back pain
This single-blind, randomized, clinical trial was aimed at determining the long-term clinical effects of spinal manipulative therapy (SMT) or mobilization (MOB) as an adjunct to neurodynamic mobilization (NM) in the management of individuals with Lumbar Disc Herniation with Radiculopathy (DHR).
Forty participants diagnosed as having a chronic DHR (≥3 months) were randomly allocated into two groups with 20 participants each in the SMT and MOB groups.
Participants in the SMT group received high-velocity, low-amplitude manipulation, while those in the MOB group received Mulligans’ spinal mobilization with leg movement. Each treatment group also received NM as a co-intervention, administered immediately after the SMT and MOB treatment sessions. Each group received treatment twice a week for 12 weeks.
The following outcomes were measured at baseline, 6, 12, 26, and 52 weeks post-randomization; back pain, leg pain, activity limitation, sciatica bothersomeness, sciatica frequency, functional mobility, quality of life, and global effect. The primary outcomes were pain and activity limitation at 12 weeks post-randomization.
The results indicate that the MOB group improved significantly better than the SMT group in all outcomes (p < 0.05), and at all timelines (6, 12, 26, and 52 weeks post-randomization), except for sensory deficit at 52 weeks, and reflex and motor deficits at 12 and 52 weeks. These improvements were also clinically meaningful for neurodynamic testing and sensory deficits at 12 weeks, back pain intensity at 6 weeks, and for activity limitation, functional mobility, and quality of life outcomes at 6, 12, 26, and 52 weeks of follow-ups. The risk of being improved at 12 weeks post-randomization was 40% lower (RR = 0.6, CI = 0.4 to 0.9, p = 0.007) in the SMT group compared to the MOB group.
The authors concluded that this study found that individuals with DHR demonstrated better improvements when treated with MOB plus NM than when treated with SMT plus NM. These improvements were also clinically meaningful for activity limitation, functional mobility, and quality of life outcomes at long-term follow-up.
Yet again, I find it hard to resist playing the devil’s advocate: had the researchers added a third group with sham-MOB, they would have perhaps found that this group would have recovered even faster. In other words, this study might show that SMT is no good for DHR (which I find unsurprising), but it does NOT demonstrate MOB to be an effective therapy.
Low back pain (LBP) affects almost all of us at some stage. It is so common that it has become one of the most important indications for most forms of so-called alternative medicine (SCAM). In the discussions about the value (or otherwise) of SCAMs for LBP, we sometimes forget that there are many conventional medical options to treat LBP. It is therefore highly relevant to ask how effective they are. This overview aimed to summarise the evidence from Cochrane Reviews of the efficacy, effectiveness, and safety of systemic pharmacological interventions for adults with non‐specific LBP.
The Cochrane Database of Systematic Reviews was searched from inception to 3 June 2021, to identify reviews of randomised controlled trials (RCTs) that investigated systemic pharmacological interventions for adults with non‐specific LBP. Two authors independently assessed eligibility, extracted data, and assessed the quality of the reviews and certainty of the evidence using the AMSTAR 2 and GRADE tools. The review focused on placebo comparisons and the main outcomes were pain intensity, function, and safety.
Seven Cochrane Reviews that included 103 studies (22,238 participants) were included. There was high confidence in the findings of five reviews, moderate confidence in one, and low confidence in the findings of another. The reviews reported data on six medicines or medicine classes: paracetamol, non‐steroidal anti‐inflammatory drugs (NSAIDs), muscle relaxants, benzodiazepines, opioids, and antidepressants. Three reviews included participants with acute or sub‐acute LBP and five reviews included participants with chronic LBP.
Acute LBP
Paracetamol
There was high‐certainty evidence for no evidence of difference between paracetamol and placebo for reducing pain intensity (MD 0.49 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐1.99 to 2.97), reducing disability (MD 0.05 on a 0 to 24 scale (higher scores indicate worse disability), 95% CI ‐0.50 to 0.60), and increasing the risk of adverse events (RR 1.07, 95% CI 0.86 to 1.33).
NSAIDs
There was moderate‐certainty evidence for a small between‐group difference favouring NSAIDs compared to placebo at reducing pain intensity (MD ‐7.29 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐10.98 to ‐3.61), high‐certainty evidence for a small between‐group difference for reducing disability (MD ‐2.02 on a 0‐24 scale (higher scores indicate worse disability), 95% CI ‐2.89 to ‐1.15), and very low‐certainty evidence for no evidence of an increased risk of adverse events (RR 0.86, 95% CI 0. 63 to 1.18).
Muscle relaxants and benzodiazepines
There was moderate‐certainty evidence for a small between‐group difference favouring muscle relaxants compared to placebo for a higher chance of pain relief (RR 0.58, 95% CI 0.45 to 0.76), and higher chance of improving physical function (RR 0.55, 95% CI 0.40 to 0.77), and increased risk of adverse events (RR 1.50, 95% CI 1. 14 to 1.98).
Opioids
None of the included Cochrane Reviews aimed to identify evidence for acute LBP.
Antidepressants
No evidence was identified by the included reviews for acute LBP.
Chronic LBP
Paracetamol
No evidence was identified by the included reviews for chronic LBP.
NSAIDs
There was low‐certainty evidence for a small between‐group difference favouring NSAIDs compared to placebo for reducing pain intensity (MD ‐6.97 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐10.74 to ‐3.19), reducing disability (MD ‐0.85 on a 0‐24 scale (higher scores indicate worse disability), 95% CI ‐1.30 to ‐0.40), and no evidence of an increased risk of adverse events (RR 1.04, 95% CI ‐0.92 to 1.17), all at intermediate‐term follow‐up (> 3 months and ≤ 12 months postintervention).
Muscle relaxants and benzodiazepines
There was low‐certainty evidence for a small between‐group difference favouring benzodiazepines compared to placebo for a higher chance of pain relief (RR 0.71, 95% CI 0.54 to 0.93), and low‐certainty evidence for no evidence of difference between muscle relaxants and placebo in the risk of adverse events (RR 1.02, 95% CI 0.67 to 1.57).
Opioids
There was high‐certainty evidence for a small between‐group difference favouring tapentadol compared to placebo at reducing pain intensity (MD ‐8.00 on a 0 to 100 scale (higher scores indicate worse pain), 95% CI ‐1.22 to ‐0.38), moderate‐certainty evidence for a small between‐group difference favouring strong opioids for reducing pain intensity (SMD ‐0.43, 95% CI ‐0.52 to ‐0.33), low‐certainty evidence for a medium between‐group difference favouring tramadol for reducing pain intensity (SMD ‐0.55, 95% CI ‐0.66 to ‐0.44) and very low‐certainty evidence for a small between‐group difference favouring buprenorphine for reducing pain intensity (SMD ‐0.41, 95% CI ‐0.57 to ‐0.26).
There was moderate‐certainty evidence for a small between‐group difference favouring strong opioids compared to placebo for reducing disability (SMD ‐0.26, 95% CI ‐0.37 to ‐0.15), moderate‐certainty evidence for a small between‐group difference favouring tramadol for reducing disability (SMD ‐0.18, 95% CI ‐0.29 to ‐0.07), and low‐certainty evidence for a small between‐group difference favouring buprenorphine for reducing disability (SMD ‐0.14, 95% CI ‐0.53 to ‐0.25).
There was low‐certainty evidence for a small between‐group difference for an increased risk of adverse events for opioids (all types) compared to placebo; nausea (RD 0.10, 95% CI 0.07 to 0.14), headaches (RD 0.03, 95% CI 0.01 to 0.05), constipation (RD 0.07, 95% CI 0.04 to 0.11), and dizziness (RD 0.08, 95% CI 0.05 to 0.11).
Antidepressants
There was low‐certainty evidence for no evidence of difference for antidepressants (all types) compared to placebo for reducing pain intensity (SMD ‐0.04, 95% CI ‐0.25 to 0.17) and reducing disability (SMD ‐0.06, 95% CI ‐0.40 to 0.29).
The authors concluded as follows: we found no high‐ or moderate‐certainty evidence that any investigated pharmacological intervention provided a large or medium effect on pain intensity for acute or chronic LBP compared to placebo. For acute LBP, we found moderate‐certainty evidence that NSAIDs and muscle relaxants may provide a small effect on pain, and high‐certainty evidence for no evidence of difference between paracetamol and placebo. For safety, we found very low‐ and high‐certainty evidence for no evidence of difference with NSAIDs and paracetamol compared to placebo for the risk of adverse events, and moderate‐certainty evidence that muscle relaxants may increase the risk of adverse events. For chronic LBP, we found low‐certainty evidence that NSAIDs and very low‐ to high‐certainty evidence that opioids may provide a small effect on pain. For safety, we found low‐certainty evidence for no evidence of difference between NSAIDs and placebo for the risk of adverse events, and low‐certainty evidence that opioids may increase the risk of adverse events.
This is an important overview, in my opinion. It confirms what I and others have been stating for decades: WE CURRENTLY HAVE NO IDEAL SOLUTION TO LBP.
This is regrettable but true. It begs the question of what one should recommend to LBP sufferers. Here too, I have to repeat myself: (apart from staying as active as possible) the optimal therapy is the one that has the most favourable risk/benefit profile (and does not cost a fortune). And this option is not drugs, chiropractic, osteopathy, acupuncture, or any other SCAM – it is (physio)therapeutic exercise which is cheap, safe, and (mildly) effective.
If you think that scanning through dozens of new scientific articles every week is a dry and often somewhat tedious exercise, you are probably correct. But every now and then, this task is turned into prime entertainment by some pseudoscientists trying to pretend to be scientists. Take, for instance, the latest homeopathy study by Indian researchers with no less than 9 seemingly impressive affiliations:
- 1Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 2Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE, Sector III, Salt Lake, Kolkata, West Bengal, India.
- 3Department of Homoeopathy, State Homoeopathic Dispensary, Karaila, Pratapgarh, Uttar Pradesh, India.
- 4Department of Homoeopathy, State Homoeopathic Dispensary, Tulsipur, Shrawasti, Uttar Pradesh, India.
- 5Department of Materia Medica, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 6State Homoeopathic Dispensary, Mangalbari Rural Hospital, Matiali Block, Jalpaiguri, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 7Department of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 8Department of Homoeopathy, East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre, Village and Post Office: Gouripur (South), Police Station Bishnupur, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 9Department of Repertory, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
Now that I have whetted your appetite, here is their study:
Lumbar spondylosis (LS) is a degenerative disorder of the lumbar spine. Despite substantial research efforts, no gold-standard treatment for LS has been identified. The efficacy of individualized homeopathic medicines (IHMs) in lumbar spondylosis (LS) is unknown. In this double-blind, randomized, placebo-controlled trial, the efficacy of IHMs was compared with identical-looking placebos in the treatment of low back pain associated with LS. It was conducted at the National Institute of Homoeopathy, West Bengal, India.
Patients were randomized to receive IHMs or placebos; standardized concomitant care was administered in both groups. The Oswestry low back pain and disability questionnaire (ODQ) was used as the primary outcome measure; the Roland-Morris questionnaire (RMQ) and the short form of the McGill pain questionnaire (SF-MPQ) served as secondary outcome measures. They were measured at baseline and every month for 3 months. Intention-to-treat analyses (ITT) were used to detect any inter-group differences using two-way repeated measures analysis of variance models overall and by unpaired t-tests at different time points.
Enrolment was stopped prematurely because of time restrictions; 55 patients had been randomized (verum: 28; control: 27); 49 could be analyzed by ITT (verum: 26; control: 23).
The results are as follows:
- Inter-group differences in ODQ (F 1, 47 = 0.001, p = 0.977), RMQ (F 1, 47 = 0.190, p = 0.665) and SF-MPQ total score (F 1, 47 = 3.183, p = 0.081) at 3 months were not statistically significant.
- SF-MPQ total score after 2 months (p = 0.030) revealed an inter-group statistical significance, favoring IHMs against placebos.
- Some of the SF-MPQ sub-scales at different time points were also statistically significant: e.g., the SF-MPQ average pain score after 2 months (p = 0.002) and 3 months (p = 0.007).
- Rhus Toxicodendron, Sulphur, and Pulsatilla nigricans were the most frequently indicated medicines.
The authors concluded that owing to failure in detecting a statistically significant effect for the primary outcome and in recruiting a sufficient number of participants, our trial remained inconclusive.
Now that I (and hopefully you too) have recovered from laughing out loud, let me point out why this paper had me in stitches:
- The trial was aborted not because of a “time limit” but because of slow recruitment, I presume. The question is why were not more patients volunteering? Low back pain with LS is extremely common. Could it be that patients know only too well that homeopathy does not help with low back pain?
- If a trial gets aborted because of very low patient numbers, it is probably best not to publish it or at least not to evaluate its results at all.
- If the researchers insist on publishing it, their paper should focus on the reason why it did not succeed so that others can learn from their experience by avoiding their mistakes.
- However, once the researchers do run statistical tests, they should be honest and conclude clearly that, because the primary outcome measure showed no inter-group difference, the study failed to demonstrate that the treatment is effective.
- The trial did not “remain inconclusive”; it was squarely negative.
- The editor of the journal HOMEOPATHY should know better than to publish such nonsense.
A final thought: is it perhaps the ultimate proof of homeopathy’s ‘like cures like’ assumption to use sound science (i.e. an RCT), submit it to the homeopathic process of endless dilutions and succussions, and – BINGO – generate utter nonsense?
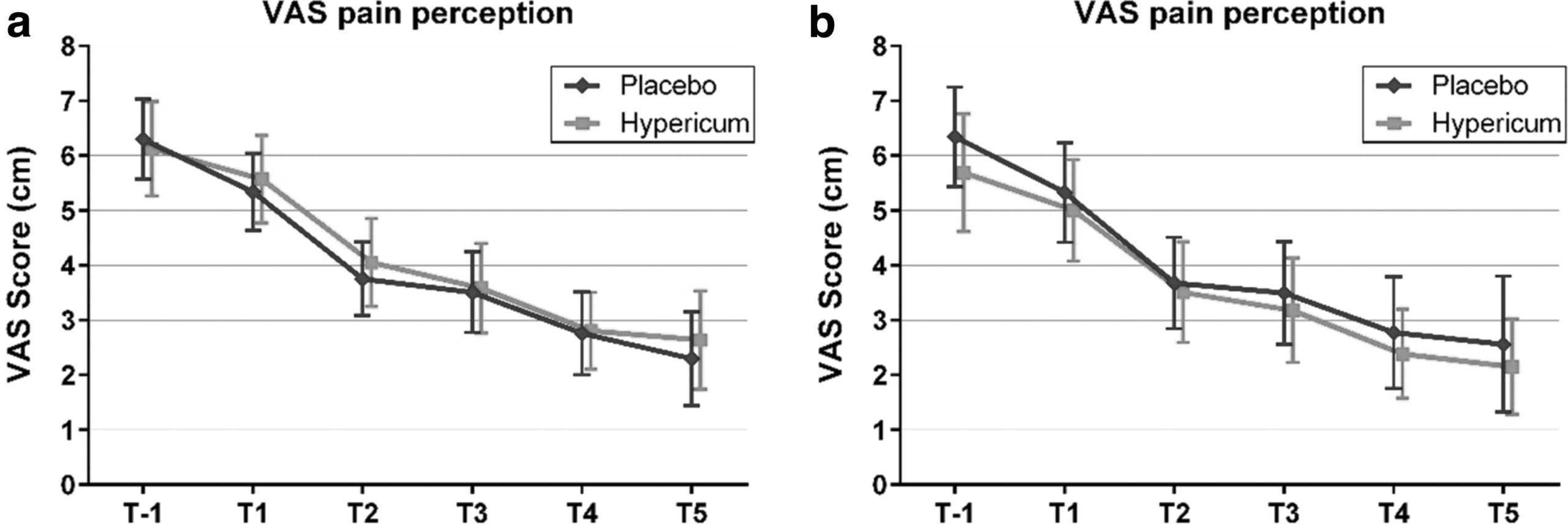
Hypericum perforatum (St John’s wort) is often recommended as a remedy to relieve pain caused by nerve damage. This trial investigated whether homeopathic Hypericum leads to a reduction in postoperative pain and a decrease in pain medication compared with placebo.
The study was designed as a randomized double-blind, monocentric, placebo-controlled clinical trial with inpatients undergoing surgery for lumbar sequestrectomy. Homeopathic treatment was compared to placebo, both in addition to usual pain management. The primary endpoint was pain relief measured with a visual analog scale. Secondary endpoints were the reduction of inpatient postoperative analgesic medication and change in sensory and affective pain perception.
The results show that the change in pain perception between baseline and day 3 did not significantly differ between the study arms. With respect to pain medication, total morphine equivalent doses did not differ significantly. However, a statistical trend and a moderate effect (d = 0.432) in the decrease of pain medication consumption in favor of the Hypericum group was observed.
The authors concluded that this is the first trial of homeopathy that evaluated the efficacy of Hypericum C200 after lumbar monosegmental spinal sequestrectomy. Although no significant differences between the groups could be shown, we found that patients who took potentiated Hypericum in addition to usual pain management showed lower consumption of analgesics. Further investigations, especially with regard to pain medication, should follow to better classify the described analgesic reduction.
For a number of reasons, this is a remarkably mysterious and quite hilarious study:
- Hypericum is recommended as an analgesic for neuropathic pain.
- According to the ‘like cures like’ axiom of homeopathy, it therefore must increase pain in such situations.
- Yet, the authors of this trial mounted an RCT to see whether it reduces pain.
- Thus they either do not understand homeopathy or wanted to sabotage it.
- As they are well-known pro-homeopathy researchers affiliated with a university that promotes homeopathy (Witten/Herdecke University, Herdecke, Germany), both explanations are highly implausible.
- The facts that the paper was published in a pro-SCAM journal (J Integr Complement Med), and the study was sponsored by the largest German firm of homeopathics (Deutsche Homoeopathische Union) renders all this even more puzzling.
- However, these biases do explain that the authors do their very best to mislead us by including some unwarranted ‘positive’ findings in their overall conclusions.
In the end, none of this matters, because the results of the study reveal that firstly the homeopathic ‘law of similars’ is nonsense, and secondly one homeopathic placebo (i.e. Hypericum C200) produces exactly the same outcomes as another, non-homeopathic placebo.
Osteopathy is currently regulated in 12 European countries: Cyprus, Denmark, Finland, France, Iceland, Italy, Liechtenstein, Luxembourg, Malta, Portugal, Switzerland, and the UK. Other countries such as Belgium and Norway have not fully regulated it. In Austria, osteopathy is not recognized or regulated. The Osteopathic Practitioners Estimates and RAtes (OPERA) project was developed as a Europe-based survey, whereby an updated profile of osteopaths not only provides new data for Austria but also allows comparisons with other European countries.
A voluntary, online-based, closed-ended survey was distributed across Austria in the period between April and August 2020. The original English OPERA questionnaire, composed of 52 questions in seven sections, was translated into German and adapted to the Austrian situation. Recruitment was performed through social media and an e-based campaign.
The survey was completed by 338 individuals (response rate ~26%), of which 239 (71%) were female. The median age of the responders was 40–49 years. Almost all had preliminary healthcare training, mainly in physiotherapy (72%). The majority of respondents were self-employed (88%) and working as sole practitioners (54%). The median number of consultations per week was 21–25 and the majority of respondents scheduled 46–60 minutes for each consultation (69%).
The most commonly used diagnostic techniques were: palpation of position/structure, palpation of tenderness, and visual inspection. The most commonly used treatment techniques were cranial, visceral, and articulatory/mobilization techniques. The majority of patients estimated by respondents consulted an osteopath for musculoskeletal complaints mainly localized in the lumbar and cervical region. Although the majority of respondents experienced a strong osteopathic identity, only a small proportion (17%) advertise themselves exclusively as osteopaths.
The authors concluded that this study represents the first published document to determine the characteristics of the osteopathic practitioners in Austria using large, national data. It provides new information on where, how, and by whom osteopathic care is delivered. The information provided may contribute to the evidence used by stakeholders and policy makers for the future regulation of the profession in Austria.
This paper reveals several findings that are, I think, noteworthy:
- Visceral osteopathy was used often or very often by 84% of the osteopaths.
- Muscle energy techniques were used often or very often by 53% of the osteopaths.
- Techniques applied to the breasts were used by 59% of the osteopaths.
- Vaginal techniques were used by 49% of the osteopaths.
- Rectal techniques were used by 39% of the osteopaths.
- “Taping/kinesiology tape” was used by 40% of osteopaths.
- Applied kinesiology was used by 17% of osteopaths and was by far the most-used diagnostic approach.
Perhaps the most worrying finding of the entire paper is summarized in this sentence: “Informed consent for oral techniques was requested only by 10.4% of respondents, and for genital and rectal techniques by 21.0% and 18.3% respectively.”
I am lost for words!
I fail to understand what meaningful medical purpose the fingers of an osteopath are supposed to have in a patient’s vagina or rectum. Surely, putting them there is a gross violation of medical ethics.
Considering these points, I find it impossible not to conclude that far too many Austrian osteopaths practice treatments that are implausible, unproven, potentially harmful, unethical, and illegal. If patients had the courage to take action, many of these charlatans would probably spend some time in jail.
This double-blind, randomized study assessed the effectiveness of physiotherapy instrument mobilization (PIM) in patients with low back pain (LBP) and compared it with the effectiveness of manual mobilization.
Thirty-two participants with LBP were randomly assigned to one of two groups:
- The PIM group received lumbar mobilization using an activator instrument, stabilization exercises, and education.
- The manual group received lumbar mobilization using a pisiform grip, stabilization exercises, and education.
Both groups had 4 treatment sessions over 2-3 weeks. The following outcomes were measured before the intervention, and after the first and fourth sessions:
- Numeric Pain Rating Scale (NPRS),
- Oswestry Disability Index (ODI) scale,
- Pressure pain threshold (PPT),
- lumbar spine range of motion (ROM),
- lumbar multifidus muscle activation.
There were no differences between the PIM and manual groups in any outcome measures. However, over the period of study, there were improvements in both groups in NPRS (PIM: 3.23, Manual: 3.64 points), ODI (PIM: 17.34%, Manual: 14.23%), PPT (PIM: ⩽ 1.25, Manual: ⩽ 0.85 kg.cm2), lumbar spine ROM (PIM: ⩽ 9.49∘, Manual: ⩽ 0.88∘), and/or lumbar multifidus muscle activation (percentage thickness change: PIM: ⩽ 4.71, Manual: ⩽ 4.74 cm; activation ratio: PIM: ⩽ 1.17, Manual: ⩽ 1.15 cm).
The authors concluded that both methods of lumbar spine mobilization demonstrated comparable improvements in pain and disability in patients with LBP, with neither method exhibiting superiority over the other.
If this conclusion is meant to tell us that both treatments were equally effective, I beg to differ. The improvements documented here are consistent with improvements caused by the natural history of the condition, regression towards the mean, and placebo effects. The data do not prove that they are due to the treatments. On the contrary, they seem to imply that patients get better no matter what therapy is used. Thus, I feel that the results are entirely in keeping with the hypothesis that spinal mobilization is a placebo treatment.
So, allow me to re-phrase the authors’ conclusion as follows:
Lumbar mobilizations do not seem to have specific therapeutic effects and might therefore be considered to be ineffective for LBP.
This systematic review, meta-analysis, and meta-regression investigated the effects of individualized interventions, based on exercise alone or combined with psychological treatment, on pain intensity and disability in patients with chronic non-specific low-back pain.
Databases were searched up to January 31, 2022, to retrieve respective randomized clinical trials of individualized and/or personalized and/or stratified exercise interventions with or without psychological treatment compared to any control.
The findings show:
- Fifty-eight studies (n = 10084) were included. At short-term follow-up (12 weeks), low-certainty evidence for pain intensity (SMD -0.28 [95%CI -0.42 to -0.14]) and very low-certainty evidence for disability (-0.17 [-0.31 to -0.02]) indicates superior effects of individualized versus active exercises, and very low-certainty evidence for pain intensity (-0.40; [-0.58 to -0.22])), but not (low-certainty evidence) for disability (-0.18; [-0.22 to 0.01]) compared to passive controls.
- At long-term follow-up (1 year), moderate-certainty evidence for pain intensity (-0.14 [-0.22 to -0.07]) and disability (-0.20 [-0.30 to -0.10]) indicates effects versus passive controls.
Sensitivity analyses indicate that the effects on pain, but not on disability (always short-term and versus active treatments) were robust. Pain reduction caused by individualized exercise treatments in combination with psychological interventions (in particular behavioral-cognitive therapies) (-0.28 [-0.42 to -0.14], low certainty) is of clinical importance.
The certainty of the evidence was downgraded mainly due to evidence of risk of bias, publication bias, and inconsistency that could not be explained. Individualized exercise can treat pain and disability in chronic non-specific low-back pain. The effects in the short term are of clinical importance (relative differences versus active 38% and versus passive interventions 77%), especially in regard to the little extra effort to individualize exercise. Sub-group analysis suggests a combination of individualized exercise (especially motor-control-based treatments) with behavioral therapy interventions to boost effects.
The authors concluded that the relative benefit of individualized exercise therapy on chronic low back pain compared to other active treatments is approximately 38% which is of clinical importance. Still, sustainability of effects (> 12 months) is doubtable. As individualization in exercise therapies is easy to implement, its use should be considered.
Johannes Fleckenstein, the 1st author from the Goethe-University Frankfurt, Institute of Sports Sciences, Department of Sports Medicine and Exercise Physiology, sees in the study “an urgent health policy appeal” to strengthen combined services in care and remuneration. “Compared to other countries, such as the USA, we are in a relatively good position in Germany. For example, we have a lower prescription of strong narcotics such as opiates. But the rate of unnecessary X-ray examinations, which incidentally can also contribute to the chronicity of pain, or inaccurate surgical indications is still very high.”
Personally, I find the findings of this paper rather unsurprising. As a clinician, many years ago, prescribing exercise therapy for low back pain was my daily bread. None of my team would have ever conceived the idea that exercise does not need to be individualized according to the needs and capabilities of each patient. Therefore, I suggest rephrasing the last sentence of the conclusion: As individualization in exercise therapies is easy to implement, its use should be standard procedure.
This study described osteopathic practise activity, scope of practice and the osteopathic patient profile in order to understand the role osteopathy plays within the United Kingdom’s (UK) health system a decade after the authors’ previous survey.
The researchers used a retrospective questionnaire survey design to ask about osteopathic practice and audit patient case notes. All UK-registered osteopaths were invited to participate in the survey. The survey was conducted using a web-based system. Each participating osteopath was asked about themselves, and their practice and asked to randomly select and extract data from up to 8 random new patient health records during 2018. All patient-related data were anonymized.
The survey response rate was 500 osteopaths (9.4% of the profession) who provided information about 395 patients and 2,215 consultations. Most osteopaths were:
- self-employed (81.1%; 344/424 responses),
- working alone either exclusively or often (63.9%; 237/371),
- able to offer 48.6% of patients an appointment within 3 days (184/379).
Patient ages ranged from 1 month to 96 years (mean 44.7 years, Std Dev. 21.5), of these 58.4% (227/389) were female. Infants <1 years old represented 4.8% (18/379) of patients. The majority of patients presented with musculoskeletal complaints (81.0%; 306/378) followed by pediatric conditions (5%). Persistent complaints (present for more than 12 weeks before the appointment) were the most common (67.9%; 256/377) and 41.7% (156/374) of patients had co-existing medical conditions.
The most common treatment approaches used at the first appointment were:
- soft-tissue techniques (73.9%; 292/395),
- articulatory techniques (69.4%; 274/395),
- high-velocity low-amplitude thrust (34.4%; 136/395),
- cranial techniques (23%).
The mean number of treatments per patient was 7 (mode 4). Osteopaths’ referral to other healthcare practitioners amounted to:
- GPs 29%
- Other complementary therapists 21%
- Other osteopaths 18%
The authors concluded that osteopaths predominantly provide care of musculoskeletal conditions, typically in private practice. To better understand the role of osteopathy in UK health service delivery, the profession needs to do more research with patients in order to understand their needs and their expected outcomes of care, and for this to inform osteopathic practice and education.
What can we conclude from a survey that has a 9% response rate?
Nothing!
If I ignore this fact, do I find anything of interest here?
Not a lot!
Perhaps just three points:
- Osteopaths use high-velocity low-amplitude thrusts, the type of manipulation that has most frequently been associated with serious complications, too frequently.
- They also employ cranial osteopathy, which is probably the least plausible technique in their repertoire, too often.
- They refer patients too frequently to other SCAM practitioners and too rarely to GPs.
To come back to the question asked in the title of this post: What do UK osteopaths do? My answer is
ALMOST NOTHING THAT MIGHT BE USEFUL.
England’s record goalscorer Ellen White has revealed she suffered a punctured lung while receiving acupuncture treatment. The injury accelerated her decision to retire. White, 33, said she was still coming to terms with the “traumatic” injury.
Manchester City had sourced a “specialist” – evidently not such an excellent acupuncturist because the complication is avoidable with proper knowledge of anatomy – outside the club to provide her with acupuncture to treat her back problem because of a high number of injuries in the squad at the time. “If you’d said to me two or three years ago that you’re going to retire, I would have said ‘absolutely not’, but I’ve got to a time in my career,” she said. “I had a challenging time last year – coming back from the Olympics, I basically punctured my lung, and it was a lot for me to have to go through and a big reason that accelerated my want to retire.”
The injury happened when she returned to her club with a back spasm last summer. “It punctured my lung which isn’t something that happens normally, obviously,” she said. “It was a really traumatic time for me and something that I’m still figuring out now, still working through. I had to wait for the lung to basically inflate again. I had a needle put into my chest to drag all the air out then hopefully the lung would inflate again – which it has. At the time, I think for me, I just got into a zone of: ‘I need to get back playing. We’ve got these games – I want to be back playing for my club; I want to be back playing for England. I went very tunnel vision,” she said. “It wasn’t until a good two or three months later, it just hit me like a train, what actually happened and how traumatic it was.”
Despite her quick return to goalscoring form, which included becoming the Lionesses record goalscorer in November, the striker says she is still affected by the injury and suffers “phantom pain” where it feels like it is happening again. “It’s important for me now to tell my story, and say it was a big factor in my year and leading up to the decision of wanting to retire. Obviously, there are other factors that come into that as well. I don’t want it to happen to anybody else again is my main thing. I don’t want to walk away from the sport having not told it and not say that I want things in place for it not to happen to anyone else.”
______________________________
Pneumothorax is by far the most common of all the serious, potentially fatal complications caused by acupuncture. In thin individuals, several acupuncture points over the upper thorax are just a few centimeters away from the lung. Therefore, it is easily possible to puncture a lung by inserting an acupuncture needle. This is from my 2010 review of the subject:
About 90 deaths after acupuncture have been anecdotally documented in the medical literature. Thus, acupuncture has been associated with more deaths than most other ‘alternative’ therapies except herbal medicine … The fatalities are usually due to an acupuncture needle penetrating a vital organ. This, in turn, can cause pneumothorax, cardiac tamponade, or major haemorrhage. Most instances of this nature are reported in the Asian literature which, for most of us, is not easily accessible.
A 2013 review of ours located 1104 cases that had been reported in the Korean literature alone. However, the truth of the matter is that nobody can be sure of the exact incidence figures. Why? Because there is no monitoring system that would reliably record such incidences.
I would argue that every single case of acupuncture-induced pneumothorax tells us that the acupuncturist was not adequately trained. With proper knowledge of anatomy, such complications should not happen. Therefore, such instances are a rude reminder that so-called alternative medicine (SCAM) is far too often in the hands of “specialists” who are a danger to the public.
Trevor Zierke is a D.C. who published several videos that have gone viral after saying that “literally 99% of my profession” is a scam. “When I say almost all the usual lines chiropractors tell you are lies, I mean almost all of them,” he stated. Zierke then went on to give examples of issues chiropractors allegedly make up, including someone’s spine being “misaligned,” tension on nerves causing health problems, and someone having back pain because their hips are off-center. “Almost all of these aren’t true,” he concluded.
In a follow-up video, he claimed that the reasons most people are told they need to go to a chiropractor are “overblown or just flat out lies proven wrong by research.” He also noted that, while there are many scams, that “doesn’t mean you can’t get help from a chiropractor.”
In a third TikTok video, Zierke offered some valid reasons to see a chiropractor. He said that one can seek help from a chiropractor if one has musculoskeletal pain that has been ongoing for more than one to two days, and that’s about it. He stated that issues that a chiropractor couldn’t really fix include “GI pain, hormonal issues, nutrition,” among others.
In comments, users were largely supportive of Zierke’s message.
One said: “As a physiotherapist, I’ve been trying to tell this but I don’t want to like offend any chiropractor in doing so,” a commenter shared.
“Working in a chiropractic office, this is fair,” a further user wrote. “I have issues that I know an adjustment will help & other pain that would be better stretched/released.”
In an email, Zierke reiterated the intention of his videos: “I would just like to clarify that chiropractors, in general, are not a scam or are inherently scammers (I myself am a practicing chiropractor), but rather a lot of very popular sales tactics, phrases, and wording used to imply patients need treatment, and methods of treatment, have never been proven to be true,” he explained. “When chiropractors say & use these methods stating things that are not factually true—I believe it’s scammy behavior and practices. There are still a lot of very good, honest, and integral chiropractors out there,” he concluded. “They can provide a lot of help and relief to patients. But that’s unfortunately not the majority, and I’ve heard too many stories of people falling victim to some of these scam-like tactics from bad apple chiropractors.”
None of what DC Zierke said can surprise those who have been following my blog. On the contrary, I could add a few recent posts to his criticism of chiropractic, for example:
- Pediatric chiropractic seems to be on the rise
- Catastrophic injuries after chiropractic treatment
- Chiropractic: “a safe form of treatment”?
- Malpractice Litigation Involving Chiropractic Spinal Manipulation
- Best Practices for the Chiropractic Care of Children
- No effect from adding chiropractic manipulations to exercises for neck pain
- Hurray! The new professional standard by the General Chiropractic Council protects UK chiropractors
- Manual therapy (mainly chiropractic and osteopathy) does not have clinically relevant effects on back pain compared with sham treatment
- Chiropractic Paediatric Courses … it is high time to stop this dangerous nonsense
- Chiropractic ‘subluxation’ is by no means a notion of the past
- Another indirect risk of chiropractic
- And again: chiropractic for infant colic
- Chiropractic misinformation during the COVID-19 pandemic
- The lack of chiropractic ethics: “valid consent was not obtained in a single case”
I rest my case.