causation
There are plenty of people who find it hard to accept that highly diluted homeopathic remedies are placebos. They religiously believe in the notion that homeopathy works and studiously ignore the overwhelming evidence (plus a few laws of nature). Yet, they pretend to staunchly believe in science and keep on conducting (pseudo?) scientific studies of homeopathy. To me, this seems oddly schizophrenic because, on the one hand, they seem to accept science by conducting trials, while, on the other hand, they reject science by negating the scientific consensus.
The objective of this recent study was to evaluate the quality of life (QoL) of women treated with homeopathy within the Public Health System of Belo Horizonte, Brazil.
The study was designed as a prospective randomized controlled pragmatic trial. The patients were divided into two independent groups, one group underwent homeopathic treatment during a 6-month period, while the other did not receive any homeopathic treatment. In both randomized groups, patients maintained their conventional medical treatment as necessary. The World Health Organization Quality of Life abbreviated questionnaire (WHOQOL-BREF) was used for QoL analysis prior to treatment and 6 months later.
Randomization was successful in that it resulted in similar baseline results in three domains of QoL analysis for both groups. After 6 months’ treatment, the investigators noted a statistically significant difference between groups in the physical domain of WHOQOL-BREF: the average score improved to 63.6 ± (SD) 15.8 in the homeopathy group, compared with 53.1 ± (SD) 16.7 in the control group.
The authors concluded that homeopathic treatment showed a positive impact at 6 months on the QoL of women with chronic diseases. Further studies should be performed to determine the long-term effects of homeopathic treatment on QoL and its determinant factors.
I would not be surprised if the world of homeopathy were to celebrate this trial as yet another proof that homeopathy is effective. I am afraid, however, that I might have to put a damper on their excitement:
THIS STUDY DOES NOT SHOW WHAT YOU THINK IT DOES.
Why not?
Regular readers of this blog will have already guessed it: the trail follows the infamous ‘A+B versus B’ design. Some people will think that I am obsessed with this theme – but I am not; it’s just that, in SCAM, it comes up with such depressing regularity. And as this blog is mainly about commenting on newly published research, I am unable to avoid the subject.
So, let me explain it again.
Think of it in monetary terms: you have an amount X, your friend has the same amount X plus an extra sum Y. Who do you think has more money? You don’t need to be a genius to guess, do you?
The same happens in the above ‘A+B versus B’ trial:
- the patients in group 1 received homeopathy (A) plus usual care (B);
- the patients in group 2 received usual care (B) and nothing else.
You don’t need to be a genius to guess who might have the better outcomes.
Because of homeopathy?
No! Because of the patients’ expectation, the placebo effect, and the extra attention of the homeopaths. They call this trial design ‘pragmatic’. I feel it is an attempt to mislead the public.
So, allow me to re-write the authors’ conclusion as follows:
The effect of a homeopathic consultation and the administration of a placebo generated a positive impact at 6 months on the QoL of women with chronic diseases. This was entirely predictable and totally unrelated to homeopathy. Further studies to determine the long-term effects of homeopathic treatment on QoL and its determinant factors are not needed.
This study was aimed at determining the effectiveness of electroacupuncture or auricular acupuncture for chronic musculoskeletal pain in cancer survivors.
The Personalized Electroacupuncture vs Auricular Acupuncture Comparativeness Effectiveness (PEACE) trial is a randomized clinical trial that was conducted from March 2017 to October 2019 (follow-up completed April 2020) across an urban academic cancer center and 5 suburban sites in New York and New Jersey. Study statisticians were blinded to treatment assignments. The 360 adults included in the study had a prior cancer diagnosis but no current evidence of disease, reported musculoskeletal pain for at least 3 months, and self-reported pain intensity on the Brief Pain Inventory (BPI) ranging from 0 (no pain) to 10 (worst pain imaginable).
Patients were randomized 2:2:1 to:
- electroacupuncture (n = 145),
- auricular acupuncture (n = 143),
- or usual care (n = 72).
Intervention groups received 10 weekly sessions of electroacupuncture or auricular acupuncture. Ten acupuncture sessions were offered to the usual care group from weeks 12 through 24.
The primary outcome was a change in the average pain severity score on the BPI from baseline to week 12. Using a gatekeeping multiple-comparison procedure, electroacupuncture and auricular acupuncture were compared with usual care using a linear mixed model. Noninferiority of auricular acupuncture to electroacupuncture was tested if both interventions were superior to usual care.
Among 360 cancer survivors (mean [SD] age, 62.1 [12.7] years; mean [SD] baseline BPI score, 5.2 [1.7] points; 251 [69.7%] women; and 88 [24.4%] non-White), 340 (94.4%) completed the primary end point. Compared with usual care, electroacupuncture reduced pain severity by 1.9 points (97.5% CI, 1.4-2.4 points; P < .001) and auricular acupuncture reduced by 1.6 points (97.5% CI, 1.0-2.1 points; P < .001) from baseline to week 12. Noninferiority of auricular acupuncture to electroacupuncture was not demonstrated. Adverse events were mild; 15 of 143 (10.5%) patients receiving auricular acupuncture and 1 of 145 (0.7%) patients receiving electroacupuncture discontinued treatments due to adverse events (P < .001).
The authors of this study concluded that, in this randomized clinical trial among cancer survivors with chronic musculoskeletal pain, electroacupuncture and auricular acupuncture produced greater pain reduction than usual care. However, auricular acupuncture did not demonstrate noninferiority to electroacupuncture, and patients receiving it had more adverse events.
I think the authors made a mistake in formulating their conclusions. Perhaps they allow me to correct it:
In this randomized clinical trial among cancer survivors with chronic musculoskeletal pain, electroacupuncture plus usual care and auricular acupuncture plus usual care produced greater pain reduction than usual care alone.
I know, I must sound like a broken record, but – because it followed the often-discussed ‘A+B versus B’ design – this study does simply not show what the authors conclude. In fact, it tells us very little about any effects caused by the two acupuncture versions per se. The study does not control for placebo effects and therefore its results are consistent with acupuncture itself having no effect at all.
Here is an attempt at explaining the ‘A+B versus B’ study design I posted previously:
As regularly mentioned on this blog, there are several ways to design a study such that the risk of producing a negative result is minimal. The most popular one in SCAM research is the ‘A+B versus B’ design…
Imagine you have an amount of money A and your friend owns the same sum plus another amount B. Who has more money? Simple, it is, of course your friend: A+B will always be more than A [unless B is a negative amount]. For the same reason, such “pragmatic” trials will always generate positive results [unless the treatment in question does actual harm]. Treatment as usual plus acupuncture is more than treatment as usual alone, and the former is therefore more than likely to produce a better result. This will be true, even if acupuncture is a pure placebo – after all, a placebo is more than nothing, and the placebo effect will impact on the outcome, particularly if we are dealing with a highly subjective symptom such as fatigue.
Imagine the two interventions had been a verbal encouragement or pat on the shoulder or a pat on the right shoulder for group 1 and one on the left for group 2. The findings could well have been very similar. To provide evidence that acupuncture PRODUCES PAIN REDUCTION, we need proper tests of the hypothesis. And to ‘determine the effectiveness of electroacupuncture or auricular acupuncture for chronic musculoskeletal pain in cancer survivors’, we need a different methodology.
This is, of course, all very elementary. Nothing elaborate or complicated! Scientists know it; editors know it; reviewers know it. Or at least they should know it. Therefore, I am at a loss trying to understand why even journals of high standing publish IMPROPER tests, better known as pseudo-science.
It is hard not to conclude that they deliberately try to mislead us.
When I yesterday reported about Charles’ new paper in a medical journal, I omitted to go into any sort of detail. Merely mumbling ‘this is bait and switch‘ and ‘there is no good evidence that social prescribing is effective‘, is not good enough. Charles deserves better! That’s why today I provide a more detailed analysis of what he wrote on social prescribing.
Social prescribing is a concept that emerged in the UK more than a decade ago [1]. It aims to connect patients to different types of community support, including social events, fitness classes, and social services. Trained professionals, often called link workers or community connections, work with healthcare providers to offer referrals to these types of support. Social prescribing largely exists to fill in healthcare treatment gaps. The basic medical treatment cannot address every concern. Primary care providers don’t always have enough time to get to know their patients and understand the complete picture of their lives.
For example, loneliness can cause stress, which can eventually affect sleep, nutrition, and physical health. Doctors may not be able to offer much help for this problem. That’s where link workers step in. They can provide more specialized support if someone struggles to meet basic wellness or social needs. They get to know a patient’s unique needs and help you take action to meet those needs by referring him or her to helpful resources in the community.[2]
Charles elaborated on social prescribing (or social prescription, as he calls it for some reason) as follows [the numbers in square brackets were added me and refer to my comments below]:
… For a long time, I have been an advocate of what is now called social prescription and this may just be the key to integrating the biomedical, the psychosocial and the environmental, as well as the nature of the communities within which we live and which have such an enormous impact on our health and wellbeing [1]. In particular, I believe that social prescription can bring together the aims of the health service, local authorities, and the voluntary and volunteer sector. Biomedicine has been spectacularly successful in treating and often curing disease that was previously incurable. Yet it cannot hold all the answers, as witnessed, for instance, by the increasing incidence of long-term disease, antibiotic resistance and opiate dependence [2]. Social prescription enables medicine to go beyond pills and procedures and to recognise the enormous health impact of the lives we lead and the physical and social environment within which we live [3]. This is precisely why I have spent so many years trying to demonstrate the vitally important psychosocial, environmental and financial added value of genuinely, sustainable urban planning, design and construction [4].
There is research from University College London, for instance, which shows that you are almost three times more likely to overcome depression if you have a hobby [5]. Social prescription enables doctors to provide their patients with a bespoke prescription that might help them at a time of need …
When we hear that a quarter of 14–16-year-old girls are self-harming and almost a third of our children are overweight or obese, it should make us realise that we will have to be a bit more radical in addressing these problems [5]. And though social prescription cannot do everything, I believe that, used imaginatively, it can begin to tackle these deep-rooted issues [6]. As medicine starts to grapple with these wider determinants of health [7], I also believe that medicine will need to combine bioscience with personal beliefs, hopes, aspirations and choices [8].
Many patients choose to see complementary practitioners for interventions such as manipulation, acupuncture and massage [9]. Surely in an era of personalised medicine, we need to be open-minded about the choices that patients make and embrace them where they clearly improve their ability to care for themselves? [10] Current NHS guidelines on pain that acknowledge the role of acupuncture and mindfulness may lead, I hope, to a more fruitful discussion on the role of complementary medicine in a modern health service [11]. I have always advocated ‘the best of both worlds’ [12], bringing evidence-informed [13] conventional and complementary medicine together and avoiding that gulf between them, which leads, I understand, to a substantial proportion of patients feeling that they cannot discuss complementary medicine with their doctors [14].
I believe it is more important than ever that we should aim for this middle ground [15]. Only then can we escape divisions and intolerance on both sides of the conventional/complementary equation where, on the one hand, the appropriate regulation of the proven therapies of acupuncture and medical herbalism [15] is opposed while, on the other, we find people actually opposing life-saving vaccinations. Who would have thought, for instance, that in the 21st century that there would be a significant lobby opposing vaccination, given its track record in eradicating so many terrible diseases and its current potential to protect and liberate some of the most vulnerable in our society from coronavirus? [16] …
My comments are as follows:
- Is Charles not a little generous to his own vision? Social prescribing is not nearly the same as the concept of integrated medicine which he has been pushing for years.
- There is no good evidence that social prescribing will reduce ‘of long-term disease, antibiotic resistance, and opiate dependence’.
- Here Charles produces a classic ‘strawman fallacy’. Medicine is much more than pills and procedures, and I suspect he knows it (not least because he uses proper medicine as soon as he is really ill).
- Charles has not so much ‘demonstrated’ the importance of ‘psychosocial, environmental and financial added value of genuinely, sustainable urban planning, design, and construction’ as talked about it.
- That does not necessarily mean that social prescribing is effective; correlation is not causation!
- There is no good evidence that social prescribing is effective against self-harm or obesity.
- Medicine has been trying to grapple with ‘wider issues’ for centuries.
- Medicine has done that for many years but we always had to be mindful of the evidence base. It would be unwise to adopt interventions without evidence demonstrating that they do more good than harm.
- Many patients also choose to smoke, drink, or sky-dive. Patient choice is no indicator of efficacy or harmlessness.
- Yes, we should embrace them where they clearly improve their ability to care for themselves. However, the evidence all too often fails to show that they improve anything.
- As we have seen, this discussion has been going on for decades and was not always helped by Charles.
- The best of both worlds can only be treatments that demonstrably generate more good than harm – and that’s called evidence-based medicine. Or, to put it bluntly: in medicine ‘best’ does not signify royal approval.
- ‘Evidence-informed’ is an interesting term. Proper medicine thrives to be evidence-based; royal medicine merely needs to be ‘evidence-informed’? This new term seems to imply that evidence is not all that important. Why? Perhaps because, for alternative medicine, it is largely not based on good evidence?
- If we want to bridge the gulf, we foremost require sound evidence. Today, plenty of such evidence is available. The problem is that it does often not show what Charles seems to think it shows.
- Even the best regulation of nonsense must result in nonsense.
- The anti-vaccination sentiments originate to an alarmingly large extent from the realm of alternative medicine.[4]
REFERENCES
[1] Brandling J, House W. Social prescribing in general practice: adding meaning to medicine. Br J Gen Pract. (2009) 59:454–6. doi: 10.3399/bjgp09X421085
[2] Social Prescribing: Definition, Examples, and More (healthline.com)
[3] Schmidt K, Ernst E. MMR vaccination advice over the Internet. Vaccine. 2003 Mar 7;21(11-12):1044-7. doi: 10.1016/s0264-410x(02)00628-x. PMID: 12559777.
Therapeutic touch (TT) is a form of paranormal or energy healing developed by Dora Kunz (1904-1999), a psychic and alternative practitioner, in collaboration with Dolores Krieger, a professor of nursing. According to Kunz, TT has its origins in ancient Yogic texts. TT is popular and practiced predominantly by US nurses; it is currently being taught in more than 80 colleges and universities in the U.S., and in more than seventy countries. According to one TT-organisation, TT is a holistic, evidence-based therapy that incorporates the intentional and compassionate use of universal energy to promote balance and well-being. It is a consciously directed process of energy exchange during which the practitioner uses the hands as a focus to facilitate the process.
The assumptions that form the basis for TT are not biologically plausible. But that does not necessarily mean it is ineffective.
This study was conducted to assess the effect of therapeutic touch on stress, daytime sleepiness, sleep quality, and fatigue among students of nursing and midwifery.
A total of 96 students were randomized into three groups: the therapeutic touch (TT) group, the sham therapeutic touch (STT) group, and the control group. The TT group was subjected to therapeutic touch twice a week for 4 weeks with each session lasting 20 min.
When the TT group was compared to the STT and control groups following the intervention, the decrease in the levels of stress, fatigue, and daytime sleepiness, as well as the increase in the sleep quality were found to be significant.
The authors concluded that TT, which is one form of complementary therapy, was relatively effective in decreasing the levels of stress, fatigue and daytime sleepiness, and in increasing the sleep quality of university students of nursing and midwifery.
Several previous trials and reviews of TT are available. However, many of them were conducted ardent proponents of TT, seriously flawed, and thus less than reliable. One rigorous pre-clinical study, co-designed by a 9-year-old girl, found that experienced TT practitioners were unable to detect the investigator’s “energy field.” Their failure to substantiate TT’s most fundamental claim is unrefuted evidence that the claims of TT are groundless and that further professional use is unjustified.
In my recent book, I concluded that there are no reasons to assume that TT causes any meaningful effects beyond placebo. One could, however, argue that, like all forms of paranormal healing, it undermines rational thinking.
Does the new study change my judgment?
I am afraid not!
This recent article is truly remarkable:
There is a faction within the chiropractic profession passionately advocating against the routine use of X-rays in the diagnosis, treatment and management of patients with spinal disorders (aka subluxation). These activists reiterate common false statements such as “there is no evidence” for biomechanical spine assessment by X-ray, “there are no guidelines” supporting routine imaging, and also promulgate the reiterating narrative that “X-rays are dangerous.” These arguments come in the form of recycled allopathic “red flag only” medical guidelines for spine care, opinion pieces and consensus statements. Herein, we review these common arguments and present compelling data refuting such claims. It quickly becomes evident that these statements are false. They are based on cherry-picked medical references and, most importantly, expansive evidence against this narrative continues to be ignored. Factually, there is considerable evidential support for routine use of radiological imaging in chiropractic and manual therapies for 3 main purposes: 1. To assess spinopelvic biomechanical parameters; 2. To screen for relative and absolute contraindications; 3. To reassess a patient’s progress from some forms of spine altering treatments. Finally, and most importantly, we summarize why the long-held notion of carcinogenicity from X-rays is not a valid argument.
Not only is low dose radiation not detrimental, but it also protects us from cancer, according to the authors:
Exposures to low-dose radiation incites multiple and multi-hierarchical biopositive mechanisms that prevent, repair or remove damage caused mostly by endogenous reactive oxygen species (ROS) and H2O2 from aerobic metabolism. Indeed, non-radiogenic (i.e. naturally occurring) molecular damage occurs daily at rates many orders of magnitude greater than the rate of damage caused by low-dose radiation such as diagnostic X-rays. It is estimated that the endogenous genetic damage caused on a daily basis from simply breathing air is about one million times the damage initially resulting from an X-ray. We concur that “it is factually preposterous to have radiophobic cancer concerns from medical X-rays after considering the daily burden of endogenous DNA damage.”
And, of course, radiological imaging makes sense in cases of non-specific back pain due to ‘malalignment’ of the spine:
Pressures to restrict the use of “repeat” (i.e. follow-up) X-rays for assessing patient response to treatment shows a complete disregard for the evidence discussed that definitively illustrates how modern spine rehabilitation techniques and practices successfully re-align the spine and pelvis for a wide variety of presenting subluxation/deformity patterns. The continued anti-X-ray sentiment from “consensus” and opinion within chiropractic needs to stop; it is antithetical to scientific reality and to the practice of contemporary chiropractic practice. We reiterate a quote from the late Michael A. Persinger: “what is happening in recent years is that facts are being defined by consensus. If a group of people think that something is correct, therefore it’s true, and that’s contradictory to science.”
Thus, the authors feel entitled to conclude:
Routine and repeat X-rays in the nonsurgical treatment of patients with spine disorders is an evidence-based clinical practice that is warranted by those that practice spine-altering methods. The evidence supporting such practices is based on definitive evidence supporting the rationale to assess a patient’s spinopelvic parameters for biomechanical diagnosis, to screen for relative and absolute contraindications for specific spine care methods, and to re-assess the spine and postural response to treatment.
The traditional and underlying presumption of the carcinogenicity from X-rays is not a valid notion because the LNT is not valid for low-dose exposures. The ALARA radiation protection principle is obsolete, the threshold for harm is high, low-dose exposures prevent cancers by stimulating and upregulating the body’s innate adaptive protection mechanisms, the TCD concept in invalid, and aged cohort studies assumed to show cancers resulting from previous X-rays are not generalizable to the wider population because they represent populations predisposed to cancers.
Red flags, or suspected serious underlying disease is a valid consideration warranting screening imaging by all spine care providers. We contend, however, that as long as the treating physician or rehabilitation therapist is practicing evidence-based methods, proven to improve spine and postural parameters in order to provide relief for the myriad of spinal disorders, spinal X-rays are unequivocally justified. Non-surgical spine care guidelines need to account for proven and evolving non-surgical methods that are radiographically guided, patient-centered, and competently practiced by those specialty trained in such methods. This is over and above so-called “red flag only” guidelines. The efforts to universally dissuade chiropractors from routine and repeat X-ray imaging is neither scientifically justified nor ethical.
There seems to be just one problem here: the broad consensus is against almost anything these authors claim.
Oh, I almost forgot: this paper was authored and sponsored by CBP NonProfit.
“The mission of Chiropractic BioPhysics® (CBP®) Non-Profit is to provide a research based response to these changing times that is clinically, technically, and philosophically sound. By joining together, we can participate in the redefinition and updating of the chiropractic profession through state of the art spine research efforts. This journey, all of us must take as a Chiropractic health care profession to become the best we can be for the sake of the betterment of patient care. CBP Non-Profit’s efforts focus on corrective Chiropractic care through structural rehabilitation of the spine and posture. Further, CBP Non-Profit, Inc. has in its purpose to fund Chiropractic student scholarships where appropriate as well as donate needed chiropractic equipment to chiropractic colleges; always trying to support chiropractic advancement and education.”
This study aimed to evaluate the effect of Traditional Chinese Medicine (TCM) on patients with gastric cancer following surgery and adjuvant chemotherapy in Taiwan. The cohort sampling data set was obtained from the Registry of Catastrophic Illness Patient Database, a research database of patients with severe illnesses from the National Health Insurance Research Database, Taiwan. Patients who had received a new diagnosis of gastric cancer and had undergone surgery were enrolled. the researchers matched TCM users and nonusers at a ratio of 1 : 3 based on the propensity score, and TCM users were also grouped into short-term and long-term users.
The number of TCM users and nonusers was 1701 and 5103 after applying the propensity score at a ratio of 1 : 3. Short-term users and long-term TCM users were independently associated with a decreased risk of death with HRs of 0.59 (95% confidence interval (CI), 0.55-0.65) and 0.41 (95% CI, 0.36-0.47), respectively, compared with TCM nonusers. The researchers also obtained similar results when they adjusted for covariates in the main model, as well as each of the additional listed covariates. They also observed similar HR trends in short-term users and long-term TCM users among men and women aged <65 years and ≥65 years. The most commonly prescribed single herb and herbal formula in our cohort were Hwang-Chyi (Radix Hedysari; 11.8%) and Xiang-Sha-Liu-Jun-Zi-Tang (15.5%), respectively.

The authors concluded that TCM use was associated with higher survival in patients with gastric cancer after surgery and adjuvant chemotherapy. TCM could be used as a complementary and alternative therapy in patients with gastric cancer after surgery and adjuvant chemotherapy.
This is an interesting study which seems well-done – except for one fatal mistake: even in the title, the authors imply a causal relationship between TCM and survival. Their conclusion has two sentences; the first one speaks correctly of an association. The second, however, not only implies causality but goes much further in suggesting that TCM should be used to prolong the life of patients. Yet, there are, of course, dozens of factors that could interfere with the findings or be the true cause of the observed outcome.
Anyone with a minimum of critical thinking ability should know that CORRELATION IS NOT CAUSATION; sadly, the authors of this study seem to be the exception.
Several previously published clinical trials have suggested that both acupuncture and sham acupuncture exert significant, non-specific effects on treatment outcomes when compared to no-treatment controls. A recently developed framework (mechanisms in orthodox and complementary and alternative medicine-MOCAM) suggests that the non-specific effects of acupuncture originate from multiple domains (e.g. patient characteristics, acupuncturist skill/technique, the patient-acupuncturist relationship, and the acupuncture environment). However, it remains to be determined precisely how these domains influence the non-specific effects of treatment among patients receiving acupuncture and sham acupuncture in clinical trials.
To address this issue, researchers conducted a systematic review to synthesize existing qualitative evidence on how trial participants randomized to acupuncture and sham acupuncture groups experience non-specific effects, regardless of the types of medical conditions investigated.
This systematic review included primary qualitative studies embedded in randomized controlled trials designed to investigate acupuncture or sham acupuncture interventions. Eligible studies published in English were derived from a search of five international databases. The methodological quality of included studies was evaluated using the Critical Appraisal Skills Programme (CASP) tool. Using a framework synthesis approach, the identified MOCAM framework was adapted based on the synthesis of the available qualitative evidence.
A total of 20 studies of high methodological quality were included. The proposed model indicated that the effects of acupuncture may be increased by:
- maintaining a professional status,
- applying a holistic treatment approach,
- practicing empathy,
- providing patients with an appropriate explanation of the theory behind acupuncture and sham acupuncture.
From the patient’s perspective, the efficacy of treatment can be increased by:
- following the lifestyle modification advice provided by acupuncturists,
- maintaining a positive attitude toward treatment efficacy,
- actively engaging with acupuncturists during the consultation,
- making behavioral changes based on experience gained during the trial.
The authors concluded that the results of this study may provide a basis for improving and standardizing key components of non-specific effects in acupuncture treatment, and for improving the isolation of specific effects in future clinical trials involving acupuncture and sham acupuncture.
The authors also state that having a positive attitude and high expectations regarding treatment efficacy can lead to positive health outcomes, along with a sense of curiosity and altruistic desire to join clinical trials. Indeed, previous clinical trials have reported that higher expectations regarding treatment effects may help to reduce fatigue and alleviate osteoarthritis in both acupuncture and sham acupuncture groups. Similar benefits of positive expectations have also been observed among patients with irritable bowel syndrome in sham acupuncture trials.
SO CLOSE AND YET SO FAR!
So close to admitting that these findings indicate quite strongly that acupuncture is but a theatrical placebo.
As we have often discussed, proponents of so-called alternative medicine (SCAM), have an unfortunate tendency to mislead the public about vitamins and other supplements. Consequently, there is much uncertainty in many people’s minds. It is, therefore, all the more important to highlight new information that might counter this phenomenon.
This study tested whether high-dose zinc and/or high-dose ascorbic acid reduce the severity or duration of symptoms compared with usual care among ambulatory patients with SARS-CoV-2 infection. It was designed as a multicenter, single health system randomized clinical factorial open-label trial and enrolled 214 adult patients with a diagnosis of SARS-CoV-2 infection confirmed with a polymerase chain reaction assay who received outpatient care in sites in Ohio and Florida. The trial was conducted from April 27, 2020, to October 14, 2020.
Patients were randomized in a 1:1:1:1 allocation ratio to receive either:
- zinc gluconate (50 mg),
- ascorbic acid (8000 mg),
- both of these agents,
- standard care only.
The treatments lasted 10 days.
The primary endpoint was the number of days required to reach a 50% reduction in symptoms, including the severity of fever, cough, shortness of breath, and fatigue (rated on a 4-point scale for each symptom). Secondary endpoints included days required to reach a total symptom severity score of 0, cumulative severity score at day 5, hospitalizations, deaths, adjunctive prescribed medications, and adverse effects of the study supplements.
A total of 214 patients were randomized, with a mean (SD) age of 45.2 (14.6) years and 132 (61.7%) women. The study was stopped for a low conditional power for benefit with no significant difference among the 4 groups for the primary endpoint. Patients who received usual care without supplementation achieved a 50% reduction in symptoms at a mean (SD) of 6.7 (4.4) days compared with 5.5 (3.7) days for the ascorbic acid group, 5.9 (4.9) days for the zinc gluconate group, and 5.5 (3.4) days for the group receiving both (overall P = .45). There was no significant difference in secondary outcomes among the treatment groups.
The authors concluded that, in this randomized clinical trial of ambulatory patients diagnosed with SARS-CoV-2 infection, treatment with high-dose zinc gluconate, ascorbic acid, or a combination of the 2 supplements did not significantly decrease the duration of symptoms compared with standard of care.
This study has several limitations (and its authors are laudably frank about them):
- Its sample size is small.
- It has no placebo control group.
- It is open-label.
- Patients were not masked to which therapy they received.
The trial nevertheless adds important information about the value of using zinc or vitamin C or both in the management of COVID patients.
Just as I read that the right-wing preacher Lance Wallnau once claimed he had cured Rush Limbaugh of his lung cancer – Limbaugh died yesterday of that cancer – I found this paper in the bizarre journal ‘EXPLORE’ reporting a much more successful (or should I say ‘tall’?) tale of healing by prayer.
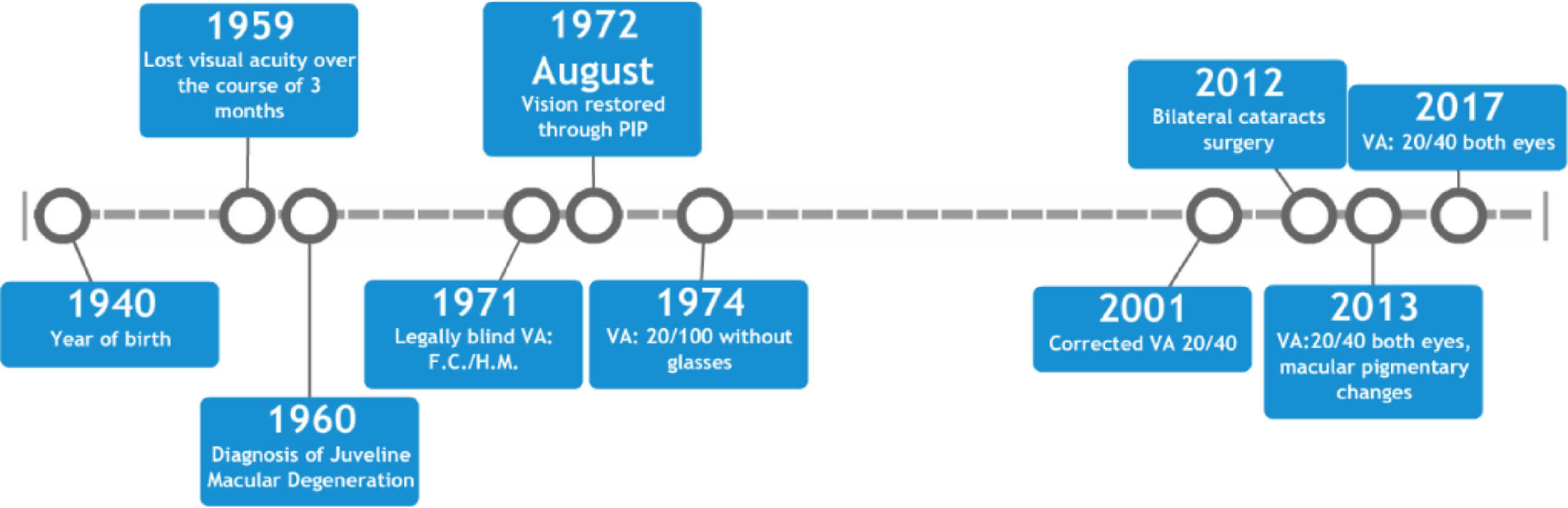
This case report describes an 18-year-old female who lost the majority of her central vision over the course of three months in 1959. Medical records from 1960 indicate visual acuities (VA) of less than 20/400 for both eyes corresponding to legal blindness. On fundus examination of the eye, there were dense yellowish-white areas of atrophy in each fovea and the individual was diagnosed with juvenile macular degeneration (JMD).
In 1971, another examination recorded her uncorrected VA as finger counting on the right and hand motion on the left. She was diagnosed with macular degeneration (MD) and declared legally blind. In 1972, having been blind for over 12 years, the patient reportedly regained her vision instantaneously after receiving proximal-intercessory-prayer (PIP). Subsequent medical records document repeated substantial improvement; including uncorrected VA of 20/100 in each eye in 1974 and corrected VAs of 20/30 to 20/40 were recorded from 2001 to 2017.
To date, her eyesight has remained intact for forty-seven years, according to the authors of this paper.
The course of these events is summarised in the graph below.
And here is what the patients was reported stating:
“What people need to understand is ‘I was blind’, totally blind and attended the School for the Blind. I read Braille and walked with a white cane. Never had I seen my husband or daughters face. I was blind when my husband prayed for me- then just like that- in a moment, after years of darkness I could see perfectly! It was miraculous! My daughter’s picture was on the dresser. I could see what my little girl and husband looked like, I could see the floor, the steps. Within seconds, my life had drastically changed. I could see, I could see!”
This report originates from the GLOBAL MEDICAL RESEARCH INSTITUTE. Their website claims that our mission is to investigate the effects of prayer in the resolution of conditions where the prognosis is typically poor, even with medical intervention. We are also developing randomized, controlled clinical trials of healing prayer effects.
Three questions came to my mind while reading all this:
- Are RCTs in prayer really needed? The believers already ‘know’ and will not trust the findings of the research, if they are not positive.
- Who do they try to convince the public with a case report that dates back 47 years?
- What do they think of Carl Sagan’s bon mot, ‘EXTRAORDINARY CLAIMS REQUIRE EXTRAORDINARY EVIDENCE’?
The drop in cases and deaths due to COVID-19 infections in India has been attributed to India’s national policy of using homeopathy. Early in the epidemic, the national “Ministry of AYUSH, recommended the use of Arsenic album 30 as preventive medicine against COVID-19. Its prophylactic use has been advised in states like Karnataka, Tamil Nadu, Kerala, and Maharashtra. The ‘OFFICIAL HOMEOPATHY RESOURCE’ is now claiming that homeopathy is the cause of the observed outcome:
And now the results of that policy and use are clear, even though skeptics and other scientists in the conventional paradigm are mystified as to why the drop is so dramatic. They know nothing about homeopathy and its history of successfully treating epidemics.
India has a population of 1 billion, 300 million people. Relative to this massive population the number of cases per day and especially the number of deaths per day are now exceptionally low. According to the Daily Mail:
“Scientists are trying to work out why coronavirus cases in India are falling when at one point it looked like the country might overtake the US as the worst-hit nation.
In September the country was reporting some 100,00 new cases per day, but that went into decline in October and is now sitting at around 10,000 per day – leaving experts struggling to explain why.”
END OF QUOTE
According to my sources, the number of daily new cases in India rose steadily to reach its maximum of almost 100000 new cases per day in mid-September. Thereafter, the figure fell in almost the same fashion as they had previously risen.

Currently, they have reached a plateau of about 13000 cases per day, and around 100 patients per day are reported to dies of COVID-19 every day. There are several possible contributors to these relatively positive outcomes:
- India has administered the Covid-19 vaccine to about 10 million people in one month since launching the world’s largest vaccination program on Jan. 16. However, this timing cannot explain the fall of cases before mid-January.
- The Indian government has attributed the dip in cases partly to mask-wearing, which is mandatory in public in India and violations can draw hefty fines.
- Large areas of India have reached herd immunity.
- Some of the various non-homeopathic remedies that have been recommended by the Ministry of AYUSH might be effective.
- There might be a host of other factors that I don’t know about.
- The figures coming out of India may not be reliable.
- The homeopathic remedy Arsenic album 30 might indeed be an effective preventative.
Which of these explanations are valid?
Most likely, it is not one but several working together. However, the hypothesis that homeopathy has anything to do with the course of the pandemic in India seems most unlikely. Apart from the fact that highly diluted homeopathic remedies are implausible and have not been shown to be effective, the timing of events is clearly against this explanation: if I am correctly informed, the homeopathic remedies were dished out months before the decline in cases started. In fact, simply going by the timing, one would need to assume that homeopathy led to the enormous increase before the remarkable drop.
Of course, it would be interesting to see the results of the homeopathy trials that allegedly started in India about 8 months ago. They could bring us closer to the truth. But somehow, I am not holding my breath.