Monthly Archives: September 2018
Endocrine therapy (ET) is often used to reduce the risk of recurrence in hormone receptor-expressing disease. It is associated with worsening of climacteric symptoms can therefore have a negative impact on the quality of life (QoL) of those affected. Homeopathy is sometimes recommended for management of hot flushes (HF), and a new study aimed to test whether it is effective.
In this multi-centre, double-blind, placebo-controlled RCT, women were included suffering from histologically proven non-metastatic localized breast cancer, with Eastern Cooperative Oncology Group-Performance Status (ECOG-PS) ≤ 1, treated for at least 1 month with adjuvant ET, and complaining about moderate to severe HF. Patients scheduled for chemotherapy, or radiotherapy, or those with associated pathology known to induce HF were excluded. After a 2- to 4-week placebo administration, patients were randomly assigned to receiving the homeopathic medicine complex Actheane® (arm A) or placebo (arm P). Randomization was stratified by adjuvant ET (taxoxifen/aromatase inhibitor) and recruiting site. HF scores (HFS) were calculated as the mean of HF frequencies before randomization, at 4, and at 8 weeks post-randomization (pre-, 4w,- and 8w-) weighted by a 4-level intensity scale. The primary endpoint was the variation between pre- and 4week-HFS. Secondary endpoints included HFS variation between pre- and 8week-HFS. Compliance and tolerance were assessed 8 weeks after randomization, and QoL and satisfaction were assessed at 4- and 8-week post-randomization.
In total, 138 patients were randomized (A, 65; P, 73). Median 4week-HFS absolute variation (A, - 2.9; P, - 2.5 points, p = 0.756) and relative decrease (A, - 17%; P, - 15%, p = 0.629) were not statistically different between the two arms. However, 4week-HFS decreased for 46 (75%) in A vs 48 (68%) patients in P arm. 4week-QoL was stable or improved for respectively 43 (72%) vs 51 (74%) patients (p = 0.470).
The authors concluded that the efficacy endpoint was not reached, and BRN-01 administration was not demonstrated as an efficient treatment to alleviate HF symptoms due to adjuvant ET in breast cancer patients. However, the study drug administration led to decreased HFS with a positive impact on QoL. Without any recommended treatment to treat or alleviate the HF-related disabling symptoms, Actheane® could be a promising option, providing an interesting support for better adherence to ET, thereby reducing the risk of recurrence with a good tolerance profile.
At the start of their abstract, the authors state that homeopathy might allow a better management of hot flushes (HF). Frankly, I fail to see the evidence for this statement. The only study I know of (by a known advocate of homeopathy) showed no effect of homeopathy.
Acthéane is a mixture marketed by Boiron of 5 ingredients:
– Actaea racemosa 4 CH : 0,5 mg
– Arnica montana 4 CH : 0,5 mg
– Glonoinum 4 CH : 0,5 mg
– Lachesis mutus 5 CH : 0,5 mg
– Sanguinaria canadensis 4 CH : 0,5 mg
I am not aware of evidence that this remedy might work.
If there is no plausible rationale for conducting a study, does that not mean it is ethically questionable to do it?
Apart from that, the study seems well-designed. It is not very well presented, but the paper is clear enough. Its results are as one would expect from a rigorous trial of homeopathy. The fact that the authors try to squeeze out some positive messages from this squarely negative study is, of course, pathetic. To mention in the abstract that 4week-HFS decreased for 46 (75%) in A vs 48 (68%) patients (not the primary outcome measure) in P arm is little more than an embarrassing tribute to the sponsor, in my view.
Boiron Canada state on their website that Acteane® is a homeopathic medicine used for the relief of perimenopause and menopause symptoms such as hot flashes, night sweats, sleep disorders, headache, irritability and mood swings.
 The benefits of Acteane, a new solution for women:
The benefits of Acteane, a new solution for women:
• Hormone-free
• Soy-free
• Can be associated with other treatments used during perimenopause
• Non-drowsy
• Chewable tablets
• Does not require water
WILL THEY NOW ADD ‘EFFECT-FREE’ TO THEIR LIST?
Do musculoskeletal conditions contribute to chronic non-musculoskeletal conditions? The authors of a new paper – inspired by chiropractic thinking, it seems – think so. Their meta-analysis was aimed to investigate whether the most common musculoskeletal conditions, namely neck or back pain or osteoarthritis of the knee or hip, contribute to the development of chronic disease.
The authors searched several electronic databases for cohort studies reporting adjusted estimates of the association between baseline neck or back pain or osteoarthritis of the knee or hip and subsequent diagnosis of a chronic disease (cardiovascular disease , cancer, diabetes, chronic respiratory disease or obesity).
There were 13 cohort studies following 3,086,612 people. In the primary meta-analysis of adjusted estimates, osteoarthritis (n= 8 studies) and back pain (n= 2) were the exposures and cardiovascular disease (n=8), cancer (n= 1) and diabetes (n= 1) were the outcomes. Pooled adjusted estimates from these 10 studies showed that people with a musculoskeletal condition have a 17% increase in the rate of developing a chronic disease compared to people without a musculoskeletal condition.
The authors concluded that musculoskeletal conditions may increase the risk of chronic disease. In particular, osteoarthritis appears to increase the risk of developing cardiovascular disease. Prevention and early
treatment of musculoskeletal conditions and targeting associated chronic disease risk factors in people with long
standing musculoskeletal conditions may play a role in preventing other chronic diseases. However, a greater
understanding about why musculoskeletal conditions may increase the risk of chronic disease is needed.
For the most part, this paper reads as if the authors are trying to establish a causal relationship between musculoskeletal problems and systemic diseases at all costs. Even their aim (to investigate whether the most common musculoskeletal conditions, namely neck or back pain or osteoarthritis of the knee or hip, contribute to the development of chronic disease) clearly points in that direction. And certainly, their conclusion that musculoskeletal conditions may increase the risk of chronic disease confirms this suspicion.
In their discussion, they do concede that causality is not proven: While our review question ultimately sought to assess a causal connection between common musculoskeletal conditions and chronic disease, we cannot draw strong conclusions due to poor adjustment, the analysis methods employed by the included studies, and a lack of studies investigating conditions other than OA and cardiovascular disease…We did not find studies that satisfied all of Bradford Hill’s suggested criteria for casual inference (e.g. none estimated dose–response effects) nor did we find studies that used contemporary causal inference methods for observational data (e.g. a structured identification approach for selection of confounding variables or assessment of the effects of unmeasured or residual confounders. As such, we are unable to infer a strong causal connection between musculoskeletal conditions and chronic diseases.
In all honesty, I would see this a little differently: If their review question ultimately sought to assess a causal connection between common musculoskeletal conditions and chronic disease, it was quite simply daft and unscientific. All they could ever hope is to establish associations. Whether these are causal or not is an entirely different issue which is not answerable on the basis of the data they searched for.
An example might make this clearer: people who have yellow stains on their 2nd and 3rd finger often get lung cancer. The yellow fingers are associated with cancer, yet the link is not causal. The association is due to the fact that smoking stains the fingers and causes cancer. What the authors of this new article seem to suggest is that, if we cut off the stained fingers of smokers, we might reduce the cancer risk. This is clearly silly to the extreme.
So, how might the association between musculoskeletal problems and systemic diseases come about? Of course, the authors might be correct and it might be causal. This would delight chiropractors because DD Palmer, their founding father, said that 95% of all diseases are caused by subluxation of the spine, the rest by subluxations of other joints. But there are several other and more likely explanations for this association. For instance, many people with a systemic disease might have had subclinical problems for years. These problems would prevent them from pursuing a healthy life-style which, in turn, resulted is musculoskeletal problems. If this is so, musculoskeletal conditions would not increase the risk of chronic disease, but chronic diseases would lead to musculoskeletal problems.
Don’t get me wrong, I am not claiming that this reverse causality is the truth; I am simply saying that it is one of several possibilities that need to be considered. The fact that the authors failed to do so, is remarkable and suggests that they were bent on demonstrating what they put in their conclusion. And that, to me, is an unfailing sign of poor science.
 The AMERICAN INSTITUTE OF HOMEOPATHY (AIH) is the oldest national medical association in the United States. The AIH’s mission is “to promote the science and art of homeopathic medicine, to safeguard the interests of the homeopathic medical profession, to improve the standards of homeopathic medical education, to educate the medical and scientific communities about the scientific basis for homeopathic medicine, and to increase public knowledge and acceptance of homeopathy as a medical specialty.”
The AMERICAN INSTITUTE OF HOMEOPATHY (AIH) is the oldest national medical association in the United States. The AIH’s mission is “to promote the science and art of homeopathic medicine, to safeguard the interests of the homeopathic medical profession, to improve the standards of homeopathic medical education, to educate the medical and scientific communities about the scientific basis for homeopathic medicine, and to increase public knowledge and acceptance of homeopathy as a medical specialty.”
The AIH is about to hold its annual conference. This year’s theme is “Tackling Patients with Severe Pathology”. The announcement reads as follows:
Homeopathy has been found to be effective in the great majority of patients suffering from infectious and autoimmune diseases. The limits of homeopathic treatment are encountered in the treatment of patients with Parkinson’s disease, ALS and late-stage cancers. After finding a way to treat patients with Parkinson’s disease with homeopathy, Dr. Saine began to apply this approach to cancer patients in stages III and IV. In this seminar, he will review case analysis, posology and case management for this cohort of patients.
We are fortunate to have the opportunity to learn from Dr. Saine in this seminar. He is recognized as one of the foremost homeopathic teachers and clinicians in the world, with special expertise in extremely difficult cases of severe and advanced pathology.
Who, for heaven sake, is this foremost homeopathic teachers and clinicians in the world, Dr Saine?, I asked myself after reading this (and even more so after listening to the rather spectacular video provided with the announcement). Here is what I found out about him:
Dr. Saine is a 1982 graduate of the National College of Naturopathic Medicine in Portland, Oregon. He is board-certified in homeopathy (1988) by the Homeopathic Academy of Naturopathic Physicians and has been teaching and lecturing on homeopathy since 1985. He is considered one of the world’s foremost experts on the subject of homeopathy.
And this is what non-doctor* Saine writes about medicine etc.:
The Organon of Medicine is a blueprint on how to practice medicine rationally and wisely through an integration of all the fundamental principles of medicine into a comprehensive whole. Unfortunately, to the detriment of the sick, very few homeopaths have delved, as Hahnemann did, into the practice of lifestyle medicine and the use of complementary care to homeopathy.
With rare exceptions, patients will present with a portion of their disease that ensues from an unhealthy environment or ways of living. The role of the physician is to determine in the equation of disease what is primarily due to an untuned vital force versus a causa occasionalis, as both will have to be addressed in due time.
After reading and listening to all this I am mildly shocked.
It does not seem to me that the AIH is fit for purpose. Neither am I convinced that non-doctor Saine should be let near any patient, let alone one with cancer or another severe pathology.
There should be a law protecting patients from this sort of thing!
[*in the context of healthcare, a doctor is for me someone who has studied medicine]Fish oil (omega-3 PUFA) preparations are today extremely popular and amongst the best-researched dietary supplement. During the 1970s, two Danish scientists, Bang and Dyerberg, remarked that Greenland Eskimos had a baffling lower prevalence of coronary artery disease than mainland Danes. They also noted that their diet contained large amounts of seal and whale blubber and suggested that this ‘Eskimo-diet’ was a key factor in the lower prevalence. Subsequently, a flurry of research stared to investigate the phenomenon, and it was shown that the ‘Eskimo-diet’ contained unusually high concentrations of omega-3 polyunsaturated fatty acids from fish oils (seals and whales feed predominantly on fish).
Initial research also demonstrated that the regular consumption of fish oil has a multitude of cardiovascular and anti-inflammatory effects. This led to the promotion of fish oil supplements for a wide range of conditions. Meanwhile, many of these encouraging findings have been overturned by more rigorous studies, and the enthusiasm for fish oil supplements has somewhat waned. But now, a new paper has come out with surprising findings.
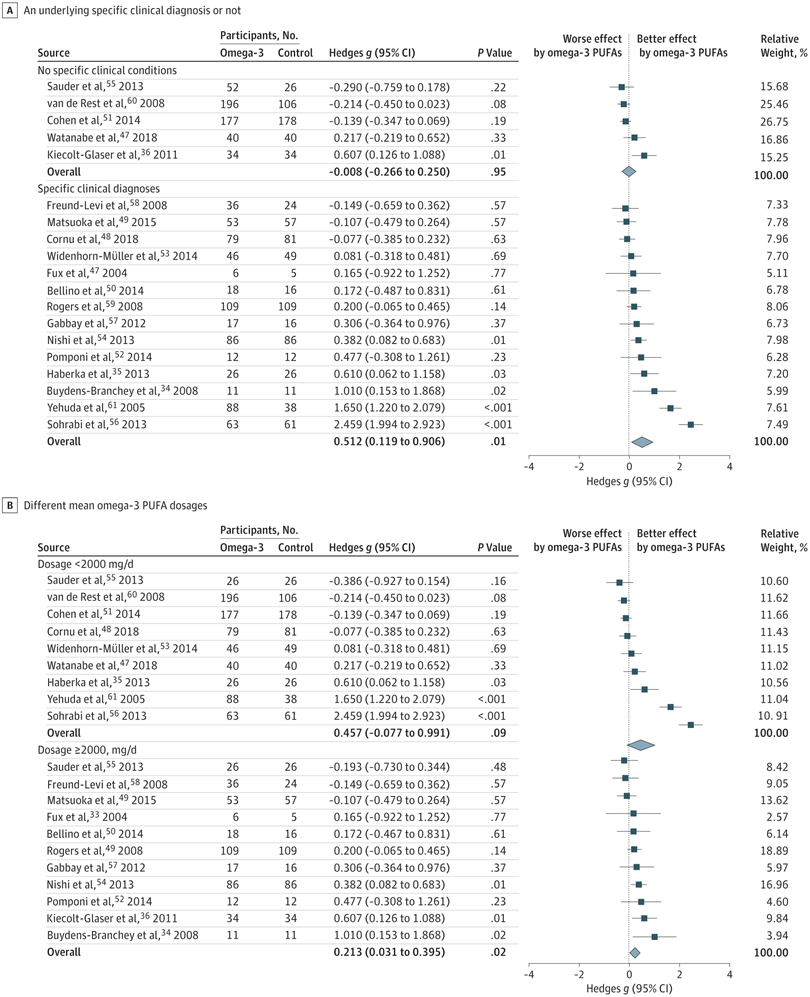
The objective of this meta-analysis was to evaluate the association of anxiety symptoms with omega-3 PUFA treatment compared with controls in varied populations.
A search was performed of clinical trials assessing the anxiolytic effect of omega-3 PUFAs in humans, in either placebo-controlled or non–placebo-controlled designs. Of 104 selected articles, 19 entered the final data extraction stage. Two authors independently extracted the data according to a predetermined list of interests. A random-effects model meta-analysis was performed. Changes in the severity of anxiety symptoms after omega-3 PUFA treatment served as the main endpoint.
In total, 1203 participants with omega-3 PUFA treatment and 1037 participants without omega-3 PUFA treatment showed an association between clinical anxiety symptoms among participants with omega-3 PUFA treatment compared with control arms. Subgroup analysis showed that the association of treatment with reduced anxiety symptoms was significantly greater in subgroups with specific clinical diagnoses than in subgroups without clinical conditions. The anxiolytic effect of omega-3 PUFAs was significantly better than that of controls only in subgroups with a higher dosage (at least 2000 mg/d) and not in subgroups with a lower dosage (<2000 mg/d).
The authors concluded that this review indicates that omega-3 PUFAs might help to reduce the symptoms of clinical anxiety. Further well-designed studies are needed in populations in whom anxiety is the main symptom.
I think this is a fine meta-analysis reporting clear results. I doubt that this paper truly falls under the umbrella of alternative medicine, but fish oil is a popular food supplement and should be mentioned on this blog. Of course, the average effect size is modest, but the findings are nevertheless intriguing.
Samuel Hahnemann invented homeopathy about 200 years ago. His placebos were better than (or not as bad as) the ‘heroic’ medicine of his time which frequently was more dangerous than the disease it aimed to cure. Thus, homeopathy took Germany by storm. When, about 100 years ago, medicine finally became scientific and was able to offer more and more effective treatments, the popularity of homeopathy began to wane. Yet, before its natural demise, during the Third Reich, it received a significant boost from Nazi-greats such as Hess and Himmler. After this nightmare was over, German homeopathy went into another slow decline. But when the New Age movement and the current boom in alternative medicine reached Germany, homeopathy seemed to thrive once again.
In the 1990s evidence-based medicine (EBM) grew into one of the central concepts of medicine. In Germany, however, EBM had a relatively hard time to get established. This might be one of the reasons why homeopathy continued to prosper, despite the arrival of ever clearer evidence that highly diluted homeopathic remedies are pure placebos. While, in the UK, we had an increasingly lively debate about the uselessness of homeopathy, Germany remained the promised land of homeopathy. Sales figures of homeopathics continued to increase steadily and reached a level of about half a billion Euros per annum.
The golden age of German homeopathy had dawned:
- The media, often sponsored by homeopathic interest groups, kept on promoting homeopathy largely unopposed.
- The mighty Carstens Stiftung worked tirelessly to promote it.
- Homeopathy became established in many medical schools.
- Homeopathy was available and often advertised in almost all pharmacies.
- The public was convinced that homeopathy worked.
- The Heilpraktiker adopted homeopathy fully.
- The medical and other conventional healthcare professions embraced it to a large degree.
- The adult education institutes (Volkshochschulen) offered courses.
- Politicians were squarely on the side of homeopathy,
- Health insurances, paid for it.
Of course, there were also some (and always had been) opposing voiced and organisations, such as the GWUP (the German sceptic organisation), for example. But somehow, they remained relatively low-key. When, every now and then, courageous journalists dared to think of a critical take on homeopathy, they had to search far and wide to find a German-speaking expert who was willing or able to tell them the truth: that homeopathy is neither biologically plausible nor evidence-based and therefore an expensive, potentially harmful waste of money that makes a mockery of EBM. During this period, journalists (far too) often asked me for some critical comments. I hardly ever published my research in German, but they nevertheless would find me via my Medline-listed papers. I often felt like a very lone voice in a German desert.
For the German homeopathic industry, I evidently was more than just a lone voice. Unbeknown to me, they clubbed together and financed a PR-man/journalist (at the tune of Euro 30 000/year) to write as many defamatory articles about me as he could muster. First, I was bewildered by his activity, then I tried to communicate with him (only to get mis-quoted), and eventually I ignored his writings. Yet, a German investigative journalist found Fritzsche’s one-sided activities offensive and started investigating. His research and subsequent article disclosed the fact that he was being paid by the homeopathic industry. Once I learn about this scandal, I wrote to some of the financiers directly and asked for an explanation. As a result, they discontinued their sponsorship. Shortly afterwards, Fritzsche committed suicide.
At heart, I have always been an optimist and strongly believe that in medicine the truth, in this case the evidence, will always prevail, no matter what obstacles others might put in its way. Recent developments seem to suggest that I might be right.
In the last few years, several individuals in Germany have, from entirely different angles, taken a fresh look at the evidence on homeopathy and found it to be desperately wanting. Independent of each other, they published articles and books about their research and insights. Here are 5 examples:
Die Homöopathie-Lüge: So gefährlich ist die Lehre von den weißen Kügelchen, Christian Weymayr, Nicole Heißmann, 2012
In Sachen Homöopathie: Eine Beweisaufnahme, Norbert Aust, 2013
Homöopathie neu gedacht: Was Patienten wirklich hilft, Natalie Grams, 2015
Der Glaube an die Globuli: Die Verheißungen der Homöopathie, Norbert Schmacke, Bernd Hontschik, 2015
Der wahrscheinlich teuerste Zucker der Welt: Was Sie über Homöopathie und Alternativmedizin wissen sollten, Oliver Grunau, 2017
Inevitably, these individuals came into contact with each other and subsequently founded several working-groups to discuss their concerns and coordinate their activities. Thus the INH and the Muensteraner Kreis were born. So, now we have at least three overlapping groups of enthusiastic, multidisciplinary experts who voluntarily work towards informing the German public that paying for homeopathy out of public funds is unethical, nonsensical and not in the interest of progress:
- the GWUP,
- the INH
- and the Muensteraner Kreis.
No wonder then, that the German homeopathic industry and other interested parties got worried. When they realised that (presumably due to the work of these altruistic enthusiasts) the sales figures of homeopathics in Germany had, for the first time since many years, started declining, they panicked.
Their reaction was, as far as I can see, similar to their previous response to criticism: they started a media campaign in an attempt to sway public opinion. And just like before, they have taken to employing PR-people who currently spend their time defaming all individuals voicing criticism of homeopathy in Germany. Their prime targets are those experts who are most exposed to activities of responsibly informing the public about homeopathy via lectures, publications social media, etc. All of us currently receive floods of attack, insults and libellous defamations. As before (innovation does not seem to be a hallmark of homeopathy), these attacks relate to claims that:
- we are incompetent,
- we do not care about the welfare of patients,
- we are habitual liars,
- we are on the payroll of the pharmaceutical industry,
- we aim at limiting patient choice,
- we do what we do because we crave the limelight.
So, what is going to happen?
I cannot read tea leaves but am nevertheless sure of a few things:
- The German homeopathy lobby will not easily give up; after all, they have half a billion Euros per year to lose.
- They will not argue on the basis of science or evidence, because they know that neither are in their favour.
- They will fight dirty and try to defame everyone who stands in their way.
- They will use their political influence and their considerable financial power.
AND YET THEY WILL LOSE!
Not because we are so well organised or have great resources – in fact, as far as I can see, we have none – but because, in medicine, the evidence is invincible and will eventually prevail. Progress might be delayed, but it cannot be halted by those who cling to an obsolete dogma.
Proof of Principle or Concept studies are investigations usually for an early stage of clinical drug development when a compound has shown potential in animal models and early safety testing. This step often links between Phase-I and dose ranging Phase-II studies. These small-scale studies are designed to detect a signal that the drug is active on a patho-physiologically relevant mechanism, as well as preliminary evidence of efficacy in a clinically relevant endpoint.
For therapies that have been in use for many years, proof of concept studies are unusual to say the least. A proof of concept study of osteopathy has never been heard of. This is why I was fascinated by this new paper. The objective of this ‘proof of concept’ study was to evaluate the effect of osteopathic manipulative therapy (OMTh) on chronic symptoms of multiple sclerosis (MS).
Patients (n=22) with MS received 5 forty-minute MS health education sessions (control group) or 5 OMTh sessions (OMTh group). All participants completed a questionnaire that assessed their level of clinical disability, fatigue, depression, anxiety, and quality of life before the first session, one week after the final session, and 6 months after the final session. The Extended Disability Status Scale, a modified Fatigue Impact Scale, the Beck Depression Inventory-II, the Beck Anxiety Inventory, and the 12-item Short Form Health Survey were used to assess clinical disability, fatigue, depression, anxiety, and quality of life, respectively. In the OMTh group, statistically significant improvements in fatigue and depression were found one week after the final session. A non-significant increase in quality of life was also found in the OMTh group one week after the final session.
The authors concluded that the results demonstrate that OMTh should be considered in the treatment of patients with chronic symptoms of MS.
Who said that reading alternative medicine research papers is not funny? I for one laughed heartily when I read this (no need at all to go into the many obvious flaws of the study). Calling a pilot study ‘proof of concept’ is certainly not without hilarity. Drawing definitive conclusions about the effectiveness of OMTh is outright laughable. But issuing a far-reaching recommendation for use of OMTh in MS is just better than the best comedy. This had me in stiches!
I congratulate the Journal of the American Osteopathic Association and the international team of authors for providing us with such fun.
“An exhaustive study of homeopathic remedies for Eczema“, this is the title of an article I just stumbled across. It leaves no doubt that homeopathy is effective for eczema (which is also what I was told all those years ago when I trained in a homeopathic hospital). Here are a few excerpts from the article:
The appropriate internal remedy will usually be one of the following, according to the indications:
Aconite
In the simpler forms of eczema, and when there is much febrile disturbance. Acute cases, with stinging and pricking of the skin, in plethoric persons.
Alumina
Hard crusts on the scalp, face and extremities. Gnawing itching, worse in the evening, not relieved by scratching. Aggravated on alternate days and from eating new potatoes. Dryness of the skin.Constipation.
Ammonium carbonicum
Eczema in the bends of the extremities. Excoriations between the legs, and about the anus and genitals. Violent itching relieved by scratching. Aggravated by either cold applications or hot poultices. In children.
Ammonium muriaticum
Anacardium orientale
Acute eczema on the face, neck and chest. Intense itching usually aggravated, but occasionally relieved by scratching. Redness of the skin with eruption of small vesicles. Sensitiveness to draught.
Antimonium crudum
Pustular eczema about the face and joints. Painful cracks in the corners of the mouth. Violent itching and burning, better in the open air, worse after bathing. Thick, heavy, yellow crusts upon the face. Gastric derangement with thick white coated tongue. In children who grow fat.
Antimonium tartaricum
Eruptions about the nose and eyes, neck and shoulders, and back of the ears. Vesicles surrounded by a red areola. Pustules, as large as peas. Itching worse in the evening, better in the open air. Eruption leaves bluish-red stains upon the face. Child wants to be carried; cries if touched.Desire for acids ; aversion to milk. Rattling cough.
Apis mellifica
Red and edematous skin, with burning and stinging. Better from cold applications, worse after warm applications. Large vesicles. Urine scanty and high colored.
Argentum nitricum
Eczema on the genitals. Urging to urinate. In children who eat too much sweets.
Arsenicum album
Eczema on the face, legs and genitals. Intense burning of the surface. Itching worse during the first hours of sleep. Better from external heat ; worse from cold or from scratching. Dry scaly eruption with parchment-like skin. Falling out of hair in patches. Useful in chronic cases.
Arundo
Eruption on the chest, upper extremities and behind the ears. Intolerable itching, crawling sensation, especially over the loins and shoulders. In young children.
Astacus fluviatilis
Thick crusts on the scalp. Enlargement of the lymphatic glands. Clay colored stools.
Aurum muriaticum
Smarting, itching papular eruption on the lips or above the pubis. Constant desire to be out in the open air. In corpulent old people. After abuse of mercury.
END OF QUOTE
And the evidence, where is the evidence for these seemingly detailed recommendations?
The answer is, there is none, at least not in this article.
So, I look into Medline. Apart from some observational studies, the most recent relevant paper on controlled clinical trials happens to be my very own systematic review published in the British Journal of Dermatology entitled “Homeopathy for eczema: a systematic review of controlled clinical trials.” Here is its abstract:
BACKGROUND:
Homeopathy is often advocated for patients with eczema.
OBJECTIVES:
This article systematically reviews the evidence from controlled clinical trials of any type of homeopathic treatment for any type of eczema.
METHODS:
Electronic searches were conducted in Medline, Embase and the Cochrane Library with no restrictions on time or language. In addition, the bibliographies of the retrieved articles and our departmental files were hand searched. All controlled trials of homeopathy in patients with eczema were considered. Their methodological quality was estimated using the Jadad score.
RESULTS:
One randomized and two nonrandomized clinical trials met the inclusion criteria. All were methodologically weak. None demonstrated the efficacy of homeopathy.
CONCLUSIONS:
The evidence from controlled clinical trials therefore fails to show that homeopathy is an efficacious treatment for eczema.
________________________________________________________________
So, what does that tell us?
I think it demonstrates the following relevant points:
- Homeopaths seem convinced to be able to treat eczema effectively.
- They teach this to junior clinicians and tell it to their patients.
- They trumpet this message out on the internet (a Google search on ‘homeopathy for eczema’ generates 242 000 hits).
- They even claim that they have done ‘exhaustive studies’ that prove their point.
- Yet, the actual evidence fails to show that homeopathy works for eczema.
Does that mean homeopaths are lying?
Does that mean homeopaths mislead their patients thus causing needless suffering?
Does that mean homeopaths care more about their cash-flow than the welfare of their patients?
What do you think?
Osteopathy is a form of manual therapy invented by the American Andrew Taylor Still (1828-1917). Today, US osteopaths (doctors of osteopathy or DOs) practise no or little manual therapy; they are fully recognised as medical doctors who can specialise in any medical field after their training which is almost identical with that of MDs. Outside the US, osteopaths practice almost exclusively manual treatments and are considered alternative practitioners. This post deals with the latter category of osteopaths.
Still defined his original osteopathy as a science which consists of such exact, exhaustive, and verifiable knowledge of the structure and function of the human mechanism, anatomical, physiological and psychological, including the chemistry and physics of its known elements, as has made discoverable certain organic laws and remedial resources, within the body itself, by which nature under the scientific treatment peculiar to osteopathic practice, apart from all ordinary methods of extraneous, artificial, or medicinal stimulation, and in harmonious accord with its own mechanical principles, molecular activities, and metabolic processes, may recover from displacements, disorganizations, derangements, and consequent disease, and regained its normal equilibrium of form and function in health and strength.
Based on such vague and largely nonsensical statements, traditional osteopaths feel entitled to offer treatments for most human diseases, conditions and symptoms. The studies they produce to back up their claims tend to be as poor as Still’s original assumptions were fantastic.
Here is an apt example:
The aim of this new study was to study the effect of osteopathic manipulation on pain relief and quality of life improvement in hospitalized oncology geriatric patients.
The researchers conducted a non-randomized controlled clinical trial with 23 cancer patients. They were allocated to two groups: the study group (OMT [osteopathic manipulative therapy] group, N = 12) underwent OMT in addition to physiotherapy (PT), while the control group (PT group, N = 12) underwent only PT. Included were postsurgical cancer patients, male and female, age ⩾65 years, with an oncology prognosis of 6 to 24 months and chronic pain for at least 3 months with an intensity score higher than 3, measured with the Numeric Rating Scale. Exclusion criteria were patients receiving chemotherapy or radiotherapy treatment at the time of the study, with mental disorders (Mini-Mental State Examination [MMSE] = 10-20), with infection, anticoagulation therapy, cardiopulmonary disease, or clinical instability post-surgery. Oncology patients were admitted for rehabilitation after cancer surgery. The main cancers were colorectal cancer, osteosarcoma, spinal metastasis from breast and prostatic cancer, and kidney cancer.
The OMT, based on osteopathic principles of body unit, structure-function relationship, and homeostasis, was designed for each patient on the basis of the results of the osteopathic examination. Diagnosis and treatment were founded on 5 models: biomechanics, neurologic, metabolic, respiratory-circulatory, and behaviour. The OMT protocol was administered by an osteopath with clinical experience of 10 years in one-on-one individual sessions. The techniques used were: dorsal and lumbar soft tissue, rib raising, back and abdominal myofascial release, cervical spine soft tissue, sub-occipital decompression, and sacroiliac myofascial release. Back and abdominal myofascial release techniques are used to improve back movement and internal abdominal pressure. Sub-occipital decompression involves traction at the base of the skull, which is considered to release restrictions around the vagus nerve, theoretically improving nerve function. Sacroiliac myofascial release is used to improve sacroiliac joint movement and to reduce ligament tension. Strain-counter-strain and muscle energy technique are used to diminish the presence of trigger points and their pain intensity. OMT was repeated once every week during 4 weeks for each group, for a total of 4 treatments. Each treatment lasted 45 minutes.
At enrolment (T0), the patients were evaluated for pain intensity and quality of life by an external examiner. All patients were re-evaluated every week (T1, T2, T3, and T4) for pain intensity, and at the end of the study treatment (T4) for quality of life.
The OMT added to physiotherapy produced a significant reduction in pain both at T2 and T4. The difference in quality of life improvements between T0 and T4 was not statistically significant. Pain improved in the PT group at T4. Between-group analysis of pain and quality of life did not show any significant difference between the two treatments.
The authors concluded that our study showed a significant improvement in pain relief and a nonsignificant improvement in quality of life in hospitalized geriatric oncology patients during osteopathic manipulative treatment.
GOOD GRIEF!
Where to begin?
Even if there had been a difference in outcome between the two groups, such a finding would not have shown an effect of OMT per se. More likely, it would have been due to the extra attention and the expectation in the OMT group (or caused by the lack of randomisation). The A+B vs B design used for this study does not control for non-specific effects. Therefore it is incapable of establishing a causal relationship between the therapy and the outcome.
As it turns out, there were no inter-group differences. How can this be? I have often stated that A+B is always more than B alone. And this is surely true!
So, how can I explain this?
As far as I can see, there are two possibilities:
- The study was underpowered, and thus an existing difference was not picked up.
- The OMT had a detrimental effect on the outcome measures thus neutralising the positive effects of the extra attention and expectation.
And which possibility does apply in this case?
Nobody can know from these data.
Integrative Cancer Therapies, the journal that published this paper, states that it focuses on a new and growing movement in cancer treatment. The journal emphasizes scientific understanding of alternative and traditional medicine therapies, and the responsible integration of both with conventional health care. Integrative care includes therapeutic interventions in diet, lifestyle, exercise, stress care, and nutritional supplements, as well as experimental vaccines, chrono-chemotherapy, and other advanced treatments. I feel that the editors should rather focus more on the quality of the science they publish.
My conclusion from all this is the one I draw so depressingly often: fatally flawed science is not just useless, it is unethical, gives clinical research a bad name, hinders progress, and can be harmful to patients.
The UK Royal Pharmaceutical Society have published a quick reference guide on homeopathy. In it, they make the following 5 ‘key points’:
- The Royal Pharmaceutical Society (RPS) does not endorse homeopathy as a form of treatment because there is no scientific basis for homeopathy nor any evidence to support the clinical efficacy of homeopathic products beyond a placebo effect.
- The RPS does not support the prescribing of homeopathic products on the NHS.
- Pharmacists should ensure, wherever possible, that patients do not stop taking their prescribed conventional medication, if they are taking or are considering taking a homeopathic product.
- Pharmacists must be aware that patients requesting homeopathic products may have serious underlying undiagnosed medical conditions which may require referral to another healthcare professional.
- Pharmacists must advise patients considering a homeopathic product about their lack of efficacy beyond that of a placebo.
 This publication is a few months old, but I only saw it recently. It could not be clearer and it is much more to the point than the General Pharmaceutical Council’s ‘Standards for Pharmacy Professionals‘ which state:
This publication is a few months old, but I only saw it recently. It could not be clearer and it is much more to the point than the General Pharmaceutical Council’s ‘Standards for Pharmacy Professionals‘ which state:
People receive safe and effective care when pharmacy professionals reflect on the application of their knowledge and skills and keep them up-to-date, including using evidence in their decision making. A pharmacy professional’s knowledge and skills must develop over the course of their career to reflect the changing nature of healthcare, the population they provide care to and the roles they carry out. There are a number of ways to meet this standard and below are examples of the attitudes and behaviours expected.
People receive safe and effective care when pharmacy professionals:
- recognise and work within the limits of their knowledge and skills, and refer to others when needed
- use their skills and knowledge, including up-to-date evidence, to deliver care and improve the quality of care they provide
- carry out a range of continuing professional development (CPD) activities relevant to their practice
- record their development activities to demonstrate that their knowledge and skills are up to date
- use a variety of methods to regularly monitor and reflect on their practice, skills and knowledge
The two statements together should suffice to finally get some sense into UK pharmacies when it comes to the sale of homeopathic remedies. What is needed now, I think, is an (under-cover?) investigation to see how many UK community pharmacists abide by this guidance.
If anyone has the means to conduct it, I would be delighted to advise them on the best methodology.
I remember reading this paper entitled ‘Comparison of acupuncture and other drugs for chronic constipation: A network meta-analysis’ when it first came out. I considered discussing it on my blog, but then decided against it for a range of reasons which I shall explain below. The abstract of the original meta-analysis is copied below:
The objective of this study was to compare the efficacy and side effects of acupuncture, sham acupuncture and drugs in the treatment of chronic constipation. Randomized controlled trials (RCTs) assessing the effects of acupuncture and drugs for chronic constipation were comprehensively retrieved from electronic databases (such as PubMed, Cochrane Library, Embase, CNKI, Wanfang Database, VIP Database and CBM) up to December 2017. Additional references were obtained from review articles. With quality evaluations and data extraction, a network meta-analysis (NMA) was performed using a random-effects model under a frequentist framework. A total of 40 studies (n = 11032) were included: 39 were high-quality studies and 1 was a low-quality study. NMA showed that (1) acupuncture improved the symptoms of chronic constipation more effectively than drugs; (2) the ranking of treatments in terms of efficacy in diarrhoea-predominant irritable bowel syndrome was acupuncture, polyethylene glycol, lactulose, linaclotide, lubiprostone, bisacodyl, prucalopride, sham acupuncture, tegaserod, and placebo; (3) the ranking of side effects were as follows: lactulose, lubiprostone, bisacodyl, polyethylene glycol, prucalopride, linaclotide, placebo and tegaserod; and (4) the most commonly used acupuncture point for chronic constipation was ST25. Acupuncture is more effective than drugs in improving chronic constipation and has the least side effects. In the future, large-scale randomized controlled trials are needed to prove this. Sham acupuncture may have curative effects that are greater than the placebo effect. In the future, it is necessary to perform high-quality studies to support this finding. Polyethylene glycol also has acceptable curative effects with fewer side effects than other drugs.
END OF 1st QUOTE
This meta-analysis has now been retracted. Here is what the journal editors have to say about the retraction:
After publication of this article [1], concerns were raised about the scientific validity of the meta-analysis and whether it provided a rigorous and accurate assessment of published clinical studies on the efficacy of acupuncture or drug-based interventions for improving chronic constipation. The PLOS ONE Editors re-assessed the article in collaboration with a member of our Editorial Board and noted several concerns including the following:
- Acupuncture and related terms are not mentioned in the literature search terms, there are no listed inclusion or exclusion criteria related to acupuncture, and the outcome measures were not clearly defined in terms of reproducible clinical measures.
- The study included acupuncture and electroacupuncture studies, though this was not clearly discussed or reported in the Title, Methods, or Results.
- In the “Routine paired meta-analysis” section, both acupuncture and sham acupuncture groups were reported as showing improvement in symptoms compared with placebo. This finding and its implications for the conclusions of the article were not discussed clearly.
- Several included studies did not meet the reported inclusion criteria requiring that studies use adult participants and assess treatments of >2 weeks in duration.
- Data extraction errors were identified by comparing the dataset used in the meta-analysis (S1 Table) with details reported in the original research articles. Errors included aspects of the study design such as the experimental groups included in the study, the number of study arms in the trial, number of participants, and treatment duration. There are also several errors in the Reference list.
- With regard to side effects, 22 out of 40 studies were noted as having reported side effects. It was not made clear whether side effects were assessed as outcome measures for the other 18 studies, i.e. did the authors collect data clarifying that there were no side effects or was this outcome measure not assessed or reported in the original article. Without this clarification the conclusion comparing side effect frequencies is not well supported.
- The network geometry presented in Fig 5 is not correct and misrepresents some of the study designs, for example showing two-arm studies as three-arm studies.
- The overall results of the meta-analysis are strongly reliant on the evidence comparing acupuncture versus lactulose treatment. Several of the trials that assessed this comparison were poorly reported, and the meta-analysis dataset pertaining to these trials contained data extraction errors. Furthermore, potential bias in studies assessing lactulose efficacy in acupuncture trials versus lactulose efficacy in other trials was not sufficiently addressed.
While some of the above issues could be addressed with additional clarifications and corrections to the text, the concerns about study inclusion, the accuracy with which the primary studies’ research designs and data were represented in the meta-analysis, and the reporting quality of included studies directly impact the validity and accuracy of the dataset underlying the meta-analysis. As a consequence, we consider that the overall conclusions of the study are not reliable. In light of these issues, the PLOS ONE Editors retract the article. We apologize that these issues were not adequately addressed during pre-publication peer review.
LZ disagreed with the retraction. YM and XD did not respond.
END OF 2nd QUOTE
Let me start by explaining why I initially decided not to discuss this paper on my blog. Already the first sentence of the abstract put me off, and an entire chorus of alarm-bells started ringing once I read further.
- A meta-analysis is not a ‘study’ in my book, and I am somewhat weary of researchers who employ odd or unprecise language.
- We all know (and I have discussed it repeatedly) that studies of acupuncture frequently fail to report adverse effects (in doing this, their authors violate research ethics!). So, how can it be a credible aim of a meta-analysis to compare side-effects in the absence of adequate reporting?
- The methodology of a network meta-analysis is complex and I know not a lot about it.
- Several things seemed ‘too good to be true’, for instance, the funnel-plot and the overall finding that acupuncture is the best of all therapeutic options.
- Looking at the references, I quickly confirmed my suspicion that most of the primary studies were in Chinese.
In retrospect, I am glad I did not tackle the task of criticising this paper; I would probably have made not nearly such a good job of it as PLOS ONE eventually did. But it was only after someone raised concerns that the paper was re-reviewed and all the defects outlined above came to light.
While some of my concerns listed above may have been trivial, my last point is the one that troubles me a lot. As it also related to dozens of Cochrane reviews which currently come out of China, it is worth our attention, I think. The problem, as I see it, is as follows:
- Chinese (acupuncture, TCM and perhaps also other) trials are almost invariably reporting positive findings, as we have discussed ad nauseam on this blog.
- Data fabrication seems to be rife in China.
- This means that there is good reason to be suspicious of such trials.
- Many of the reviews that currently flood the literature are based predominantly on primary studies published in Chinese.
- Unless one is able to read Chinese, there is no way of evaluating these papers.
- Therefore reviewers of journal submissions tend to rely on what the Chinese review authors write about the primary studies.
- As data fabrication seems to be rife in China, this trust might often not be justified.
- At the same time, Chinese researchers are VERY keen to publish in top Western journals (this is considered a great boost to their career).
- The consequence of all this is that reviews of this nature might be misleading, even if they are published in top journals.
I have been struggling with this problem for many years and have tried my best to alert people to it. However, it does not seem that my efforts had even the slightest success. The stream of such reviews has only increased and is now a true worry (at least for me). My suspicion – and I stress that it is merely that – is that, if one would rigorously re-evaluate these reviews, their majority would need to be retracted just as the above paper. That would mean that hundreds of papers would disappear because they are misleading, a thought that should give everyone interested in reliable evidence sleepless nights!
So, what can be done?
Personally, I now distrust all of these papers, but I admit, that is not a good, constructive solution. It would be better if Journal editors (including, of course, those at the Cochrane Collaboration) would allocate such submissions to reviewers who:
- are demonstrably able to conduct a CRITICAL analysis of the paper in question,
- can read Chinese,
- have no conflicts of interest.
In the case of an acupuncture review, this would narrow it down to perhaps just a handful of experts worldwide. This probably means that my suggestion is simply not feasible.
But what other choice do we have?
One could oblige the authors of all submissions to include full and authorised English translations of non-English articles. I think this might work, but it is, of course, tedious and expensive. In view of the size of the problem (I estimate that there must be around 1 000 reviews out there to which the problem applies), I do not see a better solution.
(I would truly be thankful, if someone had a better one and would tell us)