Monthly Archives: March 2022
Barrie R. Cassileth died on Feb. 26 at an assisted-living home in Beverly Hills, California. I knew about Barrie because she was the 1st author of a most remarkable study published in 1991 in the prestigious NEJM. Here is the abstract:
Background: Cancer treatments without proved efficacy have achieved new levels of popularity, particularly among well-educated patients. The value of these therapies is vigorously debated.
Methods: We compared the length of survival and quality of life in patients who received treatment at a prominent unorthodox cancer clinic in addition to conventional treatment and in matched control patients from an academic cancer center who received only conventional treatment. All the patients had documented extensive malignant disease associated with a predicted median survival time of less than one year. The study sample consisted of 78 pairs of patients matched according to sex, race, age, diagnosis, and time from the diagnosis of metastatic or recurrent disease, who were enrolled over a period of 3 1/2 years. Periodic follow-up (approximately every two months) continued until death.
Results: There was no difference between the two patient groups in length of survival. Median survival for both groups was 15 months (P = 0.22; relative risk, 1.23; 95 percent confidence interval, 0.88 to 1.72). Quality-of-life scores were consistently better among conventionally treated patients from enrollment on.
Conclusions: For this sample of patients with extensive disease and for this particular unorthodox treatment regimen, conventional and unorthodox treatments produced similar results. 
In 1995, I met her for the first time when we both served on an NIH panel, and we kept in contact. When I had flown to Boston for a conference she even drove from New York to see me and have a chat. In 1998, she asked me to come to New York because she needed to discuss something important with me and wanted my advice. It turned out that she had been offered to create the Integrative Medicine Service at Memorial Sloan Kettering Cancer Center in New York sponsored by Laurance Rockefeller. She was very much in two minds about accepting. Her fear was that she would have to become an advocate of alternative medicine. I tried to reassure her and pointed out that I did not exactly turn into an advocate after accepting the Exeter post.
In the end, she accepted and, in the years that followed, we met several times at conferences, became friends, and published a few papers together. I even persuaded her to come to one of our annual conferences at Exeter as a keynote speaker. By then, she had clearly become an advocate of complementary medicine.
What had happened?
Barrie was very keen to differentiate alternative from complementary therapies in cancer care. The former she sharply condemned, while advocating the latter for improving the quality of life of cancer patients. When we discussed these issues, I argued that the ‘alternative versus complementary’ was a somewhat artificial division and that the overlap was large. I also pointed out that some of the complementary treatments she was backing were not based on good evidence. In other words, our views had begun to differ. We remained friends but gradually drifted apart and eventually lost contact.
Barrie Joyce Rabinowitz was born on April 22, 1938, in Philadelphia. She attended Bennington College in Vermont and spent a summer teaching art in Pownal, Massachusetts. She graduated with a degree in social sciences in 1959, a year after marrying Peter Cassileth. Barrie received a master’s degree in psychology from Albert Einstein University and a Ph.D. in medical sociology in 1978 from the University of Pennsylvania, where Peter Cassileth was an oncologist. As part of her doctoral program, Barrie worked closely with adult leukemia patients. After being hired at Pennsylvania as an assistant professor, she helped establish one of the first palliative cancer care programs in the US. Before accepting the post at Slone-Kettering, she taught at Duke, Harvard, and the University of North Carolina. In 2003, she became the founding president of the Society for Integrative Oncology.
While at Slone-Kettering, Barrie published several excellent books and high-quality studies of complementary medicine. She kept on working well after the normal retirement age. Her last RCT was only published in 2018. Here is the abstract:
Purpose: Approximately 20% of breast cancer survivors develop breast cancer-related lymphedema (BCRL), and current therapies are limited. We compared acupuncture (AC) to usual care wait-list control (WL) for treatment of persistent BCRL.
Methods: Women with moderate BCRL lasting greater than six months were randomized to AC or WL. AC included twice weekly manual acupuncture over six weeks. We evaluated the difference in circumference and bioimpedance between affected and unaffected arms. Responders were defined as having a decrease in arm circumference difference greater than 30% from baseline. We used analysis of covariance for circumference and bioimpedance measurements and Fisher’s exact to determine the proportion of responders.
Results: Among 82 patients, 73 (89%) were evaluable for the primary endpoint (36 in AC, 37 in WL). 79 (96%) patients received lymphedema treatment before enrolling in our study; 67 (82%) underwent ongoing treatment during the trial. We found no significant difference between groups for arm circumference difference (0.38 cm greater reduction in AC vs. WL, 95% CI – 0.12 to 0.89, p = 0.14) or bioimpedance difference (1.06 greater reduction in AC vs. WL, 95% CI – 5.72 to 7.85, p = 0.8). There was also no difference in the proportion of responders: 17% AC versus 11% WL (6% difference, 95% CI – 10 to 22%, p = 0.5). No severe adverse events were reported.
Conclusions: Our acupuncture protocol appeared to be safe and well tolerated. However, it did not significantly reduce BCRL in pretreated patients receiving concurrent lymphedema treatment. This regimen does not improve upon conventional lymphedema treatment for breast cancer survivors with persistent BCRL.
Her contribution to our knowledge about complementary therapies is outstanding, and I am sure that her papers will be cited for decades to come. She will be missed and remembered as an innovator in the field of palliative cancer care.
Barrie had been married three times. Her third husband, Richard Cooper, who was the Director of the Center for the Future of the Healthcare Workforce and a Senior Fellow in the Leonard Davis Institute of Health Economics at the University of Pennsylvania, died in 2016. Barrie is survived by her siblings, Stephen and Ruth Rabinowitz; her daughters, Jodi Cassileth Greenspan and Wendy Cassileth; her son, Gregory Cassileth; and 6 grandchildren.
You haven’t heard of religious/spiritual singing and movement as a treatment for mental health?
Me neither!
But it does exist. This review explored the evidence of religious/spiritual (R/S) singing and R/S movement (dynamic meditation and praise dance), in relation to mental health outcomes.
After registering with PROSPERO (CRD42020189495), a systematic search of three major databases (CINAHL, MEDLINE, and PsycINFO) was undertaken using predetermined eligibility criteria. Reference lists of identified papers and additional sources such as Google Scholar were searched. The quality of studies was assessed using the Mixed Method Appraisal Tool (MMAT). Data were extracted, tabulated, and synthesized according to the Preferred Reporting Items for Systematic Reviews (PRISMA) guidelines.
Seven of the 259 identified articles met inclusion criteria. Three studies considered R/S singing, while four considered R/S movement. In R/S movements, three studies considered dynamic meditation while one investigated praise dance. Although moderate to poor in quality, included studies indicated a positive trend for the effectiveness of R/S singing and movement in dealing with mental health concerns.
The authors concluded that, while R/S singing and R/S movement (praise dance and dynamic meditation) may be of value as mental health strategies, findings of the review need to be considered with caution due to methodological constraints. The limited number and poor quality of included studies highlight the need for further quality research in these R/S practices in mental health.
I am glad the authors caution us not to take their findings seriously. To be honest, I was not in danger of making this mistake. Neither do I feel the need for further research in this area. Mental health is a serious issue, and personally, I think we should research it not by conducting ridiculous studies of implausible modalities.
PS
I do not doubt that the experience of singing or movement can help in certain situations. However, I have my doubts about religious/spiritual singing and movement therapy.
Yes, Today is ‘WORLD SLEEP DAY‘ and you are probably in bed hoping this post will put you back to sleep.
This study aimed to synthesise the best available evidence on the safety and efficacy of using moxibustion and/or acupuncture to manage cancer-related insomnia (CRI).
The PRISMA framework guided the review. Nine databases were searched from its inception to July 2020, published in English or Chinese. Randomised clinical trials (RCTs) of moxibustion and or acupuncture for the treatment of CRI were selected for inclusion. The methodological quality was assessed using the method suggested by the Cochrane collaboration. The Cochrane Review Manager was used to conduct a meta-analysis.
Fourteen RCTs met the eligibility criteria; 7 came from China. Twelve RCTs used the Pittsburgh Sleep Quality Index (PSQI) score as continuous data and a meta-analysis showed positive effects of moxibustion and or acupuncture (n = 997, mean difference (MD) = -1.84, 95% confidence interval (CI) = -2.75 to -0.94, p < 0.01). Five RCTs using continuous data and a meta-analysis in these studies also showed significant difference between two groups (n = 358, risk ratio (RR) = 0.45, 95% CI = 0.26-0.80, I 2 = 39%).
The authors concluded that the meta-analyses demonstrated that moxibustion and or acupuncture showed a positive effect in managing CRI. Such modalities could be considered an add-on option in the current CRI management regimen.
Even at the risk of endangering your sleep, I disagree with this conclusion. Here are some of my reasons:
- Chinese acupuncture trials invariably are positive which means they are as reliable as a 4£ note.
- Most trials were of poor methodological quality.
- Only one made an attempt to control for placebo effects.
- Many followed the A+B versus B design which invariably produces (false-) positive results.
- Only 4 out of 14 studies mentioned adverse events which means that 10 violated research ethics.
Sorry to have disturbed your sleep!
This review assessed the magnitude of reporting bias in trials assessing homeopathic treatments and its impact on evidence syntheses.
A cross-sectional study and meta-analysis. Two persons independently searched Clinicaltrials.gov, the EU Clinical Trials Register and the International Clinical Trials Registry Platform up to April 2019 to identify registered homeopathy trials. To determine whether registered trials were published and to detect published but unregistered trials, two persons independently searched PubMed, Allied and Complementary Medicine Database, Embase and Google Scholar up to April 2021. For meta-analyses, the authors used random effects models to determine the impact of unregistered studies on meta-analytic results.
The investigators reported the proportion of registered but unpublished trials and the proportion of published but unregistered trials. They also assessed whether primary outcomes were consistent between registration and publication
Since 2002, almost 38% of registered homeopathy trials have remained unpublished, and 53% of published randomised controlled trials (RCTs) have not been registered. Retrospective registration was more common than prospective registration. Furthermore, 25% of primary outcomes were altered or changed compared with the registry. Although we could detect a statistically significant trend toward an increase of registrations of homeopathy trials (p=0.001), almost 30% of RCTs published during the past 5 years had not been registered.
A meta-analysis stratified by registration status of RCTs revealed substantially larger treatment effects of unregistered RCTs (SMD: −0.53, 95% CI −0.87 to −0.20) than registered RCTs (SMD: −0.14, 95% CI −0.35 to 0.07).
The authors concluded that registration of published trials was infrequent, many registered trials were not published and primary outcomes were often altered or changed. This likely affects the validity of the body of evidence of homeopathic literature and may overestimate the true treatment effect of homeopathic remedies.
An obvious investigation to do (why did I not have this idea?)!
And a finding that will surprise few (except fans of homeopathy who will, of course, dispute it).
The authors also mention that reporting biases are likely to have a substantial impact on the estimated treatment effect of homeopathy. Using data from a highly cited meta-analysis of homeopathy RCTs, our example showed that unregistered trials yielded substantially larger treatment effects than registered trials. They also caution that, because of the reporting biases identified in their analysis, effect estimates of meta-analyses of homeopathy trials might substantially overestimate the true treatment effect of homeopathic remedies and need to be interpreted cautiously.
In other words, the few reviews suggesting that homeopathy works beyond placebo (and are thus celebrated by homeopaths) are most likely false-positive. And the many reviews showing that homeopathy does not work would demonstrate this fact even clearer if the reporting bias had been accounted for.
Or, to put it bluntly:
The body of evidence on homeopathy is rotten to the core and therefore not reliable.
Plantar fasciitis (PF) is a chronic degenerative condition causing marked thickening and fibrosis of the plantar fascia, and collagen necrosis, chondroid metaplasia and calcification. There is little convincing evidence in support of various approaches, including homeopathy, for treating PF. This study was undertaken to examine the efficacy of individualized homeopathic medicines (IHMs) compared with placebo in the treatment of PF.
This double-blind, randomized, placebo-controlled trial was conducted at the outpatient departments of Mahesh Bhattacharyya Homoeopathic Medical College and Hospital, West Bengal, India. Patients were randomized to receive either IHMs or identical-looking placebo in the mutual context of conservative non-medicinal management. The Foot Function Index (FFI) questionnaire, as an outcome measure, was administered at baseline, and every month, up to 3 months. Group differences (unpaired t-tests) and effect sizes (Cohen’s d) were calculated on an intention-to-treat sample. The sample was analyzed statistically after adjusting for baseline differences.
The target sample size was 128; however, only 75 could be enrolled (IHMs: 37; Placebo: 38). Attrition rate was 9.3% (IHMs: 4, Placebo: 3). Differences between groups in total FFI% score favored IHMs against placebo at all the time points, with large effect sizes: month 1 (mean difference, -10.0; 95% confidence interval [CI], -15.7 to -4.2; p = 0.001; d = 0.8); month 2 (mean difference, -14.3; 95% CI, -20.4 to -8.2; p <0.001; d = 1.1); and month 3 (mean difference, -23.3; 95% CI, -30.5 to -16.2; p <0.001; d = 1.5). Similar significant results were also observed on three FFI sub-scales (pain%, disability%, and activity limitation%). Natrum muriaticum (n = 14; 18.7%) and Rhus toxicodendron and Ruta graveolens (n = 11 each; 14.7%) were the most frequently prescribed medicines. No harms, serious adverse events, or intercurrent illnesses were recorded in either of the groups.
The authors concluded that IHMs acted significantly better than placebo in the treatment of PF; however, the trial being underpowered, the results should be interpreted as preliminary only. Independent replications are warranted.
It is nice to see homeopaths stress the importance of independent replication. It is less nice, however, to note their main conclusion:
IHMs acted significantly better than placebo.
This essentially is what will stick in the minds of the pro-homeopathy reader, and this is the information that will enter into future meta-analyses and systematic reviews of homeopathy. But this is also untrue! The qualifier that follows is but a lame excuse for drawing a wrong conclusion. In my view, a correct conclusion would read something like this:
Our study failed to recruit a sufficient number of patients. Therefore, no conclusions about the efficacy of IHM can be drawn from it.
Vaccine hesitancy is currently recognized by the WHO as a major threat to global health. During the COVID-19 pandemic, there has been a growing interest in the role of social media in the propagation of false information and fringe narratives regarding vaccination. Using a sample of approximately 60 billion tweets, Danish investigators conducted a large-scale analysis of the vaccine discourse on Twitter. They used methods from deep learning and transfer learning to estimate the vaccine sentiments expressed in tweets, then categorize individual-level user attitudes towards vaccines. Drawing on an interaction graph representing mutual interactions between users, They analyzed the interplay between vaccine stances, interaction network, and the information sources shared by users in vaccine-related contexts.
The results show that strongly anti-vaccine users frequently share content from sources of a commercial nature; typically sources that sell alternative health products for profit. An interesting aspect of this finding is that concerns regarding commercial conflicts of interests are often cited as one of the major factors in vaccine hesitancy.
The authors furthermore demonstrate that the debate is highly polarized, in the sense that users with similar stances on vaccination interact preferentially with one another. Extending this insight, the authors provide evidence of an epistemic echo chamber effect, where users are exposed to highly dissimilar sources of vaccine information, enforcing the vaccination stance of their contacts.
The authors concluded that their findings highlight the importance of understanding and addressing vaccine mis- and disinformation in the context in which they are disseminated in social networks.
In the article, the authors comment that their findings paint a picture of the vaccine discourse on Twitter as highly polarized, where users who express similar sentiments regarding vaccinations are more likely to interact with one another, and tend to share contents from similar sources. Focusing on users whose vaccination stances are the positive and negative extremes of the spectrum, we observe relatively disjoint ‘epistemic echo chambers’ which imply that members of the two groups of users rarely interact, and in which users experience highly dissimilar ‘information landscapes’ depending on their stance. Finally, we find that strongly anti-vaccine users much more frequently share information from actors with a vested commercial interest in promoting medical misinformation.
One implication of these findings is that online (medical) misinformation may present an even greater problem than previously thought, because beliefs and behaviors in tightly knit, internally homogeneous communities are more resilient, and provide fertile ground for fringe narratives, while mainstream information is attenuated. Furthermore, such polarization of communities may become self-perpetuating, because individuals avoid those not sharing their views, or because exposure to mainstream information might further entrench fringe viewpoints.
- COVID vaccinations are not 100% harmless but they generate much more good than harm.
- They are certainly far less dangerous than the disease.
- COVID infections are not ‘just a flu’ but have serious consequences.
The last point was well-documented in a recent Lancet paper. Here is its abstract in full
Mortality statistics are fundamental to public health decision making. Mortality varies by time and location, and its measurement is affected by well known biases that have been exacerbated during the COVID-19 pandemic. This paper aims to estimate excess mortality from the COVID-19 pandemic in 191 countries and territories, and 252 subnational units for selected countries, from Jan 1, 2020, to Dec 31, 2021.
Methods
All-cause mortality reports were collected for 74 countries and territories and 266 subnational locations (including 31 locations in low-income and middle-income countries) that had reported either weekly or monthly deaths from all causes during the pandemic in 2020 and 2021, and for up to 11 year previously. In addition, we obtained excess mortality data for 12 states in India. Excess mortality over time was calculated as observed mortality, after excluding data from periods affected by late registration and anomalies such as heat waves, minus expected mortality. Six models were used to estimate expected mortality; final estimates of expected mortality were based on an ensemble of these models. Ensemble weights were based on root mean squared errors derived from an out-of-sample predictive validity test. As mortality records are incomplete worldwide, we built a statistical model that predicted the excess mortality rate for locations and periods where all-cause mortality data were not available. We used least absolute shrinkage and selection operator (LASSO) regression as a variable selection mechanism and selected 15 covariates, including both covariates pertaining to the COVID-19 pandemic, such as seroprevalence, and to background population health metrics, such as the Healthcare Access and Quality Index, with direction of effects on excess mortality concordant with a meta-analysis by the US Centers for Disease Control and Prevention. With the selected best model, we ran a prediction process using 100 draws for each covariate and 100 draws of estimated coefficients and residuals, estimated from the regressions run at the draw level using draw-level input data on both excess mortality and covariates. Mean values and 95% uncertainty intervals were then generated at national, regional, and global levels. Out-of-sample predictive validity testing was done on the basis of our final model specification.
Findings
Although reported COVID-19 deaths between Jan 1, 2020, and Dec 31, 2021, totalled 5·94 million worldwide, we estimate that 18·2 million (95% uncertainty interval 17·1–19·6) people died worldwide because of the COVID-19 pandemic (as measured by excess mortality) over that period. The global all-age rate of excess mortality due to the COVID-19 pandemic was 120·3 deaths (113·1–129·3) per 100 000 of the population, and excess mortality rate exceeded 300 deaths per 100 000 of the population in 21 countries. The number of excess deaths due to COVID-19 was largest in the regions of south Asia, north Africa and the Middle East, and eastern Europe. At the country level, the highest numbers of cumulative excess deaths due to COVID-19 were estimated in India (4·07 million [3·71–4·36]), the USA (1·13 million [1·08–1·18]), Russia (1·07 million [1·06–1·08]), Mexico (798 000 [741 000–867 000]), Brazil (792 000 [730 000–847 000]), Indonesia (736 000 [594 000–955 000]), and Pakistan (664 000 [498 000–847 000]). Among these countries, the excess mortality rate was highest in Russia (374·6 deaths [369·7–378·4] per 100 000) and Mexico (325·1 [301·6–353·3] per 100 000), and was similar in Brazil (186·9 [172·2–199·8] per 100 000) and the USA (179·3 [170·7–187·5] per 100 000).
Interpretation
The full impact of the pandemic has been much greater than what is indicated by reported deaths due to COVID-19 alone. Strengthening death registration systems around the world, long understood to be crucial to global public health strategy, is necessary for improved monitoring of this pandemic and future pandemics. In addition, further research is warranted to help distinguish the proportion of excess mortality that was directly caused by SARS-CoV-2 infection and the changes in causes of death as an indirect consequence of the pandemic.
I am posting this in the hope that the many proponents of so-called alternative medicine (SCAM) who deny proven facts about COVID might learn and stop falling victim to proctophasia.
The associations between so-called alternative medicine (SCAM) and negative attitudes to vaccinations are, as discussed repeatedly on this blog, strong and undeniable. A new paper sheds more light on these issues.
By far the most common strategy used in the attempt to modify negative attitudes toward vaccination is to appeal to evidence-based reasoning. However, focusing on science comprehension is inconsistent with one of the key facts of cognitive psychology: Humans are biased information processors and often engage in motivated reasoning. On this basis, it is hypothesized that negative attitudes can be explained primarily by factors unrelated to the empirical evidence for vaccination; including some shared attitudes that also attract people to SCAM.
This study tested psychosocial factors associated with SCAM endorsement in past research; including aspects of spirituality, intuitive (vs analytic) thinking styles, and the personality trait of openness to experience. These relationships were tested in a cross-sectional, stratified CATI survey (N = 1256, 624 Females).
Questions regarding SCAM were derived from a previously validated instrument, designed to standardize the measurement of SCAM utilization, and distinguish between those that use a particular SCAM from those that do not. Each SCAM item provided an indication of whether the respondent had utilized each of the following therapeutic or self-treatment activities within the last 12 months:
- herbal and homeopathic remedies,
- energy-based and body therapies (including therapeutic massage),
- vitamins, yoga, meditation, prayer, body therapies, hypnosis, spiritual healing,
- and chiropractic or osteopathic treatments.
The results show that educational level and thinking style did not predict vaccination rejection. Psychosocial factors such as
- preferring SCAM to conventional medicine (OR .49, 95% CI .36-.66),
- endorsement of spirituality as a source of knowledge (OR .83, 95% CI .71-.96),
- openness (OR .86, 95% CI .74-.99),
all predicted negative attitudes to vaccination. Furthermore, for 9 of the 12 SCAMs surveyed, utilisation in the last 12 months was associated with lower levels of vaccination endorsement. Additionally, the rank-order correlation between the number of different alternative therapies used in the last 12 months and vaccination attitude score was significant. Finally, analytical thinking style was negatively related to all forms of CAM, with this relationship significant in three cases:
- herbal remedies ρ = −.08, p = .0014,
- homeopathy, ρ = −.06, p = .0236,
- prayer for the purpose of healing, ρ = −.15, p < .0001.
The authors concluded that vaccination scepticism appears to be the outcome of a particular cultural and psychological orientation leading to unwillingness to engage with the scientific evidence. Vaccination compliance might be increased either by building general confidence and understanding of evidence-based medicine, or by appealing to features usually associated with SCAM, e.g. ‘strengthening your natural resistance to disease’.
In the discussion section of their paper, the authors argue that these results describe a vaccine sceptic as viewing themselves as anti-authoritarian and unconventional, with a preference for unorthodox treatments with spiritual or ‘life-affirming’ features. The significant effect for personality, but not for cognitive style, is congruent with the notion that it is a reluctance to engage with the evidence, rather than a lack of capacity to appropriately process the evidence, that predicts vaccination scepticism…
SCAM endorsement and vaccination scepticism are components of a common attitudinal stance, with some shared psychosocial determinants. The results of the present study indicate that vaccination rejection is related to psychosocial factors: a general preference for complementary over conventional medicines, valuing diverse and unconventional alternatives, and a spiritual orientation to attitude formation. The null findings with regard to cognitive style and educational level suggest that factors unrelated to the actual empirical evidence for vaccination – i.e. a particular personality and attitudinal mindset are most instrumental in determining vaccination attitudes. Efforts to counter vaccination concerns should be mindful that negative vaccination views appear to form part of a broader attitudinal system that does not necessarily trust empirical or positivist evidence from authoritative sources. Vaccination promotion efforts may benefit from targeting groups associated with SCAM and building general confidence in scientific medicine, rather than targeting specific misunderstandings regarding vaccination.
The present study investigated the impact of a purposefully designed Islamic religion-based intervention on reducing depression and anxiety disorders among Muslim patients using a randomised controlled trial design. A total of 62 Muslim patients (30 women and 32 men) were divided by gender into two groups, with each group assigned randomly to either treatment or control groups. The participants who received the Islamic-based intervention were compared to participants who received the control intervention.
The Islamic-Based Intervention that was applied to the two experimental groups (i.e. one male, one female) has several components. These components were based on moral and religious concepts and methods, including moral confession, repentance, insight, learning, supplication, seeking Allah’s mercy, seeking forgiveness, remembrance of Allah, patience, trust in Allah, self-consciousness, piety, spiritual values, and moral principles. The techniques implemented in the intervention included the art of asking questions, clarifying, listening, interacting, summarising, persuading, feedback, empathy, training practice, reflecting feelings, discussion, and dialogue, lecturing, brainstorming, reinforcement, modeling, positive self-talk, evaluation, homework, practical applications, activation games (play through activities), emotional venting, stories, presentation, correction of thoughts, and relaxation. The two control groups (i.e. one male, one female) received the energy path program provided by the Al-Nour Centre. This program aimed to enhance self-confidence and modify people’s behavior with anxiety disorders, depression, and obsessive-compulsive disorder. Both interventions comprised 30 sessions over 30 h; two sessions were conducted per week, and each session lasted for 60 min (one hour). The duration of the intervention was 15 weeks.
Taylor’s manifest anxiety scale and Steer and Beck’s depression scale were used for examining the effects on depression and anxiety levels. The results revealed that the Islamic intervention significantly reduced anxiety levels in women and depression levels in men compared to the typical care control groups.
The authors concluded that religious intervention played a vital role in lowering the patients’ level of anxiety among women and depression among men. In general, religious practices prevent individuals from becoming subject to mental disorders, i.e. anxiety and depression.
The authors comment that the Islamic religion-based intervention (RSAFI) significantly reduced the levels of depression and anxiety among the participants. Also, there was a substantial improvement in the patients’ general health after the intervention. They were satisfied and believed that everything happening to them was destined by Allah. These results could be attributed to the different intervention practices that relied on the guidance of the Holy Quran and Sunnah. For instance, Saged et al. (2020) confirmed that the Holy Quran significantly impacts healing patients who suffer from physical, psychological, and mental disorders. In this respect, Moodley et al. (2018) concluded that having faith in Allah offers a relatively quick approach to healing patients suffering from heartache and depression. This goes hand in hand because the recitation of the Quran and remembrance of Allah help patients feel relaxed and peaceful. Muslims believe that the Quran is the word of Allah and that Allah’s words exert a significant impact on the healing of mental health patients, as, ultimately, Almighty Allah is the one who cures illnesses.
When discussing the limitations of their study, the authors state that the sample of this study was limited to the patients with anxiety and depression disorders at the Al-Nour Centre in Kuala Lumpur, so the results cannot be generalized to other samples. Furthermore, the treatment of anxiety was restricted to females, whereas the treatment of depression was restricted to males. Additionally, the selection of females and males as samples for the study was based on their pre-measurement of anxiety and depression, which serve as self-report measures.
The authors seem to be unconcerned about the fact that the 2 interventions (verum and control) were clearly distinguishable and their patients thus were not blinded (and neither were the evaluators). This obviously means that the observed effect might have nothing at all to do with the Islamic-Based Intervention but could be entirely due to expectation and persuasion.
Why might the authors not even bother to discuss such an obvious possibility?
A look at their affiliations might provide the answer:
- 1Academy of Islamic Studies, University of Malaya, 50603, Kuala Lumpur, Malaysia. [email protected].
- 2Academy of Islamic Studies, University of Malaya, 50603, Kuala Lumpur, Malaysia.
- 3Faculty of Education, Universiti Teknologi Malaysia, Johor, Malaysia.
- 4Faculty of Education, University of Malaya, 50603, Kuala Lumpur, Malaysia.
- 5Islamic Banking and Finance, International Islamic University Malaysia, Selangor, Malaysia.
- 6Department of Hadith and Associated Sciences, Nourah Bint Abdulrahman University, Riyadh, Saudi Arabia.
Yes, the fear of nuclear radiation has gripped the minds of many consumers. And who would blame them? We are all frightened of Putin’s next move. There is plenty of uncertainty. But, let me assure you, there is one certainty:
Homeopathy does not help against the effects of nuclear radiation.
But this indisputable fact has never stopped a homeopath.
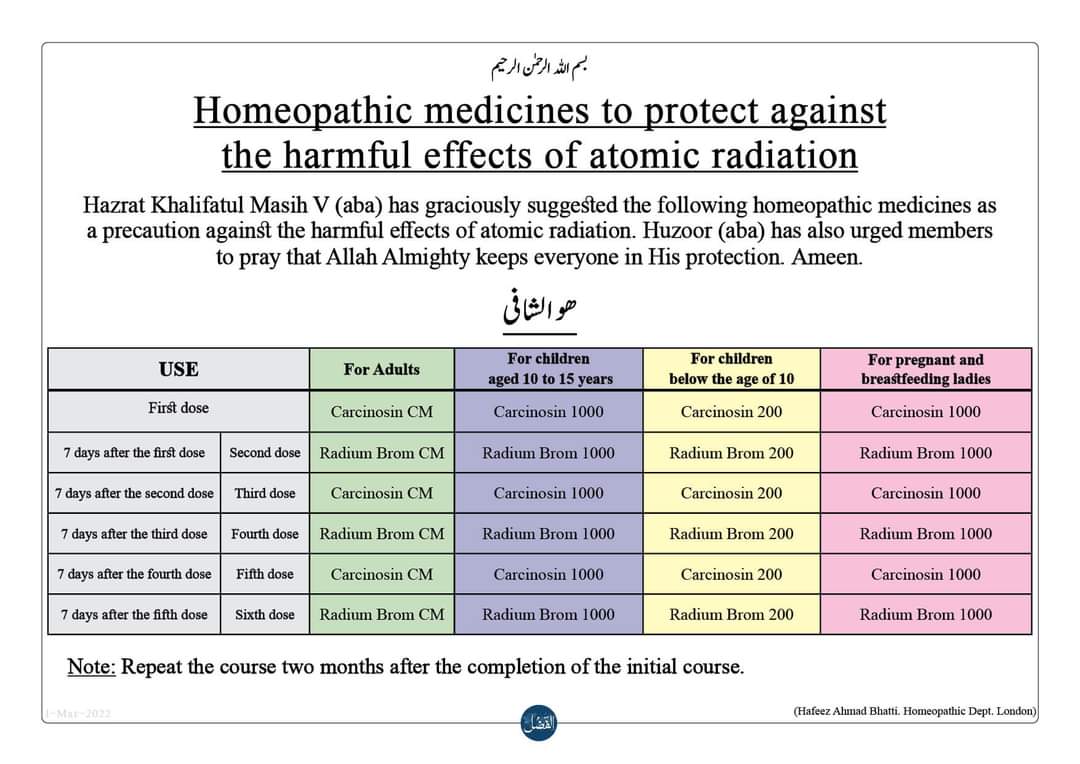
Many of them are currently trying to persuade us that homeopathy can protect us. Here, for example, is something I found on Twitter:
But there is more, much more. If you go on the Internet, you find dozens of websites making wild claims. Here is just one example:
Homeopathic remedies as a preventive for adults
To be taken on an annual or bi-annual basis:
Week 1: Carcinosin in CM potency
Week 2: Radium Bromide in CM potency
Week 3: Carcinosin in CM potency
Week 4: Radium Bromide in CM potency
Week 5: Carcinosin in CM potency
Week 6: Radium Bromide in CM potency
Homeopathic remedies as a preventive for children (13 years old)
100
To be taken on an annual or bi-annual basis:
Week 1: Carcinosin in 1000 potency
Week 2: Radium Bromide in 1000 potency
Week 3: Carcinosin in 1000 potency
Week 4: Radium Bromide in 1000 potency
Week 5: Carcinosin in 1000 potency
Week 6: Radium Bromide in 1000 potency.
___________________________
Ridiculous? YES
Irresponsible? YES
Dangerous? YES