politics
Sorry, but (exceptionally) this post is not about so-called alternative medicine (SCAM).
During the last weekend, I had the displeasure watching video clips of Donald Trump being unable to lift a glass of water one-handedly and being unable to walk normally down a ramp. Many observers agree that his health has been in steady decline ever since he was taken to the hospital late last year. Now Trump seems to have deteriorated to the point where he sounds and acts like a zombie, loses his temper, acts irrationally, etc. To me, there is no question: this man is seriously ill, physically and mentally.
Why is that any of my business?
The answer is simple: because he is rapidly destroying not just the US but, with it, much of the world as I know it. Therefore, I feel that Trump’s health should be all our business.
So, what disease might he be suffering from?
There is very little to go by for answering this question. His medical check-ups have apparently attested him perfect health, but they seem as trustworthy as a 4 £ note. Even when he was rushed to hospital, we learnt nothing about his condition. This means, we merely have little more than what we see of his behaviour to suggest a diagnosis which inevitably must remain guesswork.
Watching Trump, I often asked myself: could he be suffering from neurosyphilis? It would certainly fit in with his past life-style.
Neurosyphilis is a syphilis infection of the spinal cord or brain of people who had syphilis that has not been adequately treated. It can occur many years after they had their first infection. The physical symptoms are highly variable and can include:
- Having abnormal gait
- Loss of balance
- Not being able to walk normally
- Visual disturbances
- Headaches
- Incontinence
- Numbness in legs, toes, or feet
- Seizures
- Tremors
- Stiff neck
- Muscular weakness
- Abdominal pain
Most of these have been displayed by Trump. In addition, there are mental symptoms that are also highly variable and can include:
- Irritability
- Loss of ability to concentrate
- Delusional thinking
- Grandiosity
- Problems with memory
- Lack of insight
- Impaired judgment
- Emotional instability
Patchy hair loss can also be a sign of the later stages of syphilis, and is something that I find hard to miss when observing Trump.


I know that neurosyphilis is highly speculative as a diagnosis of Trump’s condition. What is not speculative, however, is that he is gravely ill. As such, he should not be in the Oval Office making decisions that affect us all.
Whatever disease Trump has, he is a serious danger to mankind.
Yesterday, it was announced that UK universities are not doing well according to international league tables. Of the UK’s 84 ranked universities, 66 saw their staff to student ratio decline while 59 had a drop in research citations. International student numbers at 51 universities also fell.
No reason to despair; help is on the way!
The University of Exeter reported that “as International Education Champion, Sir Steve will have a leading role in a 10-year strategy to both increase the number of international students choosing to study in the UK higher education system to 600,000 and increase the value of education exports to £35 billion per year by 2030. The University of Exeter is delighted and proud with this appointment…
The role of International Education Champion will be to work with organisations across the breadth of the education sector, including universities, schools, the EdTech industry, vocational training, and early years schooling providers. Steve will also help target priority regions worldwide to build networks and promote the UK as the international education partner of choice. The role will additionally help to boost the numbers of international students in the UK.
The appointment of Sir Steve Smith fulfils a priority action from the International Education Strategy, published by the Department for Education and the Department for International Trade. Sir Steve will spearhead overseas activity and address a number of market access barriers on behalf of the whole education sector, including concerns over the global recognition of UK degrees and other qualifications. Sir Steve’s experience, knowledge and global connections will help to develop long-term relationships with international governments and overseas stakeholders…”
Shortly after becoming VC at Exeter, Prof Smith closed two Departments: Music and Chemistry. Apparently, they were not bringing in enough cash. Several years later, he had a key role in closing my unit. It had attracted a complaint from Prince Charles’ 1st private secretary (full story here, in case you are interested).
I hope Sir Steve is more productive in boosting international education. One thing seems certain to me: post-Brexit/post-COVID academia in the UK will need a boost after what our current government has done to it.
By guest blogger Loretta Marron
Although assumed to be traditional, what we know today as ‘Traditional Chinese Medicine’ (TCM) was invented in the 1950s for political reasons by then Chairman Mao. It has since been proclaimed by Xi Jinping, now life-President of the People’s Republic of China, as the “jewel” in the millennia of Chinese civilization.
In May this year, Xi “announced plans to criminalise criticism of traditional Chinese medicine”. Speaking out against TCM could land you years in prison, prosecuted for “picking fights to disturb public order” and “defaming” the practice.
With the industry expected to earn $420 billion by the end of 2020, covid-19 has provided Xi with a platform to promote unproven, potentially harmful TCM. To keep these profits filling Chinese coffers, the World Health Organization (WHO) remains silent and those challenging TCM are silenced.
In January, the late Dr Li Wenliang was arrested and gaoled for warning China about covid-19. Li was one of up to nine people who were disciplined for spreading rumours about it. As the virus silently spread around the world, Beijing told the WHO that there was ‘no clear evidence’ of spread between humans.
As their death toll passed 1,000, Beijing’s response was to remove senior officials and to sack hundreds over their handling of the outbreak. With the support of the WHO, claims continue to be made that TCM “has been proved effective in improving the cure rate”, denying the simple fact that “patients would have recovered even if they hadn’t taken the Chinese medicine”.
With cases now heading for 8 million, and over four hundred thousand people confirmed dead world-wide and with economies in free-fall, Beijing continues, “to protect its interests and people overseas; to gain leadership of international governance”,for financial gain, to aggressively use its national power. Under the guise of ‘International Aid’, during the pandemic, Beijing promoted treatments based on unproven traditional medicine, sending TCM practitioners to countries including Italy, France and Iran.
Countries challenging Beijing can expect claims of racism and financial retaliation.
Back in 2016, the Chinese State Council released a “Strategic Development Plan for Chinese Medicine (2016-2030)”, seeking to spread ‘knowledge’ into campuses, homes and abroad.
In July 2017, a law promising equal status for TCM and western medicine came into effect. Provisions included encouragement to China’s hospitals to set up TCM centres. “The new law on traditional Chinese medicine will improve global TCM influence, and give a boost to China’s soft power”.
In 2019, after strong lobbying by the Chinese Communist Party (CCP), WHO added a chapter on TCM to their official International Classification of Diseases (ICD-11). In China, doctors are now instructed to prescribe traditional medicine to most patients.
While Chinese herbs might have exotic names, they are, once translated, often the same as western herbs, many of which might have significant interactions. WHO fails to acknowledge any drug interactions.
In 1967, Mao launched Project 523 to find a cure for chloroquine-resistant malaria. Over 240,000 compounds had already been tested and none had worked. Trained in pharmacology and modern western methods, Tu Youyou used the scientific method to test sweet wormwood, a herb traditionally used in China for fever, where she developed a useful artemisinin derivative for resistant malaria. The drug has saved millions of lives. In 2015 she won the Nobel Prize for her work. However, Tu’s work is not a blanket endorsement of TCM: without the years of research, she would not have been successful.
TCM is commercially driven. Criticism of remedies is often blocked on the Internet in China, and critics have been jailed. The majority of TCM’s are not tested for efficacy in randomized clinical trials. Clinical trials are usually of poor quality and serious side effects are underreported. China has even rolled back regulations as Beijing forcefully promotes TCM’s as an alternative to proven western medicine. An increasing number of prestigious research hospitals now prescribe and dispense herbs that may cause drug interactions alongside western medicine for major illness patients.
TCM’s are not safe. Most systematic reviews suggest that there is no good or consistent evidence for effectiveness, negative results aren’t published, research data are fabricated and TCM-exports are of dubious quality.
If the benefits of herbal remedies are to be realised, good clinical studies must be encouraged.
TCM is not medicine. It’s little more than a philosophy or a set of traditional beliefs, about various concoctions and interventions and their alleged effect on health and diseases.
To stop misleading the world with what Mao himself saw as nonsense, and to mitigate future pandemics, WHO can and should remove all mention of TCM other than to state that it is unproven and could be dangerous.
Homeopathy has had its fair share of declarations, and now there is another one. I find this new one important because it is from German medical students and might thus indicate where German homeopathy is heading.
The ‘Bundesvertretung der Medizinstudenten in Deutschland’ – the German Medical Students’ Association – has recently looked into the evidence for and against homeopathy and came up with this poignant declaration:

Here is my translation for those who cannot read German; I have added a few footnotes to explain the German context:
- Homeopathy does not work beyond placebo [1].
- The legal health insurances should not reimburse homeopathy [2].
- The law stating that homeopathy can only be sold in pharmacies should be abolished [3].
- Medicines should only be licenced, if there is a valid proof of efficacy [4].
- In public debates, it must be made clear that homeopathy is not part of naturopathy [5].
- The medical degree in homeopathy must be scrapped [6].
- The teaching of homeopathy must be evidence-based and context-related [7].
_______________________________
- This seems to refer to the wording a German manufacturer of homeopathic preparations tried to suppress.
- At the moment most German health insurances do pay for homeopathy.
- In Germany, pharmacies have a monopoly on homeopathic remedies.
- Since many years, there has been a special regulation in Germany whereby homeopathics could get a licence without proof of efficacy.
- German homeopaths tend to be keen on muddying the water by claiming homeopathy is part of naturopathy.
- All German students are being taught (and examined on) some rudimentary knowledge of homeopathy.
The new declaration is ‘spot on’. I congratulate the students for their courage and wisdom to publish it. They are the future of German medicine, a future where homeopathy’s place is exclusively in the history books as a bizarre episode of anti-science.
Someone alerted me to a short article (2008) of mine that I had forgotten about. In it, I mention the 32 Cochrane reviews of acupuncture available at the time and the fact that they showed very little in favour of acupuncture. This made me wonder to what extent the situation might have changed in the last 12 years. So, I made a renewed attempt at evaluating this evidence. The entire exercise comes in three parts:
- My original paper from 2008
- The current evidence from Cochrane reviews
- Comments on the new evidence
PART 1
Acupuncture has a long history of ups and downs. Its latest renaissance started in 1971, when a journalist in President Nixon’s press corps experienced symptomatic relief after being treated for postoperative abdominal distension. He reported this experience in The New York Times, which triggered a flurry of interest and research. In turn, it was discovered that needling might release endorphins in the brain or act via the gate control mechanism. Thus, plausible modes of action seemed to have been found, and the credibility of acupuncture increased significantly. Numerous clinical trials were initiated, and their results often suggested that acupuncture is clinically effective for a surprisingly wide range of conditions. Both a World Health Organization report and a National Institutes of Health consensus conference provided long lists of indications for which acupuncture allegedly was of proven benefit.
Many of the clinical studies, however, lacked scientific rigor. Most experts therefore remained unconvinced about the true value of acupuncture, particularly as a treatment for all ills. Some investigators began to suspect that the results were largely due to patient expectation. Others showed that the Chinese literature, a rich source of acupuncture trials, does not contain a single negative study of acupuncture, thus questioning the reliability of this body of evidence.
A major methodological challenge was the adequate control for placebo effects in clinical trials of acupuncture. Shallow needling or needling at non-acupuncture points had been used extensively for this purpose. Whenever the results of such trials did not show what acupuncture enthusiasts had hoped, they tended to claim that these types of placebos also generated significant therapeutic effects. Therefore, a negative result still would be consistent with acupuncture being effective. The development of non-penetrating needles was aimed at avoiding such problems. These “stage dagger”-like devices are physiologically inert and patients cannot tell them from real acupuncture. Thus, they fulfil the criteria for a reasonably good placebo.
The seemingly difficult question of whether acupuncture works had become complex—what type of acupuncture, for what condition, compared with no treatment, standard therapy, or to placebo, and what type of placebo? Meanwhile, hundreds of controlled clinical trials had become available, and their results were far from uniform. In this situation, systematic reviews might be helpful in establishing the truth, particularly Cochrane reviews, which tend to be more rigorous, transparent, independent, and up-to-date than other reviews. The traditional Chinese concept of acupuncture as a panacea is reflected in the fact that 32 Cochrane reviews are currently (January 2008) available, and a further 35 protocols have been registered. The notion of acupuncture as a “heal all” is not supported by the conclusions of these articles. After discarding reviews that are based on only 3 or fewer primary studies, only 2 evidence-based indications emerge: nausea/vomiting and headache. Even this evidence has to be interpreted with caution; recent trials using the above-mentioned “stage-dagger” devices as placebos suggest that acupuncture has no specific effects in either of these conditions.
Further support for the hypothesis that acupuncture is largely devoid of specific therapeutic effects comes from a series of 8 large randomized controlled trials (RCTs) initiated by German health insurers (Figure). These studies had a similar, 3-parallel-group design: pain patients were randomized to receive either real acupuncture, shallow needling as a placebo control, or no acupuncture. Even though not entirely uniform, the results of these studies tend to demonstrate no or only small differences in terms of analgesic effects between real and placebo acupuncture. Yet, considerable differences were observed between the groups receiving either type of acupuncture and the group that had no acupuncture at all.
The most recent, as-yet-unpublished trial also seems to confirm the “placebo hypothesis.” This National Institutes of Health-sponsored RCT included 640 patients with chronic back pain. They received either individualized acupuncture according to the principles of traditional Chinese medicine, or a standardized form of acupuncture, or sham acupuncture. The results demonstrate that acupuncture added to usual care was superior to usual care alone, individualized acupuncture was not more effective than standardized acupuncture, and neither type of real acupuncture was more effective than sham acupuncture.

Figure
Schematic representation of the recent acupuncture trials all following a similar 3-group design. These 8 randomized controlled trials related to chronic back pain, migraine, tension headache, and knee osteoarthritis (2 trials for each indication). Their total sample size was in excess of 5000. Patients in the “no acupuncture” group received either standard care or were put on a waiting list. Sham acupuncture consisted of shallow needling at non-acupuncture points. Real acupuncture was semi-standardized. The differences between the effects of both types of acupuncture and no acupuncture were highly significant in each study. The differences between sham and real acupuncture were, with the exception of osteoarthritis, not statistically significant.
Enthusiasts employ such findings to argue that, in a pragmatic sense, acupuncture is demonstrably useful: it is clearly better than no acupuncture at all. Even if it were merely a placebo, what really matters is to alleviate pain of suffering patients, never mind the mechanism of action. Others are not so sure and point out that all well-administrated treatments, even those that generate effects beyond placebo, will induce a placebo response. A treatment that generates only non-specific effects (for conditions that are amenable to specific treatments) cannot be categorized as truly effective or useful, they insist.
So, after 3 decades of intensive research, is the end of acupuncture nigh? Given its many supporters, acupuncture is bound to survive the current wave of negative evidence, as it has survived previous threats. What has changed, however, is that, for the first time in its long history, acupuncture has been submitted to rigorous science—and conclusively failed the test.
[references in the original paper]
Part 2 will be posted tomorrow.
The Foundation for Integrated Health (FIH) does no longer exist. But it is historically important, in my view. So, I decided to do some research in order to document its perplexing history. In the course of this activity, I found that someone had beaten me to it. This article that does the job very well; I therefore take the liberty of copying it here and adding a few points at the end:
The Foundation for Integrated Health (FIH) was a controversial charity run by Charles, Prince of Wales, founded in 1993. The Foundation promoted complementary and alternative medicine, preferring to use the term “integrated health”, and lobbied for its inclusion in the National Health Service. The charity closed in 2010 after allegations of fraud and money laundering led to the arrest of a former official.
History
Prince Charles established the charity in 1993 to explore “how safe, proven complementary therapies can work in conjunction with mainstream medicine”. [1]
Dr Michael Dixon was appointed the Foundation’s medical director. From 2005 to 2007, FIH received a grant from the Department of Health to help organise the self-regulation of complementary therapies. There had been concern that with a large proportion of the public turning to complementary approaches, there were few safeguards in place to ensure that non-statutorily regulated therapists were safe, trained and would act in an appropriate way. FIH worked to bring together the representative bodies of many complementary professions to talk and agree standards. [2] The result was the formation of the Complementary and Natural Healthcare Council (CNHC) which had hoped to register 10,000 practitioners of complementary medicine by the end of 2009 but which by September 2009 had succeeded in enrolling less than a tenth of that number due to lack of interest on the part of some of their professional associations. The Department of Health is currently continuing to fund the CNHC but future funding will be dependent on substantial progress being made towards the target (which has now been reduced to 2,000). Alternative medicine campaigners argued that the move toward regulation conferred undue respectability on unproven and possibly unsafe complementary & alternative medicine (CAM) approaches.
FIH also worked with medical schools to increase the understanding of complementary approaches amongst new doctors and ran an annual awards ceremony for integrated health schemes both within the medical world and in the community.
The papers of the Foundation for Integrated Health are held at the Wellcome Library, Archives and Manuscripts, and are available for consultation by appointment. Further details about the collection can be found on the Wellcome online catalogue. [3]
Controversy
The Prince of Wales has demonstrated an interest in alternative medicine, the promotion of which has occasionally resulted in controversy. [4] In 2004, the Foundation divided the scientific and medical community over its campaign encouraging general practitioners to offer herbal and other alternative treatments to National Health Service patients, [5] [6] and in May 2006, The Prince made a speech to an audience of health ministers from various countries at the World Health Assembly in Geneva, urging them to develop a plan for integrating conventional and alternative medicine. [7]
In April 2008, The Times published a letter from Professor Edzard Ernst that asked the Prince’s Foundation to recall two guides promoting “alternative medicine”, saying: “the majority of alternative therapies appear to be clinically ineffective, and many are downright dangerous.” A speaker for the foundation countered the criticism by stating: “We entirely reject the accusation that our online publication Complementary Healthcare: A Guide contains any misleading or inaccurate claims about the benefits of complementary therapies. On the contrary, it treats people as adults and takes a responsible approach by encouraging people to look at reliable sources of information… so that they can make informed decisions. The foundation does not promote complementary therapies.” [8] Ernst has recently published a book with science writer Simon Singh condemning alternative medicine called Trick or Treatment: Alternative Medicine on Trial . The book is ironically dedicated to “HRH the Prince of Wales” and the last chapter is very critical of his advocacy of “complementary” and “alternative” treatments. [9]
The Prince’s Duchy Originals have produced a variety of CAM products including a “Detox Tincture” that Ernst has denounced as “financially exploiting the vulnerable” and “outright quackery“. [10] In May 2009, the Advertising Standards Authority criticised an email that Duchy Originals had sent out to advertise its Echina-Relief, Hyperi-Lift and Detox Tinctures products saying it was misleading. [11]
In Ernst’s book More Good Than Harm? The Moral Maze of Complementary and Alternative Medicine he and ethicist Kevin Smith call Charles “foolish and immoral” and “conclude that it is not possible to practice alternative medicine ethically”. Ernst further claims that the private secretary of the Prince contacted the vice chancellor of Exeter University to investigate Ernst’s complaints against the “Smallwood Report” which the Prince had commissioned in 2005. While Ernst was “found not to be guilty of any wrong-doing, all local support at Exeter stopped, which eventually led to my early retirement.” [12]
Lobbying allegations
The Prince personally wrote at least seven letters [15] to the Medicines and Healthcare products Regulatory Agency (MHRA) shortly before they relaxed the rules governing labelling of herbal products such as the ones sold by his duchy, a move that has been widely condemned by scientists and medical bodies. [16]
On 31 October 2009 it was reported that Prince Charles had personally lobbied Health Secretary Andy Burnham regarding greater provision of alternative treatments on the NHS. [10]
Charity Commission complaint
Fraud allegations and closure
In 2010, following accounting irregularities noted by the foundation’s auditor, it was reported that the Metropolitan Police Economic and Specialist Crime Command had begun an inquiry into alleged fraud. [18] Within weeks, two former officials at the Prince’s Foundation were arrested for fraud believed to total £300,000. [1] [19] Four days later, on 30 April 2010, the foundation announced [20] that it would close. The foundation stated that its closure was the result of the fraud allegations. [21]
The charity’s finance director, accountant George Gray, was convicted of theft totalling £253,000 and sentenced to three years in prison. [22] [23]
Rebranding as “The College of Medicine”
Following the disbanding of the Prince’s Foundation, many of the individuals and organisations involved launched a new organisation in late 2010 called The College of Medicine, with which the Prince of Wales was not overtly involved. Several commentators writing in The Guardian and The British Medical Journal, have expressed the opinion that the new organisation is simply a re-branding of the Prince’s Foundation, [22] [24] [25] [26] [27] describing it as “Hamlet without the Prince”. [28]
In support of this connection with Prince Charles, alternative medicine critic and pharmacologist David Colquhoun has argued that the College (originally called “The College of Integrated Health”) is extremely well-funded [29] and seemed from the beginning to be very confident of the Prince’s support; explicitly describing its mission as “to take forward the vision of HRH the Prince of Wales”. [30]
These claims have been contested by the College. [31]
- 1 2 Robert Booth (26 April 2010). “Prince Charles’s aide at homeopathy charity arrested on suspicion of fraud”. London: guardian.co.uk.
- ↑ Regulating complementary therapies – Prince’s Foundation for Integrated Health
- ↑ “Wellcome Library Western Manuscripts and Archives catalogue”. Archives.wellcomelibrary.org. Retrieved 2015-09-07.
- ↑ Barnaby J. Feder, Special To The New York Times (9 January 1985). “More Britons Trying Holistic Medicine — New York Times”. Query.nytimes.com. Retrieved 2008-10-12.
- ↑ Carr-Brown, Jonathon (14 August 2005). “Prince Charles’ alternative GP campaign stirs anger”. The Times. London. Retrieved 11 March 2009.
- ↑ Revill, Jo (2004-06-27). “Now Charles backs coffee cure for cancer”. London: The Observer. Retrieved 2007-06-19.
- ↑ Cowell, Alan (2006-05-24). “Lying in wait for Prince Charles”. The New York Times. Retrieved 2009-10-15.
- ↑ Henderson, Mark (17 April 2008). “Prince of Wales’s guide to alternative medicine ‘inaccurate‘“. London: Times Online. Retrieved 2008-08-30.
- ↑ Singh, S. & Ernst, E. (2008). Trick or Treatment: Alternative Medicine on Trial. Corgi.
- 1 2 Tim Walker (31 Oct 2009). “Prince Charles lobbies Andy Burnham on complementary medicine for NHS”. London: Daily Telegraph. Retrieved 2010-04-01.
- ↑ “Duchy Originals Pork Pies”. The Quackometer Blog. 11 March 2009.
- ↑ Ernst, Edzard (2018). “Why Did We Call Prince Charles Foolish and Immoral?”. Skeptical Inquirer. Committee for Skeptical Inquiry. 42 (3): 8–9.
- ↑ Charity Commission. The Prince’s Foundation for Integrated Health, registered charity no. 1026800.
- ↑ The Prince’s Foundation for Integrated Health – 2007 accounts (PDF), Charity Commission, retrieved 2010-04-30
- ↑ “HRH “meddling in politics““. DC’s Improbable Science. March 12, 2007.
- ↑ Nigel Hawkes & Mark Henderson (September 1, 2006). “Doctors attack natural remedy claims”. The Times. London.
- ↑ Booth, Robert (19 March 2010). “Prince Charles health charity accused of vendetta against critic”. London: The Guardian.
- ↑ Delgado, Martin; Young, Andrew (4 April 2010). “Police probe into missing £300k at Prince Charles’ charity after bosses fail to file accounts”. Daily Mail. London.
- ↑ “Prince Charles charity to close amid fraud inquiry”. BBC News. 30 April 2010.
- ↑ Robert Booth (30 April 2010). “Prince of Wales’s health charity wound up in wake of fraud investigation”. The Guardian.
- ↑ Laura Donnelly (15 May 2010). “Homeopathy is witchcraft, say doctors”. London: The Telegraph.
- 1 2 Ian Sample (August 2, 2010). “College of Medicine born from ashes of Prince Charles’s holistic health charity”. London: The Guardian.
- ↑ Peter Dominiczak (20 August 2010). “Three years jail for accountant at Charles charity who stole £253,000”. Evening Standard. Archived from the original on 30 June 2011. Retrieved 2 February 2011.
- ↑ Jane Cassidy (15 June 2011). “Lobby Watch: The College of Medicine”. British Medical Journal. 343: d3712. doi:10.1136/bmj.d3712. PMID 21677014.
- ↑ David Colquhoun (12 July 2011). “The College of Medicine is Prince’s Foundation reincarnated”. British Medical Journal. 343: d4368. doi:10.1136/bmj.d4368. PMID 21750061.
- ↑ James May (12 July 2011). “College of Medicine: What is integrative health?”. British Medical Journal. 343: d4372. doi:10.1136/bmj.d4372. PMID 21750063.
- ↑ Edzard Ernst (12 July 2011). “College of Medicine or College of Quackery?”. British Medical Journal. 343: d4370. doi:10.1136/bmj.d4370. PMID 21750062.
- ↑ Nigel Hawkes (2010). “Prince’s foundation metamorphoses into new College of Medicine”. 341. British Medical Journal. p. 6126. doi:10.1136/bmj.c6126.
- ↑ David Colquhoun (July 25, 2010). “Buckinghamgate: the new “College of Medicine” arising from the ashes of the Prince’s Foundation for Integrated Health”. DC’s Improbable Science.
- ↑ David Colquhoun (29 October 2010). “Don’t be deceived. The new “College of Medicine” is a fraud and delusion”.
- ↑ Lewith, G. T.; Catto, G; Dixon, M; Glover, C; Halligan, A; Kennedy, I; Manning, C; Peters, D (12 July 011). College of Medicine replies to its critics”. British Medical Journal. 343: d4364. :10.1136/bmj.d4364. 21750060.
_________________________________________________
This article is, as far as I can see, factually correct. I might just add some details:
- Dixon became medical director of the FIH only a few months before it had to close.
- The FIH was also involved in Prince Charles’ complaint about me alleging I had breached confidence in relation to the Smallwood report, even though the FHI had officially nothing to do with the report.
- Mr Smallwood told me that, at that stage, Prince Charles considered the FIH to be ‘a waste of space’.
- Some time ago, the College of Medicine quietly re-named itself as the ‘College of Medicine and Integrated Health’.
- Prince Charles recently became the patron of the College of Medicine and Integrated Health.
People who use so-called alternative medicines (SCAM) tend to be more vaccine hesitant. One possible conclusion that can be drawn from this is that trusting SCAM results in people becoming more vaccine hesitant. An alternative possibility is that vaccine hesitancy and use of SCAM are both consequences of a distrust in conventional treatments. an International team of researchers conducted analyses designed to disentangle these two possibilities.
They measured vaccine hesitancy and SCAM use in a representative sample of Spanish residents (N = 5200). They also quantified their trust in three CCAM interventions; 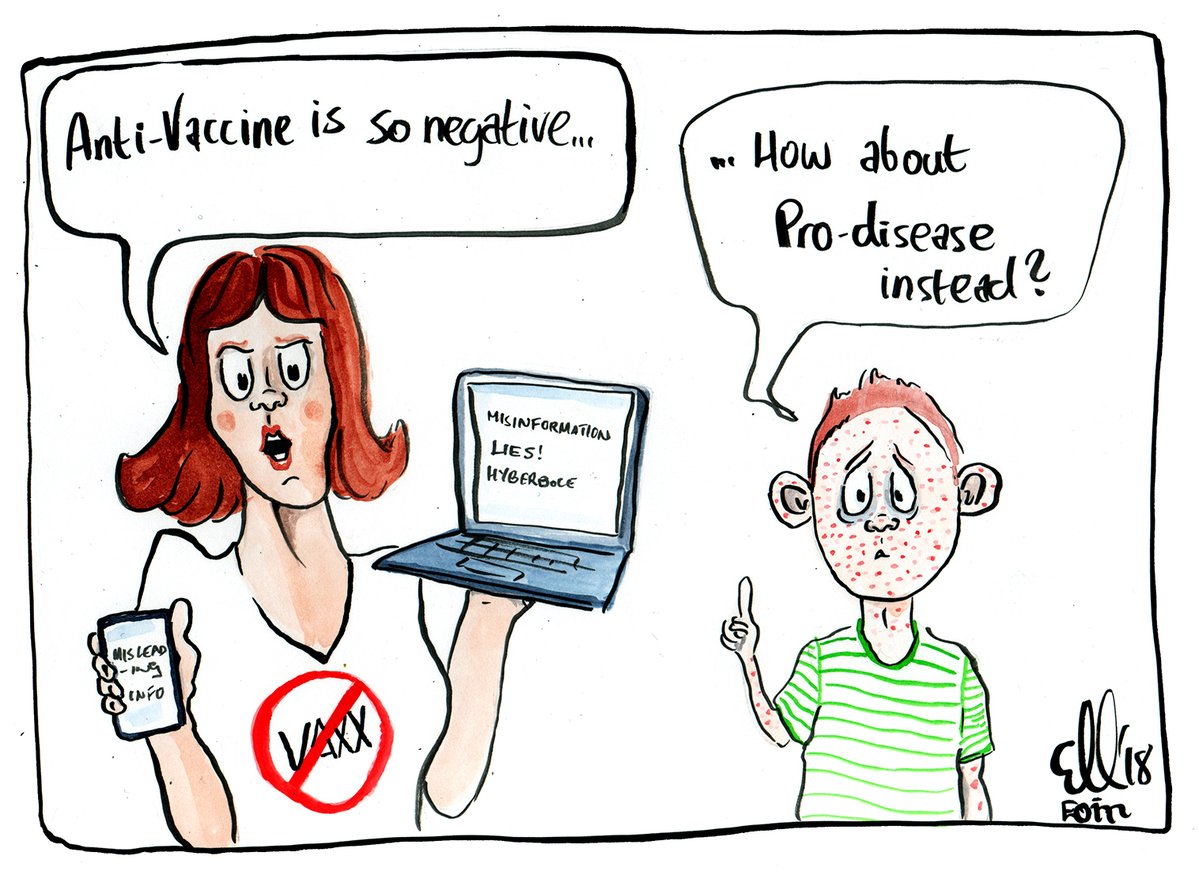
- acupuncture,
- reiki,
- homeopathy
and in two conventional medical interventions:
- chemotherapy,
- antidepressants.
Vaccine hesitancy turned out to be strongly associated with (dis)trust in conventional medicine, and this relationship was particularly strong among SCAM users. In contrast, trust in SCAM was a relatively weak predictor of vaccine hesitancy, and the relationship was equally weak regardless of whether or not participants themselves had a history of using SCAM.
According to the authors of this paper, the implication for practitioners and policy makers is that SCAM is not necessarily a major obstacle to people’s willingness to vaccinate, and that the more proximal obstacle is people’s mistrust of conventional treatments.
This is an interesting study. Yet, it begs a few questions:
- Is it possible to reliably establish trust in SCAM by asking about just 3 specific therapies?
- Is it possible to reliably establish trust in conventional medicine by asking about just 2 treatments?
- Why those therapies out of hundreds of options?
- Could it be that here are national differences (in other countries distrust in conventional medicine is not a strong determinant of SCAM use)?
- Is trust in SCAM and distrust in conventional medicine perhaps the common expression of an anti-science attitude or cultist tendencies?
THE HINDU reported on 22 May the following amazing story:
A corporator from Borivali, Riddhi Khursange, has distributed 10,000 bottles of Arsenicum Album 30, the homoeopathy medicine that was recommended by Ministry of AYUSH as a prophylactic for COVID-19. Another corporator from Ghatkopar, Pravin Chheda, has bought 25,000 bottles and has distributed over 7,100 in the past four days…
“The AYUSH Ministry must have based their claims on the benefits of the medication. The municipal corporation has also approved it for distribution,” said Mr. Chheda, who aims to distribute one lakh vials. He said all his family members have taken the three-day dose.
While the recommendation from AYUSH was issued on March 6, the Brihanmumbai Municipal Corporation (BMC) on May 8 issued a circular that 20 lakh people, including those in quarantine centres, will get the medicine.
Some experts, however, do not agree with such random, mass distribution. Also known as Ars Alb, the medication was termed as genus epidemicus (homoeopathy medicine indicated for an epidemic) during the H1N1 outbreak of 2008-2009. “Back then, Ars Alb proved extremely beneficial. But the current claim of AYUSH Ministry has not been backed by the process of genus epidemicus,” said Dr Bahubali Shah, former president of the Maharashtra Council of Homoeopathy.
“Another major problem is this general mass distribution of the medicine without an attempt to collect data on efficacy. There has to be a proper distribution protocol and a protocol for analysis. Right now, corporators, NGOs, the BMC and everyone who can get their hands on the medication are distributing it without any record-keeping,” he said.
Well-known chest physician, Dr. Zarir Udwadia, who is part of the State’s COVID-19 task force, said any alternative treatment still has to undergo a trial. “In my opinion, it should not be added on ad hoc,” said Dr. Udwadia.
The State government has set up a new committee to exclusively look at AYUSH remedies. Dr. T.P. Lahane, who is a part of the committee, said a meeting was planned on Thursday evening to discuss various options.
Meanwhile, a trial on 44 COVID-19 patients in Agra has shown that a homoeopathy medicine called Bryonia Alba was more beneficial than Ars Alb. “We have submitted our findings to Central Council of Homoeopathy and are now enrolling more patients for a bigger trial,” said Dr. Pradeep Gupta, principal of the Naiminath Homeopathy College and Hospital, who is conducting the trial.
He said 22 patients were given a placebo while 22 others were given homoeopathy medicines, Bryonia Alba, Ars Alb and Gelsemium. “19 patients who had fever, cough and weakness, responded to Bryonia within the first three days, two patients who had respiratory distress were first given Ars Alb, which relieved the breathing discomfort, but they had to be put on Bryonia Alba to relieve their fever and cough. Only one patient who came in with drowsiness was first given Gelsemium, but later put on Bryonia Alba for other symptoms,” said Dr. Gupta.
For patients in Agra, Bryonia Alba seems to be the genus epidemicus, he said. Dr. Gupta has now written to the Maharashtra government to conduct a similar trial on patients here.
Are they serious?
To me this sounds as though some amateurs are playing doctor and scientist.
I am sure we will have some homeopathy fans pointing out that India is doing very well in the pandemic and that this must be due to the widespread use of homeopathy. To this I answer that firstly India is sadly no longer doing all that well, and secondly that proof of efficacy requires more than speculation. They will reply that homeopathy has proven itself in many previous epidemics. And I will counter that this is just wishful thinking.
So, will the current pandemic finally provide the proof that homeopathy works?
No!
And the Indian homeopaths seem to be doing their utmost to obscure the picture in their hope that, in the end, they can nevertheless claim victory out of a shameful defeat.
Can I invite you to join me in a little thought experiment?
Think of a totally useless therapy. I would suggest homeopathy but there are always some who would disagree with this classification. I need a TOTALLY useless therapy, and one where we ALL can agree on the label.
What about ‘Potentised Toe-Nail Powder’ (PoToNaPo)?
PoToNaPo is made from nail clippings, thoroughly sterilised, ground to a powder, serially diluted and potentised. Does anyone claim this remedy to be effective for any condition?
No?
Splendid!
So, we all agree that PoToNaPo is completely ineffective.
Now imagine some charlatan claiming that PoToNaPo is a highly effective cancer cure. Let’s furthermore imagine that he is very successful with his claim.
(No, this is not far fetched! Think of Laetrile, Essiac, etc.)
Imagine our charlatan makes millions with PoToNaPo.
There would soon be some opposition to his quackery. The FDA would issue a statement that PoToNaPo is unproven. Perhaps the NEJM would publish an editorial saying something similar. Ethicists would frown publicly. And many sceptics would head to the pubs where clever guys would give talks about ‘the scandal of PoToNaPo’.
We all know it would happen, because it has happened with PoToNaPo-like remedies many times before.
______________
Now imagine a different scenario, namely one in which our charlatan does not claim that PoToNaPo is a cancer cure; imagine instead he had claimed that PoToNaPo is a holistic medicine that boosts your well-being via re-balancing your vital energies which, in turn, helps with anxiety which in turn might have positive effects on things like mild chronic pain, depressive mood, tension headache, insomnia, erectile dysfunction and many more symptoms of daily life.
Let’s furthermore imagine that our charlatan is very successful with these claims.
No, this is not far fetched! Think of … well … think of any SCAM really.
Imagine the charlatan makes millions with PoToNaPo.
What would happen?
- He would be invited to conferences on integrative medicine.
- Become an honorary member/sponsor of the ‘College of Medicine and Integrated Health’.
- He would be interviewed on the BBC.
- The Daily Mail would publish advertorials.
- HRH would perhaps invite him for tea.
- Trump might hint that PoToNaPo cures virus infections.
- Ainsworth might buy his patent.
- There could even be a gong waiting for him.
- And yes … some sceptics would mutter a bit, but the public would respond: what’s the harm?
We all know that things of this nature might happen, because they have happened before with PoToNaPo-like remedies.
__________________
So what’s the difference?
In both scenarios, our charlatan has marketed the same bogus remedy, PoToNaPo.
In both scenarios, he has made unsubstantiated, even fraudulent claims.
Why does he get plenty of stick in the 1st and becomes a hero in the 2nd case?
Yes, I know, the difference is the nature of the claims. But the invention, production, marketing and selling of a bogus treatment, the lying, the deceit, the fraud, the exploitation of vulnerable people are all the same.
Why then are we, as a society, so much kinder to the charlatan in the 2nd scenario?
I think we shouldn’t be; it’s not logical or consequent. I feel we should name, shame and punish both types of charlatans. They are both dangerous quacks, and it is our ethical duty to stop them.
END OF THOUGHT EXPERIMENT
The WHO have issued the following press-release:
The World Health Organization (WHO) welcomes innovations around the world including repurposing drugs, traditional medicines and developing new therapies in the search for potential treatments for COVID-19.
WHO recognizes that traditional, complementary and alternative medicine has many benefits and Africa has a long history of traditional medicine and practitioners that play an important role in providing care to populations. Medicinal plants such as Artemisia annua are being considered as possible treatments for COVID-19 and should be tested for efficacy and adverse side effects. Africans deserve to use medicines tested to the same standards as people in the rest of the world. Even if therapies are derived from traditional practice and natural, establishing their efficacy and safety through rigorous clinical trials is critical.
African governments through their Ministers of Health adopted a resolution urging Member States to produce evidence on the safety, efficacy and quality of traditional medicine at the Fiftieth Session of the WHO Regional Committee for Africa in 2000. Countries also agreed to undertake relevant research and require national medicines regulatory agencies to approve medicines in line with international standards, which include the product following a strict research protocol and undergoing tests and clinical trials. These studies normally involve hundreds of people under the monitoring of the national regulatory authorities and may take quite a few months in an expedited process.
WHO is working with research institutions to select traditional medicine products which can be investigated for clinical efficacy and safety for COVID-19 treatment. In addition, the Organization will continue to support countries as they explore the role of traditional health practitioners in prevention, control, and early detection of the virus as well as case referral to health facilities.
Over the past two decades, WHO has been working with countries to ensure safe and effective traditional medicine development in Africa by providing financial resources and technical support. WHO has supported clinical trials, leading 14 countries to issue marketing authorization for 89 traditional medicine products which have met international and national requirements for registration. Of these, 43 have been included in national essential medicines lists. These products are now part of the arsenal to treat patients with a wide range of diseases including malaria, opportunistic infections related to HIV, diabetes, sickle cell disease and hypertension. Almost all countries in the WHO African region have national traditional medicine policies, following support from WHO.
As efforts are under way to find treatment for COVID-19, caution must be taken against misinformation, especially on social media, about the effectiveness of certain remedies. Many plants and substances are being proposed without the minimum requirements and evidence of quality, safety and efficacy. The use of products to treat COVID-19, which have not been robustly investigated can put people in danger, giving a false sense of security and distracting them from hand washing and physical distancing which are cardinal in COVID-19 prevention, and may also increase self-medication and the risk to patient safety.
WHO welcomes every opportunity to collaborate with countries and researchers to develop new therapies and encourages such collaboration for the development of effective and safe therapies for Africa and the world.
________________________________
While this message – mostly directed towards Africa – seems very clear and reasonable, it is, at the same time, prone to be misunderstood. Here is an excerpt from an Ghana newspaper article commenting on the WHO initiative which demonstrates my point:
In the view of this newspaper, it stands to reason that, since the virus, was transmitted from animals, the best form of cure, is to use herbs.
We have abundance of the plant Madagascar is using to develop the cure. Medical doctors should stop seeing those practicing alternative medicine, as competitors.
The open hatred, and disdain by medical doctors, towards practitioners of alternative medicine, must be a cause for concern by all.
In the considered opinion of this newspaper, the government must bring the two together to work to avert any calamity.
The number of cases recorded so far, is a ticking time bomb. We cannot continue to treat it as business as usual, where traditional medicine practitioners, will claim to make a discovery, which will not be accepted by their counterpart who practice orthodox medicine.
If any country in Africa, should have been the first to announce a discovery of cure for coronavirus, using herbal remedy it should have been Ghana.
We can do a lot, if the two come together, instead of working at cross purpose.
This is how easily the crucial WHO message ‘the use of products to treat COVID-19, which have not been robustly investigated can put people in danger’ can be forgotten.
FIRST TEST
MAKE SURE IT WORKS
MAKE SURE IT’S REASONABLY SAFE
THEN USE IN ROUTINE CARE
Everything else is not going to be helpful!
