASTER IF YOU HAD NOT GIVEN HIM THE HOMEOPATHIC REMEDY? This question sometimes (sadly not always) leads to the realization that homeopathy may not have caused the outcome.
But when, in the middle of a pandemic during which millions of people died and continue to die, someone writes in a medical journal that 5 COVID patients responded to homeopathic treatment in an unexpectedly short time span, I feel compelled to disclose the statement as pure, unethical, irresponsible, and dangerous quackery.
The 5 patients with COVID-19 were hospitalized at a tertiary medical center in Jerusalem for moderate to severe
COVID-19-related symptoms. Each of them requested homeopathic treatment in addition to conventional therapy from the hospital’s ‘Center for Integrative Complementary Medicine’. All 5 patients were over 18 years old and had confirmed COVID-19 infection at the time of admission. They received their homeopathic medications as small round pills (globules); no further information about the homeopathic treatment was provided. Similarly, we also do not learn whether some patients who did not receive homeopathy recovered just as quickly (I am sure that worldwide thousands did), or whether some patients who did get homeopathic remedies failed to recover.
To make matters worse, the authors of this paper state this:
Several conclusions are evident from the cases presented:
1 homeopathy’s effect may be expected within minutes or, at most, hours;
2 contrary to classical homeopathic consultations, which may extend over an hour, correct medications for patients with acute COVID-19 symptoms may be determined in minutes;
3 there were no observable adverse effects to homeopathic treatment of COVID-19;
4 therapy can be administered via telehealth services, increasing safety of treating patients with active infection;
5 patient satisfaction was high; scoring their experience of homeopathic therapy on a 7-point scale, ranging
from “It greatly improved my condition” to “It greatly aggravated my condition,” all 5 patients indicated it
had greatly improved their condition.
The possibility that the outcomes are not causally related to the homeopathic treatment seems to have escaped the authors. The harm that can be done by such an article seems obvious: fans of homeopathy might be misled into assuming that homeopathy is an effective therapy for COVID infections and other serious conditions. It is not hard to imagine that this error would cost many lives.
The authors state in their article that, to the best of their knowledge, this is the first time that a tertiary medical center has permitted homeopathic therapy of patients under treatment for COVID-19-related illness.
I sincerely hope that it is also the last time!
They say, one has to try everything at least once – except line-dancing and incest. So, when I was invited to co-organize a petition, I considered it and thought: WHY NOT?
Here is the text (as translated by myself) of our petition to the German Medical Association:
Dear President Dr Reinhardt,
Dear Ms Lundershausen,
Mrs Held,
Dear Ms Johna,
We, the undersigned doctors, would like to draw your attention to the insistence of individual state medical associations on preserving “homeopathy” as a component of continuing medical education. We hope that you, by virtue of your office, will ensure a nationwide regulation so that this form of sham treatment [1], as has already happened in other European countries, can no longer call itself part of medicine.
We justify our request by the following facts:
- After the landmark vote in Bremen in September 2019 to remove “homeopathy” from the medical training regulations, 10 other state medical associations have so far followed Bremen’s example. For reasons of credibility and transparency, it would be desirable if the main features of the training content taught were not coordinated locally in the future, but centrally and uniformly across the country so that there is no “training tourism”. Because changes to a state’s own regulations of postgraduate training are only binding for the examination committee of the respective state, this does not affect national regulations but is reduced to only a symbolic character without sufficient effects on the portfolio of medical education nationwide.
- Medicine always works through the combination of a specifically effective part and non-specific placebo effects. By insisting on a pseudo-medical methodology – as is “homeopathy” represents in our opinion – patients are deprived of the specific effective part and often unnecessarily deprived of therapy appropriate to the indication. Tragically, it happens again and again that the “therapeutic window of opportunity” for an appropriate therapy is missed, tumors can grow to inoperable size, etc.
- Due to the insistence of individual state medical associations on the “homeopathic doctrine of healing” as part of the medical profession, we are increasingly exposed to the blanket accusation that, by tolerating this doctrine, we are supporting and promoting ways of thinking and world views that are detached from science. This is a dangerous situation, which in times of a pandemic manifests itself in misguided aggression reflected not just in vaccination skepticism and vaccination refusal, but also in unacceptable personal attacks and assaults on vaccinating colleagues in private practice.
Responsible:
Dr. med. Dent. Hans-Werner Bertelsen
Prof. Dr. med. Edzard Ernst
George A. Rausche
You can sign the petition here:
It has recently been reported that a Canadian naturopath claims he can treat autism with fecal transplants at a clinic in Mexico. The College of Naturopathic Physicians of B.C. has thus barred him stating that it has taken “extraordinary action” against Jason Klop in response to a complaint from a whistle-blowing former employee, who alleges that he manufactured these products in a “household lab” in B.C. without standard procedures or quality control.
While the complaint is under investigation, Klop cannot manufacture, advertise or sell fecal microbiota transplants (FMT). He’ll also be subject to random on-site audits to make sure he’s not violating his conditions.
This is the first public sign of concrete action by the college since CBC News reported on Klop’s business in January 2020 — nearly 20 months ago. Klop has been charging about $15,000 US for autistic children as young as two years old to have FMT treatment at a clinic near Tijuana. The process isn’t approved as a treatment of autism and carries serious risks of infection.
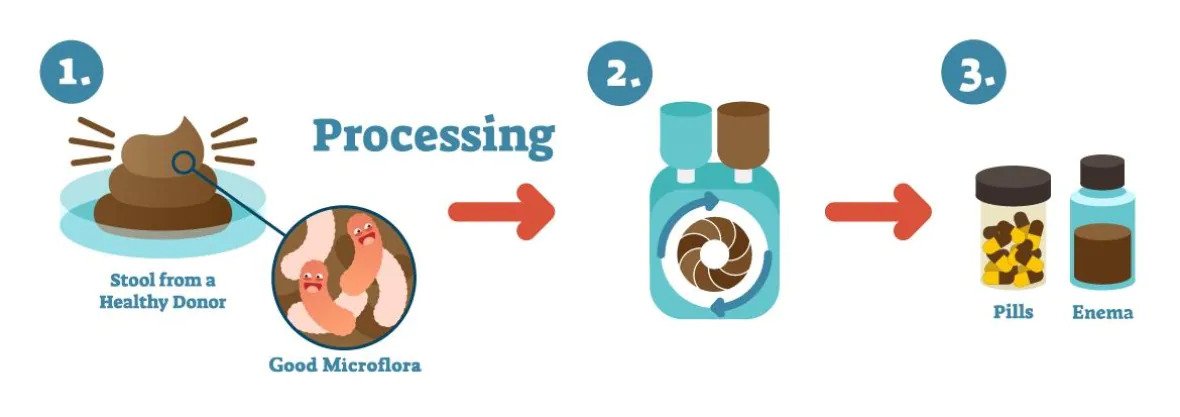
An illustration shows how fecal microbiota transplants are produced. (Vancouver Island Health Authority)
In a promotional video posted in January, Klop says he believes that “precision manipulation of the gut microbiome will solve every single chronic disease.” He also issued an affidavit boasting that he has a new lab that “produces the best and safest FMT materials in the world” and described the former employee who complained as “manifestly unreliable.” Klop argued that “lives are at stake” if he were to stop what he’s doing and described his therapy as a “life-saving measure.”
_____________________
Is there any evidence at all for FMT as a treatment of autism? A recent systematic review drew this conclusion: evidence from human studies suggesting beneficial effects of probiotic, prebiotic, and combination thereof, as well as fecal transplants in autism spectrum disorder, is limited and inconclusive.
I was alerted to this announcement by the Faculty of Homeopathy:
Faculty of Homeopathy Accredited Education
The role of Dentistry in Integrative Medicine and Homeopathy
Dentistry appears to be the Cinderella of healthcare and the importance of good oral health is hugely underestimated. The mouth is the portal into the rest of our bodies. There is increasing evidence proving that health of the oral cavity has strong links with the health of the rest of the body especially increasing risk of heart disease, low birth weight babies and type 2 diabetes. The aim of this webinar is to highlight the vital importance of dentistry and oral health in integrative medicine and why healthcare professionals need to work closely with dentists. It will also cover how, as homeopaths, we can appreciate symptoms in the mouth as indications of general health or disease and manage dental conditions.
THE TICKETS FOR THIS WEBINAR ARE LIMITED THEREFORE, PLEASE REGISTER NOW TO ENSURE ACCESS.
Some splendid platitudes there:
- the Cinderella of healthcare
- The mouth is the portal into the rest of our bodies
- health of the oral cavity has strong links with the health of the rest of the body…
But what about the importance of dentistry in integrative medicine? The importance of dentistry in medicine is fairly clear to me. However, what is the importance of dentistry in integrative medicine?
Even more puzzling seems the ‘role of dentistry in homeopathy’? What on earth do they mean by that? Perhaps they meant the ‘role of homeopathy in dentistry’?
And what is the role of homeopathy in dentistry? The British Homeopathic Dental Association should know, shouldn’t they? On their website, they explain that they are a group of dentists and dental care professionals that have an interest in using homeopathy alongside our dentistry.
On the basis of what evidence, you ask? They kindly provide an answer to that question:
In dentistry there is limited research though studies have shown improved bone healing around implants with Symphytum and reduced discomfort and improved healing time with ulcers and beneficial in oral lichen planus. These studies have small numbers and are not generally acepted as stong evidence.
Are they trying to tell us that there is no good evidence? Looks like it, doesn’t it? In this case, the above Webinar seems rather superfluous.
For those of you who want to save the money for the tickets, here is a full and evidence-based summary of all the conditions where homeopathy might be helpful in dentistry:
–
–
–
–
–
–
–
–
–
–
–
–
–
–
–
–
THE END
Homeopaths believe that their remedies work for every condition imaginable and that naturally includes irritable bowel syndrome (IBS). But what does the evidence show?
The aim of this pilot study was to evaluate the efficacy of individualized homeopathic treatment in patients with IBS. The study was carried out at the National Homeopathic Hospital of the Secretary of Health, Mexico City, Mexico and included 41 patients: 3 men and 38 women, mean age 54 ± 14.89 years, diagnosed with IBS as defined by the Rome IV Diagnostic criteria. Single individualized homeopathics were prescribed for each patient, taking into account all presenting symptoms, clinical history, and personality via repertorization using RADAR Homeopathic Software. The homeopathic remedies were used at the fifty-millesimal (LM) potency per the Mexican Homeopathic Pharmacopoeia starting with 0/1 and increasing every month (0/2, 0/3, 0/6). Severity scales were applied at the beginning of treatment and every month for 4 months of treatment. The evaluation was based on comparing symptom severity scales during treatment.
The results demonstrated that 100% of patients showed some improvement and 63% showed major improvement or were cured. The study showed a significant decrease in the severity of symptom scores 3 months after the treatment, with the pain score showing a decrease already one month after treatment.
The authors state that the results highlight the importance of individualized medicine regimens using LM potency, although the early decrease in pain observed could also be due to the fact that Lycopodium clavatum and Nux vomica were the main homeopathic medicine prescribed, and these medicines contain many types of alkaloids, which have shown significant analgesic effects on pain caused by physical and chemical stimulation.
The authors concluded that this pilot study suggests that individualized homeopathic treatment using LM potencies benefits patients with IBS.
Where to begin?
Let me mention just a few rather obvious points:
- A pilot study is not for evaluating the efficacy, but for testing the feasibility of a definitive trial.
- The study has no control group, therefore the outcome cannot be attributed to the treatment but is most likely due to a mixture of placebo effects, regression towards the mean, and natural history of IBS.
- The conclusions are not warranted.
- The paper was published in the infamous Altern Ther Health Med.
Just to make sure that nobody is fooled into believing that homeopathy might nonetheless be effective for IBS. Here is what the Cochrane review on this subject tells us: no firm conclusions regarding the effectiveness and safety of homeopathy for the treatment of IBS can be drawn. Further high quality, adequately powered RCTs are required to assess the efficacy and safety of clinical and individualised homeopathy for IBS compared to placebo or usual care.
In my view, even the conclusion of the Cochrane review is odd and slightly misleading. The correct conclusion would have been something more to the point:
THE CURRENT TRIAL EVIDENCE FAILS TO INDICATE THAT HOMEOPATHY IS AN EFFECTIVE TREATMENT FOR IBS.
This study aimed to assess the feasibility of a future definitive trial, with a preliminary assessment of differences between effects of individualized homeopathic (IH) medicines and placebos in the treatment of cutaneous warts.
A double-blind, randomized, placebo-controlled trial (n = 60) was conducted at the dermatology outpatient department of the Homoeopathic Medical College and Hospital, West Bengal. Patients were randomized to receive either IH (n = 30) or identical-looking placebos (n = 30). The primary outcome measures were numbers and sizes of warts; the secondary outcome measure was the Dermatology Life Quality Index (DLQI) questionnaire measured at baseline, and every month up to 3 months. Group differences and effect sizes were calculated on the intention-to-treat sample.
Attrition rate was 11.6% (IH, 3; placebo, 4). Intra-group changes were significantly greater in the IH group than in the placebo group. Inter-group differences were statistically non-significant (all p > 0.05, Mann-Whitney U tests) with small effect sizes, both in the primary outcomes (number of warts after 3 months: IH median [interquartile range; IQR] 1 [1, 3] vs. placebo 1 [1, 2]; p = 0.741; size of warts after 3 months: IH 5.6 mm [2.6, 40.2] vs. placebo 6.3 [0.8, 16.7]; p = 0.515) and in the secondary outcomes (DLQI total after 3 months: IH 4.5 [2, 6.2] vs. placebo 4.5 [2.5, 8]; p = 0.935). Thuja occidentalis (28.3%), Natrum muriaticum (10%), and Sulphur (8.3%) were the most frequently prescribed medicines. No homeopathic aggravations or serious adverse events were reported.
The authors concluded that, as regards efficacy, the preliminary study was inconclusive, with a statistically non-significant direction of effect favoring homeopathy. The trial succeeded in showing that an adequately powered definitive trial is both feasible and warranted.
Partly the same group of authors recently published another trial of homeopathy with similar findings. At the time, I commented as follows:
We have come across this terminology before; homeopaths seem to like it. It prevents them from calling a negative trial by its proper name: A NEGATIVE TRIAL. In their view
- a positive trial is a study where homeopathy yields better results than placebo,
- a negative trial is a study where placebo yields better results than homeopathy,
- an inconclusive trial is a study where homeopathy yields results that are not significantly different from placebo.
Is this silly?
Yes, it is completely bonkers!
Is it dishonest?
Yes, in my view, it is.
Why is it done nonetheless?
Perhaps a glance at the affiliations of the authors provides an answer. And here is the list of the affiliations of the trialists of the present cutaneous wart study:
- 1Department of Repertory, D.N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 2D.N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 3Department of Organon of Medicine and Homoeopathic Philosophy, The Calcutta Homoeopathic Medical College and Hospital, Kolkata, West Bengal, India.
- 4Department of Practice of Medicine, The Calcutta Homoeopathic Medical College and Hospital, Kolkata, West Bengal, India.
- 5Department of Repertory, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Kolkata, West Bengal, India.
- 6Department of Organon of Medicine and Homoeopathic Philosophy, D.N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
- 7Department of Pediatrics, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 8Department of Organon of Medicine and Homoeopathic Philosophy, State National Homoeopathic Medical College and Hospital, Lucknow, Uttar Pradesh.
- 9Independent Researcher; Champsara, Baidyabati, Hooghly, West Bengal, India.
- 10Independent Researcher, Shibpur, Howrah, West Bengal, India.
And, as before, this paper also contains this statement:
Conflict of interest statement
None declared.
Bromelain, papain and chymotrypsin are proteolytic enzymes. They can be found in fruits such as pineapple or papaya, but also in the human body, namely in the pancreas. Besides their enzymatic functions, they have long been said to have a wide range of positive health effects. For instance, it is claimed that they reduce side effects and even improve the outcome of cancer therapies. This systematic review examined the existing evidence on the role that these enzymes which are available as food supplements might play in cancer treatment.
A total of 15 studies with 3,008 patients could be included in this systematic review. Patients treated with enzymes were diagnosed with various entities of gastrointestinal, gynecologic, head and neck, and lung cancer as well as hematological malignancies. The therapy concepts included mainly oral intake of enzymes in addition to conventional therapies. Investigated outcomes were:
- side-effects of anticancer therapy,
- quality of life,
- anticancer effects,
- survival rates.
Due to conflicting results and moderate quality of the included studies, the evidence is insufficient to attribute positive effects to enzymes in terms of better tolerability of the various antineoplastic therapies or even improvement in treatment efficacy. In most cases, enzyme therapy was well tolerated; side-effects were mainly gastrointestinal complaints such as diarrhea or meteorism.
The authors concluded that there is no clear therapeutic benefit of enzymes neither as supportive therapy nor as part of antineoplastic therapy.
I fully agree with this conclusion. In fact, in my new book that is just being published, I summarised the evidence for enzyme therapy (and many more alternative cancer therapies) in very similar terms: the evidence to suggest that enzyme therapy might be an effective treatment for any type of cancer is less than convincing.
I find it highly irresponsible to claim otherwise. Cancer patients are vulnerable and can easily be tempted to opt for one of the many quack treatments that are said to be both effective and free of nasty adverse effects. If they do try such options, they usually pay dearly, and not just in monetary terms.

