placebo
It was only when I came across this recent paper that I realized that, apparently, I am THE WORLD CHAMPION in acupuncture reviews. The aim of this paper was to analyze the 100 most-cited systematic reviews or meta-analyses in the field of acupuncture research. 
The Web of Science Core Collection was used to retrieve lists of 100 most-cited systematic reviews or meta-analyses in the field of acupuncture research. Two authors screened literature, extracted data, and analyzed the results.
The citation number of the 100 most-cited systematic reviews or meta-analyses varied from 65 to 577; they were published between 1989 and 2018. Fourteen authors published more than 1 study as the corresponding author and 10 authors published more than 1 study as the first author.
In terms of the corresponding authors, Edzard Ernst and Linde Klaus published the most systematic reviews/meta-analyses (n = 7). The USA published most of the systematic reviews or meta-analyses (n = 24), followed by England (n = 23) and China (n = 14). Most institutions with more than 1 study were from England (4/13). The institutions with the largest numbers of most-cited systematic reviews or meta-analyses were the Technical University of Munich in Germany, the University of Maryland School of Medicine in the USA (n = 8), the Universities of Exeter and Plymouth in England (n = 6), and the University of Exeter in England (n = 6). The journal with the largest number of most-cited systematic reviews or meta-analyses was the Cochrane Database of Systematic Reviews (n = 20), followed by Pain (n = 6). The majority of the 100 most-cited reviews are on pain or pain-related conditions. Only 4 of them focus on safety issues, and all of these are by my team.
The authors concluded that the 100 most-cited systematic reviews or meta-analyses in the acupuncture research field are mostly from high impact factor journals and developed countries. It will help researchers follow research hot spots, broaden their research scope, expand their academic horizons, and explore new research ideas, thereby improving the quality of acupuncture research.
The authors show that, both in the list of corresponding as well as first authors, I am in place number one! Not only that, they furthermore reveal that my department is also in place number 1 (as Universities of Exeter and Plymouth in England (n = 6), and the University of Exeter in England (n = 6) both refer to my unit [in the 19 years it existed the Exeter medical school changed affiliation twice]). This is remarkable, particularly because acupuncture was only one of several research foci of my team (the other 3 being herbal medicine, homeopathy, and spinal manipulation), and my department was closed almost 10 years ago.
When I write about acupuncture these days (mostly on this blog), I often get the impression that the true believers in this therapy don’t especially like what I have to say. I, therefore, fear that the concept of me being the WORLD CHAMPION of acupuncture reviews might cause some degree of displeasure to them.
What can I say?
Sorry guys!
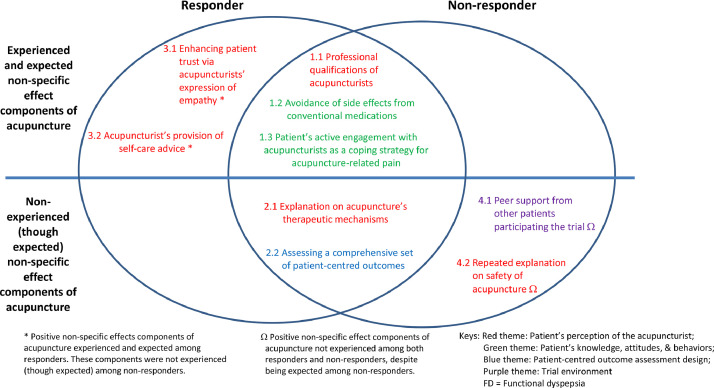
The non-specific effects constitute part of the overall effect of acupuncture. It is unclear whether responders and non-responders of acupuncture experience non-specific effects differently. This analysis aimed to compare their experiences in a nested qualitative study embedded in an acupuncture trial on functional dyspepsia.
Purposive sampling was used to capture the experience of responders (n=15) and non-responders (n=15) to acupuncture via individual in-depth interviews. Design and analysis followed a framework analysis approach, with reference to an existing model on acupuncture non-specific effects. Themes emerging outside of this model were purposefully explored.
The findings suggest that responders had a more trusting relationship with the acupuncturist in response to their expression of empathy. In turn, they were more actively engaged in lifestyle modifications and dietary advice offered by acupuncturists. Non-responders were not satisfied with the level of reassurance regarding acupuncture safety. They were also expecting more peer support from fellow participants, regarded that as an empowerment process for initiating and sustaining lifestyle changes.
The authors concluded that our results highlighted key differences in acupuncture non-specific effect components experienced by responders and non-responders. Positive non-specific effects contributing to overall benefits could be enhanced by emphasizing on empathy expression from acupuncturists, trust-building, offering appropriate explanations on safety, and organizing patient support groups. Further research on the relative importance of each component is warranted.
I doubt that this tiny study lends itself to drawing any firm conclusions. However, what they seem to imply and what the authors (proponents of acupuncture) ignore totally is the following: acupuncture responders are those people who respond to the context of the treatment situation. Thus their positive result is not due to the specific effects of acupuncture itself but to non-specific effects. In other words, acupuncture operates predominantly or entirely via non-specific effects. Or, to put it bluntly: this analysis confirms what we have discussed many times before (see for instance here, here, and here), namely that
acupuncture is a placebo therapy.
The authors of this review start their paper with the following statement:
Acupuncture has demonstrated effectiveness for symptom management among breast cancer survivors.
This, I think, begs the following question: if they already know that, why do they conduct a systematic review of the subject?
The answer becomes clear as we read thier article: they want to add another paper to the literature that shows they are correct in their assumption.
So, they do the searches and found 26 trials (2055 patients), of which 20 (1709 patients) could be included in the meta-analysis. Unsurprisingly, their results show that acupuncture was more effective than control groups in improving pain intensity [standardized mean difference (SMD) = -0.60, 95% confidence intervals (CI) -1.06 to -0.15], fatigue [SMD = -0.62, 95% CI -1.03 to -0.20], and hot flash severity [SMD = -0.52, 95% CI -0.82 to -0.22]. Compared with waitlist control and usual care groups, the acupuncture groups showed significant reductions in pain intensity, fatigue, depression, hot flash severity, and neuropathy. No serious adverse events were reported related to acupuncture intervention. Mild adverse events (i.e., bruising, pain, swelling, skin infection, hematoma, headache, menstrual bleeding) were reported in 11 studies.
The authors concluded that this systematic review and meta-analysis suggest that acupuncture significantly reduces multiple treatment-related symptoms compared with the usual care or waitlist control group among breast cancer survivors. The safety of acupuncture was inadequately reported in the included studies. Based on the available data, acupuncture seems to be generally a safe treatment with some mild adverse events. These findings provide evidence-based recommendations for incorporating acupuncture into clinical breast cancer symptom management. Due to the high risk of bias and blinding issues in some RCTs, more rigorous trials are needed to confirm the efficacy of acupuncture in reducing multiple treatment-related symptoms among breast cancer survivors.
Yes, I agree: this is an uncritical white-wash of the evidence. So, why do I bother to discuss this paper? After all, the acupuncture literature is littered with such nonsense.
Well, to my surprise, the results did contain a little gem after all.
A subgroup analysis of the data indicated that acupuncture showed no significant effects on any of the treatment-related symptoms compared with the sham acupuncture groups.
In other words, this paper confirms what has been discussed repeatedly on this blog (see for instance here, here, and here):
Acupuncture seems to be a placebo therapy!
In their 2019 systematic review of spinal manipulative therapy (SMT) for chronic back pain, Rubinstein et al included 7 studies comparing the effect of SMT with sham SMT.
They defined SMT as any hands-on treatment of the spine, including both mobilization and manipulation. Mobilizations use low-grade velocity, small or large amplitude passive movement techniques within the patient’s range of motion and control. Manipulation uses a high-velocity impulse or thrust applied to a synovial joint over a short amplitude near or at the end of the passive or physiological range of motion. Even though there is overlap, it seems fair to say that mobilization is the domain of osteopaths, while manipulation is that of chiropractors.
The researchers found:
- low-quality evidence suggesting that SMT does not result in a statistically better effect than sham SMT at one month,
- very low-quality evidence suggesting that SMT does not result in a statistically better effect than sham SMT at six and 12 months.
- low-quality evidence suggesting that, in terms of function, SMT results in a moderate to strong statistically significant and clinically better effect than sham SMT at one month. Exclusion of an extreme outlier accounted for a large percentage of the statistical heterogeneity for this outcome at this time interval (SMD −0.27, 95% confidence interval −0.52 to −0.02; participants=698; studies=7; I2=39%), resulting in a small, clinically better effect in favor of SMT.
- very low-quality evidence suggesting that, in terms of function, SMT does not result in a statistically significant better effect than sham SMT at six and 12 months.
This means that SMT has effects that are very similar to placebo (the uncertain effects on function could be interpreted as the result of residual de-blinding due to a lack of an optimal placebo or sham intervention). In turn, this means that the effects patients experience are largely or completely due to a placebo response and that SMT has no or only a negligibly small specific effect on back pain. Considering the facts that SMT is by no means risk-free and that less risky treatments exist, the inescapable conclusion is that SMT cannot be recommended as a treatment of chronic back pain.
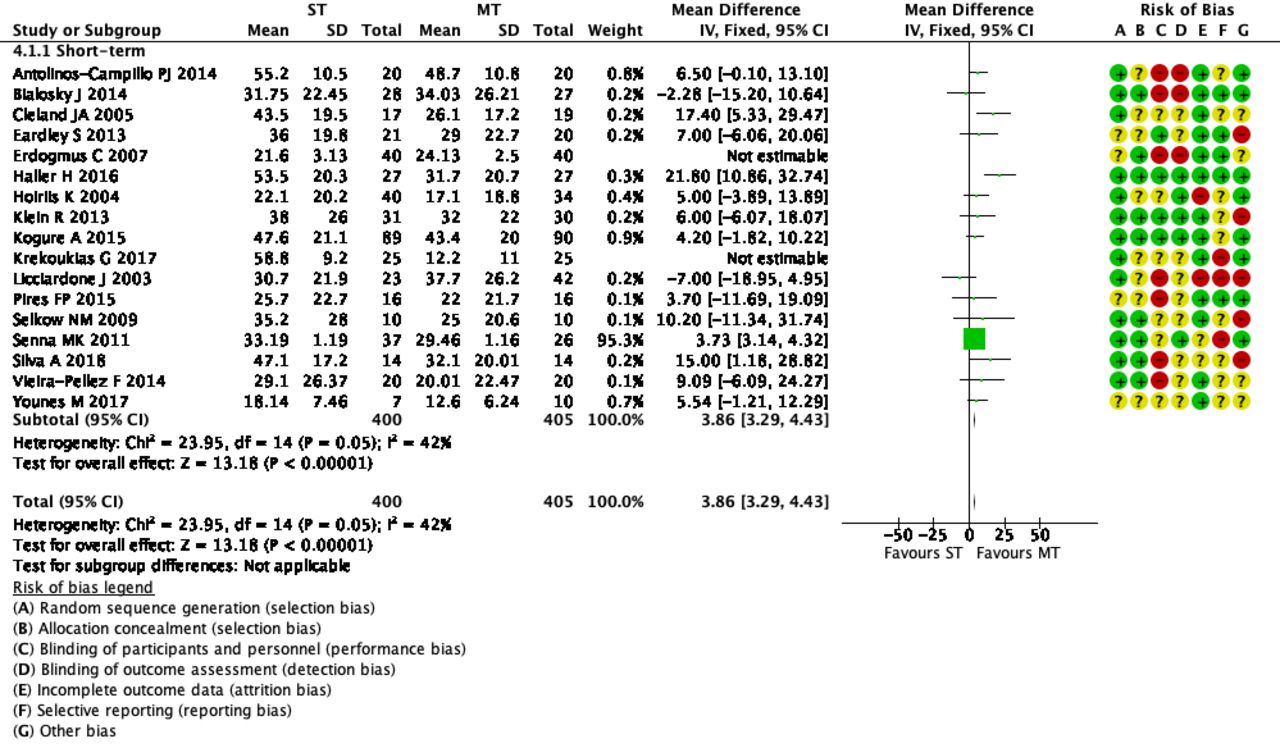
The objective of this systematic review was to assess the effects and reliability of sham procedures in manual therapy (MT) trials in the treatment of back pain (BP) in order to provide methodological guidance for clinical trial development. Different databases were screened up to 20 August 2020. Randomised clinical trials involving adults affected by BP (cervical and lumbar), acute or chronic, were included. Hand contact sham treatment (ST) was compared with different MT (physiotherapy, chiropractic, osteopathy, massage, kinesiology, and reflexology) and to no treatment. Primary outcomes were BP improvement, the success of blinding, and adverse effect (AE). Secondary outcomes were the number of drop-outs. Dichotomous outcomes were analysed using risk ratio (RR), continuous using mean difference (MD), 95% CIs. The minimal clinically important difference was 30 mm changes in pain score.
A total of 24 trials were included involving 2019 participants. Different manual treatments were provided:
- SM/chiropractic (7 studies, 567 participants).
- Osteopathy (5 trials, 645 participants).
- Kinesiology (1 trial, 58 participants).
- Articular mobilisations (6 trials, 445 participants).
- Muscular release (5 trials, 304 participants).
Very low evidence quality suggests clinically insignificant pain improvement in favour of MT compared with ST (MD 3.86, 95% CI 3.29 to 4.43) and no differences between ST and no treatment (MD -5.84, 95% CI -20.46 to 8.78).ST reliability shows a high percentage of correct detection by participants (ranged from 46.7% to 83.5%), spinal manipulation being the most recognised technique. Low quality of evidence suggests that AE and drop-out rates were similar between ST and MT (RR AE=0.84, 95% CI 0.55 to 1.28, RR drop-outs=0.98, 95% CI 0.77 to 1.25). A similar drop-out rate was reported for no treatment (RR=0.82, 95% 0.43 to 1.55).
Forest plot of comparison ST versus MT in back pain outcome at short term. MT, manual therapy; ST, sham treatment.
The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
Essentially these findings suggest that the effects patients experience after MT are not due to MT per see but to placebo effects. The review could be criticised because of the somewhat odd mix of MTs lumped together in one analysis. Yet, I think it is fair to point out that most of the studies were of chiropractic and osteopathy. Thus, this review implies that chiropractic and osteopathy are essentially placebo treatments.
The authors of the review also provide this further comment:
Similar findings were found in other reviews conducted on LBP. Ruddock et al included studies where SM was compared with what authors called ‘an effective ST’, namely a credible sham manipulation that physically mimics the SM. Pooled data from four trials showed a very small and not clinically meaningful effect in favour of MT.52
Rubinstein et al 53 compared SM and mobilisation techniques to recommended, non-recommended therapies and to ST. Their findings showed that 5/47 studies included attempted to blind patients to the assigned intervention by providing an ST. Of these five trials, two were judged at unclear risk of participants blinding. The authors also questioned the need for additional studies on this argument, as during the update of their review they found recent small pragmatic studies with high risk of bias. We agree with Rubinstein et al that recent studies included in this review did not show a higher quality of evidence. The development of RCT with similar characteristic will probably not add any proof of evidence on MT and ST effectiveness.53
If we agree that chiropractic and osteopathy are placebo therapies, we might ask whether they should have a place in the management of BP. Considering the considerable risks associated with them, I feel that the answer is obvious and simple:
NO!
This multicenter, randomized, sham-controlled trial was aimed at assessing the long-term efficacy of acupuncture for chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS). Men with moderate to severe CP/CPPS were recruited, regardless of prior exposure to acupuncture. They received sessions of acupuncture or sham acupuncture over 8 weeks, with a 24-week follow-up after treatment. Real acupuncture treatment was used to create the typical de qi sensation, whereas the sham acupuncture treatment (the authors state they used the Streitberger needle, but the drawing looks more as though they used our device) does not generate this feeling.
The primary outcome was the proportion of responders, defined as participants who achieved a clinically important reduction of at least 6 points from baseline on the National Institutes of Health Chronic Prostatitis Symptom Index at weeks 8 and 32. Ascertainment of sustained efficacy required the between-group difference to be statistically significant at both time points.
A total of 440 men (220 in each group) were recruited. At week 8, the proportions of responders were:
- 60.6% (95% CI, 53.7% to 67.1%) in the acupuncture group
- 36.8% (CI, 30.4% to 43.7%) in the sham acupuncture group (adjusted difference, 21.6 percentage points [CI, 12.8 to 30.4 percentage points]; adjusted odds ratio, 2.6 [CI, 1.8 to 4.0]; P < 0.001).
At week 32, the proportions were:
- 61.5% (CI, 54.5% to 68.1%) in the acupuncture group
- 38.3% (CI, 31.7% to 45.4%) in the sham acupuncture group (adjusted difference, 21.1 percentage points [CI, 12.2 to 30.1 percentage points]; adjusted odds ratio, 2.6 [CI, 1.7 to 3.9]; P < 0.001).
Twenty (9.1%) and 14 (6.4%) adverse events were reported in the acupuncture and sham acupuncture groups, respectively. No serious adverse events were reported. No significant difference was found in changes in the International Index of Erectile Function 5 score at all assessment time points or in peak and average urinary flow rates at week 8.
The authors concluded that, compared with sham therapy, 20 sessions of acupuncture over 8 weeks resulted in greater improvement in symptoms of moderate to severe CP/CPPS, with durable effects 24 weeks after treatment.
The study was sponsored by the China Academy of Chinese Medical Sciences and the National Administration of Traditional Chinese Medicine. The trialists originate from the following institutions:
- 1Guang’anmen Hospital, China Academy of Chinese Medical Sciences, Beijing, China (Y.S., B.L., Z.Q., J.Z., J.W., X.L., W.W., R.P., H.C., X.W., Z.L.).
- 2Key Laboratory of Chinese Internal Medicine of Ministry of Education, Dongzhimen Hospital, Beijing University of Chinese Medicine, Beijing, China (Y.L.).
- 3ThedaCare Regional Medical Center – Appleton, Appleton, Wisconsin (K.Z.).
- 4Hengyang Hospital Affiliated to Hunan University of Chinese Medicine, Hengyang, China (Z.Y.).
- 5The First Hospital of Hunan University of Chinese Medicine, Changsha, China (W.Z.).
- 6Guangdong Provincial Hospital of Traditional Chinese Medicine, Guangzhou, China (W.F.).
- 7The First Affiliated Hospital of Anhui University of Chinese Medicine, Hefei, China (J.Y.).
- 8West China Hospital of Sichuan University, Chengdu, China (N.L.).
- 9China Academy of Chinese Medical Sciences, Beijing, China (L.H.).
- 10Yantai Hospital of Traditional Chinese Medicine, Yantai, China (Z.Z.).
- 11Shaanxi Provincial Hospital of Traditional Chinese Medicine, Xi’an, China (T.S.).
- 12The Third Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, China (J.F.).
- 13Beijing Fengtai Hospital of Integrated Traditional and Western Medicine, Beijing, China (Y.D.).
- 14Xi’an TCM Brain Disease Hospital, Xi’an, China (H.S.).
- 15Dongfang Hospital Beijing University of Chinese Medicine, Beijing, China (H.H.).
- 16Luohu District Hospital of Traditional Chinese Medicine, Shenzhen, China (H.Z.).
- 17Guizhou University of Traditional Chinese Medicine, Guiyang, China (Q.M.).
These facts, together with the previously discussed notion that clinical trials from China are notoriously unreliable, do not inspire confidence. Moreover, one might well wonder about the authors’ claim that patients were blinded. As pointed out above, the real and sham acupuncture were fundamentally different: the former did generate de qi, while the latter did not! A slightly pedantic point is my suspicion that the trial did not test the efficacy but the effectiveness of acupuncture, if I am not mistaken. Finally, one might wonder what the rationale of acupuncture as a treatment of CP/CPPS might be. As far as I can see, there is no plausible mechanism (other than placebo) to explain the effects.
So, is the evidence that emerged from the new study convincing?
No, in my view, it is not!
In fact, I am surprised that a journal as reputable as the Annals of Internal Medicine published it.
The purpose of this qualitative research was to explore whether pilgrims visiting Lourdes, France had transcendent experiences and to examine their nature.
For this purpose, the researchers traveled to Lourdes and spoke with 67 pilgrims including assisted pilgrims, young volunteers, and medical staff. About two in five reported a transcendent experience: some felt they had communicated or had close contact with a divine presence, while others reported a powerful experience of something intangible and otherworldly.
The authors concluded that visiting Lourdes can have a powerful effect on a pilgrim and may include an “out of the ordinary” transcendent experience, involving a sense of relationship with the divine, or experiences of something otherworldly and intangible. There is a growing focus on Lourdes as a place with therapeutic benefits rather that cures: our analysis suggests that transcendent experiences can be central to this therapeutic effect. Such experiences can result in powerful emotional responses, which themselves may contribute to long term well-being. Our participants described a range of transcendent experiences, from the prosaic and mildly pleasant, to intense experiences that affected pilgrims’ lives. The place itself is crucially important, above all the Grotto, as a space where pilgrims perceive that the divine can break through into normal life, enabling closer connections with the divine, with nature and with the self.
Some people can have powerful effects when they expect something powerful. So what?
To make any sense out of this, we need a controlled experiment. I am glad to tell you that Austrian psychologists recently published a controlled study of this type. They tested the effects of tap water labeled as Lourdes water versus tap water labeled as tap water found that placebos in the context of religious beliefs and practices can change the experience of emotional salience and cognitive control which is accompanied by connectivity changes in the associated brain networks. They concluded that the findings of the present study allow us to draw preliminary conclusions about the placebo effect in the context of religious beliefs and practices. We found that this type of placebo can enhance emotional-somatic well-being, and can lead to changes in rsFC in cognitive control/emotional salience networks of the brain. Future research is warranted to replicate the results. Moreover, future research should investigate whether the observed effects generalize across different religious affiliations. The idea of “holy water” (or blessed water) is common in several religions, from Christianity, Islam, Buddhism to Sikhism.
Placebo can enhance emotional-somatic well-being. Expectation can play all sorts of tricks on us. This makes sense to me – much to the contrary to the ‘qualitative study’ suggesting that transcendental experiences can be central to this therapeutic effect experienced by believers in Lourdes.
Recently, I received this comment from a reader:
Edzard-‘I see you do not understand much of trial design’ is true BUT I wager that you are in the same boat when it comes to a design of a trial for LBP treatment: not only you but many other therapists. There are too many variables in the treatment relationship that would allow genuine , valid criticism of any design. If I have to pick one book of the several listed elsewhere I choose Gregory Grieve’s ‘Common Vertebral Joint Problems’. Get it, read it, think about it and with sufficient luck you may come to realize that your warranted prejudices against many unconventional ‘medical’ treatments should not be of the same strength when it comes to judging the physical therapy of some spinal problems as described in the book.
And a chiro added:
EE: I see that you do not understand much of trial design
Perhaps it’s Ernst who doesnt understand how to research back pain.
“The identification of patient subgroups that respond best to specific interventions has been set as a key priority in LBP research for the past 2 decades.2,7 In parallel, surveys of clinicians managing LBP show that there are strong views against generic treatment and an expectation that treatment should be individualized to the patient.6,22.”
Journal of Orthopaedic & Sports Physical Therapy
Published Online:January 31, 2017Volume47Issue2Pages44-48
Do I need to explain why the Grieve book (yes, I have it and yes, I read it) is not a substitute for evidence that an intervention or technique is effective? No, I didn’t think so. This needs to come from a decent clinical trial.
And how would one design a trial of LBP (low back pain) that would be a meaningful first step and account for the “many variables in the treatment relationship”?
How about proceeding as follows (the steps are not necessarily in that order):
- Study the previously published literature.
- Talk to other experts.
- Recruit a research team that covers all the expertise you need (and don’t have yourself).
- Formulate your research question. Mine would be IS THERAPY XY MORE EFFECTIVE THAN USUAL CARE FOR CHRONIC LBP? I know LBP is but a vague symptom. This does, however, not necessarily matter (see below).
- Define primary and secondary outcome measures, e.g. pain, QoL, function, as well as the validated methods with which they will be quantified.
- Clarify the method you employ for monitoring adverse effects.
- Do a small pilot study.
- Involve a statistician.
- Calculate the required sample size of your study.
- Consider going multi-center with your trial if you are short of patients.
- Define chronic LBP as closely as you can. If there is evidence that a certain type of patient responds better to the therapy xy than others, that might be considered in the definition of the type of LBP.
- List all inclusion and exclusion criteria.
- Make sure you include randomization in the design.
- Randomization should be to groups A and B. Group A receives treatment xy, while group B receives usual care.
- Write down what A and B should and should not entail.
- Make sure you include blinding of the outcome assessors and data evaluators.
- Define how frequently the treatments should be administered and for how long.
- Make sure all therapists employed in the study are of a high standard and define the criteria of this standard.
- Train all therapists of both groups such that they provide treatments that are as uniform as possible.
- Work out a reasonable statistical plan for evaluating the results.
- Write all this down in a protocol.
Such a trial design does not need patient or therapist blinding nor does it require a placebo. The information it would provide is, of course, limited in several ways. Yet it would be a rigorous test of the research question.
If the results of the study are positive, one might consider thinking of an adequate sham treatment to match therapy xy and of other ways of firming up the evidence.
As LBP is not a disease but a symptom, the study does not aim to include patients that all are equal in all aspects of their condition. If some patients turn out to respond better than others, one can later check whether they have identifiable characteristics. Subsequently, one would need to do a trial to test whether the assumption is true.
Therapy xy is complex and needs to be tailored to the characteristics of each patient? That is not necessarily an unsolvable problem. Within limits, it is possible to allow each therapist the freedom to chose the approach he/she thinks is optimal. If the freedom needed is considerable, this might change the research question to something like ‘IS THAT TYPE OF THERAPIST MORE EFFECTIVE THAN THOSE EMPLOYING USUAL CARE FOR CHRONIC LBP?’
My trial would obviously not answer all the open questions. Yet it would be a reasonable start for evaluating a therapy that has not yet been submitted to clinical trials. Subsequent trials could build on its results.
I am sure that I have forgotten lots of details. If they come up in discussion, I can try to incorporate them into the study design.
Post-traumatic stress disorder (PTSD), previously known as battle fatigue syndrome or shell shock, is a condition that can be triggered by the experience of some frightening event. PTSD can be debilitating leading to the production of feelings of helplessness, intense fear, and horror. Numerous treatments of PTSD exist but few have been shown to be truly effective. A team of Canadian researchers explored the effects of cannabis on PTSD symptoms, quality of life (QOL), and return to work (RTW). Their systematic review also investigated harms such as adverse effects and dropouts due to adverse effects, inefficacy, and all-cause dropout rates.
Their electronic searches located one RCT and 10 observational studies (n = 4672). Risk of bias (RoB) was assessed with the Cochrane risk of bias tool and ROBINS-I. Evidence from the included studies was mainly based on studies with no comparators. Results from unpooled, high RoB studies suggested that cannabis was associated with a reduction in overall PTSD symptoms and improved QOL. Dry mouth, headaches, and psychoactive effects such as agitation and euphoria were the most commonly reported adverse effects. In most studies, cannabis was well tolerated. A small proportion of patients experienced a worsening of PTSD symptoms.
The authors concluded that the evidence in the current study primarily stems from low quality and high RoB observational studies. Further RCTs investigating cannabis effects on PTSD treatment should be conducted with larger sample sizes and explore a broader range of patient-important outcomes.
Various drugs are currently used for the treatment of PTSD including selective serotonin reuptake inhibitors; tricyclic antidepressants (amitriptyline and isocarboxazid); mood stabilizers (Divalproex and lamotrigine); atypical antipsychotics (aripiprazole and quetiapine) but their effectiveness has not been proven. A recent systematic review included 30 RCTs of a range of heterogeneous non-psychological and non-pharmacological interventions. There was emerging evidence for 6 different approaches:
- acupuncture,
- neurofeedback,
- saikokeishikankyoto (a herbal preparation),
- somatic experiencing,
- transcranial magnetic stimulation,
- yoga.
This list makes me wonder: are these treatments, including cannabis, truly promising, or is PTSD one of those conditions for which nearly every treatment works a little because of its placebo effect?
This systematic review assessed the effects and reliability of sham procedures in manual therapy (MT) trials in the treatment of back pain (BP) in order to provide methodological guidance for clinical trial development.
Different databases were screened up to 20 August 2020. Randomized controlled trials involving adults affected by BP (cervical and lumbar), acute or chronic, were included. Hand contact sham treatment (ST) was compared with different MT (physiotherapy, chiropractic, osteopathy, massage, kinesiology, and reflexology) and to no treatment. Primary outcomes were BP improvement, the success of blinding, and adverse effects (AE). Secondary outcomes were the number of drop-outs. Dichotomous outcomes were analyzed using risk ratio (RR), continuous using mean difference (MD), 95% CIs. The minimal clinically important difference was 30 mm changes in pain score.
A total of 24 trials were included involving 2019 participants. Most of the trials were of chiropractic manipulation. Very low evidence quality suggests clinically insignificant pain improvement in favor of MT compared with ST (MD 3.86, 95% CI 3.29 to 4.43) and no differences between ST and no treatment (MD -5.84, 95% CI -20.46 to 8.78).ST reliability shows a high percentage of correct detection by participants (ranged from 46.7% to 83.5%), spinal manipulation is the most recognized technique. Low quality of evidence suggests that AE and drop-out rates were similar between ST and MT (RR AE=0.84, 95% CI 0.55 to 1.28, RR drop-outs=0.98, 95% CI 0.77 to 1.25). A similar drop-out rate was reported for no treatment (RR=0.82, 95% 0.43 to 1.55).
 The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
The optimal therapy for back pain does not exist or has not yet been identified; there are dozens of different approaches but none has been found to be truly and dramatically effective. Manual therapies like chiropractic and osteopathy are often used, and some data suggest that they are as good (or as bad) as most other options. This review confirms what we have discussed many times previously (e.g. here), namely that the small positive effect of MT, or specifically spinal manipulation, is largely due to placebo.
Considering this information, what is the best treatment for back pain sufferers? The answer seems obvious: it is a therapy that is as (in)effective as all the others but causes the least harm or expense. In other words, it is not chiropractic nor osteopathy but exercise.
My conclusion:
avoid therapists who use spinal manipulation for back pain.