progress
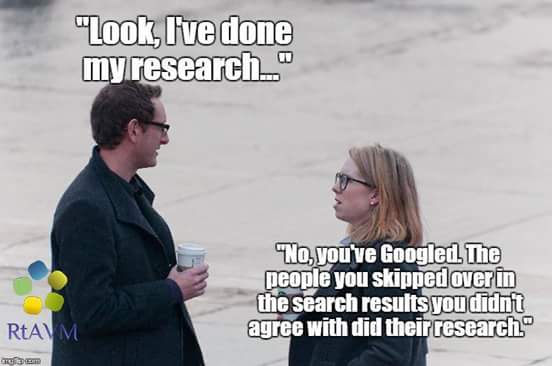
How often do we hear this sentence: “I know, because I have done my research!” I don’t doubt that most people who make this claim believe it to be true.
But is it?
What many mean by saying, “I know, because I have done my research”, is that they went on the internet and looked at a few websites. Others might have been more thorough and read books and perhaps even some original papers. But does that justify their claim, “I know, because I have done my research”?
The thing is, there is research and there is research.
The dictionary defines research as “The systematic investigation into and study of materials and sources in order to establish facts and reach new conclusions.” This definition is helpful because it mentions several issues which, I believe, are important.
Research should be:
- systematic,
- an investigation,
- establish facts,
- reach new conclusions.
To me, this indicates that none of the following can be truly called research:
- looking at a few randomly chosen papers,
- merely reading material published by others,
- uncritically adopting the views of others,
- repeating the conclusions of others.
Obviously, I am being very harsh and uncompromising here. Not many people could, according to these principles, truthfully claim to have done research in alternative medicine. Most people in this realm do not fulfil any of those criteria.
As I said, there is research and research – research that meets the above criteria, and the type of research most people mean when they claim: “I know, because I have done my research.”
Personally, I don’t mind that the term ‘research’ is used in more than one way:
- there is research meeting the criteria of the strict definition
- and there is a common usage of the word.
But what I do mind, however, is when the real research is claimed to be as relevant and reliable as the common usage of the term. This would be a classical false equivalence, akin to putting experts on a par with pseudo-experts, to believing that facts are no different from fantasy, or to assume that truth is akin to post-truth.
Sadly, in the realm of alternative medicine (and alarmingly, in other areas as well), this is exactly what has happened since quite some time. No doubt, this might be one reason why many consumers are so confused and often make wrong, sometimes dangerous therapeutic decisions. And this is why I think it is important to point out the difference between research and research.
The following announcement was made by the NHS on 7 August 2018:
The Governing Body of Bristol, North Somerset and South Gloucestershire (BNSSG) Clinical Commissioning Group (CCG) today approved changes that mean NHS funded homeopathy will only be available in exceptional circumstances in the area. The changes will mean the CCG’s Individual Funding Request (IFR) Panel would need a clinician to set out why the patient is clinically exceptional before treatment could be provided.
The decision comes after the publication of a report, which took evidence from local people, clinicians, patient groups, providers of homeopathic treatments and national guidelines.
CCG Clinical Chair Dr Jonathan Hayes said, “We are working hard to become an evidence-informed organisation because we need to make the best use of all resources to offer treatment and care to the widest range of people. The decision on homeopathy funding today is a step towards this and brings us in line with national guidelines.”
It is estimated that 41 patients receiving NHS funded homeopathic consultations in the area cost the local NHS £109,476 in the 2017/2018 financial year.
END OF QUOTE

The move is the result of 4 years of excellent work by the GOOD THINKING SOCIETY, a charity dedicate to the promotion of rational thinking.
Michael Marshall, its Project Director, said: “We are very pleased to see the Bristol CCGs take this decision to cease funding for homeopathy – every other CCG across the country has made it clear that homeopathic remedies are no better than placebo and such there is simply no place for homeopathy on the NHS.
“With the end to homeopathy funding in Bristol, the region joins NHS bodies across the rest the country in recognising that homeopathy is not a valid use of limited NHS resources. There is now no CCG in England where homeopathic pills or consultations can be routinely funded with NHS money – instead, funding can be directed towards treatments that have been shown to actually work.”
Does that not call for a knighthood for Mr Marshall?
One would have thought so!
Who will tell Prince Charles to get the ball rolling?
And while we are all waiting for the big event, you might as well donate a few £s to this truly splendid charity.
Please be generous!!!
It is no secret to regular readers of this blog that chiropractic’s effectiveness is unproven for every condition it is currently being promoted for – perhaps with two exceptions: neck pain and back pain. Here we have some encouraging data, but also lots of negative evidence. A new US study falls into the latter category; I am sure chiropractors will not like it, but it does deserve a mention.
This study evaluated the comparative effectiveness of usual care with or without chiropractic care for patients with chronic recurrent musculoskeletal back and neck pain. It was designed as a prospective cohort study using propensity score-matched controls.
Using retrospective electronic health record data, the researchers developed a propensity score model predicting likelihood of chiropractic referral. Eligible patients with back or neck pain were then contacted upon referral for chiropractic care and enrolled in a prospective study. For each referred patient, two propensity score-matched non-referred patients were contacted and enrolled. We followed the participants prospectively for 6 months. The main outcomes included pain severity, interference, and symptom bothersomeness. Secondary outcomes included expenditures for pain-related health care.
Both groups’ (N = 70 referred, 139 non-referred) pain scores improved significantly over the first 3 months, with less change between months 3 and 6. No significant between-group difference was observed. After controlling for variances in baseline costs, total costs during the 6-month post-enrollment follow-up were significantly higher on average in the non-referred versus referred group. Adjusting for differences in age, gender, and Charlson comorbidity index attenuated this finding, which was no longer statistically significant (p = .072).
The authors concluded by stating this: we found no statistically significant difference between the two groups in either patient-reported or economic outcomes. As clinical outcomes were similar, and the provision of chiropractic care did not increase costs, making chiropractic services available provided an additional viable option for patients who prefer this type of care, at no additional expense.
This comes from some of the most-renowned experts in back pain research, and it is certainly an elaborate piece of investigation. Yet, I find the conclusions unreasonable.
Essentially, the authors found that chiropractic has no clinical or economical advantage over other approaches currently used for neck and back pain. So, they say that it a ‘viable option’.
I find this odd and cannot quite follow the logic. In my view, it lacks critical thinking and an attempt to produce progress. If it is true that all treatments were similarly (in)effective – which I can well believe – we still should identify those that have the least potential for harm. That could be exercise, massage therapy or some other modality – but I don’t think it would be chiropractic care.
References
Elder C, DeBar L, Ritenbaugh C, Dickerson J, Vollmer WM, Deyo RA, Johnson ES, Haas M.
J Gen Intern Med. 2018 Jun 25. doi: 10.1007/s11606-018-4539-y. [Epub ahead of print]
PMID: 29943109
“Non-reproducible single occurrences are of no significance to science”, this quote by Karl Popper often seems to get forgotten in medicine, particularly in alternative medicine. It indicates that findings have to be reproducible to be meaningful – if not, we cannot be sure that the outcome in question was caused by the treatment we applied.
This is thus a question of cause and effect.
The statistician Sir Austin Bradford Hill proposed in 1965 a set of 9 criteria to provide evidence of a relationship between a presumed cause and an observed effect while demonstrating the connection between cigarette smoking and lung cancer. One of his criteria is consistency or reproducibility: Consistent findings observed by different persons in different places with different samples strengthens the likelihood of an effect.
By mentioning ‘different persons’, Hill seems to also establish the concept of INDEPENDENT replication.
Let me try to explain this with an example from the world of SCAM.
- A homeopath feels that childhood diarrhoea could perhaps be treated with individualised homeopathic remedies. She conducts a trial, finds a positive result and concludes that the statistically significant decrease in the duration of diarrhea in the treatment group suggests that homeopathic treatment might be useful in acute childhood diarrhea. Further study of this treatment deserves consideration.
- Unsurprisingly, this study is met with disbelieve by many experts. Some go as far as doubting its validity, and several letters to the editor appear expressing criticism. The homeopath is thus motivated to run another trial to prove her point. Its results are consistent with the finding from the previous study that individualized homeopathic treatment decreases the duration of diarrhea and number of stools in children with acute childhood diarrhea.
- We now have a replication of the original finding. Yet, for a range of reasons, sceptics are far from satisfied. The homeopath thus runs a further trial and publishes a meta-analysis of all there studies. The combined analysis shows a duration of diarrhoea of 3.3 days in the homeopathy group compared with 4.1 in the placebo group (P = 0.008). She thus concludes that the results from these studies confirm that individualized homeopathic treatment decreases the duration of acute childhood diarrhea and suggest that larger sample sizes be used in future homeopathic research to ensure adequate statistical power. Homeopathy should be considered for use as an adjunct to oral rehydration for this illness.
To most homeopaths it seems that this body of evidence from three replication is sound and solid. Consequently, they frequently cite these publications as a cast-iron proof of their assumption that individualised homeopathy is effective. Sceptics, however, are still not convinced.
Why?
The studies have been replicated alright, but what is missing is an INDEPENDENT replication.
To me this word implies two things:
- The results have to be reproduced by another research group that is unconnected to the one that conducted the three previous studies.
- That group needs to be independent from any bias that might get in the way of conducting a rigorous trial.
And why do I think this latter point is important?
Simply because I know from many years of experience that a researcher, who strongly believes in homeopathy or any other subject in question, will inadvertently introduce all sorts of biases into a study, even if its design is seemingly rigorous. In the end, these flaws will not necessarily show in the published article which means that the public will be mislead. In other words, the paper will report a false-positive finding.
It is possible, even likely, that this has happened with the three trials mentioned above. The fact is that, as far as I know, there is no independent replication of these studies.
In the light of all this, Popper’s axiom as applied to medicine should perhaps be modified: findings without independent replication are of no significance. Or, to put it even more bluntly: independent replication is an essential self-cleansing process of science by which it rids itself from errors, fraud and misunderstandings.
On this blog, we constantly discuss the shortcomings of clinical trials of (and other research into) alternative medicine. Yet, there can be no question that research into conventional medicine is often unreliable as well.
What might be the main reasons for this lamentable fact?
A recent BMJ article discussed 5 prominent reasons:
Firstly, much research fails to address questions that matter. For example, new drugs are tested against placebo rather than against usual treatments. Or the question may already have been answered, but the researchers haven’t undertaken a systematic review that would have told them the research was not needed. Or the research may use outcomes, perhaps surrogate measures, that are not useful.
Secondly, the methods of the studies may be inadequate. Many studies are too small, and more than half fail to deal adequately with bias. Studies are not replicated, and when people have tried to replicate studies they find that most do not have reproducible results.
Thirdly, research is not efficiently regulated and managed. Quality assurance systems fail to pick up the flaws in the research proposals. Or the bureaucracy involved in having research funded and approved may encourage researchers to conduct studies that are too small or too short term.
Fourthly, the research that is completed is not made fully accessible. Half of studies are never published at all, and there is a bias in what is published, meaning that treatments may seem to be more effective and safer than they actually are. Then not all outcome measures are reported, again with a bias towards those are positive.
Fifthly, published reports of research are often biased and unusable. In trials about a third of interventions are inadequately described meaning they cannot be implemented. Half of study outcomes are not reported.
END OF QUOTE
Apparently, these 5 issues are the reason why 85% of biomedical research is being wasted.
That is in CONVENTIONAL medicine, of course.
What about alternative medicine?
There is no question in my mind that the percentage figure must be even higher here. But do the same reasons apply? Let’s go through them again:
- Much research fails to address questions that matter. That is certainly true for alternative medicine – just think of the plethora of utterly useless surveys that are being published.
- The methods of the studies may be inadequate. Also true, as we have seen hundreds of time on this blog. Some of the most prevalent flaws include in my experience small sample sizes, lack of adequate controls (e.g. A+B vs B design) and misleading conclusions.
- Research is not efficiently regulated and managed. True, but probably not a specific feature of alternative medicine research.
- Research that is completed is not made fully accessible. most likely true but, due to lack of information and transparency, impossible to judge.
- Published reports of research are often biased and unusable. This is unquestionably a prominent feature of alternative medicine research.
All of this seems to indicate that the problems are very similar – similar but much more profound in the realm of alternative medicine, I’d say based on many years of experience (yes, what follows is opinion and not evidence because the latter is hardly available).
The thing is that, like almost any other job, research needs knowledge, skills, training, experience, integrity and impartiality to do it properly. It simply cannot be done well without such qualities. In alternative medicine, we do not have many individuals who have all or even most of these qualities. Instead, we have people who often are evangelic believers in alternative medicine, want to further their field by doing some research and therefore acquire a thin veneer of scientific expertise.
In my 25 years of experience in this area, I have not often seen researchers who knew that research is for testing hypotheses and not for trying to prove one’s hunches to be correct. In my own team, those who were the most enthusiastic about a particular therapy (and were thus seen as experts in its clinical application), were often the lousiest researchers who had the most difficulties coping with the scientific approach.
For me, this continues to be THE problem in alternative medicine research. The investigators – and some of them are now sufficiently skilled to bluff us to believe they are serious scientists – essentially start on the wrong foot. Because they never were properly trained and educated, they fail to appreciate how research proceeds. They hardly know how to properly establish a hypothesis, and – most crucially – they don’t know that, once that is done, you ought to conduct investigation after investigation to show that your hypothesis is incorrect. Only once all reasonable attempts to disprove it have failed, can your hypothesis be considered correct. These multiple attempts of disproving go entirely against the grain of an enthusiast who has plenty of emotional baggage and therefore cannot bring him/herself to honestly attempt to disprove his/her beloved hypothesis.
The plainly visible result of this situation is the fact that we have dozens of alternative medicine researchers who never publish a negative finding related to their pet therapy (some of them were admitted to what I call my HALL OF FAME on this blog, in case you want to verify this statement). And the lamentable consequence of all this is the fast-growing mountain of dangerously misleading (but often seemingly robust) articles about alternative treatments polluting Medline and other databases.
One of the biggest danger of SCAM, in my view, is the fact that SCAM-practitioners all too often advise their patients to forego effective conventional medicine. This probably applies to most medicines, but is best-researched for immunisations. A recent article puts it clearly:
… negative attitudes towards vaccines reflect a broader and deeper set of beliefs about health and wellbeing… this alternative worldview is influenced by ontological confusions (e.g. regarding purity, natural energy), and knowledge based on personal lived experience and trusted peers, rather than the positivist epistemological framework. [This] view is supported by recent social-psychological research, including strong correlations of vaccine scepticism with adherence to complementary and alternative medicine, magical health beliefs, and conspiracy ideation. For certain well-educated and well-resourced individuals, opposition to vaccines represents an expression of personal intuition and agency, in achieving a positive and life-affirming approach to health and wellbeing. These core beliefs are not amenable to change – and especially resistant to communications from orthodox, authoritative sources.
The authors concluded suggesting that a better long-term strategy is to combine with other disciplines in order to address the root causes of vaccine scepticism. Vaccine scepticism is unlikely to thrive in a cultural context that trusts and values the scientific consensus.
If I understand them correctly, the authors believe it is necessary to change the societal attitude to science.
I am sure they are correct.
We live in a time when anyone’s opinion is deemed as valuable as the next person’s. Pseudo-experts who have their knowledge from a couple of google searches are being considered as trustworthy as the true experts who have the background, knowledge and experience to issue responsible advice. Science is viewed by many as just another way of knowing, or even as the new cult or religion that must be viewed with suspicion.
It is clear that these are deplorable developments. But how to stop them?
This is where it gets complex.
One is tempted to lay the blame at the door of our politicians. Why do we tolerate the fact that so many of them have not the slightest inkling about science?
But hold on, WE elected them!
Why?
Because large sections of the public are ignorant too.
So, one must start much earlier. We need better science education, and that has to begin in the first year of schooling! We need evening classes in critical thinking. We need adult science courses for politicians.
But this is not going to happen, because our politicians fail to see the importance of such measures (and, of course, they might feel that an uneducated public is easier to govern than an educated one).
How to break this vicious circle?
It is clear from these simple (and simplistic) reflections that a multifactorial approach is required. And it is clear that it ought to be a strategy that prevents standards in the most general terms from slipping ever lower. But how?
I wish I knew!!!
One of the aims in running this blog has always been to stimulate critical thinking (not just in my readers but also in myself).
Critical thinking means making decisions and judgements based on (often confusing) evidence. According to the ‘National Council for Excellence in Critical Thinking’ it is the intellectually disciplined process of actively and skilfully conceptualizing, applying, analysing, synthesizing, and/or evaluating information gathered from, or generated by, observation, experience, reflection, reasoning, or communication, as a guide to belief and action.
Carl Sagan explained it best: “It seems to me what is called for is an exquisite balance between two conflicting needs: the most skeptical scrutiny of all hypotheses that are served up to us and at the same time a great openness to new ideas. Obviously those two modes of thought are in some tension. But if you are able to exercise only one of these modes, whichever one it is, you’re in deep trouble. If you are only skeptical, then no new ideas make it through to you. You never learn anything new. You become a crotchety old person convinced that nonsense is ruling the world. (There is, of course, much data to support you.) But every now and then, maybe once in a hundred cases, a new idea turns out to be on the mark, valid and wonderful. If you are too much in the habit of being skeptical about everything, you are going to miss or resent it, and either way you will be standing in the way of understanding and progress. On the other hand, if you are open to the point of gullibility and have not an ounce of skeptical sense in you, then you cannot distinguish the useful as from the worthless ones.”
 Critical thinking is not something one is born with; but I strongly believe that most people can be taught this skill. This study suggests that I may be right. The researchers measured the relationship between student’s religion, gender, and propensity for fantasy thinking with the change in belief for paranormal and pseudoscientific subjects following a science and critical thinking course. Student pre-course endorsement of religious, paranormal, and pseudo-scientific beliefs ranged from 21 to 53%, with religion having the highest endorsement rate. Pre-course belief in paranormal and pseudo-scientific subjects was correlated with high scores in some fantasy thinking scales and showed a gender and a religion effect with females having an 11.1% higher belief across all paranormal and pseudo-science subcategories. Students’ religion, and frequency of religious service attendance, was also important with agnostic or atheist students having lower beliefs in paranormal and pseudo-science subjects compared to religious students. Students with either low religious service attendance or very high attendance had lower paranormal and pseudoscientific beliefs.
Critical thinking is not something one is born with; but I strongly believe that most people can be taught this skill. This study suggests that I may be right. The researchers measured the relationship between student’s religion, gender, and propensity for fantasy thinking with the change in belief for paranormal and pseudoscientific subjects following a science and critical thinking course. Student pre-course endorsement of religious, paranormal, and pseudo-scientific beliefs ranged from 21 to 53%, with religion having the highest endorsement rate. Pre-course belief in paranormal and pseudo-scientific subjects was correlated with high scores in some fantasy thinking scales and showed a gender and a religion effect with females having an 11.1% higher belief across all paranormal and pseudo-science subcategories. Students’ religion, and frequency of religious service attendance, was also important with agnostic or atheist students having lower beliefs in paranormal and pseudo-science subjects compared to religious students. Students with either low religious service attendance or very high attendance had lower paranormal and pseudoscientific beliefs.
Following the critical thinking course, overall beliefs in paranormal and pseudo-scientific subcategories lowered 6.8–28.9%, except for superstition, which did not significantly change. Change in belief had both a gender and religion effect with greater reductions among religious students and females.
The link between religion and alternative medicine is relatively well-established. A 2014 study, for instance, showed an association between alternative medicine use and religiosity. The finding that females have an 11.1% higher belief in the paranormal and pseudo-science is new to me, but it would tie in with the well-documented fact that women use alternative medicine more frequently than men.
The most important finding, however, is clearly that critical thinking can be taught.
That must be good news! As discussed previously, critical thinkers experience fewer bad things in life than those of us who do not have acquired that skill. This cannot come as a surprise – being able to tell useful concepts from worthless ones should achieve exactly that.
An article has just been published announcing the reform of the German Heilpraktiker, the profession of alternative practitioners that has been discussed repeatedly on this blog and criticised recently by the ‘Muensteraner Kreis’. As the new article is in German, I will try to summarise the essence of it here:
The health ministers of all German counties have decided yesterday that they will start reforming the profession of the Heilpraktiker that has attracted much criticism in recent months. The current laws are no longer fit for purpose. There is neither a mandatory agreement for the education of the Heilpraktiker, nor a uniform regulation of the profession.
The senator for health from Hamburg stated: “We feel that the Heilpraktiker should not be allowed to do certain thing, but be permitted to do plenty of activities that remain legal.” At present, the Heilpraktiker is allowed to treat fractures, malignancies, give injections, and even manufacture certain medicines. “We believe there is a need for regulation to protect patients.”
Now a working group will be formed to investigate and produce a report within a year. Remarkably, the German health secretary avoided commenting. In a statement, it was said that patients must be empowered to make decisions on the basis of quality-assured information.
The full German text is below.
__________________________________________________________________________________
Nach mehreren deutschlandweit Aufsehen erregenden Todesfällen beispielsweise von Krebspatienten, die kurz nach der Therapie durch einen Heilpraktiker in Brüggen-Bracht starben, will die Politik sich nun diesen Berufszweig vornehmen. Die Gesundheitsminister aller Bundesländer haben am Donnerstag beschlossen, eine Reform anzugehen. „Das unzureichend regulierte Heilpraktikerwesen mit seiner umfassenden Heilkundebefugnis steht unverändert in der Kritik“, heißt es in einer Erklärung. Das Heilpraktikergesetz könne dem heutigen Anspruch an den Gesundheitsschutz der Patienten nicht mehr gerecht werden. Für Heilpraktiker gebe es weder verbindliche Regeln zur Ausbildung noch eine einheitliche Berufsordnung. Andere Gesundheitsberufe müssten hingegen strenge Qualifikationskriterien erfüllen.
„Wir sehen es als kritisch an, dass einige Tätigkeiten zwar den Heilpraktikern untersagt sind, aber es noch eine Fülle von Tätigkeiten gibt, die zugelassen sind“, sagte die Hamburger Senatorin für Gesundheit, Cornelia Prüfer-Storcks, auf einer Pressekonferenz – sie hatte die Initiative maßgeblich vorangetrieben. So dürfen Heilpraktiker Knochenbrüche therapieren, schwere und bösartige Erkrankungen behandeln und Injektionen geben. Selbst die Herstellung von Arzneimitteln für bestimmte Patienten sei Heilpraktikern erlaubt. „Ohne die Prüfmechanismen, die wir normalerweise haben, wenn wir Arzneimittel zulassen und produzieren“, kritisierte Prüfer-Storcks. „Wir glauben, dass es hier Regelungsbedarf gibt aus Sicht des Patientenschutzes.“
„Die Ministerinnen und Minister, Senatorinnen und Senatoren für Gesundheit sehen eine zwingende Reformbedürftigkeit des Heilpraktikerwesens“, heißt es in dem kurzen, MedWatch vorliegenden Beschluss. „Der Bund wird gebeten, eine Bund-Länder-Arbeitsgruppe einzurichten, die eine grundlegende Reform des Heilpraktikerwesens prüft.“ Das Ergebnis der Prüfung solle bis zur Gesundheitsministerkonferenz in einem Jahr vorgelegt werden.
Bundesgesundheitsminister Jens Spahn erklärte auf der Pressekonferenz das Patientenwohl zwar zum entscheidenden Maßstab für die Gesundheitspolitik. „Deshalb finde ich es richtig, dass die Gesundheitsministerkonferenz bei der Patientenorientierung ihren Schwerpunkt setzt“, sagte er. Auf mögliche Reformen des Heilpraktikerberufes ging der Minister bei der Pressekonferenz jedoch nicht ein. Inwiefern sein Haus die von den Landesministern geforderte Reform des Heilpraktikerwesens mit unterstützen wird, bleibt offen. Auf Nachfrage, ob das Ministerium eine Bund-Länder-Arbeitsgruppe unterstützen würde, versteckte sich eine Sprecherin bereits im Mai hinter der Mini-Reform von Gröhe. Mit Blick auf die kurze Zeit seit Inkrafttreten dieser Änderungen sei es angemessen, zunächst zu prüfen, ob und inwieweit diese zum Schutz des Patientenwohles beiträgt, erklärte sie – „ehe weitere gesetzliche Maßnahmen in Betracht gezogen werden sollten“.
In einem Grundsatzbeschluss sprach sich die Gesundheitsministerkonferenz außerdem für „Patientenorientierung als Element einer zukunftsweisenden Gesundheitspolitik“ aus. „Das heißt, dass der Patient natürlich das Heft in der Hand haben muss, dass er versteht, was mit ihm gemacht wird, warum es mit ihm gemacht wird, mit welchen Chancen die Behandlung verbunden ist“, sagte NRW-Gesundheitsminister Karl Laumann. Auch in der Ausbildung des Gesundheitspersonals sollten diese Aspekte einen großen Stellenwert bekommen, betonte Laumann – und erwähnte zwar Ärzte als Berufsgruppe explizit, nicht aber Heilpraktiker. Der frühere Bundespatientenbeauftragte forderte außerdem mehr Transparenz ein. In Teilen des Gesundheitssystems gebe es wegen mangelnder Transparenz „eine gewisse Misstrauenskultur“, sagte er.
Die Minister wollen laut dem Beschluss die Patientensouveränität und der Orientierung im Gesundheitswesen verbessern, die Gesundheitskompetenz und gesundheitliche Eigenverantwortung beispielsweise durch die Einrichtung eines nationalen Gesundheitsportals deutlich stärken und Kommunikation und Wissenstransfer zwischen Patienten und allen Beteiligten im Gesundheitswesen fördern. „Patienten sollen so in die Lage versetzt werden, ihre Interessen besser zu vertreten und ihre Entscheidungen auf der Basis qualitätsgesicherter Informationen zu treffen“, heißt es.
Kommunikationskompetenz und wertschätzende Beziehungsgestaltung sei im Gesundheitswesen von wesentlicher Bedeutung für die Partizipation, Qualität, Sicherheit und den Erfolg der gesundheitlichen Prävention und der medizinischen Behandlung, betonen die Minister. Allgemeinverständliche „Patientenbriefe“ sollen als erster Schritt die Informiertheit von Patienten nach Krankenhausbehandlungen erhöhen. Außerdem soll das Bundesgesundheitsminister eine Pflicht schaffen, dass niedergelassene Ärzte ihren Patienten neutrale und evidenzbasierte schriftliche Informationen zu Zusatzangeboten – sogenannten „Individuellen Gesundheitsleistungen“ – zur Verfügung stellen müssen.
Bei Behandlungsfehlern sollen nach Ansicht der Landesminister auf Bundesebene weitere Erleichterungen umgesetzt werden: Die Beweislast und das Beweismaß soll zu Gunsten von Patienten überarbeitet werden. Außerdem sollten Krankenkassen gesetzlich verpflichtet werden, Patienten beim Nachweis eines Behandlungsfehlers besser zu unterstützen.
______________________________________________________________________________
I have been banging on about the German Heilpraktiker, its infamous history and its utter inadequacy since many years. This is what I published in 1996, for instance:
Complementary medicine is increasing in popularity. In most countries its practice is in the hands of non-medically trained practitioners, professions which are often not properly regulated. When discussing solutions to this problem the German “Heilpraktiker” is often mentioned. The history and present situation of this profession are briefly outlined. The reasons why the “Heilpraktiker concept” is not an optimal solution are discussed. It is concluded that the best way forward consists of regulation and filling the considerable gaps in knowledge relating to complementary medicine.
It goes without saying that, after so many tears of warning about the risks involved in allowing poorly trained practitioners, who are all too often unable to see the limits of their competency (and after many unnecessary fatalities), I am delighted that progress seems finally to be on the horizon.
This is a somewhat unusual post.
I do not normally dwell on personal anecdotes or experiences – but this one might be relevant, and it is absolutely true.
About 7 or 8 years ago (we had just published our book Trick or Treatment), I was invited to a meeting of health insurers. Not just any old meeting, but a top-notch conference where many of the world’s most influential executives of large insurance companies were gathered. It took place in one of the most luxurious hotels of Istanbul. The most prominent speaker was the brother of France’s president Sarkozy (who flew in by helicopter and came with two body-guards). He began his lecture by stating “You of course all know me because I have a famous sister in law.”
I did not have such a witty opening phrase for my talk. My task was to review the evidence for and against the major alternative therapies (at the time, I did such lectures regularly). My audience of about 300 people listened politely to what I had to say and, during, question time, they made some relevant comments. Altogether, it was a good and well-received lecture.
But the interesting bit came later.
Over coffee, I was surrounded by people who came to me and said something like this: “We know the evidence, of course, and we know how flimsy it is, particularly for homeopathy. But we still pay for it, because the competition does it too. We cannot be seen to offer less than they do. This is purely a commercial decision about being seen to be competitive.”
Such honesty came as a surprise to me. I had expected that they were well-informed about the evidence; after all, they were in charge of huge companies selling health insurances. Not knowing about the evidence would have been negligent. But I had not expected they would volunteer their motives quite so openly. I got the impression that they were trying to justify their nonsensical actions without seeming irrational. In a way, they seemed to say: ‘Such treatments might not work for the patient, but they do work for us’.
I remember suggesting to some of these executives that they could even be more competitive, progressive and ethical by telling their customers that they took better care of their money that the competition by NOT paying for ineffective treatments. Such remarks resulted in blank faces or vague smiles. I felt my audience had not really understood the opportunity. Being honest, transparent and evidence-based was evidently not understood as a viable marketing tool.
As I said, this was almost a decade ago
… lots has happened since.
I wonder whether the message might be more attractive today.
An announcement by the UK Society of Homeopaths caught my attention. Here it is in its full and unabbreviated beauty:
START OF ANNOUNCEMENT
Homeopaths are being urged to contribute to an inquiry exploring ways to tackle a looming public health crisis threatened by ‘superbugs’ – bacteria resistant to antibiotics and other antimicrobial drugs.
The Commons Select Committee on Health and Social Care is inviting evidence for its investigation into the progress made by the government so far in responding to the challenge.
The two angles it is exploring are:
- What results have been delivered by the current UK strategy on antimicrobial resistance (AMR), launched in 2013?
- Key actions and priorities for the government’s next AMR strategy, due to be published at the end of 2018.
The Society of Homeopaths is putting together a submission and is asking members to submit their own evidence to the inquiry of using homeopathic alternatives to antimicrobials.
According to the inquiry background papers, antimicrobial resistance – in which bacteria have evolved into ‘superbugs’, resistant to drugs devised to kill them – is a “significant and increasing threat” to public health in the UK and globally. EU data indicates that it is responsible for 700,000 deaths a year worldwide and at least 50,000 in the US and Europe.
The death toll could reach 10m people a year by 2050 if the rise in resistance is not headed off, it is estimated.
Society Chief Executive Mark Taylor said: “Our members know a great deal about the alternatives to antibiotics through their own practice and knowledge. This is a timely inquiry from the Health and Social Care Committee to assess the success of the existing strategy and an opportunity to make the case again for fresh thinking on this pressing public health challenge.”
END OF ANNOUNCEMENT
Yes, of course!
We have a crisis of antibiotic resistance.
Who is going to offer the solution?
THE HOMEOPATHS!!!
How?
They are going to treat us all with homeopathic remedies when the superbugs strike.
And the result?
No more crisis.
How come?
Because they have turned it into a catastrophe!!!