Monthly Archives: February 2021
This study aimed to evaluate the effect of Traditional Chinese Medicine (TCM) on patients with gastric cancer following surgery and adjuvant chemotherapy in Taiwan. The cohort sampling data set was obtained from the Registry of Catastrophic Illness Patient Database, a research database of patients with severe illnesses from the National Health Insurance Research Database, Taiwan. Patients who had received a new diagnosis of gastric cancer and had undergone surgery were enrolled. the researchers matched TCM users and nonusers at a ratio of 1 : 3 based on the propensity score, and TCM users were also grouped into short-term and long-term users.
The number of TCM users and nonusers was 1701 and 5103 after applying the propensity score at a ratio of 1 : 3. Short-term users and long-term TCM users were independently associated with a decreased risk of death with HRs of 0.59 (95% confidence interval (CI), 0.55-0.65) and 0.41 (95% CI, 0.36-0.47), respectively, compared with TCM nonusers. The researchers also obtained similar results when they adjusted for covariates in the main model, as well as each of the additional listed covariates. They also observed similar HR trends in short-term users and long-term TCM users among men and women aged <65 years and ≥65 years. The most commonly prescribed single herb and herbal formula in our cohort were Hwang-Chyi (Radix Hedysari; 11.8%) and Xiang-Sha-Liu-Jun-Zi-Tang (15.5%), respectively.

The authors concluded that TCM use was associated with higher survival in patients with gastric cancer after surgery and adjuvant chemotherapy. TCM could be used as a complementary and alternative therapy in patients with gastric cancer after surgery and adjuvant chemotherapy.
This is an interesting study which seems well-done – except for one fatal mistake: even in the title, the authors imply a causal relationship between TCM and survival. Their conclusion has two sentences; the first one speaks correctly of an association. The second, however, not only implies causality but goes much further in suggesting that TCM should be used to prolong the life of patients. Yet, there are, of course, dozens of factors that could interfere with the findings or be the true cause of the observed outcome.
Anyone with a minimum of critical thinking ability should know that CORRELATION IS NOT CAUSATION; sadly, the authors of this study seem to be the exception.
Scientists from Israel and Iceland recently suggested that an extract of spirulina algae has the potential to reduce the chances of COVID-19 patients developing a serious case of the disease. Here is the abstract of their paper:
An array of infections, including the novel coronavirus (SARS-CoV-2), trigger macrophage activation syndrome (MAS) and subsequently hypercytokinemia, commonly referred to as a cytokine storm (CS). It is postulated that CS is mainly responsible for critical COVID-19 cases, including acute respiratory distress syndrome (ARDS). Recognizing the therapeutic potential of Spirulina blue-green algae (Arthrospira platensis), in this in vitro stimulation study, LPS-activated macrophages and monocytes were treated with aqueous extracts of Spirulina, cultivated in either natural or controlled light conditions. We report that an extract of photosynthetically controlled Spirulina (LED Spirulina), at a concentration of 0.1 µg/mL, decreases macrophage and monocyte-induced TNF-α secretion levels by over 70% and 40%, respectively. We propose prompt in vivo studies in animal models and human subjects to determine the putative effectiveness of a natural, algae-based treatment for viral CS and ARDS, and explore the potential of a novel anti-TNF-α therapy.
The Jerusalem Post reported that the research was conducted in a MIGAL laboratory in northern Israel with algae grown and cultivated by the Israeli company VAXA, which is located in Iceland. VAXA received funding from the European Union to explore and develop natural treatments for coronavirus. Iceland’s MATIS Research Institute also participated in the study.
In a small percentage of patients, infection with the coronavirus causes the immune system to release an excessive number of TNF-a cytokines, resulting in what is known as a cytokine storm. The storm causes acute respiratory distress syndrome and damage to other organs, the leading cause of death in COVID-19 patients. “If you control or are able to mitigate the excessive release of TNF-a, you can eventually reduce mortality,” said Asaf Tzachor, a researcher from the IDC Herzliya School of Sustainability and the lead author of the study. During cultivation, growth conditions were adjusted to control the algae’s metabolomic profile and bioactive molecules. The result is what Tzachor refers to as “enhanced” algae.
Tzachor said that despite the special growth mechanism, the algae are a completely natural substance and should not produce any side effects. Spirulina is approved by the US Food and Drug Administration as a dietary substance. It is administrated orally in liquid drops. “This is natural, so it is unlikely that we would see an adverse or harmful response in patients as you sometimes see in patients that are treated with chemical or synthetic drugs,” he said. The algae have been shown to reduce inflammation. Tzachor said that if proven effective, spirulina could also be used against other coronaviruses and influenza. “If we succeed in the next steps,” said Dr. Dorit Avni, director of the laboratory at MIGAL, “there is a range of diseases that can be treated using this innovative solution – as a preventative treatment or a supportive treatment.”
___________________________
This is undoubtedly interesting, and one can only hope that their research is successful. However, it is a far cry from what some journalists are already making of the news. One headline read: “Scientists Discover ‘All-Natural’ COVID Treatment That Can Prevent ‘Cytokine Storm’ In Severe Patients.”
Several previously published clinical trials have suggested that both acupuncture and sham acupuncture exert significant, non-specific effects on treatment outcomes when compared to no-treatment controls. A recently developed framework (mechanisms in orthodox and complementary and alternative medicine-MOCAM) suggests that the non-specific effects of acupuncture originate from multiple domains (e.g. patient characteristics, acupuncturist skill/technique, the patient-acupuncturist relationship, and the acupuncture environment). However, it remains to be determined precisely how these domains influence the non-specific effects of treatment among patients receiving acupuncture and sham acupuncture in clinical trials.
To address this issue, researchers conducted a systematic review to synthesize existing qualitative evidence on how trial participants randomized to acupuncture and sham acupuncture groups experience non-specific effects, regardless of the types of medical conditions investigated.
This systematic review included primary qualitative studies embedded in randomized controlled trials designed to investigate acupuncture or sham acupuncture interventions. Eligible studies published in English were derived from a search of five international databases. The methodological quality of included studies was evaluated using the Critical Appraisal Skills Programme (CASP) tool. Using a framework synthesis approach, the identified MOCAM framework was adapted based on the synthesis of the available qualitative evidence.
A total of 20 studies of high methodological quality were included. The proposed model indicated that the effects of acupuncture may be increased by:
- maintaining a professional status,
- applying a holistic treatment approach,
- practicing empathy,
- providing patients with an appropriate explanation of the theory behind acupuncture and sham acupuncture.
From the patient’s perspective, the efficacy of treatment can be increased by:
- following the lifestyle modification advice provided by acupuncturists,
- maintaining a positive attitude toward treatment efficacy,
- actively engaging with acupuncturists during the consultation,
- making behavioral changes based on experience gained during the trial.
The authors concluded that the results of this study may provide a basis for improving and standardizing key components of non-specific effects in acupuncture treatment, and for improving the isolation of specific effects in future clinical trials involving acupuncture and sham acupuncture.
The authors also state that having a positive attitude and high expectations regarding treatment efficacy can lead to positive health outcomes, along with a sense of curiosity and altruistic desire to join clinical trials. Indeed, previous clinical trials have reported that higher expectations regarding treatment effects may help to reduce fatigue and alleviate osteoarthritis in both acupuncture and sham acupuncture groups. Similar benefits of positive expectations have also been observed among patients with irritable bowel syndrome in sham acupuncture trials.
SO CLOSE AND YET SO FAR!
So close to admitting that these findings indicate quite strongly that acupuncture is but a theatrical placebo.
My recent book discusses 20 of the worst and 20 of the best so-called alternative treatments. Some people are surprised and ask HOW DID YOU MANAGE TO FIND 20? WHAT THERAPIES ARE YOU TALKING ABOUT? As the book is in German, I have for non-German speakers the translated list and my concluding remarks from the book about the 20 best:
- Alexander technique
- Autogenic training
- Chondroitin
- Feldenkrais technique
- Fish oil
- Glucosamine
- Hypnotherapy
- Hypericum
- Garlic
- Laughing therapy
- Lymphdrainage
- Music therapy
- Oil pulling
- Pilates
- Progressive muscle relaxation
- Cupping
- Tai chi
- Triggerpoint therapy
- Visualization
- Yoga
When I look at the ’20 best’, I notice a few things that are perhaps worth highlighting again. The most striking thing is certainly that they are often therapies that are so close to conventional medicine that they can hardly be counted as alternative medicine anymore. Autogenic training, chondroitin, Feldenkrais therapy, fish oil, glucosamine, hypnotherapy, St. John’s wort, laughter therapy, lymphatic drainage, music therapy, and trigger point therapy are all procedures that are now at least partially integrated into conventional medicine. This brings to mind Tim Minchin’s bon mot, “You know what they call alternative medicine that’s been proven to work? – Medicine.”
The ’20 best’ can be roughly divided into three main categories:
1. physical therapies such as Alexander Technique, Feldenkrais Therapy, Lymphatic Drainage, Pilates, Tai Chi, and Yoga.
2. relaxation therapies such as autogenic training, hypnotherapy, laughter therapy, music therapy, progressive muscle relaxation, and visualization.
3. pharmacological therapies such as chondroitin, fish oil, glucosamine, St. John’s wort, and garlic.
That exercise, relaxation, and pharmacology can be effective is probably no surprise to anyone. In other words, unlike the ’20 Most Questionable’, almost all of the ’20 Best’ are supported by some plausibility. Very rarely does one find a therapy that is both implausible and effective. Among the procedures discussed in this book, this is the case only for Feldenkrais therapy.
In the review of the ’20 Best’, I have repeatedly emphasized that the evidence, while positive, is seriously flawed and therefore not as convincing as one might wish. There may be several reasons for this:
– In most cases, there is too little research funding available to conduct a sufficient number of good studies.
– Even if the money were available, the expertise (and occasionally the will) to test the methods scientifically is often lacking.
– Clinical trials of alternative medicine are often considerably more difficult to design and conduct than studies in conventional medicine. For instance, it is not always easy to find an adequate placebo. For example, what is an appropriate placebo for a study of hypnotherapy that allows patients to be blinded?
It follows that we must occasionally turn a blind eye, but ultimately cannot be completely certain that the procedure in question is in fact anything more than a placebo.
While the ’20 Most Questionable’ include many procedures that have been touted as panaceas, this is rarely the case with the ’20 Best’. On the contrary, most of the treatments in this category are effective for only a very few indications. Here the saying of one of my clinical teachers comes to mind, “If a therapy is supposed to be good for everything, it most likely won’t work for anything.”
What further strikes me as important is the fact that while all of the methods mentioned are effective, they are invariably symptomatic. None of the ’20 Best’ represents a causal therapy that can address a disease causally and thus actually cures it. This is in stark contrast to the many claims of healing made by alternative medicine providers, who all too often advertise their methods as addressing the root cause of a condition.
If we take a close look at the ’20 best’, we must finally also ask ourselves which of these methods are actually better than the conventional treatment of the same condition. All 20 have been positively evaluated by me in terms of their benefit/risk ratio. But this does not mean that they are superior to conservative therapy with respect to this important criterion. St. John’s wort is the most likely to meet this condition; it is as effective as conventional antidepressants for mild to moderate depression and has fewer side effects than them. Its benefit/risk ratio is thus superior to that of conventional antidepressants. I am not sure about any of the other treatments in the ’20 Best’ category.
For some time now, I have been using the umbrella term ‘so-called alternative medicine’ (SCAM). As I explain below, I think it is relatively well-suited. But this is not to say that it is the only name for it. Many other umbrella terms have been used in the past.
Is there perhaps one that you prefer?
- Fringe medicine is rarely used today. It denotes the fact that the treatments under this umbrella are not in the mainstream of healthcare. Some advocates seem to find the word derogatory, and therefore it is now all but abandoned.
- Unorthodox medicine is a fairly neutral term describing the fact that medical orthodoxy tends to shun most of the treatments in question. Strictly speaking, the word is also incorrect; the correct term would be ‘heterodox medicine’.
- Unconventional is also a neutral term but it is open to misunderstandings: any new innovation in medicine might initially be called unconventional. It is therefore less than ideal.
- Traditional medicine describes the fact that most of the modalities in question have been around for centuries and thus have a long tradition of usage. However, as the term is sometimes also used for conventional medicine, it is confusing and far from ideal.
- Alternative medicine is the term everyone seems to know and which is most commonly employed in non-scientific contexts. In the late 1980s, some experts pointed out that the word could give the wrong impression: most of the treatments in question are not used as a replacement but as an adjunct to conventional medicine.
- Complementary medicine became subsequently popular based on the above consideration. It accounts for the fact that the treatments tend to be used by patients in parallel with conventional medicine.
- Complementary and alternative medicine (CAM) describes the phenomenon that many of the treatments can be employed either as a replacement of or as an adjunct to conventional medicine.
- Holistic medicine denotes the fact that practitioners often pride themselves to look after the whole patient – body, mind, and spirit. This could lead to the erroneous impression that conventional clinicians do not aim to practice holistically. As I have tried to explain repeatedly, any good healthcare always has been holistic. Therefore, the term is misleading, in my view.
- Natural medicine describes the notion that many of the methods in question are natural. The term seems attractive and is therefore good for business. However, any critical analysis will show that many of the treatments in question are not truly natural. Therefore this term too is misleading.
- Integrated medicine is currently popular and much used by Prince Charles and other enthusiasts. As we have discussed repeatedly on this blog, the term is nevertheless highly problematic.
- Integrative medicine is the word used in the US for integrated medicine.
- CAIM (complementary/alternative/integrative medicine) is a term that some US authors recently invented. I find this attempt to catch all the various terms in one just silly.
- So-called alternative medicine (SCAM) is the term I tend to use. It accounts for two important facts: 1) if a treatment does not work, it cannot possibly serve as an adequate alternative; 2) if a therapy does work, it should be part of conventional medicine. Thus, there cannot be an ‘alternative medicine’, as much as there cannot be an alternative chemistry or an alternative physics.
Yet,some advocates find ‘SCAM’ derogatory. Intriguingly, my decision to use this term was inspired by Prince Charles, arguably the world’s greatest champion of this sector of healthcare. In his book ‘HARMONY’, he repeatedly speaks of ‘so-called alternative treatments’.
You don’t believe me?
Fair enough!
In this case – and in order to save you the expense of buying Charles’ book for checking – let me provide you with a direct quote: “Some so-called alternative treatments seek to work with these functions to aid recovery…” (page 225).
And who would argue that Charles is dismissive about alternative medicine?
As we have often discussed, proponents of so-called alternative medicine (SCAM), have an unfortunate tendency to mislead the public about vitamins and other supplements. Consequently, there is much uncertainty in many people’s minds. It is, therefore, all the more important to highlight new information that might counter this phenomenon.
This study tested whether high-dose zinc and/or high-dose ascorbic acid reduce the severity or duration of symptoms compared with usual care among ambulatory patients with SARS-CoV-2 infection. It was designed as a multicenter, single health system randomized clinical factorial open-label trial and enrolled 214 adult patients with a diagnosis of SARS-CoV-2 infection confirmed with a polymerase chain reaction assay who received outpatient care in sites in Ohio and Florida. The trial was conducted from April 27, 2020, to October 14, 2020.
Patients were randomized in a 1:1:1:1 allocation ratio to receive either:
- zinc gluconate (50 mg),
- ascorbic acid (8000 mg),
- both of these agents,
- standard care only.
The treatments lasted 10 days.
The primary endpoint was the number of days required to reach a 50% reduction in symptoms, including the severity of fever, cough, shortness of breath, and fatigue (rated on a 4-point scale for each symptom). Secondary endpoints included days required to reach a total symptom severity score of 0, cumulative severity score at day 5, hospitalizations, deaths, adjunctive prescribed medications, and adverse effects of the study supplements.
A total of 214 patients were randomized, with a mean (SD) age of 45.2 (14.6) years and 132 (61.7%) women. The study was stopped for a low conditional power for benefit with no significant difference among the 4 groups for the primary endpoint. Patients who received usual care without supplementation achieved a 50% reduction in symptoms at a mean (SD) of 6.7 (4.4) days compared with 5.5 (3.7) days for the ascorbic acid group, 5.9 (4.9) days for the zinc gluconate group, and 5.5 (3.4) days for the group receiving both (overall P = .45). There was no significant difference in secondary outcomes among the treatment groups.
The authors concluded that, in this randomized clinical trial of ambulatory patients diagnosed with SARS-CoV-2 infection, treatment with high-dose zinc gluconate, ascorbic acid, or a combination of the 2 supplements did not significantly decrease the duration of symptoms compared with standard of care.
This study has several limitations (and its authors are laudably frank about them):
- Its sample size is small.
- It has no placebo control group.
- It is open-label.
- Patients were not masked to which therapy they received.
The trial nevertheless adds important information about the value of using zinc or vitamin C or both in the management of COVID patients.
On Twitter, the hype had begun even before its text was available. Priti Gandhi, for instance, tweeted:
Yet another feather in India’s cap!! 1st evidence-based, CoPP-WHO GMP certified medicine for Covid-19 released today. Congratulations to @yogrishiramdev ji, @Ach_Balkrishna ji & the team of scientists at Patanjali Research Institute. Your efforts have been successful!! #Ayurveda
So, what is it all about? This study included 100 patients and was designed to evaluate the impact of traditional Indian Ayurvedic treatment on asymptomatic patients with COVID-19 infection. It is a placebo-controlled randomized double-blind pilot clinical trial that was conducted at the Department of Medicine in the National Institute of Medical Sciences and Research, Jaipur, India.
- 1 g of Giloy Ghanvati (Tinospora cordifolia)
- 2 g of Swasari Ras (traditional herbo-mineral formulation)
- 0.5 g of Ashwagandha (Withania somnifera)
- 0.5 g of Tulsi Ghanvati (Ocimum sanctum)
The treatment was given orally to the patients in the treatment group twice per day for 7 days. Medicines were given in the form of tablets and each tablet weighed 500 mg. While Swasari Ras was administered in powdered form, 30 min before breakfasts and dinners, rest were scheduled for 30 min post-meals. Patients in the treatment group also received 4 drops of Anu taila (traditional nasal drop) in each nostril every day 1 h before breakfast. Patients in the placebo group received identical-looking tablets and drops, post-randomization, and double-blinded assortments. 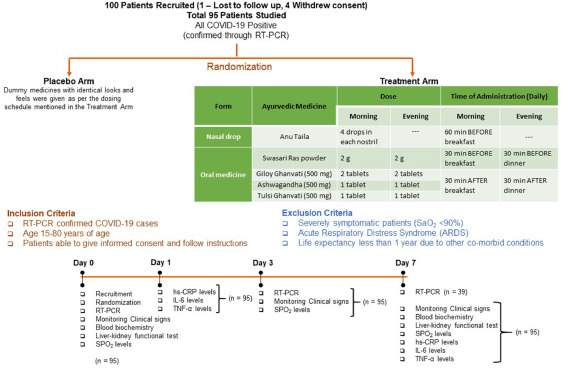 The RT-qPCR test was used for the detection of viral load in the nasopharyngeal and oropharyngeal swab samples of study participants during the study. Chemiluminescent immunometric assay was used to quantify serum levels of interleukin-6 (IL-6), tumor necrosis factor alpha (TNF-α), and high sensitivity C-reactive protein (hs-CRP) on day 1 and day 7 of the study. Patient testing negative for SARS-CoV-2 in the RT-PCR analysis was the primary outcome of this study.
The RT-qPCR test was used for the detection of viral load in the nasopharyngeal and oropharyngeal swab samples of study participants during the study. Chemiluminescent immunometric assay was used to quantify serum levels of interleukin-6 (IL-6), tumor necrosis factor alpha (TNF-α), and high sensitivity C-reactive protein (hs-CRP) on day 1 and day 7 of the study. Patient testing negative for SARS-CoV-2 in the RT-PCR analysis was the primary outcome of this study.
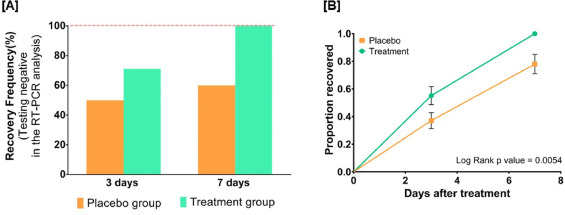
By day three, 71.1 % and 50.0 % of patients recovered in the treatment and placebo groups, respectively. The treatment group witnessed 100 % recovery by day 7, while it was 60.0 % in the placebo group. Average fold changes in serum levels of hs-CRP, IL-6, and TNF-α in the treatment group were respectively, 12.4, 2.5 and 20 times lesser than those in the placebo group at day 7. There was a 40 % absolute reduction in the risk of delayed recovery from infection in the treatment group.
The authors concluded that Ayurvedic treatment can expedite virological clearance, help in faster recovery and concomitantly reduce the risk of viral dissemination. Reduced inflammation markers suggested less severity of SARS-CoV-2 infection in the treatment group. Moreover, there was no adverse effect observed to be associated with this treatment.
I have the following concerns or questions about this trial:
- Why do the authors call it a pilot study? A pilot study is merely for testing the feasibility of a trial design and is not meant to yield definitive efficacy results.
- The authors state that the patients were asymptomatic yet in the discussion they claim they were asymptomatic or mildly symptomatic.
- Some of the effect sizes reported here are extraordinary and seem almost too good to be true.
- The claim of no adverse effect is implausible; even placebos would cause perceived adverse effects in a percentage of patients.
- If the study is solid and withstands the scrutiny of the raw data, it is of huge relevance for public health. So, why did the authors publish it in PHYTOMEDICINE, a relatively minor and little-known journal?
An article in The Economic Times’ reported this:
Patanjali Ayurved released what it called the first “evidence-based” medicine for Covid-19 on Friday. It claimed it has been “recognised by the WHO (World Health Organization) as an ayurvedic medicine for corona”.
Patanjali promoter, yoga guru Baba Ramdev, released a scientific research paper in this regard at the launch, presided over by Union health minister Harsh Vardhan and transport minister Nitin Gadkari.
The Ayurveda products maker said it has received a certification from the Ayush ministry. “Coronil has received the Certificate of Pharmaceutical Product (CoPP) from the Ayush section of Central Drugs Standard Control Organisation (CDSCO) as per the WHO certification scheme,” it said in a statement.
Under the CoPP, Coronil can be exported to 158 countries, the company said, adding that based on the presented data, the ministry has recognised Coronil as medicine for “supporting measure in Covid-19”.
Am I the only one who fears that something is not entirely kosher about the study? (This is an honest question, and I would be pleased to receive answers from my readers)
Osteopathy is hugely popular in France. Despite the fact that osteopathy has never been conclusively shown to generate more good than harm, French osteopaths have somehow managed to get a reputation as trustworthy, evidence-based healthcare practitioners. They tend to treat musculoskeletal and many other issues. Visceral manipulation is oddly popular amongst French osteopaths. Now the trust of the French in osteopathy seems to have received a serious setback.
‘LE PARISIEN‘ has just published an article about the alleged sexual misconduct of one of the most prominent French osteopaths and director of one of the foremost schools of osteopathy in France. Here are some excerpts from the article that I translated for readers who don’t speak French:
The public prosecutor’s office of Grasse (Alpes-Maritimes) has opened a judicial investigation against Marc Bozzetto, the director and founder of the school of osteopathy in Valbonne, accused of rape and sexual assault.
In total, “four victims are targeted by the introductory indictment,” said the prosecutor’s office, stating that Marc Bozzetto had already been placed in police custody since the beginning of the proceedings. The daily paper ‘Nice-Matin’ has listed six complaints and published the testimony of a seventh alleged victim.
This victim claims to have been sexually assaulted in 2013, alleging that, during a professional appointment, Bozzetto had massaged her breasts and her intimate area. “He told me that everything went through my vagina and clitoris, that I had to spread my legs and let the energy flow through my clitoris. That I had to learn how to give myself pleasure on my own,” she told Nice-Matin. The newspaper also recorded the testimonies of a former employee, a top-level sportswoman, an employee from the world of culture, and a former student.
“I take note that a judicial inquiry is open. To date, he has neither been summoned nor indicted,” said Karine Benadava, the Parisian lawyer of the 80-year-old Bozzetto. Her client had already responded following initial accusations from students: “This is a normal feeling for women, but if all the women who work on the pelvis complain, you can’t get away with it and you have to stop working as a pelvic osteopath,” replied Bozzetto. In another interview, he had declared himself “furious” and unable to understand the reaction of these two students.
The school of osteopathy trains about 300 students each five years and presents itself as the first holistic osteopathy campus in France.
______________________________
Such stories of sexual misconduct of practitioners of so-called alternative medicine (SCAM) are sadly no rarety, particularly those working in the area of manual therapy. They remind me of a case against a Devon SCAM practitioner in which I served as an expert witness many years ago. Numerous women gave witness that he ended up having his fingers in their vagina during therapy. He did not deny the fact but tried to defend himself by claiming that he was merely massaging lymph-nodes in this area. It was my task to elaborate on the plausibility of this claim. The SCAM practitioner in question was eventually sentenced to two years in prison.
It stands to reason that SCAM practitioners working in the pelvic area are at particularly high risk of going atray. The above case might be a good occasion to have a public debate in France and ask: IS VISCERAL OSTEOPATHY EVIDENCE-BASED? The answer is very clearly NO! Surely, this is a message worth noting in view of the current popularity of this ridiculous, costly, and dangerous charlatanry.
And how does one minimize the risk of sexual misconduct of SCAM professionals? The most obvious answer would be, by proper education during their training. In the case mentioned above, this might have been a problem: if the director is into sexual misconduct, what can you expect of the rest of the school? In many other cases, the problem is even greater: many SCAM practitioners have had no training at all, or no training in healthcare ethics to speak of.
Just as I read that the right-wing preacher Lance Wallnau once claimed he had cured Rush Limbaugh of his lung cancer – Limbaugh died yesterday of that cancer – I found this paper in the bizarre journal ‘EXPLORE’ reporting a much more successful (or should I say ‘tall’?) tale of healing by prayer.
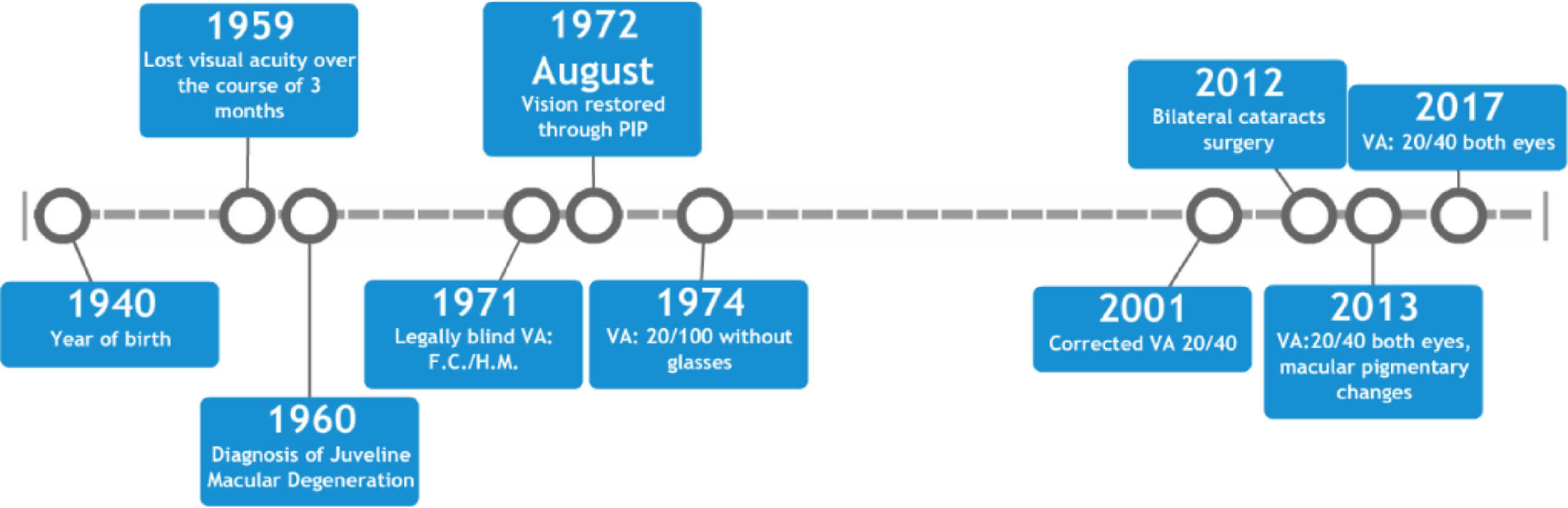
This case report describes an 18-year-old female who lost the majority of her central vision over the course of three months in 1959. Medical records from 1960 indicate visual acuities (VA) of less than 20/400 for both eyes corresponding to legal blindness. On fundus examination of the eye, there were dense yellowish-white areas of atrophy in each fovea and the individual was diagnosed with juvenile macular degeneration (JMD).
In 1971, another examination recorded her uncorrected VA as finger counting on the right and hand motion on the left. She was diagnosed with macular degeneration (MD) and declared legally blind. In 1972, having been blind for over 12 years, the patient reportedly regained her vision instantaneously after receiving proximal-intercessory-prayer (PIP). Subsequent medical records document repeated substantial improvement; including uncorrected VA of 20/100 in each eye in 1974 and corrected VAs of 20/30 to 20/40 were recorded from 2001 to 2017.
To date, her eyesight has remained intact for forty-seven years, according to the authors of this paper.
The course of these events is summarised in the graph below.
And here is what the patients was reported stating:
“What people need to understand is ‘I was blind’, totally blind and attended the School for the Blind. I read Braille and walked with a white cane. Never had I seen my husband or daughters face. I was blind when my husband prayed for me- then just like that- in a moment, after years of darkness I could see perfectly! It was miraculous! My daughter’s picture was on the dresser. I could see what my little girl and husband looked like, I could see the floor, the steps. Within seconds, my life had drastically changed. I could see, I could see!”
This report originates from the GLOBAL MEDICAL RESEARCH INSTITUTE. Their website claims that our mission is to investigate the effects of prayer in the resolution of conditions where the prognosis is typically poor, even with medical intervention. We are also developing randomized, controlled clinical trials of healing prayer effects.
Three questions came to my mind while reading all this:
- Are RCTs in prayer really needed? The believers already ‘know’ and will not trust the findings of the research, if they are not positive.
- Who do they try to convince the public with a case report that dates back 47 years?
- What do they think of Carl Sagan’s bon mot, ‘EXTRAORDINARY CLAIMS REQUIRE EXTRAORDINARY EVIDENCE’?
The drop in cases and deaths due to COVID-19 infections in India has been attributed to India’s national policy of using homeopathy. Early in the epidemic, the national “Ministry of AYUSH, recommended the use of Arsenic album 30 as preventive medicine against COVID-19. Its prophylactic use has been advised in states like Karnataka, Tamil Nadu, Kerala, and Maharashtra. The ‘OFFICIAL HOMEOPATHY RESOURCE’ is now claiming that homeopathy is the cause of the observed outcome:
And now the results of that policy and use are clear, even though skeptics and other scientists in the conventional paradigm are mystified as to why the drop is so dramatic. They know nothing about homeopathy and its history of successfully treating epidemics.
India has a population of 1 billion, 300 million people. Relative to this massive population the number of cases per day and especially the number of deaths per day are now exceptionally low. According to the Daily Mail:
“Scientists are trying to work out why coronavirus cases in India are falling when at one point it looked like the country might overtake the US as the worst-hit nation.
In September the country was reporting some 100,00 new cases per day, but that went into decline in October and is now sitting at around 10,000 per day – leaving experts struggling to explain why.”
END OF QUOTE
According to my sources, the number of daily new cases in India rose steadily to reach its maximum of almost 100000 new cases per day in mid-September. Thereafter, the figure fell in almost the same fashion as they had previously risen.

Currently, they have reached a plateau of about 13000 cases per day, and around 100 patients per day are reported to dies of COVID-19 every day. There are several possible contributors to these relatively positive outcomes:
- India has administered the Covid-19 vaccine to about 10 million people in one month since launching the world’s largest vaccination program on Jan. 16. However, this timing cannot explain the fall of cases before mid-January.
- The Indian government has attributed the dip in cases partly to mask-wearing, which is mandatory in public in India and violations can draw hefty fines.
- Large areas of India have reached herd immunity.
- Some of the various non-homeopathic remedies that have been recommended by the Ministry of AYUSH might be effective.
- There might be a host of other factors that I don’t know about.
- The figures coming out of India may not be reliable.
- The homeopathic remedy Arsenic album 30 might indeed be an effective preventative.
Which of these explanations are valid?
Most likely, it is not one but several working together. However, the hypothesis that homeopathy has anything to do with the course of the pandemic in India seems most unlikely. Apart from the fact that highly diluted homeopathic remedies are implausible and have not been shown to be effective, the timing of events is clearly against this explanation: if I am correctly informed, the homeopathic remedies were dished out months before the decline in cases started. In fact, simply going by the timing, one would need to assume that homeopathy led to the enormous increase before the remarkable drop.
Of course, it would be interesting to see the results of the homeopathy trials that allegedly started in India about 8 months ago. They could bring us closer to the truth. But somehow, I am not holding my breath.