causation
Homeopathy is sometimes claimed to be effective for primary dysmenorrhoea (PD), but the claim is not supported by sound evidence. This study was undertaken to examine the efficacy of individualized homeopathic medicines (IH) against placebo in the treatment of PD.
A double-blind, randomized, placebo-controlled trial was conducted at the gynecology outpatient department of Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, West Bengal, India. Patients were randomized to receive either IH (n=64) or identical-looking placebo (n=64). Primary and secondary outcome measures were 0-10 numeric rating scales (NRS) measuring the intensity of pain of dysmenorrhea and verbal multidimensional scoring system (VMSS) respectively, all measured at baseline, and every month, up to 3 months.
The two groups were comparable at baseline. The attrition rate was 10.9% (IH: 7, placebo: 7). Differences between groups in both pain NRS and VMSS favored IH over placebo at all time points with medium to large effect sizes. Natrum muriaticum and Pulsatilla nigricans were the most frequently prescribed medicines. No harms, serious adverse events, or intercurrent illnesses were recorded in either group.
The authors concluded that homeopathic medicines acted significantly better than placebo in the treatment of PD. Independent replication is warranted.
A previously published RCT could not show any significant effect of homeopathy on primary dysmenorrhea in comparison with placebo. The authors of the new study claim that the discrepant findings might be due to the fact that IH requires great skill. In other words, negative studies are according to this explanation negative not because homeopathy does not work but because the prescribers are not up to it. Such notions have often been voiced on this blog and elsewhere and are used as a veritable ‘get-out clause’ for homeopathy: ONLY THE POSITIVE RESULTS ARE VALID! Consequently, systematic reviews of the evidence must only consider positive trials. And this, of course, means that the findings are invariable positive.
I find this more than a little naive and would much prefer to wait for an independent replication where ‘independent’ means that the trial is run by experts who are not advocates of homeopathy (as in the present trial).
Bach flower remedies were invented in the 1920s by Dr. Edward Bach (1886-1936), a doctor homeopath who had previously worked in the London Homeopathic Hospital. They have since become very popular in Europe and beyond. Bach flower remedies are clearly inspired by homeopathy; however, they are not the same because they do not follow the ‘like cures like’ principle and are they potentized. They are manufactured by placing freshly picked specific flowers or parts of plants in water which is subsequently mixed with alcohol, bottled, and sold. Like most homeopathic remedies, they are highly dilute and thus do not contain therapeutic amounts of the plant printed on the bottle.
The aim of this new randomized, double-blind, placebo-controlled trial was to compare the efficacy of flower therapy for the treatment of anxiety in overweight or obese adults with that of a placebo. The authors examined improvement in sleep patterns, reduction in binge eating, and change in resting heart rate (RHR).
The study included 40 participants in the placebo group and 41 in the intervention group. Participants were of both genders, from 20 to 59 years of age, overweight or obese, with moderate to high anxiety. They were randomized into two groups:
- one group was treated with Bach flower remedies (BFR) (bottles containing 30 mL of 30% hydro-brandy solution with two drops each of Impatiens, White Chestnut, Cherry Plum, Chicory, Crab Apple, and Pine), purchased from Healing® Flower Essences (São Paulo, Brazil)
- the other group was given a placebo (same solution without BFR).
All patients were instructed to orally ingest the solutions by placing four drops directly in the mouth four times a day for 4 weeks.
The primary outcome was anxiety (State-Trait Anxiety Inventory [STAI]). Secondary outcomes were sleep (Pittsburgh Sleep Quality Index [PSQI]), binge eating (Binge Eating Scale [BES]), and RHR (electrocardiogram).
Multivariate analysis showed significant reductions in scores for the following variables in the intervention group when compared with the placebo group: STAI (β = −0.190; p < 0.001), PSQI (β = −0.160; p = 0.027), BES (β = −0.226; p = 0.001), and RHR (β = −0.07; p = 0.003).
The authors concluded that anxiety symptoms, binge eating, and RHRs of the individuals treated with flower therapy decreased, and their sleep patterns improved when compared with those treated with the placebo.
Did the alcohol in the verum preparation had a relaxing effect? No, I was teasing. The amount would have been too small and the effect would have been the same in both groups. But what could have caused the observed outcome? I have to admit that I have no idea.
I read the study several times and could not find a major flaw. Hence it must have been the flower remedy that caused the positive outcome? No, I am teasing again. I find this impossible to imagine. These remedies contain nothing that might explain the results and all previous systematic reviews of all the available trials have all reached a negative conclusion. Before I seriously consider the option that flower remedies are more than placebos, I would like to see an independent replication.
The integration of so-called alternative medicine (SCAM) into cancer care may reduce the adverse effects of anti-neoplastic treatment but also cause new problems and non-adherence to conventional treatment. Therefore, its net benefit is questionable.
The aim of this randomized controlled study was to investigate the impact of integrative open dialogue about SCAM on cancer patients’ health and quality of life (QoL).
Patients undergoing curative or palliative anti-neoplastic treatment were randomly assigned to standard care (SC) plus SCAM or SC alone. A nurse specialist facilitated SCAM in one or two sessions. The primary endpoint was the
frequency of grade 3–4 adverse events (AE) eight weeks after enrollment. Secondary endpoints were the frequency of grade 1–4 AE and patient-reported QoL, psychological distress, perceived information, attitude towards and use of SCAM 12 and 24 weeks after enrollment. Survival was analyzed post-hoc.
Fifty-seven patients were randomized to SCAM and 55 to SC. No significant differences were found in terms of AEs of cancer patients. A trend towards better QoL, improved survival, and a lower level of anxiety was found in the SCAM group.
The authors concluded that integration of SCAM into daily oncology care is feasible. IOD-CAM was not superior to SC in reducing the frequency of grade 3-4 AEs, but it did not compromise patient safety. Implementation of SCAM
may improve the QoL, anxiety, and emotional well-being of the patients by reducing the level of nausea, vomiting and diarrhea. Finally, SCAM potentially improves the patients’ self-care, which contributes to
increased treatment adherence and improved survival.
This is an interesting paper with a very odd conclusion. The positive trends found failed to be statistically significant. Why employ statistics only to ignore them in our interpretation of the findings?
I can well imagine that the integration of effective treatments into cancer care improves the outcome. I have no problem with this at all – except it is not called INTEGRATIVE MEDICINE but EVIDENCE-BASED MEDICINE!!! If we integrate dubious treatments into cancer care, it’s called INTEGRATIVE MEDICINE, and it’s unlikely to do any good.
In my view, this small study showed just one thing:
Integrative medicine does not reduce adverse effects in cancer patients.
Post-traumatic stress disorder (PTSD), previously known as battle fatigue syndrome or shell shock, is a condition that can be triggered by the experience of some frightening event. PTSD can be debilitating leading to the production of feelings of helplessness, intense fear, and horror. Numerous treatments of PTSD exist but few have been shown to be truly effective. A team of Canadian researchers explored the effects of cannabis on PTSD symptoms, quality of life (QOL), and return to work (RTW). Their systematic review also investigated harms such as adverse effects and dropouts due to adverse effects, inefficacy, and all-cause dropout rates.
Their electronic searches located one RCT and 10 observational studies (n = 4672). Risk of bias (RoB) was assessed with the Cochrane risk of bias tool and ROBINS-I. Evidence from the included studies was mainly based on studies with no comparators. Results from unpooled, high RoB studies suggested that cannabis was associated with a reduction in overall PTSD symptoms and improved QOL. Dry mouth, headaches, and psychoactive effects such as agitation and euphoria were the most commonly reported adverse effects. In most studies, cannabis was well tolerated. A small proportion of patients experienced a worsening of PTSD symptoms.
The authors concluded that the evidence in the current study primarily stems from low quality and high RoB observational studies. Further RCTs investigating cannabis effects on PTSD treatment should be conducted with larger sample sizes and explore a broader range of patient-important outcomes.
Various drugs are currently used for the treatment of PTSD including selective serotonin reuptake inhibitors; tricyclic antidepressants (amitriptyline and isocarboxazid); mood stabilizers (Divalproex and lamotrigine); atypical antipsychotics (aripiprazole and quetiapine) but their effectiveness has not been proven. A recent systematic review included 30 RCTs of a range of heterogeneous non-psychological and non-pharmacological interventions. There was emerging evidence for 6 different approaches:
- acupuncture,
- neurofeedback,
- saikokeishikankyoto (a herbal preparation),
- somatic experiencing,
- transcranial magnetic stimulation,
- yoga.
This list makes me wonder: are these treatments, including cannabis, truly promising, or is PTSD one of those conditions for which nearly every treatment works a little because of its placebo effect?
Due to polypharmacy and the rising popularity of so-called alternative medicines (SCAM), oncology patients are particularly at risk of drug-drug interactions (DDI) or herb-drug interactions (HDI). The aims of this study were to assess DDI and HDI in outpatients taking oral anticancer drugs.
All prescribed and non-prescribed medications, including SCAMs, were prospectively collected by hospital pharmacists during a structured interview with the patient. DDI and HDI were analyzed using four interaction software programs: Thériaque®, Drugs.com®, Hédrine, and Memorial Sloan Kettering Cancer Center (MSKCC) database. All detected interactions were characterized by severity, risk, and action mechanism. The need for pharmaceutical intervention to modify drug use was determined on a case-by-case basis.
A total of 294 patients were included, with a mean age of 67 years [55-79]. The median number of chronic drugs per patient was 8 [1-29] and 55% of patients used at least one SCAM. At least 1 interaction was found for 267 patients (90.8%): 263 (89.4%) with DDI, 68 (23.1%) with HDI, and 64 (21.7%) with both DDI and HDI. Only 13% of the DDI were found in Thériaque® and Drugs.com® databases, and 125 (2.5%) were reported with a similar level of risk on both databases. 104 HDI were identified with only 9.5% of the interactions found in both databases. 103 pharmaceutical interventions were performed, involving 61 patients (20.7%).
The authors concluded that potentially clinically relevant drug interactions were frequently identified in this study, showing that several databases and structured screening are required to detect more interactions and optimize medication safety.
These data imply that DDIs are more frequent than HDIs. This does, however, not tell us which are more important. One crucial difference between DDIs and HDIs is that the former are usually known to the oncology team who should thus be able to prevent them or deal with them appropriately; in contrast, HDIs are often not known to the oncology team because many patients fail to disclose the fact that they take herbal remedies. Some forget, some do not think of herbals as medicine, others may be worried about their physician’s reaction.
It follows that firstly, conventional healthcare practitioners should always ask about the usage of herbal remedies, and secondly, they need to be informed about which herbal remedy might interact with which drug. The first can easily be implemented into routine history-taking; the second is more problematic, not least because our knowledge about HDIs is still woefully incomplete. In view of this, it might often be wise to tell patients to stop taking herbal remedies while they are on prescription drugs.
Vertebral artery dissections (VAD) are a rare but important cause of ischemic stroke, especially in younger patients. Many etiologies have been identified, including motor vehicle accidents, cervical fractures, falls, physical exercise, and, as I have often discussed on this blog, cervical chiropractic manipulation. The goal of this study was to investigate the subgroup of patients who suffered a chiropractor-associated injury and determine how their prognosis compared to other-cause VAD.
The researchers, neurosurgeons from Chicago, conducted a retrospective chart review of 310 patients with vertebral artery dissections who presented at their institution between January 2004 and December 2018. Variables included demographic data, event characteristics, treatment, radiographic outcomes, and clinical outcomes measured using the modified Rankin Scale.
Overall, 34 out of our 310 patients suffered a chiropractor-associated injury. These patients tended to be younger (p = 0.01), female (p = 0.003), and have fewer comorbidities (p = 0.005) compared to patients with other-cause VADs. The characteristics of the injuries were similar, but chiropractor-associated injuries appeared to be milder at discharge and at follow-up. A higher proportion of the chiropractor-associated group had injuries in the 0-2 mRS range at discharge and at 3 months (p = 0.05, p = 0.04) and no patients suffered severe long-term neurologic consequences or death (0% vs. 9.8%, p = 0.05). However, when a multivariate binomial regression was performed, these effects dissipated and the only independent predictor of a worse injury at discharge was the presence of a cervical spine fracture (p < 0.001).
The authors concluded that chiropractor-associated injuries are similar to VADs of other causes, and apparent differences in the severity of the injury are likely due to demographic differences between the two populations.
The authors of the present paper are clear: “chiropractic manipulations are a risk factor for vertebral artery dissections.” This fact is further supported by a host of other investigations. For instance, the Canadian Stroke Consortium found that 28% of strokes following cervical artery dissection were preceded by chiropractic neck manipulation. Dziewas et al. obtained a similar rate in patients with vertebral artery dissections. Many chiropractors are in denial; however, this is merely due to their overt conflicts of interest.
My conclusions from the accumulated evidence are this:
Spinal manipulations of the upper spine should not be routinely used for any condition. Patients who nevertheless insist on having them must be made aware of the risks and give informed consent.
I have reported about the risks of chiropractic manipulation many times before. This is not because, as some seem to believe, I have an axe to grind but because the subject is important. This week, another case of stroke after chiropractic manipulation was in the news. Some will surely say that it is alarmist to mention such reports which lack lots of crucial details. Yet, as long as chiropractors do not establish a proper monitoring system where serious adverse effects of spinal manipulation are noted, I think it is important to record even incomplete cases in this fashion.
Barbara Shand is a working mom who lives in Alberta, Canada. She went to see a chiropractor because she had neck pain. “Near the very end of the appointment, the chiropractor asked: ‘Do you want your neck adjusted?’ I said: ‘Sure.’” “As soon as she did it, everything went black,” Shand recalls.
The patient was then rushed to a hospital by ambulance. “When I did open my eyes, I couldn’t focus. It was all blurry, I had massive vertigo, I didn’t know what was up or down,” Shand told the journalist. The diagnosis, Shand explains, was a right vertebral artery dissection, followed by a stroke. Mrs. Sands continues to struggle with coordination and balance.
The Alberta College and Association of Chiropractors acknowledges “there have been reported cases of stroke associated with visits to various healthcare practitioners, including those that provide cervical spine manipulation.” But they claim it is rare. They did not comment on the informed consent which, according to Shand’s description, was more than incomplete.
The fact that the ACAC admits that such events have happened before is laudable and a step in the right direction (some chiropractic organizations don’t even go that far). Yet, their caveat that such cases are rare is problematic. Without a monitoring system, nobody can tell how frequent they are! What we do see is merely the tip of a much bigger iceberg. There have been hundreds of cases like Mrs. Shand. The truth of the matter is this: Chiropractic neck manipulations are not supported by sound evidence of effectiveness for any condition. This means that even rare risks (if they are truly rare) would tilt the risk/benefit balance into the negative.
The conclusion is, I think, to avoid neck manipulations at all costs. Or, as one neurologist once put it:
don’t let the buggars touch your neck!
I have not often seen a paper reporting a small case series with such an impressively long list of authors from so many different institutions:
- Hospital of Lienz, Lienz, Austria.
- WissHom: Scientific Society for Homeopathy, Koethen, Germany; Umbrella Organization for Medical Holistic Medicine, Vienna, Austria; Vienna International Academy for Holistic Medicine (GAMED), Otto Wagner Hospital Vienna, Austria; Professor Emeritus, Medical University of Vienna, Department of Medicine I, Vienna, Austria. Electronic address: [email protected].
- Resident Specialist in Hygiene, Medical Microbiology and Infectious Diseases, Außervillgraten, Austria.
- St Mary’s University, London, UK.
- Umbrella Organization for Medical Holistic Medicine, Vienna, Austria.
- Shaare Zedek Medical Center, The Center for Integrative Complementary Medicine, Jerusalem, Israel.
- Apotheke Zum Weißen Engel – Homeocur, Retz, Austria.
- Reeshabh Homeo Consultancy, Nagpur, India.
- Umbrella Organization for Medical Holistic Medicine, Vienna, Austria; Vienna International Academy for Holistic Medicine (GAMED), Otto Wagner Hospital Vienna, Austria; Chair of Complementary Medicine, Medical Faculty, Sigmund Freud University Vienna, Austria; KLITM: Karl Landsteiner Institute for Traditional Medicine and Medical Anthropology, Vienna, Austria.
- WissHom: Scientific Society for Homeopathy, Koethen, Germany.
In fact, there are 12 authors reporting about 13 patients! But that might be trivial – so, let’s look at the paper itself. The aim of this study was to describe the effect of adjunctive individualized homeopathic treatment delivered to hospitalized patients with confirmed symptomatic SARS-CoV-2 infection.
Thirteen patients with COVID-19 were admitted. The mean age was 73.4 ± 15.0 (SD) years. The treating homeopathic doctor was instructed by the hospital on March 27, 2020, to adjunctively treat all inpatient COVID-19 patients homeopathically. The high potency homeopathic medicinal products were administered orally. Five globules were administered sublingually where they dissolved, three times a day. In ventilated patients in the ICU, medication was administered as a sip from a water beaker or 1 ml three times a day using a syringe. All ventilated patients exhibited dry cough resulting in respiratory failure. They were given Influenzinum, as were the patients at the general inpatient ward.
Twelve patients (92.3%) were speedily discharged without relevant sequelae after 14.4 ± 8.9 days. A single patient admitted in an advanced stage of septic disease died in the hospital. A time-dependent improvement of relevant clinical symptoms was observed in the 12 surviving patients. Six (46.2%) were critically ill and treated in the intensive care unit (ICU). The mean stay at the ICU of the 5 surviving patients was 18.8 ± 6.8 days. In six patients (46.2%) gastrointestinal disorders accompanied COVID-19.
The authors conclude that adjunctive homeopathic treatment may be helpful to treat patients with confirmed COVID-19 even in high-risk patients especially since there is no conventional treatment of COVID-19 available at present.
In the discussion section of the paper, the authors state this: “Given the extreme variability of pathology and clinical manifestations, a single universal preventive homeopathic medicinal product does not seem feasible. Yet homeopathy may have a relevant role to play precisely because of the number and diversity of its homeopathic medicinal products which can be matched with the diversity of the presentations. Patients with mild forms of disease can use homeopathic medicinal products at home using our simple algorithm. As this Case series suggests, adjunctive homeopathic treatment can play a valuable role in more serious presentations. For future pandemics, homeopathy agencies should be prepared by establishing rapid-response teams and efficacious lines of communication.”
There is nothing in this paper that would lead me to conclude that the homeopathic remedies had a positive effect on the natural history of the disease. All this article actually does do is this: it provides a near-perfect insight into the delusional megalomania of some homeopaths. These people are even more dangerous than I had feared.
This systematic review assessed the effects and reliability of sham procedures in manual therapy (MT) trials in the treatment of back pain (BP) in order to provide methodological guidance for clinical trial development.
Different databases were screened up to 20 August 2020. Randomized controlled trials involving adults affected by BP (cervical and lumbar), acute or chronic, were included. Hand contact sham treatment (ST) was compared with different MT (physiotherapy, chiropractic, osteopathy, massage, kinesiology, and reflexology) and to no treatment. Primary outcomes were BP improvement, the success of blinding, and adverse effects (AE). Secondary outcomes were the number of drop-outs. Dichotomous outcomes were analyzed using risk ratio (RR), continuous using mean difference (MD), 95% CIs. The minimal clinically important difference was 30 mm changes in pain score.
A total of 24 trials were included involving 2019 participants. Most of the trials were of chiropractic manipulation. Very low evidence quality suggests clinically insignificant pain improvement in favor of MT compared with ST (MD 3.86, 95% CI 3.29 to 4.43) and no differences between ST and no treatment (MD -5.84, 95% CI -20.46 to 8.78).ST reliability shows a high percentage of correct detection by participants (ranged from 46.7% to 83.5%), spinal manipulation is the most recognized technique. Low quality of evidence suggests that AE and drop-out rates were similar between ST and MT (RR AE=0.84, 95% CI 0.55 to 1.28, RR drop-outs=0.98, 95% CI 0.77 to 1.25). A similar drop-out rate was reported for no treatment (RR=0.82, 95% 0.43 to 1.55).
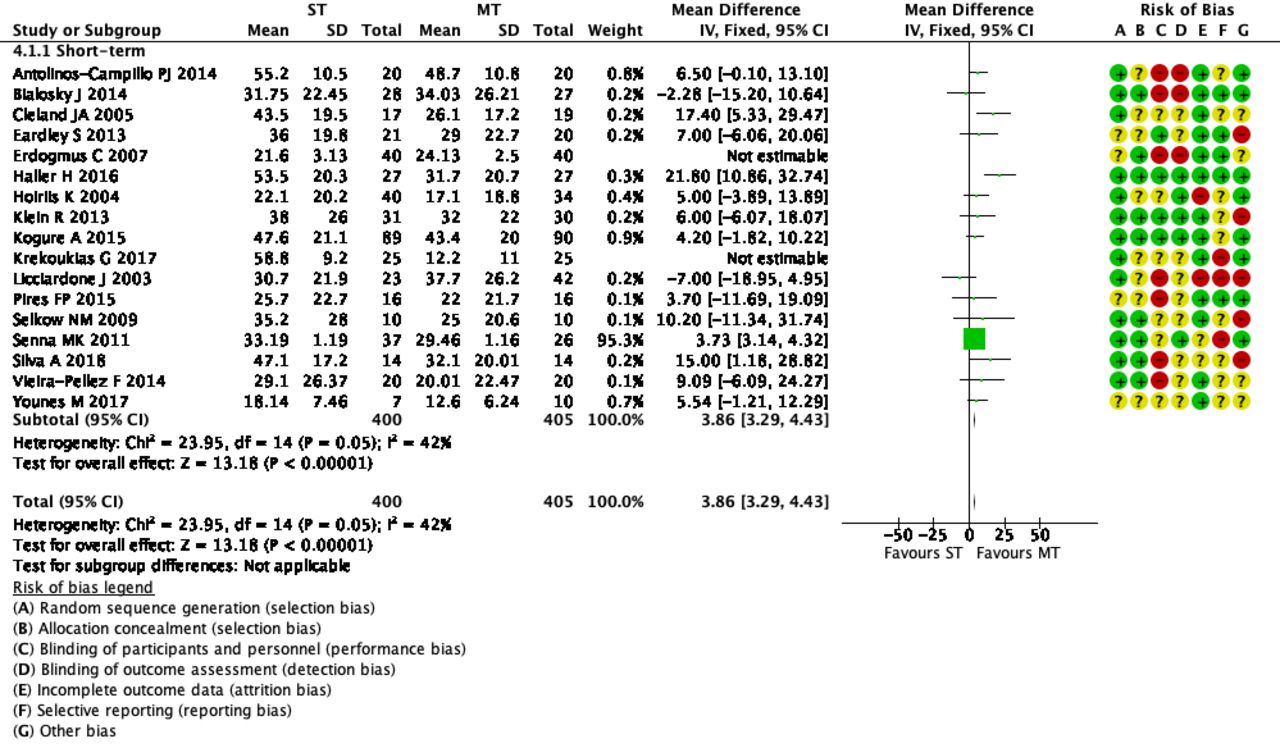 The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
The authors concluded that MT does not seem to have clinically relevant effect compared with ST. Similar effects were found with no treatment. The heterogeneousness of sham MT studies and the very low quality of evidence render uncertain these review findings. Future trials should develop reliable kinds of ST, similar to active treatment, to ensure participant blinding and to guarantee a proper sample size for the reliable detection of clinically meaningful treatment effects.
The optimal therapy for back pain does not exist or has not yet been identified; there are dozens of different approaches but none has been found to be truly and dramatically effective. Manual therapies like chiropractic and osteopathy are often used, and some data suggest that they are as good (or as bad) as most other options. This review confirms what we have discussed many times previously (e.g. here), namely that the small positive effect of MT, or specifically spinal manipulation, is largely due to placebo.
Considering this information, what is the best treatment for back pain sufferers? The answer seems obvious: it is a therapy that is as (in)effective as all the others but causes the least harm or expense. In other words, it is not chiropractic nor osteopathy but exercise.
My conclusion:
avoid therapists who use spinal manipulation for back pain.
The purpose of this study was to describe changes in opioid-therapy prescription rates after a family medicine practice included on-site chiropractic services. It was designed as a retrospective analysis of opioid prescription data. The database included opioid prescriptions written for patients seeking care at the family medicine practice from April 2015 to September 2018. In June 2016, the practice reviewed and changed its opioid medication practices. In April 2017, the practice included on-site chiropractic services. Opiod-therapy use was defined as the average rate of opioid prescriptions overall medical providers at the practice.
There was a significant decrease of 22% in the average monthly rate of opioid prescriptions after the inclusion of chiropractic services (F1,40 = 10.69; P < .05). There was a significant decrease of 32% in the prescribing rate of schedule II opioids after the inclusion of chiropractic services (F2,80 = 6.07 for the Group × Schedule interaction; P < .05). The likelihood of writing schedule II opioid prescriptions decreased by 27% after the inclusion of chiropractic services (odds ratio, 0.73; 95% confidence interval, 0.59-0.90). Changes in opioid medication practices by the medical providers included prescribing a schedule III or IV opioid rather than a schedule II opioid (F6,76 = 29.81; P < .05) and a 30% decrease in the daily doses of opioid prescriptions (odds ratio, 0.70; 95% confidence interval, 0.50-0.98).
The authors concluded that this study demonstrates that there were decreases in opioid-therapy prescribing rates after a family medicine practice included on-site chiropractic services. This suggests that inclusion of chiropractic services may have had a positive effect on prescribing behaviors of medical physicians, as they may have been able to offer their patients additional nonpharmaceutical options for pain management.
The authors are correct in concluding the inclusion of chiropractic services MAY have had a positive effect. And then again, it may not!
Cause and effect cannot be established by correlation alone.
CORRELATION IS NOT CAUSATION!
And even if the inclusion of chiropractic services caused the positive effect, it would not prove that chiropractic is effective in the management of pain. It would only mean that the physicians had an option that helped them to write fewer opioid prescriptions. Had they hired a crystal healer or a homeopath or a faith healer or any other practitioner of an ineffective therapy, the findings might have been very similar.
The long and short of it is this: if we want to use fewer opioids, there is only one way to achieve it: we must prescribe less.
