Monthly Archives: February 2022
Now that the first reviews of, and numerous comments on my new book are in, I thought I bring my readers up to date and perhaps contribute to some fun. My favorite quote comes from a comment on Harriett Hall’s review: “Nothing much new here about Chucky Windsor’s credulity…”
Perhaps I shouldn’t, but I think it is funny and thus I chose it as the title of this post. Apart from being funny, it also has a more serious background. Virtually everyone who contacted me and gave me feedback said that they knew about Charles’ advocacy of alternative medicine. So, the ‘nothing much new’ comment is apt. Yet, they all added that, before reading my book, they had no idea how deeply Charles was involved and how profoundly anti-scientific and irrational his thinking seems to be in this area. Jonathan Stea, for instance, tweeted: “I just finished reading it—review coming soon. Excellent book. I didn’t realize Prince Charles was so stubbornly in love with pseudoscience and trying to promote it for decades under the guise of alternative/integrative medicine.”
Another comment was made on my own blog: “I am an avid consumer of this and other science blogs, books, podcasts and any other media I encounter. One of my earliest exposures was your book Trick or Treat, which I credit with greatly expanding my knowledge of a subject I had dabbled in but had begun to question. I deplore the PoW’s promotion of quackery. I am American and have no dog in the value of Royalty debate. BUT, I don’t see the need to use such a deeply unflattering (and possibly photoshopped) photo of the PoW. I do not think that such a decision is in line with your list of “nots”, and I think it hinders the impact it might otherwise have on fence-sitters. It disappoints me and while I have purchased multiple copies of many of your books to pass on to friends, family, and believers, I will pass on this one.” The photo is perhaps not flattering but there a many out there that are even worse. In any case, it is the publisher who decides on the title page. In the present case, I merely asked them to make my name on the title page a little less prominent than it was on the draft.
And then there were people who emailed me directly, as this medical colleague:
Dear Dr Ernst,
as a GP and ex oral surgeon from a world famous medical school(Edinburgh), also an experienced alternative practitioner,with 51 years in NHS, more than your own clinical exposure, I’m saddened by sponsored? skewed assaults on healing modalities maybe also representing a threat to financial paradigms: I absolved myself of scientific trials “for profit only”, in deference to holistic patient care, & the Hippocratic Oath
In a similar vein, Dr. Larry Malerba, a US homeopath, posted this comment on a Medscape interview with me:
Fortunately, the book reviews were more intelligent. They confirm what I mentioned above: reviewers were amazed at the depth of Charles’ irrationality. Harriett Hall expressed it as follows: “Charles’ efforts to promote alternative medicine have been mentioned many times on SBM, but readers may not appreciate the depth of his folly. I know I didn’t, until I read this book. The full story has never been told until now.” And Paul Benedetti wrote: “In short, readable chapters, Ernst unblinkingly presents how Charles has written books and articles promoting alternative medicine and spearheaded organizations, colleges, and foundations, giving full-throated support to one unproven, often bizarre, alternative health cure after another.”
One of the nicest pieces of praise came from someone who posted this comment on Amazon:
This is a revelatory critique of where vague well-intentioned but ill-informed health ideas promoted by a powerful person do or don’t get us.
Professor Ernst’s explanations are admirably clear – and no-one is more qualified than he to write on this topic. It’s difficult to imagine a more devastating comment on the bad conseqeunces of ill-informed ideas and actions, than that found in the last two paragraphs on Page 88.
There is a great deal of valuable information here on ‘alternative medicine’ approaches, in addition to the explanations of HRH Prince Charles’ involvement with them. A most worthwhile book for anyone wanting to find out more about alternative/complementary treatment modalities.
Yes, publishing a book can be a mixed blessing. The author works tirelessly for many months (for next to no pay) only to get aggressed – not for factual errors (that would be perfectly alright) or unfounded arguments (that would be welcome) but for allegedly being in it for the money or producing ‘prejudicial propaganda’. In the case of the new book, this had to be expected. I hesitated for an entire decade writing it (hoping someone else would tackle the task) because I knew that it would be far from straightforward to criticize the future king of one’s own country.
All the more reason to take this occasion and thank those who stand by me, who find my book relevant, who agree that it is instructive, and who feel that it deserves a wide readership.
THANK YOU
Dr Akbar Khan, MD, represents a novel and exciting avenue through which, in this case, a conventionally- trained family physician has come to embrace a broad array of integrative techniques; he witnessed first hand the immense magnitude of safety and efficacy of the practice … Dr Khan describes with frustration the lack of interest displayed by conventional practitioners for safe and effective solutions simply because they come from the realm of natural medicine. “My greatest concern is helping patients.”

From left to right: Douglas Andrews, Akbar Khan, Silvana Marra and Humaira Khan
From left to right: Douglas Andrews, Akbar Khan, Silvana Marra and Humaira Khan[/caption]
An article in the ‘Toronto Sun’, however, tells a very different story. The doctor was found ‘incompetent’ in the treatment of cancer patients. Akbar Khan told one patient she had leukemia when she did not. He told others they were improving under his alternative remedies while their cancer was actually advancing. One of them was a little boy dying of a brain tumor.
Now the Toronto family doctor has been found guilty by the Ontario Physicians and Surgeons Discipline Tribunal of
- incompetence,
- failure to maintain the standard of practice,
- and conduct that’s disgraceful, dishonorable or unprofessional
in his care of a total of 12 patients between 2012 and 2017. “Whether it was ‘snake oil,’ ‘witches’ brew’ or otherwise, whatever it was that Dr. Khan was offering his patients, it was not what he claimed,” concluded the tribunal in its decision. “In doing so, Dr. Khan set aside his obligations as a physician to uphold the College’s CAM and consent policies, and in doing so, he failed his patients.”
Khan is the founder of the Medicor Cancer Centres, which offer “unique non-toxic approaches to cancer treatment.” He treated terminally-ill patients with the unproven treatments that he called “SAFE Chemotherapy” billed as “lifesaving” and more effective than conventional chemo.
There was insufficient science and evidence to support the conclusion that “SAFE chemotherapy” works, or that it can help people in the way that Dr. Khan claims it can, and he should not have used it,” the tribunal found. Yet, Khan never told his patients it wasn’t working. According to the college’s summary: “Therapy stopped only when his patients either could not afford it any longer, their condition had deteriorated to such a degree that they could not tolerate it, they were so ill that they were admitted to hospital, or they died.”
According to the tribunal, Khan’s patients paid (US)$4,200 for one cycle of “SAFE chemotherapy”, and they received between five to 24 cycles of it. One of the most heartbreaking cases involved Khan’s treatment of a six-year-old boy with brain cancer. In 2017, his parents rejected treating him with lifesaving chemo and radiation and transferred his care to Khan, who prescribed Dichloroacetate (DCA) — which is a medication usually used for metabolic disorders, and not a proven cancer treatment. When a follow-up MRI showed their son’s tumor had grown and progressed to his spine, Khan told them it must be wrong and “his current therapy is actually working very well!” The boy died in 2018.
In another disturbing case, Khan used an “unapproved” test to diagnose a 59-year-old woman with acute leukemia — and informed her by email. He treated the devastated woman with honokol, a biological extract from magnolia bark, and Low Dose Naltrexone (LDN) — both of which are “not informed by evidence and science,” and “not the appropriate treatment for this patient’s presumed cancer.” Khan referred her to an oncologist who performed a bone marrow biopsy and then gave her the good news: “You do not have cancer. You’ve never had cancer. Go home and enjoy your life.” Yet, Khan insisted the oncologist was wrong. “We were frankly shocked that instead of reassuring Ms. B that her ordeal of worrying that she had leukemia could come to a close, Dr. Khan insisted to Ms. B that indeed, she did still have leukemia and urged her to keep taking LDN ‘to keep this under control,’” the tribunal wrote. “In short, Dr. Khan gave Ms. B a diagnosis that she did not have, for which he sold her a remedy that she did not need, which — as per evidence and science — turned out to be no remedy at all.”Khan’s response to the newspaper: “Since the legal process is still ongoing with the CPSO, I know my lawyer Marie Henein would not like me to comment at this time. Perhaps in the near future, I will be able to share with you another side to the story. If so, I will contact you.”
A penalty hearing has yet to be scheduled.
In case you are interested, here is a short CV of Dr. Khan:
| 2019 | FAAO – Fellow of the American Academy of Ozone Therapy |
| 2018 | Certified medical ozone therapy doctor (general ozone therapy, basic ProlozoneTM therapy and advanced ProlozoneTM therapy), certified by the American Academy of Ozone Therapy |
| 2018 | IMD, Integrative Medical Doctor (Board of Integrative Medicine) DHS, Doctor of Humanitarian Service (Board of Integrative Medicine) |
| 1994 | CCFP, Certificant of the College of Family Physicians of Canada (University of Toronto). |
| 1992 | MD, Doctor of Medicine (University of Toronto). |
Neurosurgeons from the Philippines recently presented the case of a 36-year-old woman who presented with severe bifrontal and postural headache associated with dizziness, vomiting, and double vision. A cranial computed tomography scan showed an acute subdural hematoma (SDH) at the interhemispheric area. Pain medications were given which afforded minimal relief.
The headaches occurred 2 weeks after the patient had received a cervical chiropractic manipulation (CM). Cranial and cervical magnetic resonance imaging revealed findings supportive of intracranial hypotension and neck trauma. The patient improved with conservative management.
The authors found 12 articles of SIH and CM after a systematic review of the literature. Eleven patients (90.9%) initially presented with orthostatic headaches. Eight patients (66.7%) were initially treated conservatively but only 5 (62.5%) had a complete recovery. Recovery was achieved within 14 days from the start of supportive therapy. Among the 3 patients who failed conservative treatment, 2 underwent non-directed epidural blood patch, and one required neurosurgical intervention.
The authors concluded that this report highlights that a thorough history is warranted in patients with new-onset headaches. A history of CM must be actively sought. The limited evidence from the case reports showed that patients with SIH and SDH but with normal neurologic examination and minor spinal pathology can be managed conservatively for less than 2 weeks. This review showed that conservative treatment in a closely monitored environment may be an appropriate first-line treatment.
As the authors rightly state, their case report does not stand alone. There are many more. In 2014, an Australian chiropractor published this review:
Background: Intracranial hypotension (IH) is caused by a leakage of cerebrospinal fluid (often from a tear in the dura) which commonly produces an orthostatic headache. It has been reported to occur after trivial cervical spine trauma including spinal manipulation. Some authors have recommended specifically questioning patients regarding any chiropractic spinal manipulation therapy (CSMT). Therefore, it is important to review the literature regarding chiropractic and IH.
Objective: To identify key factors that may increase the possibility of IH after CSMT.
Method: A systematic search of the Medline, Embase, Mantis and PubMed databases (from 1991 to 2011) was conducted for studies using the keywords chiropractic and IH. Each paper was reviewed to examine any description of the key factors for IH, the relationship or characteristics of treatment, and the significance of CSMT to IH. In addition, other items that were assessed included the presence of any risk factors, neck pain and headache.
Results: The search of the databases identified 39 papers that fulfilled initial search criteria, from which only eight case reports were relevant for review (after removal of duplicate papers or papers excluded after the abstract was reviewed). The key factors for IH (identified from the existing literature) were recent trauma, connective tissue disorders, or otherwise cases were reported as spontaneous. A detailed critique of these cases demonstrated that five of eight cases (63%) had non-chiropractic SMT (i.e. SMT technique typically used by medical practitioners). In addition, most cases (88%) had minimal or no discussion of the onset of the presenting symptoms prior to SMT and whether the onset may have indicated any contraindications to SMT. No case reports included information on recent trauma, changes in headache patterns or connective tissue disorders.
Discussion: Even though type of SMT often indicates that a chiropractor was not the practitioner that delivered the treatment, chiropractic is specifically cited as either the cause of IH or an important factor. There are so much missing data in the case reports that one cannot determine whether the practitioner was negligent (in clinical history taking) or whether the SMT procedure itself was poorly administered.
The new case report can, of course, be criticized for being not conclusive and for not allowing to firmly establish the cause of the adverse event. This is to a large extent due to the nature of case reports. Essentially, they provide a ‘signal’, and once the signal is loud enough, we need to act. In this case, action would mean to prohibit the intervention that is under suspicion and initiate conclusive research to prove or disprove a causal relationship.
This is how it’s done in most areas of healthcare … except, of course in so-called alternative medicine(SCAM). Here we do not even have the most basic tool to get to the bottom of the problem, namely a transparent post-marketing surveillance system that monitors the frequency of adverse events.
And whose responsibility is it to put such a system in place?
I let you guess.
Guest post by Catherine de Jong
On the 22nd of February 2022, a criminal court in the Netherlands ruled in a case brought by a 33-year-old man who suffered a double-sided vascular dissection of his vertebral arteries during a chiropractic neck manipulation.
What happened?
On the 26th of January 2016, the man visited a chiropractor because he wanted treatment for his headache. The chiropractor treated him with manipulations of his neck. The first treatment was uneventful but apparently not effective. The man went back for a second time. Immediately after the second treatment, the patient felt a tingling sensation that started in his toes and spread all over his body. Then he lost consciousness. He was resuscitated by the chiropractor and transported to a hospital. Several days later he woke up in the ICU of the university hospital (Free University, now Amsterdam UMC). He was paralyzed and unable to speak. He stayed in the ICU for 5 weeks. After a long stay in a rehabilitation center, he is now at home. He is disabled and incapacitated for life.
Court battles
The professional liability insurance of the chiropractor recognized that the treatment of the chiropractor had caused the disability and paid for damages. The patient was thus able to buy a new wheelchair-adapted house.
Health Inspection investigated the case. They noticed that the chiropractor could not show that there was informed consent for the neck manipulation treatment, but otherwise saw no need for action.
Six days after the accident the man applied to the criminal court. The case was dropped because, according to the judge, proof of guilt beyond reasonable doubt was impossible.
In rare occasions, vertebral artery dissection (VAD) does occur spontaneously in people without trauma or a chiropractor manipulating their neck. The list of causes for VAD show, besides severe trauma to the head and neck (traffic accidents) also chiropractic treatment, and rare connective tissue diseases like Marfan syndrome. A spontaneous dissection is very rare.
It took several attempts to persuade the criminal court to start the case and the investigation into what had happened in the chiropractor’s office. Now the verdict has been given, and it was a disappointing one.
The chiropractor was acquitted. The defense of the chiropractor argued, as expected, that two pre-existent spontaneous dissections might have caused the headache and that, therefore, the manipulation of the neck would have played at most a secondary role.
It is this defense strategy, which is invariably followed in the numerous court cases in the US. Chiropractors in particular give credence to this argumentation.
The defense of the patient was a professor of neurology. He considered a causal link between manipulation to the neck and the double-sided VAD to be proven.
In the judgment, the judge refers 14 times to the ‘professional standard’ of the Dutch Chiropractors Association, apparently without realizing that this professional standard was devised by the chiropractors themselves and that it differs considerably from the guidelines of neurologists or orthopedics. In 2016, the Dutch Health Inspection disallowed neck manipulation, but chiropractors do not care.
The verdict of the judge can be found here: ECLI:EN:RBNHO:2022:1401
Chiropractic is a profession that is not recognized in the Netherlands. Enough has been written (also on this website) about the strange belief of chiropractors that a wrong position of the vertebrae (“subluxations”) is responsible for 95% of all health problems and that detecting and correcting them can relieve symptoms and improve overall health. There is no scientific evidence that chiropractic subluxations exist or that their alleged “detection” or “correction” provides any health benefit. In the Netherlands, there are about 300 practicing chiropractors. Most are educated in the UK or the USA. The training that those chiropractors receive is not recognized in the Netherlands.
Most chiropractic treatments do little harm, but that does not apply to neck manipulation. When manipulating the neck, the outstretched head is subjected to powerful stretches and rotations. This treatment can in rare cases cause damage to the arteries, which carry blood to the brain. In this case, a double-sided cervical arterial dissection can lead to strokes and cerebral infarctions. How often this occurs (where is the central complication registration of chiropractors?) is unknown, but given that the effectiveness of this treatment has never been demonstrated and that therefore its risk/benefit ratio is negative, any complication is unacceptable.
How big is the chance that a 33-year-old man walks into a chiropractor’s office with a headache and comes out with a SPONTANEOUS double-sided vertebral artery dissection that leaves him wheelchair-bound and invalid for the rest of his life? I hope some clever statisticians will tell me.
PS
Most newspaper reports of this case are in Dutch, but here is one in English
On this blog, I have been regularly discussing the risks of so-called alternative medicine (SCAM). In particular, I have often been writing about the risks of chiropractic spinal manipulations.
Why?
Some claim because I have an ax to grind – and, in a way, they are correct: I do feel strongly that consumers should be warned about the risks of all types of SCAM, and when it comes to direct risks, chiropractic happens to feature prominently.
But it’s all based on case reports which are never conclusive and usually not even well done.
This often-voiced chiropractic defense is, of course, is only partly true. But even if it were entirely correct, it would beg the question: WHY?
Why do we have to refer to case reports when discussing the risks of chiropractic? The answer is simple: Because there is no proper system of monitoring its risks.
And why not?
Chiropractors claim it is because the risks are non-existent or very rare or only minor or negligible compared to the risks of other therapies. This, I fear, is false. But how can I substantiate my fear? Perhaps by listing a few posts I have previously published on the direct risks of chiropractic spinal manipulation. Here is a list (probably not entirely complete):
- Chiropractic manipulations are a risk factor for vertebral artery dissections
- Vertebral artery dissection after chiropractic manipulation: yet another case
- The risks of (chiropractic) spinal manipulative therapy in children under 10 years
- A risk-benefit assessment of (chiropractic) neck manipulation
- The risk of (chiropractic) spinal manipulations: a new article
- New data on the risk of stroke due to chiropractic spinal manipulation
- The risks of manual therapies like chiropractic seem to out-weigh the benefits
- One chiropractic treatment followed by two strokes
- An outstanding article on the subject of harms of chiropractic
- Death by chiropractic neck manipulation? More details on the Lawler case
- Severe adverse effects of chiropractic in children Another serious complication after chiropractic manipulation; best to avoid neck manipulations altogether, I think
- Ophthalmic Adverse Effects after Chiropractic Neck Manipulation
- Is chiropractic treatment safe?
- Cervical artery dissection and stroke related to chiropractic manipulation
- We have an ethical, legal and moral duty to discourage chiropractic neck manipulations
- Cerebral Haemorrhage Following Chiropractic ‘Activator’ Treatment
- Vertebral artery dissection after chiropractic manipulation: yet another case
- Horner Syndrome after chiropractic spinal manipulation
- Phrenic nerve injury: a rare but serious complication of chiropractic neck manipulation
- Chiropractic neck manipulation can cause stroke
- Chiropractic and other manipulative therapies can also harm children
- Complications after chiropractic manipulations: probably rare but certainly serious
- Disc herniation after chiropractic
- Evidence for a causal link between chiropractic treatment and adverse effects
- More on the risks of spinal manipulation
- The risk of neck manipulation
- “As soon as the chiropractor manipulated my neck, everything went black”
- Spinal epidural haematoma after neck manipulation
- New review confirms: neck manipulations are dangerous
- Top model died ‘as a result of visiting a chiropractor’
- Another wheelchair filled with the help of a chiropractor
- Spinal manipulation: a treatment to die for?
Of course, one can argue about the conclusiveness of this or that case report, but I feel that the collective evidence discussed in these posts makes my point abundantly clear:
chiropractic spinal manipulation is not safe.
On 27 January 2022, I conducted a very simple Medline search using the search term ‘Chinese Herbal Medicine, Review, 2022’. Its results were remarkable; here are the 30 reviews I found:
- Zhu, S. J., Wang, R. T., Yu, Z. Y., Zheng, R. X., Liang, C. H., Zheng, Y. Y., Fang, M., Han, M., & Liu, J. P. (2022). Chinese herbal medicine for myasthenia gravis: A systematic review and meta-analysis of randomized clinical trials. Integrative medicine research, 11(2), 100806.
- Lu, J., Li, W., Gao, T., Wang, S., Fu, C., & Wang, S. (2022). The association study of chemical compositions and their pharmacological effects of Cyperi Rhizoma (Xiangfu), a potential traditional Chinese medicine for treating depression. Journal of ethnopharmacology, 287, 114962.
- Su, F., Sun, Y., Zhu, W., Bai, C., Zhang, W., Luo, Y., Yang, B., Kuang, H., & Wang, Q. (2022). A comprehensive review of research progress on the genus Arisaema: Botany, uses, phytochemistry, pharmacology, toxicity and pharmacokinetics. Journal of ethnopharmacology, 285, 114798.
- Nanjala, C., Ren, J., Mutie, F. M., Waswa, E. N., Mutinda, E. S., Odago, W. O., Mutungi, M. M., & Hu, G. W. (2022). Ethnobotany, phytochemistry, pharmacology, and conservation of the genus Calanthe R. Br. (Orchidaceae). Journal of ethnopharmacology, 285, 114822.
- Li, M., Jiang, H., Hao, Y., Du, K., Du, H., Ma, C., Tu, H., & He, Y. (2022). A systematic review on botany, processing, application, phytochemistry and pharmacological action of Radix Rehmnniae. Journal of ethnopharmacology, 285, 114820.
- Mutinda, E. S., Mkala, E. M., Nanjala, C., Waswa, E. N., Odago, W. O., Kimutai, F., Tian, J., Gichua, M. K., Gituru, R. W., & Hu, G. W. (2022). Traditional medicinal uses, pharmacology, phytochemistry, and distribution of the Genus Fagaropsis (Rutaceae). Journal of ethnopharmacology, 284, 114781.
- Xu, Y., Liu, J., Zeng, Y., Jin, S., Liu, W., Li, Z., Qin, X., & Bai, Y. (2022). Traditional uses, phytochemistry, pharmacology, toxicity and quality control of medicinal genus Aralia: A review. Journal of ethnopharmacology, 284, 114671.
- Peng, Y., Chen, Z., Li, Y., Lu, Q., Li, H., Han, Y., Sun, D., & Li, X. (2022). Combined therapy of Xiaoer Feire Kechuan oral liquid and azithromycin for mycoplasma Pneumoniae pneumonia in children: A systematic review & meta-analysis. Phytomedicine : international journal of phytotherapy and phytopharmacology, 96, 153899.
- Xu, W., Li, B., Xu, M., Yang, T., & Hao, X. (2022). Traditional Chinese medicine for precancerous lesions of gastric cancer: A review. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie, 146, 112542.
- Wang, Y., Greenhalgh, T., Wardle, J., & Oxford TCM Rapid Review Team (2022). Chinese herbal medicine (“3 medicines and 3 formulations”) for COVID-19: rapid systematic review and meta-analysis. Journal of evaluation in clinical practice, 28(1), 13–32.
- Chen, X., Lei, Z., Cao, J., Zhang, W., Wu, R., Cao, F., Guo, Q., & Wang, J. (2022). Traditional uses, phytochemistry, pharmacology and current uses of underutilized Xanthoceras sorbifolium bunge: A review. Journal of ethnopharmacology, 283, 114747.
- Liu, X., Li, Y., Bai, N., Yu, C., Xiao, Y., Li, C., & Liu, Z. (2022). Updated evidence of Dengzhan Shengmai capsule against ischemic stroke: A systematic review and meta-analysis. Journal of ethnopharmacology, 283, 114675.
- Chen, J., Zhu, Z., Gao, T., Chen, Y., Yang, Q., Fu, C., Zhu, Y., Wang, F., & Liao, W. (2022). Isatidis Radix and Isatidis Folium: A systematic review on ethnopharmacology, phytochemistry and pharmacology. Journal of ethnopharmacology, 283, 114648.
- Tian, J., Shasha, Q., Han, J., Meng, J., & Liang, A. (2022). A review of the ethnopharmacology, phytochemistry, pharmacology and toxicology of Fructus Gardeniae (Zhi-zi). Journal of ethnopharmacology, 114984. Advance online publication.
- Wong, A. R., Yang, A., Li, M., Hung, A., Gill, H., & Lenon, G. B. (2022). The Effects and Safety of Chinese Herbal Medicine on Blood Lipid Profiles in Placebo-Controlled Weight-Loss Trials: A Systematic Review and Meta-Analysis. Evidence-based complementary and alternative medicine : eCAM, 2022, 1368576.
- Lu, C., Ke, L., Li, J., Wu, S., Feng, L., Wang, Y., Mentis, A., Xu, P., Zhao, X., & Yang, K. (2022). Chinese Medicine as an Adjunctive Treatment for Gastric Cancer: Methodological Investigation of meta-Analyses and Evidence Map. Frontiers in pharmacology, 12, 797753.
- Niu, L., Xiao, L., Zhang, X., Liu, X., Liu, X., Huang, X., & Zhang, M. (2022). Comparative Efficacy of Chinese Herbal Injections for Treating Severe Pneumonia: A Systematic Review and Bayesian Network Meta-Analysis of Randomized Controlled Trials. Frontiers in pharmacology, 12, 743486.
- Zhang, L., Huang, J., Zhang, D., Lei, X., Ma, Y., Cao, Y., & Chang, J. (2022). Targeting Reactive Oxygen Species in Atherosclerosis via Chinese Herbal Medicines. Oxidative medicine and cellular longevity, 2022, 1852330.
- Zhou, X., Guo, Y., Yang, K., Liu, P., & Wang, J. (2022). The signaling pathways of traditional Chinese medicine in promoting diabetic wound healing. Journal of ethnopharmacology, 282, 114662.
- Yang, M., Shen, C., Zhu, S. J., Zhang, Y., Jiang, H. L., Bao, Y. D., Yang, G. Y., & Liu, J. P. (2022). Chinese patent medicine Aidi injection for cancer care: An overview of systematic reviews and meta-analyses. Journal of ethnopharmacology, 282, 114656.
- Liu, H., & Wang, C. (2022). The genus Asarum: A review on phytochemistry, ethnopharmacology, toxicology and pharmacokinetics. Journal of ethnopharmacology, 282, 114642.
- Lin, Z., Zheng, J., Chen, M., Chen, J., & Lin, J. (2022). The Efficacy and Safety of Chinese Herbal Medicine in the Treatment of Knee Osteoarthritis: An Updated Systematic Review and Meta-Analysis of 56 Randomized Controlled Trials. Oxidative medicine and cellular longevity, 2022, 6887988.
- Yu, R., Zhang, S., Zhao, D., & Yuan, Z. (2022). A systematic review of outcomes in COVID-19 patients treated with western medicine in combination with traditional Chinese medicine versus western medicine alone. Expert reviews in molecular medicine, 24, e5.
- Mo, X., Guo, D., Jiang, Y., Chen, P., & Huang, L. (2022). Isolation, structures and bioactivities of the polysaccharides from Radix Hedysari: A review. International journal of biological macromolecules, 199, 212–222.
- Yang, L., Chen, X., Li, C., Xu, P., Mao, W., Liang, X., Zuo, Q., Ma, W., Guo, X., & Bao, K. (2022). Real-World Effects of Chinese Herbal Medicine for Idiopathic Membranous Nephropathy (REACH-MN): Protocol of a Registry-Based Cohort Study. Frontiers in pharmacology, 12, 760482.
- Zhang, R., Zhang, Q., Zhu, S., Liu, B., Liu, F., & Xu, Y. (2022). Mulberry leaf (Morus alba L.): A review of its potential influences in mechanisms of action on metabolic diseases. Pharmacological research, 175, 106029.
- Yuan, J. Y., Tong, Z. Y., Dong, Y. C., Zhao, J. Y., & Shang, Y. (2022). Research progress on icariin, a traditional Chinese medicine extract, in the treatment of asthma. Allergologia et immunopathologia, 50(1), 9–16.
- Zeng, B., Wei, A., Zhou, Q., Yuan, M., Lei, K., Liu, Y., Song, J., Guo, L., & Ye, Q. (2022). Andrographolide: A review of its pharmacology, pharmacokinetics, toxicity and clinical trials and pharmaceutical researches. Phytotherapy research : PTR, 36(1), 336–364.
- Zhang, L., Xie, Q., & Li, X. (2022). Esculetin: A review of its pharmacology and pharmacokinetics. Phytotherapy research : PTR, 36(1), 279–298.
- Wang, D. C., Yu, M., Xie, W. X., Huang, L. Y., Wei, J., & Lei, Y. H. (2022). Meta-analysis on the effect of combining Lianhua Qingwen with Western medicine to treat coronavirus disease 2019. Journal of integrative medicine, 20(1), 26–33. https://doi.org/10.1016/j.joim.2021.10.005
The amount of reviews alone is remarkable, I think: more than one review per day! Apart from their multitude, the reviews are noteworthy for other reasons as well.
- Their vast majority arrived at positive or at least encouraging conclusions.
- Most of the primary studies are from China (and we have often discussed how unreliable these trials are).
- Many of the primary studies are not accessible.
- Those that are accessible tend to be of lamentable quality.
I fear that all this is truly dangerous. The medical literature is being swamped with reviews of Chinese herbal medicine and other TCM modalities. Collectively they give the impression that these treatments are supported by sound evidence. Yet, the exact opposite is the case.
The process that is happening in front of our very eyes is akin to that of money laundering. Unreliable and often fraudulent data is being white-washed and presented to us as evidence.
The result:
WE ARE BEING SYSTEMATICALLY MISLED!
The ‘HEALY’ device is an odd form of so-called alternative medicine (SCAM) if there ever was one. Let me cite just two examples to show you how it is being promoted:
Healy technology is German, based on the scientific principles of quantum physics Healy devices analyse and measure the energetic imbalances on three levels – physical, mental, ad emotional – in order to emit specifically customised frequencies which will readjust your emotional and cellular energy centres to align with bio-energetic balance.
The Healy is a bio-resonance tool that works to support your body’s energetic field and promote deep cellular healing.
Reduced cell voltage occurs in almost all cases of acute and chronic dis-ease. Reduced cell voltage causes the cell’s internal metabolic processes to malfunction leading to disease. The Healy helps restore equilibrium through the use of resonant frequency waves. It works to stimulate and restore optimum cellular function with the use of very specific, harmonic energetic currents.
The Healy is a small, very complex piece of equipment. Using precise frequencies and low intensity currents, the Healy works to reverse the process of decreasing cell voltage by restoring the natural voltage of the cell membrane. Compromised cells lead us to experience a debilitating range of different symptoms, such as the inability to concentrate, learning difficulties, stress/burnout, physical diseases and illness, slow recovery from injury, cellulite, skin breakouts, mental health challenges and emotional instability…
The Healy delivers energy frequencies to positively influence the body to function at it’s natural, harmonic frequency. We were not designed to be depressed, anxious, highly reactive or suffer from chronic pain and exhausting conditions of disease. These are symptoms of much deeper imbalances and your Healy is a way to take back control of your wellbeing to positively influence all the cells in your body to start functioning just as nature intended.
Such advertising is disturbing and dangerous. It might make some consumers believe that the ‘Healy’ is based on cutting-edge science, and they might thus use it for serious conditions which, in extreme cases, could cost them their life. In truth, the ‘Healy’ is based on the purest BS that I have encountered for a long time. But the proof of the pudding is in the eating, you might say. Perhaps the ‘Healy’ is based on odd assumptions, but what counts is that it works.
Is there any sound evidence that the ‘Healy’ is effective?
No!
There is, as far as I can see, no scientific evidence to suggest that the ‘Healy’ is effective to prevent, cure or alleviate any condition or symptom.
If that is so, why is the ‘Healy’ licensed by the authorities of several countries?
Search me!
I really don’t know. All I do know is that I am unable to find any good evidence that the ‘Healy’ helps anyone – except, of course, those entrepreneurs who earn their living by exploiting vulnerable patients.
Enthusiasts of so-called alternative medicine (SCAM) seem remarkably often those who deny the evidence related to the dire consequences of a COVID-19 infection. Consequently, they also deny the value of COVID vaccinations. Because on this blog we have had so many examples of this phenomenon, let me today show an interesting study that might give them food for thought.
The cardiovascular complications of acute coronavirus disease 2019 (COVID-19) are well described, but the post-acute cardiovascular manifestations of COVID-19 have not yet been comprehensively characterized. The authors of this study used national healthcare databases from the US Department of Veterans Affairs to build a cohort of 153,760 individuals with COVID-19, as well as two sets of control cohorts with 5,637,647 (contemporary controls) and 5,859,411 (historical controls) individuals, to estimate risks and 1-year burdens of a set of pre-specified incident cardiovascular outcomes.
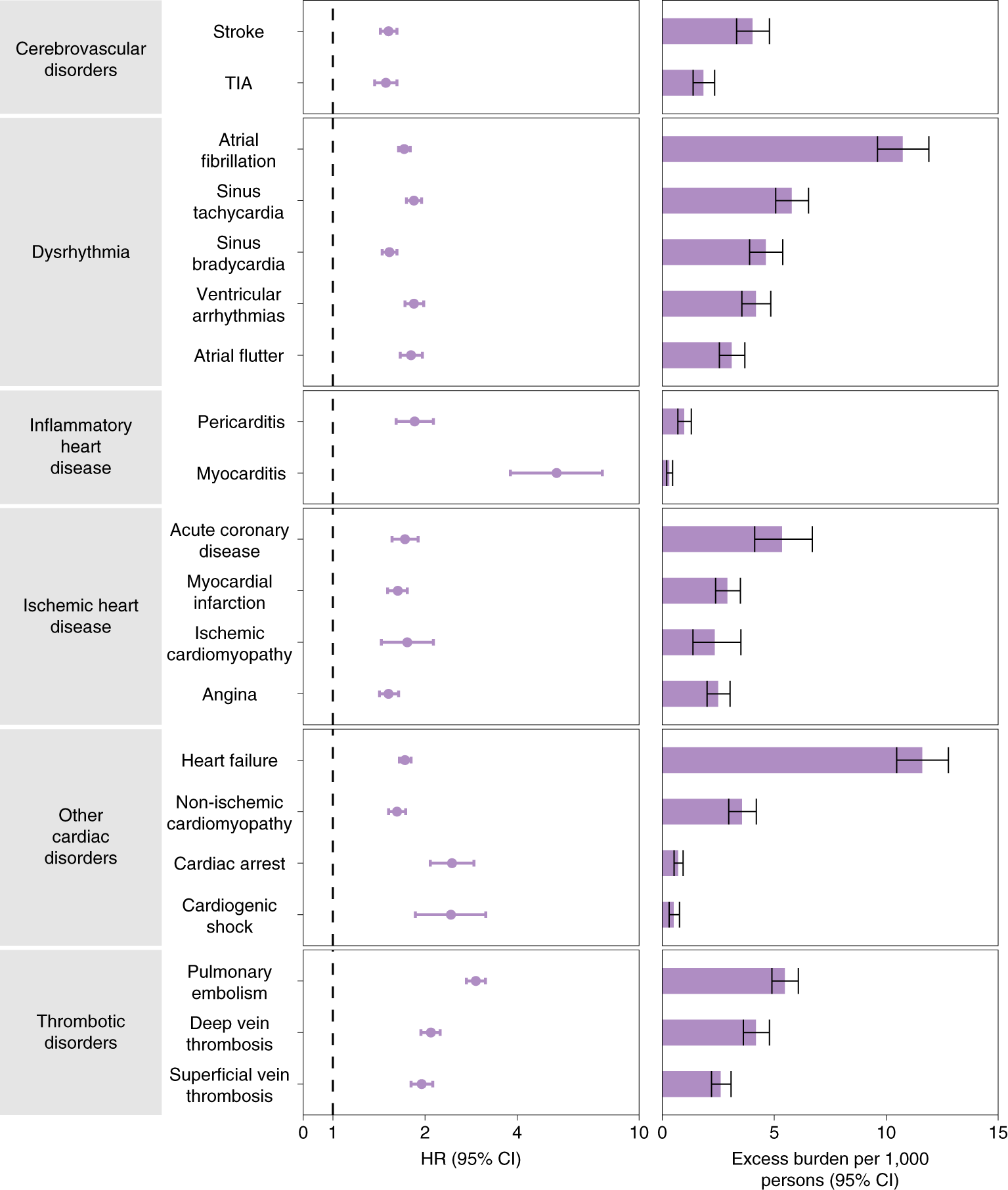
The results show that beyond the first 30 d after infection, individuals with COVID-19 are at increased risk of incident cardiovascular disease spanning several categories, including cerebrovascular disorders, dysrhythmias, ischemic and non-ischemic heart disease, pericarditis, myocarditis, heart failure, and thromboembolic disease. These risks and burdens were evident even among individuals who were not hospitalized during the acute phase of the infection and increased in a graded fashion according to the care setting during the acute phase (non-hospitalized, hospitalized, and admitted to intensive care).
Risks and 12-month burdens of incident post-acute COVID-19 cardiovascular outcomes compared with the contemporary control cohort.
Outcomes were ascertained 30 d after the COVID-19-positive test until the end of follow-up. COVID-19 cohort (n = 153,760) and contemporary control cohort (n = 5,637,647). Adjusted HRs and 95% CIs are presented. The length of the bar represents the excess burden per 1,000 persons at 12 months, and associated 95% CIs are also shown.
The authors concluded that the results provide evidence that the risk and 1-year burden of cardiovascular disease in survivors of acute COVID-19 are substantial. Care pathways of those surviving the acute episode of COVID-19 should include attention to cardiovascular health and disease.
I know, this is a case-control study and correlation is not causation. But to investigate the possibility of a causal link further, the authors also tested the robustness of results in several sensitivity analyses involving the outcomes of MACE and any cardiovascular outcome. The sensitivity analyses were performed in comparisons involving COVID-19 versus the contemporary control and COVID-19 versus the historical control and, additionally, COVID-19 by care setting versus both controls.
(1) To test whether the inclusion of additional algorithmically selected covariates would challenge the robustness of study results, they selected and used 300 high-dimensional variables (instead of the 100 used in the primary analyses) to construct the inverse probability weighting.
(2) They then also tested the results in models specified to include only pre-defined covariates (that is, without the inclusion of algorithmically selected covariates) to build the inverse probability weighting.
(3) They changed the analytic approach by using the doubly robust method (instead of the inverse weighting method used in primary analyses) to estimate the magnitude of the associations between COVID-19 exposure and the pre-specified outcomes.
All sensitivity analyses yielded results consistent with those produced using the primary approach. This means that it is likely that the cause of the outcomes was the COVID-19 exposure.
How often have we seen advocates of SCAM argue against vaccination by pointing to the risk of myocarditis and other cardiovascular conditions, no matter how minuscule that risk truly is? This study quantifies the relative risk of several different cardiovascular outcomes after COVID-19 infection and the risk of myocarditis clearly stands out. I hope that the findings of this important study will make the COVID deniers reconsider their attitude.
Vertebral artery dissection is an uncommon, but potentially fatal, vascular event. This case aimed to describe the pathogenesis and clinical presentation of vertebral artery dissection in a term pregnant patient. Moreover, the authors focused on the differential diagnosis, reviewing the available evidence.
A 39-year-old Caucasian woman presented at 38 + 4 weeks of gestation with a short-term history of vertigo, nausea, and vomiting. Symptoms appeared a few days after cervical spine manipulation by an osteopathic specialist. Urgent magnetic resonance imaging of the head was obtained and revealed an ischemic lesion of the right posterolateral portion of the brain bulb. A subsequent computed tomography angiographic scan of the head and neck showed a right vertebral artery dissection. Based on the correlation of the neurological manifestations and imaging findings, a diagnosis of vertebral artery dissection was established. The patient started low-dose acetylsalicylic acid and prophylactic enoxaparin following an urgent cesarean section.
Right vertebral artery dissection with ischemia in the posterolateral medulla oblongata. In DWI (a) and ADC map (b) the arrow shows a punctate, shiny ischemic lesion, with typical reduction of ADC in the right posterolateral medulla oblongata. c and d CT angiography (axial and 3D reformat, c and d, respectively) showing a focal dissection of the V2 distal segment of the right vertebral artery, with the arrow in figure c pointing to the dissection. e MRI angiography (time of flight, TOF) showing the absence of visualization of right PICA.
The authors concluded that vertebral artery dissection is a rare but potential cause of neurologic impairments in pregnancy and during the postpartum period. It should be considered in the differential diagnosis for women who present with headache and/or vertigo. Women with a history of migraines, hypertension, or autoimmune disorders in pregnancy are at higher risk, as well as following cervical spine manipulations. Prompt diagnosis and management of vertebral artery dissection are essential to ensure favorable outcomes.
In the discussion section, the authors point out that the incidence of VAD in pregnancy is twice as common as in the rest of the female population. They also mention that a review of the literature regarding adverse effects of spinal manipulation in the pregnant and postpartum periods identified adverse events in five pregnant women and two postpartum women. The authors also include a table that summarizes all cases of VAD reported both prior and after delivery, with 24 cases distributed with a prevalence during the postpartum period (19 of the 24 cases). The clinical presentation of these cases is varied, with a higher frequency of headaches, vertigo, and diplopia, and the risk factors most represented are hypertension and migraines.
The authors finish with this advice: practitioners who do spinal manipulations should be aware of the possible complications of neck manipulation in pregnancy and the postpartum period, particularly in mothers with underlying medical disorders that may predispose to vessel fragility and VAD.
I would add advice of a different nature: consumers should always question whether the risks of any intervention outweigh its benefit. In the case of neck manipulations, the answer is not positive.
Since about two years, I am regularly trying to warn people of charlatans of all types who mislead the public on COVID-related subjects. In this context, a recent paper in JAMA is noteworthy. Allow me to quote just a few passages from it:
COVID-19 misinformation and disinformation flood the public discourse; physicians are not the only source. But their words and actions “may well be the most egregious of all because they undermine the trust at the center of the patient-physician relationship, and because they are directly responsible for people’s health,” Pawleys Island, South Carolina, family medicine physician Gerald E. Harmon, MD, president of the American Medical Association (AMA), (which publishes JAMA), wrote recently. In November, the AMA House of Delegates adopted a new policy to counteract disinformation by health care professionals.
… Few physicians have been disciplined so far, even though the Federation of State Medical Boards (FSMB), representing the state and territorial boards that license and discipline physicians, and, in some cases, other health care professionals, and the American Board of Medical Specialties (ABMS), consisting of the boards that determine whether physicians can be board-certified, have issued statements cautioning against spreading false COVID-19 claims.
In July 2021, the FSMB warned that spreading COVID-19 misinformation could put a physician’s license at risk. The organization said it was responding “to a dramatic increase in the dissemination of COVID-19 vaccine misinformation and disinformation by physicians and other health care professionals.”
The ABMS released a statement in September 2021. “The spread of misinformation and the misapplication of medical science by physicians and other medical professionals is especially harmful as it threatens the health and well being of our communities and at the same time undermines public trust in the profession and established best practices in care,” the ABMS said.
In an annual survey of its 70 member boards conducted in fall 2021, the FSMB asked about complaints and disciplinary actions related to COVID-19. Of the 58 boards that responded, 67% said they had seen an uptick in complaints about licensees spreading false or misleading COVID-19 misinformation, according to results released in December 2021. But only 12 (21%) of the 58 boards said they’d taken disciplinary action against a physician for that reason…
- What percentage of lay-homeopaths misinform their patients?
- What percentage of chiropractors misinform their patients?
- What percentage of energy healers misinform their patients?
- What percentage of naturopaths misinform their patients?
- What percentage of acupuncturists misinform their patients?
- etc., etc.
As the total number of SCAM practitioners might, in some parts of the world, easily outnumber doctors, these questions are highly relevant. Yet, I am not aware of any reliable data on these issues. Judging from what I have observed (and written about) during the pandemic, I guess that the percentages are likely to be substantial and way higher than those for doctors. To me, this suggests that we ought to focus much more on SCAM practitioners if, in future health crises, we want to prevent the confusion and harm that misinformation inevitably causes.



Medscape and Ernst deserve each other. What a sad old fellow, desperate to live down his homeopathic past by producing a steady stream of deeply prejudicial anti-homeopathy propaganda. What kind of person dedicates his life to hate speech against the second most popular medical therapy worldwide? No doubt, he’s convinced himself that it’s a noble endeavor. Sad and comical.