survey
According to Healthcare.gov, a primary care provider in the US is “a physician (MD or DO), nurse practitioner, clinical nurse specialist or physician assistant, as allowed under state law, who provides, coordinates or helps a patient access a range of healthcare services.” A growing movement exists to expand who can act as a primary care privider (PCP). Chiropractors have been a part of this expansion, but is that wise? This is the question recently asked by Katie Suleta of THE AMERICAN COUNCIL ON SCIENCE AND HEALTH In it, she explains that:
- chiropractors would like to act as PCPs,
- chiropractors are not trained in pharmacology,
- chiropractors receive some training in supplements,
- chiropractors wish to avoid pumping the body full of “synthetic” hormones and substances.
Subsequently, she adresses the chiropractic profession’s stance on vaccines.
First, look at similar professional organizations to establish a reasonable expectation. The American Medical Association has firmly taken a stance on vaccines and provides resources for physicians to help communicate with patients. There is no question about where they stand on the topic, whether it be vaccines in general or COVID-19 vaccines specifically. Ditto the American Osteopathic Association and American Association of Colleges of Osteopathic Medicine. There is a contingent of vaccine-hesitant MDs and DOs. There is also an anti-vax contingent of MDs and DOs. The vaccine hesitant can be considered misguided and cautious, while anti-vaxxers often have more misinformation and an underlying political agenda. The two groups pose a threat but are, thankfully, the minority. They’re also clearly acting against the recommendations of their professional organizations.
Let’s now turn to the American Chiropractic Association (ACA). Unlike the American Medical Association or American Osteopathic Association, they seem to take no stance on vaccines. None. Zip. Zilch. As of this writing, if you go to the ACA website and search for “vaccines,” zero results are returned. Venturing over to the ACA-CDID, there is a category under their “News and Articles” section for ‘Vaccines.’ This seems promising! However, when you click on it, it returns one article on influenza vaccines from Fox News from 2017. It’s not an original article. It’s not a perspective piece. No recommendations are to be found—nothing even on the COVID-19 vaccines. Basically, there is effectively nothing on ACA-CDID’s website either. We’re oh for two.
The last one we’ll try is DABCI University. No, it’s not a professional organization, but it does train DCs. The words ‘university’ and ‘internist’ are involved, so they must talk about vaccines…right? Wrong again. While there is a lot of content available only to paying members and students, the sections of their website that are publicly available are noticeably short on vaccine information. There is a section dedicated to articles, currently including five whole articles, and not a single one talked about vaccines. One report addresses the pharmacokinetics of coffee enemas, but none talks about one of the most fundamental tools PCPs have to help prevent illness.
Why It’s Important
Chiropractic was defined by DD. Palmer, its founder, as “a science of healing without drugs.” It relies on spinal manipulation. In traditional chiropractic, there is no room for medications at all. A rift has developed within the profession, and some chiropractors, those seeking that internal medicine certification, “try to avoid pumping the body with synthetic hormones and other prescriptions.”
During the COVID-19 pandemic, several prominent chiropractors publicly pushed anti-vaccine views. To highlight just a few prominent examples: Vax Con ’21, Mile Hi Chiro, and Ben Tapper. Vax Con ’21 was organized and orchestrated by the Chiropractic Society of Wisconsin. It featured Judy Mikovits, of Plandemic fame, as a speaker and touted her book with a forward written by Robert F. Kennedy Jr. It offered continuing education units (CEUs) to DCs to attend this anti-vaccine conference that peddled misinformation about COVID-19 vaccines and other prevention measures. Healthcare providers are often required to complete a certain number of continuing education units to maintain licensure, ensuring that they stay current and sharp as healthcare evolves or, in this case, devolves.
This conference was not unique in this either. Mile Hi Chiro was just held in Denver in September of this year, had several questionable speakers (including RFK and Ben Tapper of Disinformation Dozen fame), and offered continuing education. If professional conferences offer continuing education units for attendees and push vaccine misinformation, that should concern everyone. Especially if the profession in question wants to act as PCPs.
Despite training in a system that believes “the body has an innate intelligence, and the power to heal itself if it is functioning properly, and that chiropractic care can help it do that,” without medications, but frequently with supplements, roughly 58% of Oregon’s chiropractors were vaccinated against COVID-19. That said, their training and inclination, along with the silence of their professional organizations and the chiropractic conferences featuring anti-vaccine sentiment, make them a profession that, at the very least, doesn’t consider vaccinations or medications viable health alternatives. We’re now talking about an entire profession that wants to be PCPs.
Irrespective of your belief about the efficacy of COVID-19 vaccination, the germ theory of disease remains unchallenged. Anyone unwilling to work to treat and prevent infectious diseases within their community with the most effective means at our disposal should not be allowed to dispense medical advice. Chiropractors lack the basic training that a PCP should have. I’ve said it before and I’ll say it again: I want healthcare accessible for everyone. But, if you’re looking for a PCP, consider going to an MD, DO, NP, or PA – they come fully equipped for your primary care needs.
Regular readers of this blog will be aware that I have discussed the thorny issue of chiros and vaccinations many times before, e.g.:
- Chiropractic and Public Health
- The International Chiropractors Association’s Statement on Vaccination
- The General Chiropractic Council’s ‘Registrant Survey 2020’ has just been published
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Vaccination: chiropractors “espouse views which aren’t evidence based”
- Patients consulting chiropractors, homeopaths, or naturopaths are less likely to agree to the flu jab
- “The uncensored truth” about COVID-19 vaccines” … as told by some chiro loons
- Beliefs and behaviors of US chiropractors
- Media attention forces (some) chiropractors to get their act together
- Ever wondered why so many chiropractors are profoundly anti-vax?
I agree with Katie Suleta that the issue is important and thank her for raising it. I also agree with her conclusion that, if you’re looking for a PCP, consider going to an MD, DO, NP, or PA – they come fully equipped for your primary care needs.
Do not consult chiropractors.
The utilization of certain forms of so-called alternative medicine (SCAM) is prevalent among adults. While researchers have extensively studied the factors influencing SCAM use in Western countries, significant barriers to its adoption remain. This paper draws attention to the obstacles faced by individuals in their journey to using SCAM.
Qualitative interviews were conducted with 21 patients who had turned to SCAM for managing a chronic illness/condition and had been chosen through a ‘snowball sampling’ strategy. These in-depth, face-to-face interviews occurred in Miami, USA, during 2014-15. The sampling, data collection, and analysis processes of this study adhered to the principles outlined in Charmaz’s constructivist grounded theory approach.
From the data, three central barriers to SCAM utilization in the US emerged: 1) Financial barriers: A significant portion of SCAM treatments is not covered by insurance, making them cost-prohibitive for many. 2) Skepticism and discouragement: Both conventional medical practitioners and a segment of the public exhibited a noticeable trend towards discouraging SCAM use. 3) Evaluation challenges: Patients expressed difficulty in assessing the efficacy and benefits of various SCAM treatments compared to their costs.
The author concluded that despite the widespread interest in and use of SCAM in the US, numerous barriers hinder its broader integration into mainstream healthcare. These obstacles not only restrict healthcare choices for the general public but also appear to favor a select demographic, potentially based on income and availability of information.
So, 21 individuals chosen via a snowball sampling strategy located in Miami feel that there were obstacles to using SCAM.
No!
These obstacles existed about 10 myears ago.
No!
The obstacles only existed in the imagination of these 21 guys.
No!
The alleged obstacles are hardly relevant and therefore are not truly obstacles.
The only truly relevant obstacle to SCAM-use is the fact that most SCAMs have either not been shown to work, or shown not to work!
Perhaps surprisingly, the author concedes that their study has certain limitations: “This study had some inherent limitations. The sample, while chosen based on theoretical sampling to achieve theoretical saturation, was both small and self-selected. This limits the broad applicability of the findings. Moreover, individuals from lower socio-economic backgrounds were not represented in the sample, which may have overlooked important perspectives on affordable SCAM options. The sample did not offer a detailed exploration of SCAM perceptions across diverse demographic categories, such as social class or ethnicity. It’s also essential to highlight that this research was conducted exclusively in Miami, a city with a significant population of ethnic minorities in the US. This demographic context could have uniquely influenced the feedback from SCAM users.”
If I may, I will another limitation: This study was utter nonsense from its conception to its publication!
You might think that all of this is quite trivial and that I am rather petty. If you look into Medline and realize how many such useless and counter-productive SCAM studies are being published, you might change your mind.
Conspiracy beliefs (CBs) can have substantial consequences on health behaviours by influencing both conventional and non-conventional medicine uptake. They can target powerful groups (i.e. upward CBs) or powerless groups (i.e. downward CBs). Considering their repercussions in oncology, it appears useful to understand how CBs are related to the intentions to use conventional and so-called alternative medicines (SCAM), defined as “medical products and practices that are not part of standard medical care” including practices
such as mind–body therapies, botanicals, energy healing or naturopathic medicine.
This paper includes two pre-registered online correlational studies on a general French population (Study 1 N = 248, recruited on social media Mage = 40.07, SDage = 14.78; 205 women, 41 men and 2 non-binaries; Study 2 N = 313, recruited on social media and Prolific, Mage = 28.91, SDage = 9.60; 154 women, 149 men and 10 non-binaries). the researchers investigated the links between generic and chemotherapy-related CBs and intentions to use conventional or SCAMs. Study 2 consisted of a conceptual replication of Study 1, considering the orientation of CBs.
Generic CBs and chemotherapy-related CBs appear strongly and positively correlated, negatively correlated with intentions to take conventional medicine and positively with intentions to take SCAM. The link between generic CBs and medication intention is fully mediated by chemotherapy-related CBs. When distinguished, upward CBs are a stronger predictor of chemotherapy-related CBs than downward CBs.
The authors concluded that the findings suggest that intentions to use medicine are strongly associated with CBs. This has several important implications for further research and practice, notably on the presence and effects of CBs on medication behaviours in cancer patients.
Sadly, the influence of CBs is not confined to the field of oncology but applies across all diseases and conditions. We have seen and discussed these issues in several previous posts, e.g.:
- Conspiracy Beliefs Predict Health Behavior and Well-being during the Pandemic
- Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines
- Mistrust + Misinformation —> CONSPIRACY THEORY
- Conspiracy theories and dangerous recommendations via YouTube videos
- Conspiracy theories, assumptions, opinions, evidence and scientific facts
- A conspiracy theory seems to be driving the popularity of alternative medicine
The most impressive evidence, however, is regularly being provided by some of the people who post comments on this blog. Collectively, this evidence has prompted me to postulate that SCAM itself can be seen as a consiracy theory.
Many of you will be familiar with the ‘ALTERNATIVE MEDICINE HALL OF FAME’. It is my creation and meant to honour reserchers who have dedicated much of their professional career to investigating a form of so-called alternative medicine (SCAM) without ever publishing negative conclusions about it. Obviously, if anyone studies any therapy, he/she will occasionally produce a negative finding. This would be the case, even if he/she tests an effective treatment. However, if the treatment in question comes from the realm of SCAM, one would expect negative results fairly regularly. No therapy works well under all conditions, and to the best of my knowledge, no SCAM is a panacea!
This is why researchers who defy this inevitability are remarkable. If someone tests a treatment that is at best dubious and at worst bogus, we are bound to see some studies that are not positive. He/she would thus have a high or normal ‘TRUSTWORTHINESS INDEX‘ (another creation of mine which, I think, is fairly self-explanatory). Conversely, any researcher who does manage to publish nothing but positive results of a SCAM is bound to have a very low ‘TRUSTWORTHINESS INDEX‘. In other words, these people are special, so much so that I decided to honour such ‘geniuses’ by admitting them to my ALTERNATIVE MEDICINE OF FAME.
So far, this elite group of people comprises the following individuals:
- Helge Franke (osteopathy, Germany)
- Tery Oleson (acupressure , US)
- Jorge Vas (acupuncture, Spain)
- Wane Jonas (homeopathy, US)
- Harald Walach (various SCAMs, Germany)
- Andreas Michalsen ( various SCAMs, Germany)
- Jennifer Jacobs (homeopath, US)
- Jenise Pellow (homeopath, South Africa)
- Adrian White (acupuncturist, UK)
- Michael Frass (homeopath, Austria)
- Jens Behnke (research officer, Germany)
- John Weeks (editor of JCAM, US)
- Deepak Chopra (entrepreneur, US)
- Cheryl Hawk (chiropractor, US)
- David Peters (osteopathy, homeopathy, UK)
- Nicola Robinson (TCM, UK)
- Peter Fisher (homeopathy, UK)
- Simon Mills (herbal medicine, UK)
- Gustav Dobos (various SCAMs, Germany)
- Claudia Witt (homeopathy, Germany/Switzerland)
- George Lewith (acupuncture, UK)
- John Licciardone (osteopathy, US)
You will notice that the group does not yet contain a representative of anthroposophic medicine. Today, I intend to rectify this oversight by admitting Helmut Kiene (1952-). He has published plenty of studies and reviews on his pet subject; here are the ones that I found on Medline:
- Anthroposophic therapies in chronic disease: the Anthroposophic Medicine Outcomes Study (AMOS). Eur J Med Res. 2004 Jul 30;9(7):351-60.
- Anthroposophic medical therapy in chronic disease: a four-year prospective cohort study. Hamre HJ, Witt CM, Glockmann A, Ziegler R, Willich SN, Kiene H.BMC Complement Altern Med. 2007 Apr 23;7:10. doi: 10.1186/1472-6882-7-10.
- Anthroposophic art therapy in chronic disease: a four-year prospective cohort study. Hamre HJ, Witt CM, Glockmann A, Ziegler R, Willich SN, Kiene H.Explore (NY). 2007 Jul-Aug;3(4):365-71. doi: 10.1016/j.explore.2007.04.008.
- Rhythmical massage therapy in chronic disease: a 4-year prospective cohort study. Hamre HJ, Witt CM, Glockmann A, Ziegler R, Willich SN, Kiene H.J Altern Complement Med. 2007 Jul-Aug;13(6):635-42. doi: 10.1089/acm.2006.6345
- Anthroposophic vs. conventional therapy for chronic low back pain: a prospective comparative study. Hamre HJ, Witt CM, Glockmann A, Wegscheider K, Ziegler R, Willich SN, Kiene H.Eur J Med Res. 2007 Jul 26;12(7):302-10.
- Viscum album L. extracts in breast and gynaecological cancers: a systematic review of clinical and preclinical research. Kienle GS, Glockmann A, Schink M, Kiene H.J Exp Clin Cancer Res. 2009 Jun 11;28(1):79. doi: 10.1186/1756-9966-28-79.
- Anthroposophic therapy for children with chronic disease: a two-year prospective cohort study in routine outpatient settings. Hamre HJ, Witt CM, Kienle GS, Meinecke C, Glockmann A, Willich SN, Kiene H.BMC Pediatr. 2009 Jun 19;9:39. doi: 10.1186/1471-2431-9-39
- Predictors of outcome after 6 and 12 months following anthroposophic therapy for adult outpatients with chronic disease: a secondary analysis from a prospective observational study. Hamre HJ, Witt CM, Kienle GS, Glockmann A, Willich SN, Kiene H.BMC Res Notes. 2010 Aug 3;3:218. doi: 10.1186/1756-0500-3-218.
- Pulpa dentis D30 for acute reversible pulpitis: A prospective cohort study in routine dental practice. Hamre HJ, Mittag I, Glockmann A, Kiene H, Tröger W.Altern Ther Health Med. 2011 Jan-Feb;17(1):16-21.
- Use and safety of anthroposophic medications for acute respiratory and ear infections: a prospective cohort study. Hamre HJ, Glockmann A, Fischer M, Riley DS, Baars E, Kiene H.
- [Clinical research on anthroposophic medicine:update of a health technology assessment report and status quo]. Kienle GS, Glockmann A, Grugel R, Hamre HJ, Kiene H.Forsch Komplementmed. 2011;18(5):269-82. doi: 10.1159/000331812. Epub 2011 Oct 4.
- Anthroposophical medicine: a systematic review of randomised clinical trials. Kienle GS, Hamre HJ, Kiene H.Wien Klin Wochenschr. 2004 Jun 30;116(11-12):407-8; author reply 408. doi: 10.1007/BF03040923.
- Eurythmy therapy in chronic disease: a four-year prospective cohort study. Hamre HJ, Witt CM, Glockmann A, Ziegler R, Willich SN, Kiene H.BMC Public Health. 2007 Apr 23;7:61. doi: 10.1186/1471-2458-7-61.
- Long-term outcomes of anthroposophic therapy for chronic low back pain: A two-year follow-up analysis. Hamre HJ, Witt CM, Kienle GS, Glockmann A, Ziegler R, Willich SN, Kiene H.J Pain Res. 2009 Jun 25;2:75-85. doi: 10.2147/jpr.s5922.
- Health costs in anthroposophic therapy users: a two-year prospective cohort study. Hamre HJ, Witt CM, Glockmann A, Ziegler R, Willich SN, Kiene H.BMC Health Serv Res. 2006 Jun 2;6:65. doi: 10.1186/1472-6963-6-65.
- Use and safety of anthroposophic medications in chronic disease: a 2-year prospective analysis. Hamre HJ, Witt CM, Glockmann A, Tröger W, Willich SN, Kiene H.Drug Saf. 2006;29(12):1173-89. doi: 10.2165/00002018-200629120-00008.
- Anthroposophic therapy for chronic depression: a four-year prospective cohort study. Hamre HJ, Witt CM, Glockmann A, Ziegler R, Willich SN, Kiene H.BMC Psychiatry. 2006 Dec 15;6:57. doi: 10.1186/1471-244X-6-57.
- Health costs in patients treated for depression, in patients with depressive symptoms treated for another chronic disorder, and in non-depressed patients: a two-year prospective cohort study in anthroposophic outpatient settings. Hamre HJ, Witt CM, Glockmann A, Ziegler R, Kienle GS, Willich SN, Kiene H.Eur J Health Econ. 2010 Feb;11(1):77-94. doi: 10.1007/s10198-009-0203-0.
- Outcome of anthroposophic medication therapy in chronic disease: a 12-month prospective cohort study. Hamre HJ, Witt CM, Glockmann A, Ziegler R, Kienle GS, Willich SN, Kiene H.Drug Des Devel Ther. 2009 Feb 6;2:25-37.
- Clinical research in anthroposophic medicine. Hamre HJ, Kiene H, Kienle GS.Altern Ther Health Med. 2009 Nov-Dec;15(6):52-5.
- Anthroposophic therapy for attention deficit hyperactivity: a two-year prospective study in outpatients. Hamre HJ, Witt CM, Kienle GS, Meinecke C, Glockmann A, Ziegler R, Willich SN, Kiene H.Int J Gen Med. 2010 Aug 30;3:239-53. doi: 10.2147/ijgm.s11725.
- Anthroposophic therapy for asthma: A two-year prospective cohort study in routine outpatient settings. Hamre HJ, Witt CM, Kienle GS, Schnürer C, Glockmann A, Ziegler R, Willich SN, Kiene H.J Asthma Allergy. 2009 Nov 24;2:111-28.
- Anthroposophic therapy for migraine: a two-year prospective cohort study in routine outpatient settings. Hamre HJ, Witt CM, Kienle GS, Glockmann A, Ziegler R, Rivoir A, Willich SN, Kiene H.Open Neurol J. 2010;4:100-10.
- Antibiotic Use in Children with Acute Respiratory or Ear Infections: Prospective Observational Comparison of Anthroposophic and Conventional Treatment under Routine Primary Care Conditions. Hamre HJ, Glockmann A, Schwarz R, Riley DS, Baars EW, Kiene H, Kienle GS.Evid Based Complement Alternat Med. 2014;2014:243801.
- An assessment of the scientific status of anthroposophic medicine, applying criteria from the philosophy of science. Baars EW, Kiene H, Kienle GS, Heusser P, Hamre HJ.Complement Ther Med. 2018 Oct;40:145-150.
- Anthroposophic vs. conventional therapy of acute respiratory and ear infections: a prospective outcomes study. Hamre HJ, Fischer M, Heger M, Riley D, Haidvogl M, Baars E, Bristol E, Evans M, Schwarz R, Kiene H.Wien Klin Wochenschr. 2005 Apr;117(7-8):256-68. doi: 10.1007/s00508-005-0344-9.
- Long-term outcomes of anthroposophic treatment for chronic disease: a four-year follow-up analysis of 1510 patients from a prospective observational study in routine outpatient settings. Hamre HJ, Kiene H, Glockmann A, Ziegler R, Kienle GS.BMC Res Notes. 2013 Jul 13;6:269. doi: 10.1186/1756-0500-6-269
- Eurythmy Therapy in anxiety. Kienle GS, Hampton Schwab J, Murphy JB, Andersson P, Lunde G, Kiene H, Hamre HJ.Altern Ther Health Med. 2011 Jul-Aug;17(4):56-63
- Mistletoe in cancer – a systematic review on controlled clinical trials. Kienle GS, Berrino F, Büssing A, Portalupi E, Rosenzweig S, Kiene H.Eur J Med Res. 2003 Mar 27;8(3):109-19.
- Anthroposophic therapy of respiratory and ear infections. Hamre HJ, Fischer M, Heger M, Riley D, Haidvogl M, Baars E, Bristol E, Evans M, Schwarz R, Kiene H.Wien Klin Wochenschr. 2005 Jul;117(13-14):500-1. doi: 10.1007/s00508-005-0389-9
- Complementary cancer therapy: a systematic review of prospective clinical trials on anthroposophic mistletoe extracts.
Eur J Med Res. 2007 Mar 26;12(3):103-19.
- Review article: Influence of Viscum album L (European mistletoe) extracts on quality of life in cancer patients: a systematic review of controlled clinical studies. Kienle GS, Kiene H.Integr Cancer Ther. 2010 Jun;9(2):142-57.
- [Anthroposophic medicine: health technology assessment report – short version].
Forsch Komplementmed. 2006;13 Suppl 2:7-18. doi: 10.1159/000093481. Epub 2006 Jun 26.
- Bilateral Asynchronous Renal Cell Carcinoma With Lung Metastases: A Case Report of a Patient Treated Solely With High-dose Intravenous and Subcutaneous Viscum album Extract for a Second Renal Lesion. Reynel M, Villegas Y, Kiene H, Werthmann PG, Kienle GS.Anticancer Res. 2019 Oct;39(10):5597-5604. doi: 10.21873/anticanres.13754.
- Long-term survival of a patient with an inoperable thymic neuroendocrine tumor stage IIIa under sole treatment with Viscum album extract: A CARE compliant clinical case report. Reynel M, Villegas Y, Werthmann PG, Kiene H, Kienle GS.Medicine (Baltimore). 2020 Jan;99(5):e18990. doi: 10.1097/MD.0000000000018990
- Long-Term Survival of a Patient with Recurrent Dedifferentiated High-Grade Liposarcoma of the Retroperitoneum Under Adjuvant Treatment with Viscum album L. Extract: A Case Report. Reynel M, Villegas Y, Werthmann PG, Kiene H, Kienle GS.Integr Cancer Ther. 2021 Jan-Dec;20:1534735421995258. doi: 10.1177/1534735421995258.
- Intralesional and subcutaneous application of Viscum album L. (European mistletoe) extract in cervical carcinoma in situ: A CARE compliant case report. Reynel M, Villegas Y, Kiene H, Werthmann PG, Kienle GS.Medicine (Baltimore). 2018 Nov;97(48):e13420.
- High-Dose Viscum album Extract Treatment in the Prevention of Recurrent Bladder Cancer: A Retrospective Case Series.
Perm J. 2015 Fall;19(4):76-83. doi: 10.7812/TPP/15-018.
- Disappearance of an advanced adenomatous colon polyp after intratumoural injection with Viscum album (European mistletoe) extract: a case report. von Schoen-Angerer T, Goyert A, Vagedes J, Kiene H, Merckens H, Kienle GS.J Gastrointestin Liver Dis. 2014 Dec;23(4):449-52. doi: 10.15403/jgld.2014.1121.234.acpy.
- Viscum Album in the Treatment of a Girl With Refractory Childhood Absence Epilepsy. von Schoen-Angerer T, Madeleyn R, Kienle G, Kiene H, Vagedes J.J Child Neurol. 2015 Jul;30(8):1048-52. doi: 10.1177/0883073814541473. Epub 2014 Jul 17.
- Improvement of Asthma and Gastroesophageal Reflux Disease With Oral Pulvis stomachicus cum Belladonna, a Combination of Matricaria recutita, Atropa belladonna, Bismuth, and Antimonite: A Pediatric Case Report. von Schoen-Angerer T, Madeleyn R, Kiene H, Kienle GS, Vagedes J.Glob Adv Health Med. 2016 Jan;5(1):107-11. doi: 10.7453/gahmj.2015.019. Epub 2016 Jan 1.
- Use of Iscador, an extract of European mistletoe (Viscum album), in cancer treatment: prospective nonrandomized and randomized matched-pair studies nested within a cohort study. Grossarth-Maticek R, Kiene H, Baumgartner SM, Ziegler R.Altern Ther Health Med. 2001 May-Jun;7(3):57-66, 68-72, 74-6 passim
WHAT A LIST!
It makes several things very clear to me:
- Kiene is a productive researcher
- He likes observational studies and case reports
- He dislikes the idea of rigorously testing a hypothesis
- He never publishes a negative finding about anthroposophical medicine
- He certainly deserves to be admitted to the ALTERNATIVE MEDICINE HALL OF FAME!
Welcome Helmut
Vaccine hesitancy has become a threat to public health, especially as it is a phenomenon that has also been observed among healthcare professionals.
In this study, an international team of researchers analyzed the relationship between endorsement of so-called alternative medicine (SCAM) and vaccination attitudes and behaviors among healthcare professionals, using a cross-sectional sample of physicians with vaccination responsibilities from four European countries:
- Germany,
- Finland,
- Portugal,
- France.
In total the sample amounted to 2,787 physicians.
The results suggest that, in all the participating countries, SCAM endorsement is associated with lower frequency of vaccine recommendation, lower self-vaccination rates, and being more open to patients delaying vaccination, with these relationships being mediated by distrust in vaccines. A latent profile analysis revealed that a profile characterized by higher-than-average SCAM endorsement and lower-than-average confidence and recommendation of vaccines occurs, to some degree, among 19% of the total sample, although these percentages varied from one country to another:
- 24% in Germany,
- 18% in France,
- 10% in Finland,
- 6% in Portugal.
These results constitute a call to consider health care professionals’ attitudes toward SCAM as a factor that could hinder the implementation of immunization campaigns.
The authors also point out that the link between SCAM endorsement and negative attitudes toward vaccines has been documented in previous research among the general public. A systematic review, which categorized arguments against vaccines retrieved from peer-reviewed articles and debunking texts published by international fact checking agencies, identified a category of arguments largely based on alternative health beliefs related to SCAM. This category was the third most common in the scientific and fact-checking literature. Furthermore, in a British study, anti-vaccination arguments related to SCAM were also among the most endorsed arguments by individuals. These results suggest that SCAM beliefs play an important role in individuals’ justification of their hesitant attitudes toward vaccines for both adults and children. Analyses of samples from the Australian, Finnish, American, and Spanish general populations found that positive attitudes toward SCAM were related to negative attitudes toward vaccines. In a recent large-scale study in 18 European countries, parental consultation with homeopaths was associated with higher vaccine hesitancy than consultation with pediatricians or nurses. Moreover, a systematic review found that SCAM use tended to be positively associated with lower childhood immunization. Similar findings were reported also from the US and Australia.
There are several potential causes for the observed relationship between vaccine hesitancy and SCAM. Since SCAM use occurs more frequently at the poles of the disease spectrum (i.e., in cases of minor or life-threatening illness), SCAM use has been identified as a marker of both misperception of risk and frustration with regular healthcare (e.g., negative prognosis or lack of remission of symptoms). Accordingly, SCAM-related health conceptions could be motivating healthcare practitioners (HCPs) to be more reluctant to recommend and receive vaccinations both for illnesses that are perceived as minor and in cases of severe clinical pictures. There are also reasons related to the potential alignment between SCAM and the ideology or worldview of the HCP, such as their distrust in “Big Pharma” or a general disregard for scientific knowledge. Along the same lines, it has been shown that the main reasons for their preference for SCAM included a greater affinity between SCAM, their do-it-yourself approach to health care, and their sympathy for natural and allegedly harm-free products in contrast to medications marketed by pharmaceutical companies, which were perceived as ineffective, “toxic” and “adulterating.”
Besides these implicit reasons, some SCAM traditions are theoretically incompatible with vaccination and portrayed as a valid, or even superior, alternative to scientific knowledge. A quantitative study found that pro-SCAM and anti-vaccination attitudes both reflect beliefs contrary to basic scientific knowledge, such as “an imbalance between energy currents lies behind many illnesses” and “an illness should be treated with a medicine that has properties similar to those of the illness.” An example of these SCAM-related beliefs that contradict the theoretical basis of vaccinations is “homeopathic immunization” through so-called “nosodes” – orally administered extreme dilutions of infectious agents. Similarly, Rudolf Steiner and Ryke Geerd Hamer, promoters of anthroposophic medicine and ‘German New Medicine’, respectively, have sown doubts about vaccinations based on their conceptions of the etiology and treatment of diseases. Consequently, strong science denial and vaccine hesitancy can be found within these communities, and outbreaks of vaccine-preventable diseases, such as measles and whooping cough, have been reported in educational centers linked to anthroposophy.
PS
This project has received funding from the European Union’s Horizon 2020 research and innovation programme.
So-called alternative medicine (SCAM) is widely used in Saudi Arabia. One of the common practices is the use of camel urine alone or mixed with camel milk for the treatment of cancer, which is often supported by religious beliefs.
This study observed cancer patients who insisted on using camel urine, and to offer some clinically relevant recommendations. The authors observed 20 cancer patients (15 male, 5 female) from September 2020 to January 2022 who insisted on using camel urine for treatment. They documented the demographics of each patient, the method of administering the urine, reasons for refusing conventional treatment, period of follow-up, and the outcome and side effects.
All the patients had radiological investigations before and after their treatment with camel urine. All of them used a combination of camel urine and camel milk, and their treatment ranged from a few days to 6 months. They consumed an average of 60 ml urine/milk per day. No clinical benefit was observed after the treatment; 2 patients developed brucellosis. Eleven patients changed their mind and accepted conventional antineoplastic treatment and 7 were too weak to receive further treatment; they died from the disease.
The authors concluded that camel urine had no clinical benefits for any of the cancer patients, it may even have caused zoonotic infection. The promotion of camel urine as a traditional medicine should be stopped because there is no scientific evidence to support it.
If you suspected that this was a hoax, you were wrong!
Here is a recent paper on the ‘therapeutic potentials of camel urine’:
Camel urine has traditionally been used to treat multiple human diseases and possesses the most beneficial effects amongst the urine of other animals. However, scientific review evaluating the anticancer, antiplatelet, gastroprotective and hepatoprotective effects of camel urine is still scarce. Thus, this scoping review aimed to provide scientific evidence on the therapeutic potentials of camel urine. Three databases were searched to identify relevant articles (Web of Science, PubMed and Scopus) up to September 2020. Original articles published in English that investigated the effects of camel urine in various diseases were included. The literature search identified six potential articles that met all the inclusion criteria. Three articles showed that camel urine possesses cytotoxic activities against different types of cancer cells. Two studies revealed camel urine’s protective effects against liver toxicity and gastric ulcers, whilst another study showed the role of camel urine as an antiplatelet agent. All studies demonstrated significant positive effects with different effective dosages. Thus, camel urine shows promising therapeutic potential in treating human diseases, especially cancer. However, the standardised dosage and potential side effects should be determined before camel urine could be offered as an alternative treatment.
I have often asked myself the question whether some SCAMs are too absurd to merit scientific study. Over the years, I changed my mind on it; while initially I tended to answer it in the negative, I now think that YES: some ideas – even those that are ancient and, as Charles Windsor would argue, have thus stood the ‘test of time’ – are not worth the effort. Camel urine as a therapy might well be one of them.
The KFF provides reliable, accurate, and non-partisan information to help inform health policy in the US. The KFF has just released its ‘Health Misinformation Tracking Poll Pilot‘ examining the public’s media use and trust in sources of health information and measuring the reach of specific false and inaccurate claims surrounding three health-related topics: COVID-19 and vaccines, reproductive health, and gun violence. It makes grimm reading indeed. Here are but a few excerpts pertaining to health/vaccination:
Health misinformation is widespread in the US with 96% of adults saying they have heard at least one of the ten items of health-related misinformation asked about in the survey. The most widespread misinformation items included in the survey were related to COVID-19 and vaccines, including that the COVID-19 vaccines have caused thousands of deaths in otherwise healthy people (65% say they have heard or read this) and that the MMR vaccines have been proven to cause autism in children (65%).
Regardless of whether they have heard or read specific items of misinformation, the survey also asked people whether they think each claim is definitely true, probably true, probably false, or definitely false. For most of the misinformation items included in the survey, between one-fifth and one-third of the public say they are “definitely” or “probably true.” The most frequently heard claims are related to COVID-19 and vaccines.
Uncertainty is high when it comes to health misinformation. While fewer than one in five adults say each of the misinformation claims examined in the survey are “definitely true,” larger shares are open to believing them, saying they are “probably true.” Many lean towards the correct answer but also express uncertainty, saying each claim is “probably false.” Fewer tend to be certain that each claim is false, with the exception of the claim that more people have died from the COVID-19 vaccines than from the virus itself, which nearly half the public (47%) recognizes as definitely false.
Across the five COVID-19 and vaccine related misinformation items, adults without a college degree are more likely than college graduates to say these claims are definitely or probably true. Notably, Black adults are at least ten percentage points more likely than White adults to believe some items of vaccine misinformation, including that the COVID-19 vaccines have caused thousands of sudden deaths in otherwise healthy people, and that the MMR vaccines have been proven to cause autism in children. Black (29%) and Hispanic (24%) adults are both more likely than White adults (17%) to say that the false claim that “more people have died from the COVID-19 vaccine than have died from the COVID-19 virus” is definitely or probably true. Those who identify as Republicans or lean towards the Republican Party and pure independents stand out as being more likely than Democratic leaning adults to say each of these items is probably or definitely true. Across community types, rural residents are more likely than their urban and suburban counterparts to say that some false claims related to COVID vaccines are probably or definitely true, including that the vaccines have been proven to cause infertility and that more people have died from the vaccine than from the virus.
Educational attainment appears to play a particularly important role when it comes to susceptibility to COVID-19 and vaccine misinformation. Six in ten adults with college degrees say none of the five false COVID-19 and vaccine claims are probably or definitely true, compared to less than four in ten adults without a degree. Concerningly, about one in five rural residents (19%), adults with a high school education or less (18%), Black adults (18%), Republicans (20%), and independents (18%) say four or five of the false COVID-19 and vaccine misinformation items included in the survey are probably or definitely true.
________________________________
If you have followed some of the comments on this blog, you might find it hard to be surprised!
I do encourage you to read the full article.
The increasing demand for fertility treatments has led to the rise of private clinics offering so-called alternative medicine (SCAM) treatments. Even King Charles has recently joined in with this situalion. One of the most frequently offered SCAM infertility treatment is acupuncture. However, there is no good evidence to support the effectiveness of acupuncture in treating infertility.
This study evaluated the scope of information provided by SCAM fertility clinics in the UK. A content analysis was conducted on 200 websites of SCAM fertility clinics in the UK that offer acupuncture as a treatment for infertility. Of the 48 clinics that met the eligibility criteria, the majority of the websites did not provide sufficient information on: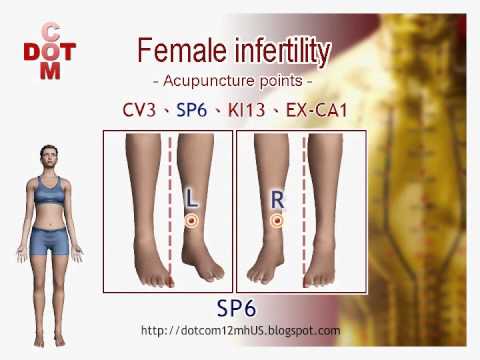
- the efficacy,
- the risks,
- the success rates
of acupuncture for infertility.
The authors concluded that this situation has the potential to infringe on patient autonomy, provide false hope and reduce the chances of pregnancy ever being achieved as fertility declines during the time course of ineffective acupuncture treatment.
The authors are keen to point out that their investigation has certain limitations. The study only analysed the information provided on the clinics’ websites and did not assess the quality of the treatment provided by the clinics.
Therefore, the study’s fndings cannot be generalized to the quality of the acupuncture treatment provided by the clinics.
Nonetheless the paper touches on very important issues: far too many health clinics that offer SCAM for this or that indication operate way outside the ethically (and legally) acceptable norm. They advertise their services without making it clear that they are neither effective nor safe. Desperate consumers thus fall for their promises. In the case of infertility, this might result merely in frustration and loss of (often substantial amounts of) money. In the case of serious disease, such as cancer, this often results in premature death.
It is time, I think, that this entire sector is regualted in a way that it does not endanger the well-being, health, or life of consumers.
Spiritual healing has been defined as the direct interaction between one individual (the healer) and a patient, with the intention of improving the patient’s condition or curing the illness. Treatment can occur through personal, direct contact between healer and patient or at a (sometimes large) distance. Spiritual healers, who are usually not medically qualified, believe that the therapeutic effect results from the channelling of ‘energy’ from an undefined source via the healer to the patient. The main problem with this concept is that there is no evidence that this energy actually exists. Therefore, the assumptions on which spiritual healing is based lack plausibility.
The central claim of healers is that they promote or facilitate self-healing and wellbeing, both of which could be relevant to patients with any type of condition. An article by enthusiasts of spiritual healing explains: “All conditions can be treated by spiritual healing—but not all people. Some people are more receptive than others to this treatment, due to a number of factors such as karma and mental outlook. As such the results of healing can vary a great deal. If the patient has faith in the technique and the healer, this will of course aid the healing process, but is not necessary; this is not faith healing as practiced in some religions—it is based instead on spiritual energy. This being the case, it is possible for a skeptic to receive healing and benefit from it.”
The evidence from clinical trials of spiritual healing is contradictory. Many studies have serious flaws, and the most reliable trials fail to show effects beyond placebo. Research papers often fail to differentiate between different types of paranormal healing. One Cochrane, for instance, review “found inconclusive evidence that interventions with spiritual or religious components for adults in the terminal phase of a disease may or may not enhance well-being. Such interventions are under-evaluated. All five studies identified were undertaken in the same country, and in the multi-disciplinary palliative care interventions it is unclear if all participants received support from a chaplain or a spiritual counsellor. Moreover, it is unclear in all the studies whether the participants in the comparative groups received spiritual or religious support, or both, as part of routine care or from elsewhere. The paucity of quality research indicates a need for more rigorous studies.”
Many people believe that spiritual healing is harmless. Sadly, this is not the case. The BBC’s ‘Women’s Hour’ reported on 9 August this year about serious abuses of spiritual healers. Here you can find the published test of the broadcast:
Spiritual healing is extremely popular in many countries in the Middle East and North Africa. But the practice is unregulated and that means women are vulnerable to sexual exploitation. An investigation by BBC News Arabic has uncovered allegations of widespread sexual abuse by healers in Sudan and Morocco. Clare McDonnell is joined by the BBC’s Hanan Razek and Senior Women’s Rights Researcher at Human Rights Watch, Rothna Begum, to discuss.
And here you can listen to the actual broadcast. Briefly, what it reveales is deeply shocking:
- Spiritual healing is extremely popular in Sudan and Morocco.
- Healers charge hefty sums and healing is big business.
- Anyone regardless of background or training can call themselves a healer.
- There is no regulation whatsoever.
- Healers claim to cure illnesses, expell evil spirits, help with emotional problems, etc.
- For the programme, the BBC asked 80 women who had received healing.
- They accused 60 different healers of sexual transgression, including rape.
- Undercover recording revealed a healer placing his hand on a woman’s abdomen and then putting a finger “all the way down”.
- The police refuses to investigate if a women complains.
- The authorities refuse to take notice of the problem.
- A minister was quoted stating that there is no need for regulation.
- Another one said that the political athmosphere is not allowing to investigate the issue.
______________________
The references for the evidence cited above can be found here.
“We are hugely concerned about the welfare of doctors and healthcare workers with long COVID”. These are the first words of a comprehensive survey of UK doctors with post-acute COVID health complications. It reveals that these doctors experience symptoms such as:
- fatigue,
- headaches,
- muscular pain,
- nerve damage,
- joint pain,
- respiratory problems.
Around 60% of doctors said that post-acute COVID ill health has affected their ability to carry out day-to-day activities on a regular basis. 18% reported that they were now unable to work due to their post-acute COVID ill-health, and only 31% said they were working full-time, compared with more than half before the onset of their illness.
The report demands financial support for doctors and healthcare staff with post-acute COVID, post-acute COVID to be recognized as an occupational disease in healthcare workers, with a definition that covers all of the debilitating disease’s symptoms and for improved access to physical and mental health services to aid comprehensive assessment, appropriate investigations and treatment. The report also calls for greater workplace protection for healthcare staff risking their lives for others and better support for post-acute COVID sufferers to return to work safely if they can, including a flexible approach to the use of workplace adjustments.
In November 2021, an online survey investigating the emotional states of depression, anxiety, stress, compassion satisfaction, and compassion fatigue was administered to 78 Italian healthcare workers (HCWs). Between 5 and 20% of the cohort showed the effects of the adverse psychological impact of the pandemic and more than half of them experienced medium levels of compassion fatigue as well as a medium level of compassion satisfaction. The results also show that those with fewer years of clinical practice might be at greater risk of burnout, anxiety, and stress symptoms and might develop a lower level of compassion satisfaction. Moreover, the factors that potentially contribute to poor mental health, compassion fatigue, and compassion satisfaction seem to differ between residents and specialist physicians.
A cross-sectional study was conducted from September 2021 to April 2022 and targeted all physicians working at King Fahd Hospital of the University, Al Khobar, Saudi Arabia. Patient Health Questionnaire-9 and General Anxiety Disorder-7 were used to elicit self-reported data regarding depression and anxiety, respectively. In addition, sociodemographic and job-related data were collected. A total of 438 physicians responded, of which 200 (45.7%) reported symptoms of depression and 190 (43.4%) of anxiety. Being aged 25-30 years, female, resident, and reporting a reduction in work quality were factors significantly associated with both anxiety and depression. Female gender (AOR = 3.570; 95% CI = 2.283-5.582; P < 0.001), working an average 9-11 hours/day (AOR = 2.130; 95% CI = 1.009-4.495; P < 0.047), and self-perceived reduction in work quality (AOR = 3.139; 95% CI = 2.047-4.813; P < 0.001) were significant independent predictors of anxiety. Female gender (AOR = 2.929; 95% CI = 1.845-4.649; P < 0.001) and self-perceived reduction in work quality (AOR = 3.141; 95% CI = 2.053-4.804; P < 0.001) were significant independent predictors of depression.
An observational, multicenter cross-sectional study was conducted at eight tertiary care centers in India. The consenting participants were HCWs between 12 and 52 weeks post-discharge after COVID-19 infection. The mean age of the 679 eligible participants was 31.49 ± 9.54 years. The overall prevalence of COVID sequelae was 30.34%, with fatigue (11.5%) being the most common followed by insomnia (8.5%), difficulty in breathing during activity (6%), and pain in joints (5%). The odds of having any sequelae were significantly higher among participants who had moderate to severe COVID-19 (OR 6.51; 95% CI 3.46-12.23) and lower among males (OR 0.55; 95% CI 0.39-0.76). Besides these, other predictors for having sequelae were age (≥45 years), presence of any comorbidity (especially hypertension and asthma), category of HCW (non-doctors vs doctors), and hospitalization due to COVID-19.
Such data are scary. Not only will we have a tsunami of long-Covid patients from the general public, and not only do we currently lack effective causal treatments for the condition, but also is the number of HCWs who are supposed to deal with all this drastically reduced.
Most if not all countries are going to be affected by these issues. But the UK public might suffer the most, I fear. The reasons are obvious if you read a previous post of mine: in the UK, we have significantly fewer doctors, nurses, hospital beds, and funding (as well as politicians who care and would be able to do something about the problem) than in other comparable countries. To me, this looks like the emergence of a perfect storm.
