symptom-relief
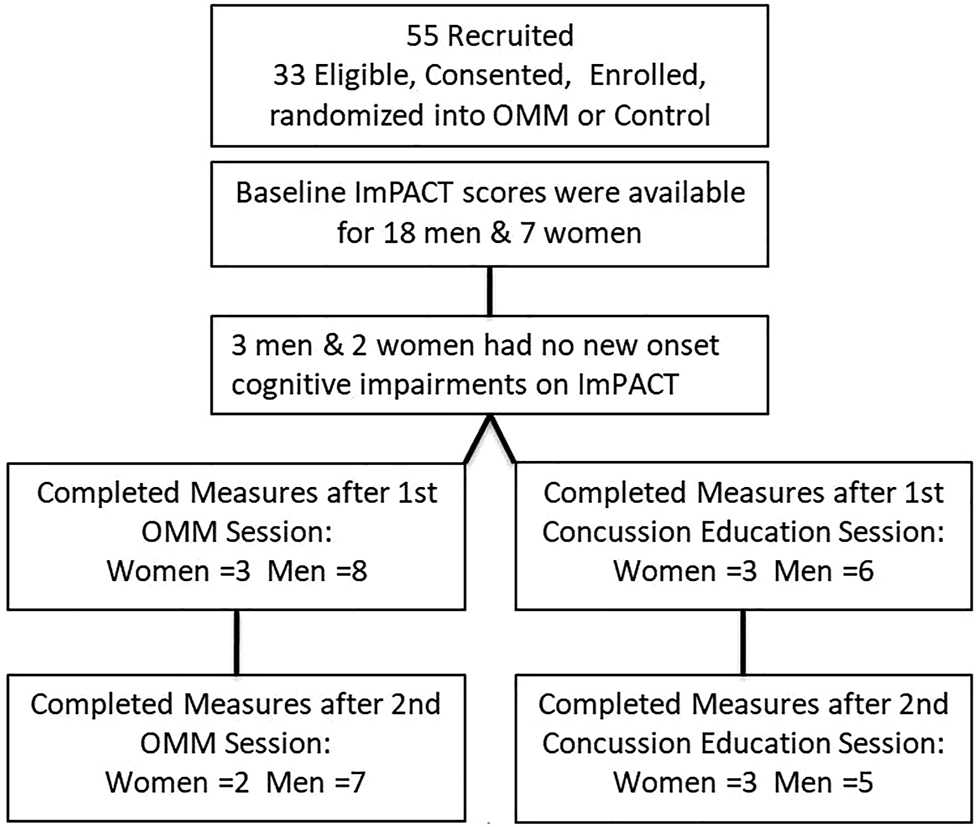
This study from the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine tested whether new-onset impairments (NOI) of neurological functions identified by Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) will improve more so after osteopathic manipulative medicine (OMM) than after concussion-education.
College athletes presenting to the outpatient academic healthcare center (AHCC) with concussion due to head injury within the preceding 2 weeks were recruited for this IRB-approved, randomized, single-blinded trial. Consented men and women were randomized into two groups:
- the verum group received two OMM treatments;
- the control group received two concussion-education sessions.
Preseason, Baseline, ImPACT was compared to Post-Injury scores to determine NOI. Baseline, Post-Injury, and Post-Interventions ImPACTs were compared by analysis of variance (ANOVA, α≤0.05). Post-Injury correlations and mean changes in King-Devick (KD) scores were analyzed.
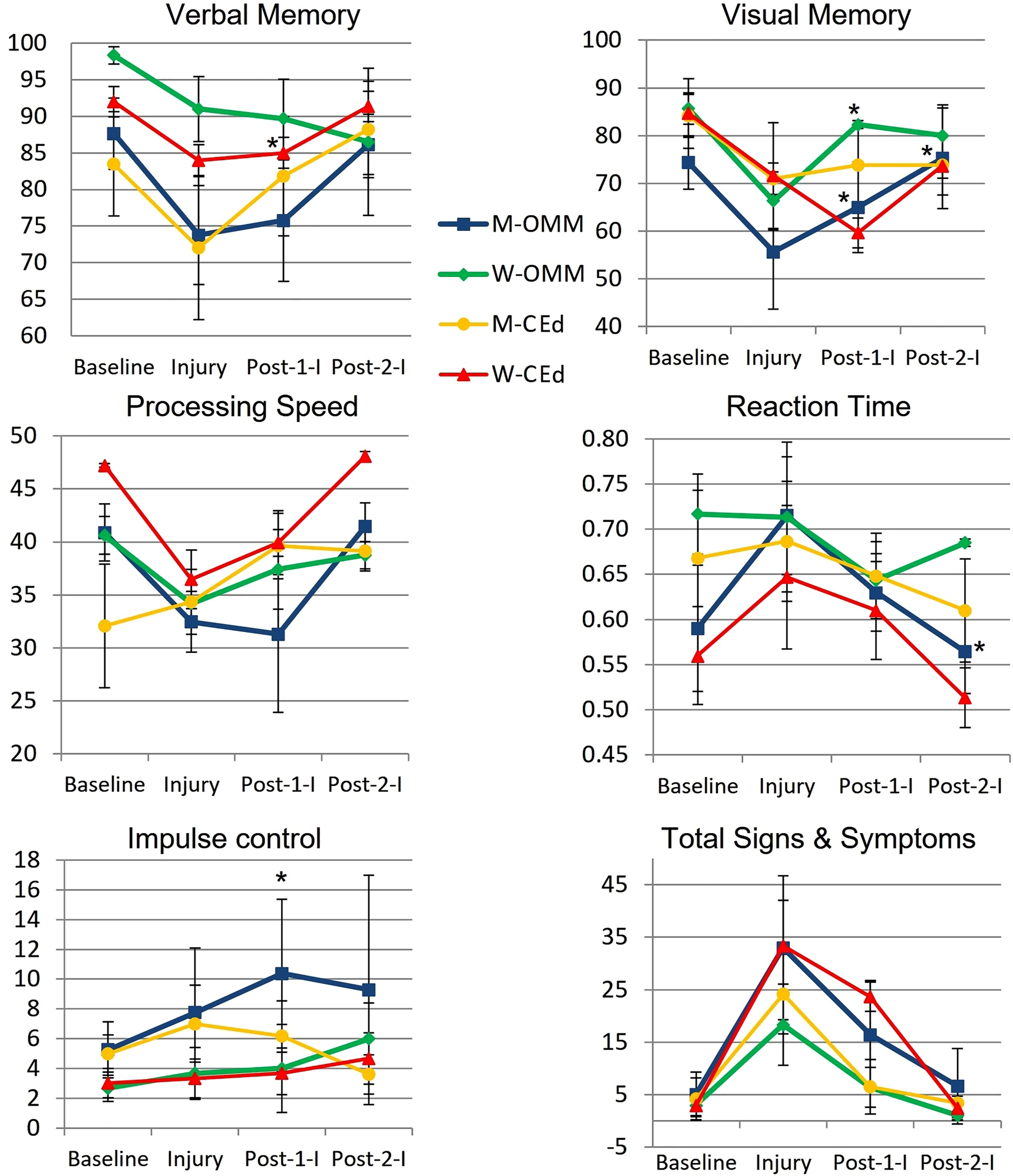
Post-Injury NOI were found in 77.8% (14/18) men and 85.7% (6/7) women, including ImPACT subscore indices for verbal and visual memory, processing speed (PS), and reaction time (RT). Of those with NOI, mean visual memory recovered by 50.0% following one and by 104.9% (p=0.032) following two OMM treatments in men and by 82.8% (p=0.046) following one treatment in women. Following two interventions, the mean RT in men receiving OMM improved by 0.10 more than education (p=0.0496). The effect sizes of OMM were large (Cohen’s d=1.33) on visual memory and small (Cohen’s d=0.31) on RT.
The authors concluded that NOI in visual memory and RT following concussion significantly improved in the OMM group compared to the education group. Integrating OMM utilizing physical exam and this treatment was a safe individualized approach in athletes with acute uncomplicated concussions. Further research is warranted to improve the utilization of OMM for individuals with concussion.
What the abstract does not tell you is that the two groups were extremely small and that they became even smaller, as some patients were lost to follow-up.
In addition, the results were all over the place.
Furthermore, it is noteworthy that neither the therapists nor the patients were blinded and the observation period was short. Finally, the authors state in their conclusions that OMM is safe. Considering the sample size and the attrition rate (perhaps all those patients lost to follow-up died?), this is of course ridiculously wishful thinking.
So, what can we conclude from this study? I don’t know about you, but I conclude that the department of Osteopathic Manipulative Medicine, New York Institute of Technology College of Osteopathic Medicine could do with a good science teacher.
Wellness seems to be everywhere these days – I mean of course the term, not the state or condition. On Medline, we find in excess of 500 000 articles on wellness, just for the year 2022! Wellness is en vogue, sexy, politically correct, etc. It looks good to talk and write about it. Most importantly it is good business. A report by the Global Wellness Institute stated that in 2020 the wellness industry was valued at $4.5 trillion and continues to grow at a frightening rate.
Having studied some of the recent literature on the subject, I get the impression that, for many, wellness is foremost an excuse for waffling utter nonsense. Let me, therefore, today ask just 5 simple questions about wellness that are likely to reduce the wellness of the ‘wellness brigade’:
1.What is wellness?
It is quite evidently a sector that is unable to define itself. Here are just a few of the definitions that have been suggested. Wellness is:
- the active pursuit of activities, choices and lifestyles that lead to a state of holistic health
- the result of personal initiative, seeking a more optimal, holistic and balanced state of health and well-being across multiple dimensions
- an active process of becoming aware of and making choices towards a healthy and fulfilling life
- the state of being in good health, especially as an actively pursued goal
- a state beyond absence of illness but rather aims to optimize well-being
- the act of practicing healthy habits on a daily basis to attain better physical and mental health outcomes
- an active process through which people become aware of, and make choices toward, a more successful existence
- the optimal state of health of individuals and groups
A 2018 review revealed that there is a lack of a uniform definition of wellness and showed that there is insufficient evidence to support the clinical utility of a single particular wellness instrument.
2. How do we measure wellness?
The short answer to this question is: nobody is quite sure. There simply is no generally accepted, well-validated measure. A few domains come to mind:
- physical functioning,
- somatic symptoms, e.g. pain,
- psychological symptoms,
- social functioning,
- needs and satisfaction.
But there is no simple means to quantify wellness. If you think that I am exaggerating, consider this recent review: 79 mental wellness instruments were identified. Most studies did not provide a definition for mental wellness. We identified thirteen mental wellness concepts from 97 studies, namely: life satisfaction, mental wellbeing [general], resilience, self-efficacy, self- esteem, connectedness, coping, self-control, mindfulness/spiritual, hope, sense of coherence, happiness, and life purpose.
3. What affects wellness?
The short answer is: potentially everything. My very own wellness, for instance, deteriorates sharply, if I have to read yet another nonsensical article about it.
4. Which interventions improve wellness?
As we have seen in my previous post, this is where so-called alternative medicine (SCAM) comes in. Since there is no measure to quantify wellness, we just have to take the word of SCAM proponents for it: SCAM improves wellness!!!
Which specific SCAM?
Can I see the evidence?
Sorry, no questions allowed!
And if you dare to insist on evidence, the ‘wellness brigade’ would just give you a pitiful smile and say: wellness has to be experienced, not measured.
5. Are there risks?
Yes, of course! Here are just some of them:
- The treatments advocated for wellness almost invariably cost money.
- The treatments advocated for wellness almost invariably cause direct and indirect harm, as discussed in many of my previous posts.
- Wellness treatments tend to give the impression that one can buy wellness like an expensive piece of clothing without putting in any real effort oneself.
Considering all this, I’d like to offer my very own definition of the sector:
Wellness is a fashionable paradise for charlatans in which they are protected from scientific scrutiny and feel at liberty to bullshit to their hearts’ content.
Drip IV is “Australia’s first and leading mobile healthcare company specialising in assisting with nutritional deficiencies”. They claim to provide a mobile IV service that is prescribed and tailored individually to your nutritional needs. Treatment plans and customised infusions are determined by a medical team to suit individual requirements. They deliver vitamins, minerals and amino acids directly to the body via the bloodstream, a method they state allows for optimal bioavailability.
These claims are a little puzzling to me, not least because vitamins, minerals and amino acids tailored individually to the nutritional needs of the vast majority of people would mean administering nothing at all. But I guess that virtually every person who consults the service will get an infusion [and pay dearly for it].
The Australian Therapeutic Goods Administration (TGA) seems to have a similarly dim view on Drip IV. The TGA has just issued 20 infringement notices totalling $159,840 to the company and to one of its executive officers. The reason: unlawful advertising of intravenous infusion products to Australian consumers on a company website and social media. Ten notices totalling $133,200 were issued to the company and ten notices totalling $26,640 were issued to an executive officer. The TGA considers the intravenous infusion products to be therapeutic goods because of the claims made about them, and the advertising to be unlawful because the advertisements allegedly:
- contained prohibited representations, such as claims regarding cancer.
- contained restricted representations such as that the products would alleviate fatigue caused by COVID-19, assist in the treatment of Graves’ Disease and Alzheimer’s Disease, and support the treatment of autoimmune diseases such as Multiple Sclerosis. No TGA approval had been given to make such claims.
- referred to ingredients that are prescription only, such as glutathione. Prescription medicines cannot be advertised directly to the public in Australia.
- contained a statement or picture suggesting or implying the products were ‘TGA Approved’. Advertising of therapeutic goods cannot include a government endorsement.
- contained a statement or picture expressing that the goods were ‘miraculous’.
Vitamin infusions have become very popular around the globe. There are now thousands of clinics offering this service, and many of them advertise aggressively with claims that are questionable. Here is just one example from the UK:
Modern life is hectic. If you are looking to boost your wellbeing, increase your energy levels, lift your mood and hydrate your body, Vitamin IV Infusions are ideal. Favoured by celebrities such as Madonna, Simon Cowell and Rihanna, Vitamin IV Infusions are an easy, effective way of delivering vitamins, minerals and amino acids directly into your bloodstream via an IV (intravenous) drip. Vitamins are essential for normal growth and staying healthy – but our bodies can’t produce all of the nutrients we need to function and thrive. That’s why more than one in three people take daily vitamin supplements – often without realising that only 15% of the active nutrients consumed orally actually find their way into their bloodstream. With Vitamin IV Infusions, the nutrients enter your bloodstream directly and immediately, and are delivered straight to your cells. We offer four different Vitamin IV Infusions, so you can choose the best combination for your personal needs, while boosting your general health, energy and wellbeing.
My advice to consumers is a little different and considerably less costly:
- to ensure you get enough vitamins, minerals, and amino acids, eat a balanced diet;
- to boost your well-being, sit down and calculate the savings you made by NOT using such a service;
- to increase your energy levels, take a nap;
- to lift your mood, recount the money you saved and think of what nice things you might buy with it;
- to hydrate your body drink a glass of water.
Perhaps it is time the authorities in all countries had a look at what these clinics are offering and what health claims they are making. Perhaps it is time they act as the TGA just did.
If you think that scanning through dozens of new scientific articles every week is a dry and often somewhat tedious exercise, you are probably correct. But every now and then, this task is turned into prime entertainment by some pseudoscientists trying to pretend to be scientists. Take, for instance, the latest homeopathy study by Indian researchers with no less than 9 seemingly impressive affiliations:
- 1Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 2Department of Organon of Medicine and Homoeopathic Philosophy, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Block GE, Sector III, Salt Lake, Kolkata, West Bengal, India.
- 3Department of Homoeopathy, State Homoeopathic Dispensary, Karaila, Pratapgarh, Uttar Pradesh, India.
- 4Department of Homoeopathy, State Homoeopathic Dispensary, Tulsipur, Shrawasti, Uttar Pradesh, India.
- 5Department of Materia Medica, National Institute of Homoeopathy, Ministry of AYUSH, Govt. of India, Salt Lake, Kolkata, West Bengal, India.
- 6State Homoeopathic Dispensary, Mangalbari Rural Hospital, Matiali Block, Jalpaiguri, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 7Department of Repertory, The Calcutta Homoeopathic Medical College and Hospital, Govt. of West Bengal, Kolkata, West Bengal, India.
- 8Department of Homoeopathy, East Bishnupur State Homoeopathic Dispensary, Chandi Daulatabad Block Primary Health Centre, Village and Post Office: Gouripur (South), Police Station Bishnupur, West Bengal, under Department of Health & Family Welfare, Govt. of West Bengal, India.
- 9Department of Repertory, D. N. De Homoeopathic Medical College and Hospital, Govt. of West Bengal, Tangra, Kolkata, West Bengal, India.
Now that I have whetted your appetite, here is their study:
Lumbar spondylosis (LS) is a degenerative disorder of the lumbar spine. Despite substantial research efforts, no gold-standard treatment for LS has been identified. The efficacy of individualized homeopathic medicines (IHMs) in lumbar spondylosis (LS) is unknown. In this double-blind, randomized, placebo-controlled trial, the efficacy of IHMs was compared with identical-looking placebos in the treatment of low back pain associated with LS. It was conducted at the National Institute of Homoeopathy, West Bengal, India.
Patients were randomized to receive IHMs or placebos; standardized concomitant care was administered in both groups. The Oswestry low back pain and disability questionnaire (ODQ) was used as the primary outcome measure; the Roland-Morris questionnaire (RMQ) and the short form of the McGill pain questionnaire (SF-MPQ) served as secondary outcome measures. They were measured at baseline and every month for 3 months. Intention-to-treat analyses (ITT) were used to detect any inter-group differences using two-way repeated measures analysis of variance models overall and by unpaired t-tests at different time points.
Enrolment was stopped prematurely because of time restrictions; 55 patients had been randomized (verum: 28; control: 27); 49 could be analyzed by ITT (verum: 26; control: 23).
The results are as follows:
- Inter-group differences in ODQ (F 1, 47 = 0.001, p = 0.977), RMQ (F 1, 47 = 0.190, p = 0.665) and SF-MPQ total score (F 1, 47 = 3.183, p = 0.081) at 3 months were not statistically significant.
- SF-MPQ total score after 2 months (p = 0.030) revealed an inter-group statistical significance, favoring IHMs against placebos.
- Some of the SF-MPQ sub-scales at different time points were also statistically significant: e.g., the SF-MPQ average pain score after 2 months (p = 0.002) and 3 months (p = 0.007).
- Rhus Toxicodendron, Sulphur, and Pulsatilla nigricans were the most frequently indicated medicines.
The authors concluded that owing to failure in detecting a statistically significant effect for the primary outcome and in recruiting a sufficient number of participants, our trial remained inconclusive.
Now that I (and hopefully you too) have recovered from laughing out loud, let me point out why this paper had me in stitches:
- The trial was aborted not because of a “time limit” but because of slow recruitment, I presume. The question is why were not more patients volunteering? Low back pain with LS is extremely common. Could it be that patients know only too well that homeopathy does not help with low back pain?
- If a trial gets aborted because of very low patient numbers, it is probably best not to publish it or at least not to evaluate its results at all.
- If the researchers insist on publishing it, their paper should focus on the reason why it did not succeed so that others can learn from their experience by avoiding their mistakes.
- However, once the researchers do run statistical tests, they should be honest and conclude clearly that, because the primary outcome measure showed no inter-group difference, the study failed to demonstrate that the treatment is effective.
- The trial did not “remain inconclusive”; it was squarely negative.
- The editor of the journal HOMEOPATHY should know better than to publish such nonsense.
A final thought: is it perhaps the ultimate proof of homeopathy’s ‘like cures like’ assumption to use sound science (i.e. an RCT), submit it to the homeopathic process of endless dilutions and succussions, and – BINGO – generate utter nonsense?
The McTimoney College of Chiropractic just announced that it has established a new four-year program in veterinary chiropractic for college students:
It means that those without a prior degree can undertake the training and education necessary to enter this coveted career. To date, animal chiropractors were required to have a prior qualification in human chiropractic or a degree in the relevant sciences.
Applications for the new program are being accepted from September 2023. Students will attend Abingdon-based University, Oxford, and a variety of practical locations, enabling the development of academic knowledge and the application of practical skills together . Modules include anatomy and physiology, veterinary science, practice and professionalism, and clinical skills, with a research dissertation running over the four-year course.
University director Christina Cunliffe said the new program was an exciting step in the development of chiropractic care for animals.
“Building on our decades of experience graduating confident, competent, and highly-skilled animal chiropractors, now is the time to open up this exciting career opportunity to college students.”
For the past 50 years, McTimoney College of Chiropractic has been training and educating human chiropractors to the highest regulatory standards. Over the past 20 years, animal chiropractic has developed to meet the requirements for this gentle, holistic treatment in the veterinary world.
Prospective students are invited to a Open House at McTimoney College of Chiropractic in Abingdon on February 16.
McTimoney Chiropractic for Animals identifies areas of stiffness, asymmetry, and poor range of motion within the skeletal system, particularly the spine and pelvis. This affects the muscles that surround these structures, as well as the nerve impulses that pass from the central nervous system to the periphery of the body. The adjustments are very light and fast, stimulating an instant response in the affected soft tissues and joints, promoting relaxation of muscle spasms, improving nerve function, and helping the skeletal structure regain better symmetry and movement again.
In many cases, animals suffer from underlying conditions such as arthritic changes or degenerative diseases that force them to compensate in their posture and movement in an attempt to remain comfortable. However, these offsets become increasingly entrenched and can be painful or uncomfortable, requiring chiropractic care to provide some relief. In other cases, the animals are working hard or competing and as such accumulate tension and asymmetries due to the demands of their work. Once again, chiropractic care helps relieve pain and promote performance, whether it’s faster speeds over hurdles for racehorses and events, better jumping style in showjumpers, or more extravagant movements for dressage stars.
Two recent graduates of the school’s Master of Animal Handling (Chiropractic) program did not hesitate to recommend the university. Natalie McQuiggan said that she had wanted to do McTimoney Chiropractic from a very young age, “but the process of doing it always seemed really daunting.
“But from the start, the staff and teachers were lovely and welcoming, and queries were answered promptly. I have really enjoyed my two years in the Master of Animal Handling (Chiropractic) program and would recommend anyone thinking of doing it to just do it.”
Pollyanna Fitzgerald said the university offered a supportive and welcoming learning environment, allowing her to grow and develop as a student and future professional. “There is always someone to talk to and offer encouragement when needed. As a student I have learned a lot and have been encouraged to believe in myself and it has been a wonderful place to learn.”
A free webinar, McTimoney’s Animal Chiropractic as a Careeron January 24 at 7:30 p.m. (GMT), is open to those who wish to learn more about the McTimoney technique and its application, and the training paths available to those interested in becoming a McTimoney Animal Chiropractor.
________________________
I think this announcement is puzzling on several levels:
- I was unable to find an ‘Abingdon-based University, Oxford’; could it be this institution that is a college and not a university?
- Christina Cunliffe seems to be (or has been?) affiliated with the McTimoney College of Chiropractic which is a bit odd, in my opinion.
- The college does not have ‘decades of experience’; it was founded only in 2001.
- Most importantly, I am unable to find a jot of good evidence that veterinary chiropractic is effective for any condition (see also here, here, and here). In case anyone is aware of any, please let me know. I’d be delighted to revise my judgment.
If I am right, the new course could be a fine example of quackademia where students are ripped off and taught to later rip off the owners of animals after the academically trained quacks have mistreated them.
In this study, the impact of a multimodal integrative oncology pre- and intraoperative intervention on pain and anxiety among patients undergoing gynecological oncology surgery was explored.
Study participants were randomized into three groups:
- Group A received preoperative touch/relaxation techniques, followed by intraoperative acupuncture, plus standard care;
- Group B received preoperative touch/relaxation only, plus standard care;
- Group C (the control group) received standard care.
Pain and anxiety were scored before and after surgery using the Measure Yourself Concerns and Wellbeing (MYCAW) and Quality of Recovery (QOR-15) questionnaires, using Part B of the QOR to assess pain, anxiety, and other quality-of-life parameters.
A total of 99 patients participated in the study: 45 in Group A, 25 in Group B, and 29 in Group C. The three groups had similar baseline demographic and surgery-related characteristics. Postoperative QOR-Part B scores were significantly higher in the treatment groups (A and B) when compared with controls (p = .005), including for severe pain (p = .011) and anxiety (p = .007). Between-group improvement for severe pain was observed in Group A compared with controls (p = .011). Within-group improvement for QOR depression subscales was observed in only the intervention groups (p <0.0001). Compared with Group B, Group A had better improvement of MYCAW-reported concerns (p = .025).
The authors concluded that a preoperative touch/relaxation intervention may significantly reduce postoperative anxiety, possibly depression, in patients undergoing gynecological oncology surgery. The addition of intraoperative acupuncture significantly reduced severe pain when compared with controls. Further research is needed to confirm these findings and better understand the impact of intraoperative acupuncture on postoperative pain.
Regular readers of my blog know only too well what I am going to say about this study.
Imagine you have a basket full of apples and your friend has the same plus a basket full of pears. Who do you think has more fruit?
Dumb question, you say?
Correct!
Just as dumb, it seems, as this study: therapy A and therapy B will always generate better outcomes than therapy B alone. But that does not mean that therapy A per se is effective. Because therapy A generates a placebo effect, it might just be that it has no effect beyond placebo. And that acupuncture can generate placebo effects has been known for a very long time; to verify this we need no RCT.
As I have so often pointed out, the A+B versus B study design never generates a negative finding.
This is, I fear, precisely the reason why this design is so popular in so-called alternative medicine (SCAM)! It enables promoters of SCAM (who are not as dumb as the studies they conduct) to pretend they are scientists testing their therapies in rigorous RCTs.
The most disappointing thing about all this is perhaps that more and more top journals play along with this scheme to mislead the public!
I have tried!
Honestly!
But at present, it is simply not possible to escape the revelations and accusations by Harry Windsor.
So, eventually, I gave in and had a look at the therapy he often refers to. He claims that he is deeply traumatized by what he had to go through and, to help him survive the ordeal, Harry has been reported to use EMDR.
Eye Movement Desensitization and Reprocessing (EMDR) is a fringe psychotherapy that was developed to alleviate the distress associated with traumatic memories. It is supposed to facilitate the accessing and processing of traumatic memories and other adverse life experiences with a view of bringing these to an adaptive resolution. The claim is that, after successful treatment with EMDR therapy, affective distress is relieved, negative beliefs are reformulated, and physiological arousal is reduced.
During EMDR therapy the patient must attend to emotionally disturbing material in brief sequential doses while simultaneously focusing on an external stimulus. Therapist-directed lateral eye movements are commonly used as external stimulus but a variety of other stimuli including hand-tapping and audio stimulation can also be employed.
Francine Shapiro, the psychologist who invented EMDR claims to have serendipitously discovered this technique by experiencing spontaneous saccadic eye movements in response to disturbing thoughts during a walk in the woods. Yet, as GM Rosen explains, this explanation is difficult to accept because normal saccadic eye movements appear to be physiologically undetectable and are typically triggered by external stimuli.
Shapiro hypothesizes that EMDR therapy facilitates the access to the traumatic memory network, so that information processing is enhanced, with new associations forged between the traumatic memory and more adaptive memories or information. These new associations are alleged to result in complete information processing, new learning, elimination of emotional distress, and development of cognitive insights.
EMDR therapy uses a three-pronged protocol:
- (1) the past events that have laid the groundwork for dysfunction are processed, forging new associative links with adaptive information;
- (2) the current circumstances that elicit distress are targeted, and internal and external triggers are desensitized;
- (3) imaginal templates of future events are incorporated, to assist the client in acquiring the skills needed for adaptive functioning.
The question I ask myself is, of course: Does EMDR work?
The evidence is mixed and generally flimsy. A systematic review showed that “limitations to the current evidence exist, and much current evidence relies on small sample sizes and provides limited follow-up data”.
What might be particularly interesting in relation to Harry Windsor is that EMDR techniques have been associated with memory-undermining effects and may undermine the accuracy of memory, which can be risky if patients, later on, serve as witnesses in legal proceedings.
Personally, I think that Harry’s outbursts lend support to the hypothesis that EMDR is not effective. In the interest of the royal family, we should perhaps see whether so-called alternative medicine (SCAM) does offer an effective treatment against navel gazing?
Every now and then, I like to look at what our good friend and SCAM entrepreneur Gwyneth Paltrow is offering via her extraordinary ripoff called GOOP. When I recently browsed through her goodies, I find lots of items that made me blush (common decency does not permit me to go into details here). But I also found something that I am sure many of us might need after the over-indulgence of recent weeks:Preview Changes (opens in a new tab)
“The Martini” Emotional Detox Bath Soak
The product is described as follows:
This body-and-spirit-centering bath soak, infused with Himalayan pink salt, helps take the edge off during turbulent times (or after a crazy day). Called “The Martini” after the traditional name for the last take of the day in filmmaking, the soak is made with pharmaceutical-grade Epsom salts, chia-seed oil, passionflower, valerian root, myrrh, Australian sandalwood, and wild-crafted frankincense.
Here at goop we believe in making every choice count, which is why we’ve always been outspoken about the toxic ingredients used in personal-care and beauty products (all are effectively unregulated in this country). We’re also passionate about the idea that beauty comes from the inside out. So we use clinically proven and best-in-class ingredients at active levels to create skin care, skin-boosting ingestibles, and body essentials that are luxurious, deliver high-performance results, and enliven the senses with exquisite textures and beautiful scents. We don’t rest until we think our products are perfect—safe enough and powerful enough for noticeable results. (All our products are formulated without parabens, petroleum, phthalates, SLS, SLES, PEGs, TEA, DEA, silicones, or artificial dyes or fragrances. And our formulas are not tested on animals.) We hope you love them as much as we do.
Yes, there is a whole world out there of which a retired chap like myself knows as good as nothing. And it has its very own terminology: 
- emotional detox
- body-and-spirit-centering
- pharmaceutical-grade Epsom salts
- wild-crafted
- clinically proven and best-in-class ingredients
- skin-boosting ingestibles
- body essentials
- high-performance results
By now, I am sure, you are dying to learn what the Emotional Detox Bath Soak contains:
Sodium Chloride, Magnesium Sulfate, Passiflora Incarnata Extract, Valeriana Officinalis Root Extract, Salvia Hispanica Seed Oil, Helianthus Annuus (Sunflower) Seed Oil, Rosmarinus Officinalis (Rosemary), Leaf Extract, Maltodextrin, Boswellia Carterii Oil, Commiphora Myrrha Oil, Fusanus Spicatus Wood Oil, Cyperus Scariosus (Nagarmotha) Oil, Vetiveria Zizanoides Root Oil, Simmondsia Chinensis (Jojoba) Seed Oil, Tocopherol.
Clinically proven, you ask?
Well, perhaps not in the sense that sad, retired academics tend to understand the term, but you have to realize, this is a different world where words have different meanings, the meaning entretreneurs want them to have. What is proven though is this: at $40 a tiny jar, the detox bath will eliminate some cash from your pocket – after all, that’s what detox is all about, isn’t it?
This pilot study tested the feasibility of using US Food and Drug Administration (FDA)–recommended endpoints to evaluate the efficacy of acupuncture in the treatment of IBS. It was designed as a multicenter randomized clinical trial, conducted in 4 tertiary hospitals in China from July 1, 2020, to March 31, 2021, and 14-week data collection was completed in March 2021. Individuals with a diagnosis of IBS with diarrhea (IBS-D) were randomized to 1 of 3 groups:
- acupuncture groups 1 (using specific acupoints [SA])
- acupuncture group 2 (using nonspecific acupoints [NSA])
- sham acupuncture group (non-acupoints [NA])
Patients in all groups received twelve 30-minute sessions over 4 consecutive weeks at 3 sessions per week, ideally every other day.
The primary outcome was the response rate at week 4, which was defined as the proportion of patients whose worst abdominal pain score (score range, 0-10, with 0 indicating no pain and 10 indicating unbearable severe pain) decreased by at least 30% and the number of type 6 or 7 stool days decreased by 50% or greater.
Ninety patients (54 male [60.0%]; mean [SD] age, 34.5 [11.3] years) were enrolled, with 30 patients in each group. There were substantial improvements in the primary outcomes for all groups
- response rates in the SA group = 46.7% [95% CI, 28.8%-65.4%]
- response rate in the NSA group = 46.7% [95% CI, 28.8%-65.4%]
- response rate in the NA group = 26.7% [95% CI, 13.0%-46.2%]
The difference between the groups was not statistically significant (P = .18). The response rates of adequate relief at week 4 were 64.3% (95% CI, 44.1%-80.7%) in the SA group, 62.1% (95% CI, 42.4%-78.7%) in the NSA group, and 55.2% (95% CI, 36.0%-73.0%) in the NA group (P = .76). Adverse events were reported in 2 patients (6.7%) in the SA group and 3 patients (10%) in NSA or NA group.
The authors concluded that acupuncture in both the SA and NSA groups showed clinically meaningful improvement in IBS-D symptoms, although there were no significant differences among the 3 groups. These findings suggest that acupuncture is feasible and safe; a larger, sufficiently powered trial is needed to accurately assess efficacy.
WHAT A LOAD OF TOSH!
Here are some of the most obvious issues I have with this new study:
- A pilot study is not about reporting effectiveness/efficacy but about testing the feasibility of a study.
- That acupuncture is feasible has been known for ~2000 years.
- The conclusion that acupuncture is safe is not warranted on the basis of the data; for that we would need a much larger investigation.
- The authors seem to have used our sham needle without acknowledging it.
- The authors are affiliated with the International Acupuncture and Moxibustion Innovation Institute, School of Acupuncture-Moxibustion and Tuina, Beijing University of Chinese Medicine, yet they state that they have no conflicts of interest.
- The results are clearly negative, yet the authors seem to attempt to draw a positive conclusion.
The main question that occurs to me is this: how low has the JAMA sunk to publish such junk?
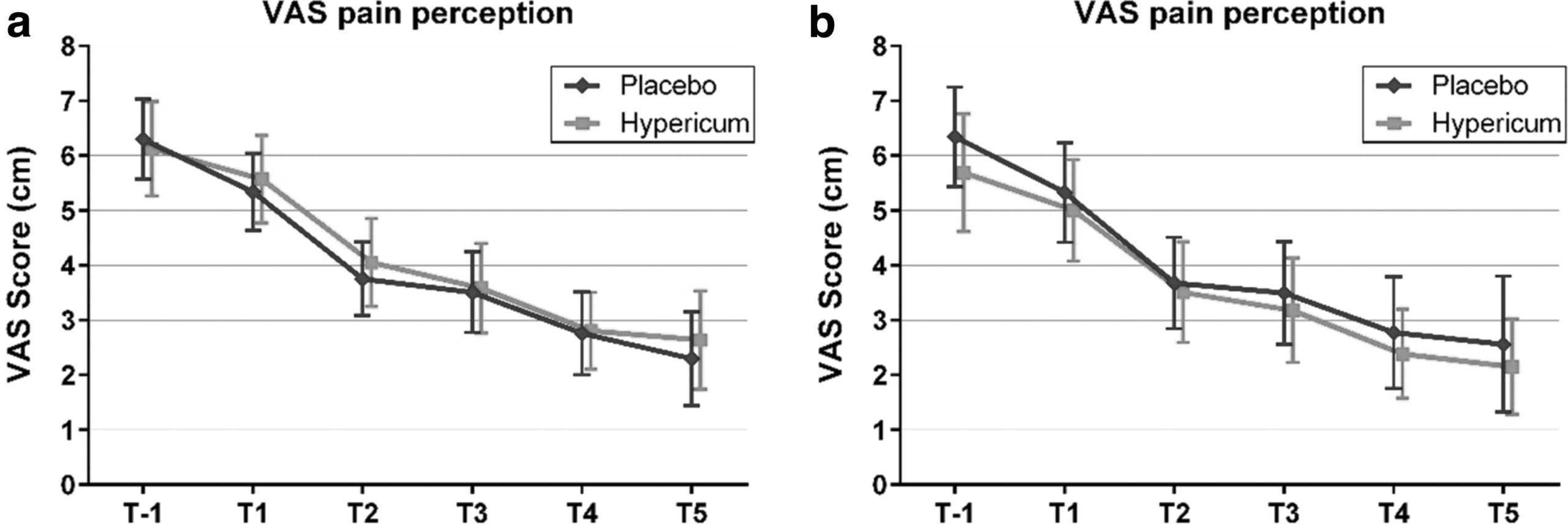
Hypericum perforatum (St John’s wort) is often recommended as a remedy to relieve pain caused by nerve damage. This trial investigated whether homeopathic Hypericum leads to a reduction in postoperative pain and a decrease in pain medication compared with placebo.
The study was designed as a randomized double-blind, monocentric, placebo-controlled clinical trial with inpatients undergoing surgery for lumbar sequestrectomy. Homeopathic treatment was compared to placebo, both in addition to usual pain management. The primary endpoint was pain relief measured with a visual analog scale. Secondary endpoints were the reduction of inpatient postoperative analgesic medication and change in sensory and affective pain perception.
The results show that the change in pain perception between baseline and day 3 did not significantly differ between the study arms. With respect to pain medication, total morphine equivalent doses did not differ significantly. However, a statistical trend and a moderate effect (d = 0.432) in the decrease of pain medication consumption in favor of the Hypericum group was observed.
The authors concluded that this is the first trial of homeopathy that evaluated the efficacy of Hypericum C200 after lumbar monosegmental spinal sequestrectomy. Although no significant differences between the groups could be shown, we found that patients who took potentiated Hypericum in addition to usual pain management showed lower consumption of analgesics. Further investigations, especially with regard to pain medication, should follow to better classify the described analgesic reduction.
For a number of reasons, this is a remarkably mysterious and quite hilarious study:
- Hypericum is recommended as an analgesic for neuropathic pain.
- According to the ‘like cures like’ axiom of homeopathy, it therefore must increase pain in such situations.
- Yet, the authors of this trial mounted an RCT to see whether it reduces pain.
- Thus they either do not understand homeopathy or wanted to sabotage it.
- As they are well-known pro-homeopathy researchers affiliated with a university that promotes homeopathy (Witten/Herdecke University, Herdecke, Germany), both explanations are highly implausible.
- The facts that the paper was published in a pro-SCAM journal (J Integr Complement Med), and the study was sponsored by the largest German firm of homeopathics (Deutsche Homoeopathische Union) renders all this even more puzzling.
- However, these biases do explain that the authors do their very best to mislead us by including some unwarranted ‘positive’ findings in their overall conclusions.
In the end, none of this matters, because the results of the study reveal that firstly the homeopathic ‘law of similars’ is nonsense, and secondly one homeopathic placebo (i.e. Hypericum C200) produces exactly the same outcomes as another, non-homeopathic placebo.