risk/benefit
I usually take ‘market reports’ with a pinch of salt. Having said that, this document makes some rather interesting predictions:
The size of the market for so-called alternative medicine (SCAM) is projected to expand from USD 147.7 billion in 2023 to approximately USD 1489.4 billion by the year 2033. This projection indicates a remarkable Compound Annual Growth Rate (CAGR) of 26% over the forecast period.
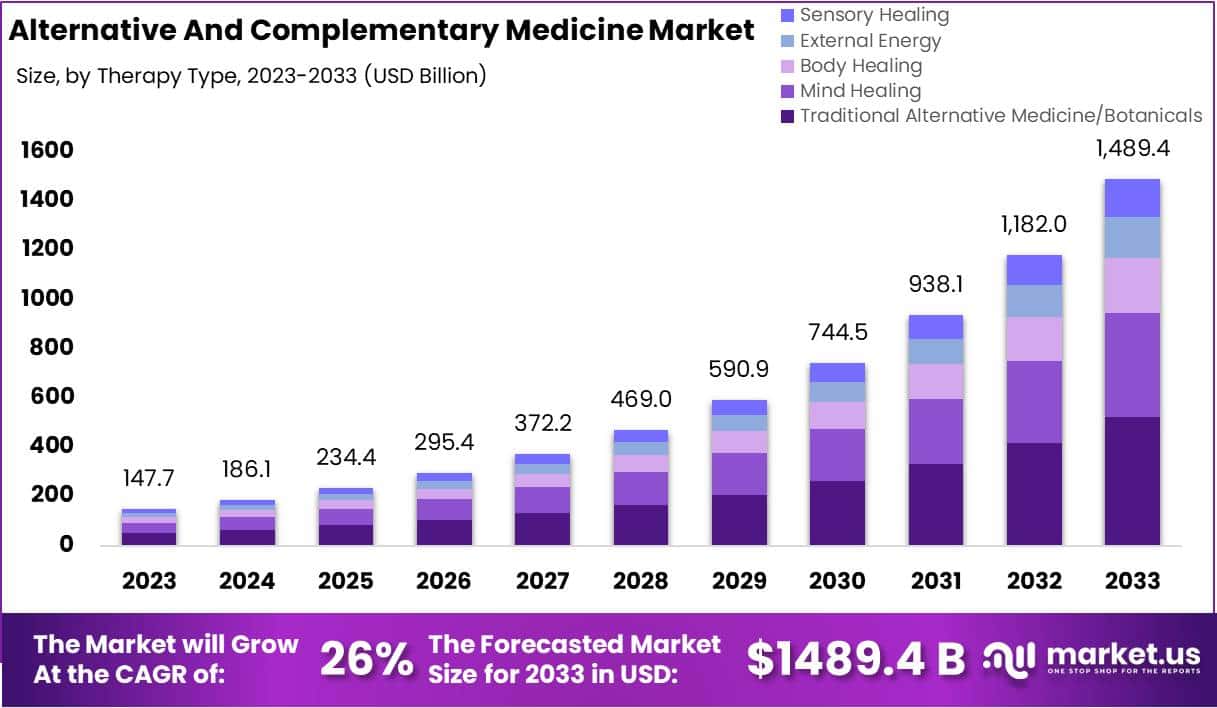
The market for SCAM is experiencing significant growth, fueled by increasing consumer interest in natural and holistic health solutions. This trend reflects a broader shift in societal attitudes towards health and wellness, emphasizing preventive care and natural health practices.
The market’s dynamics are influenced by various factors, including consumer preferences, regulatory standards, and evolving perceptions of health and wellness. As the popularity of these alternative therapies grows, it is crucial for individuals to consult with healthcare professionals to ensure that these non-conventional approaches are safely and effectively incorporated into their overall health regimen. The increasing acceptance of SCAM underscores a collective move towards more personalized and holistic healthcare solutions, resonating with today’s health-conscious consumers.
In 2023, Traditional Alternative Medicine/Botanicals led the market, capturing a 35.2% share, which reflects a strong consumer inclination towards these treatments. Dietary Supplements were prominent in the market, securing a 25.1% share in 2023, which underscores the high consumer demand for nutritional aids. Direct Sales were the most favored distribution channel, accounting for 43.2% of the market share in 2023, which indicates their significant impact on guiding consumer purchases. Pain Management was the predominant application area, holding a 24.9% market share in 2023, propelled by the growing acknowledgment of non-pharmacological treatment options. Adults represented a substantial portion of the market, making up 62.33% in 2023, signifying a marked preference for SCAM therapies within this age group. Europe stood out as the market leader, claiming a 42.6% share in 2023, a position supported by widespread acceptance, governmental backing, and an increasing elderly population. The regions of North America and Asia-Pacific are highlighted as areas with potential, signaling opportunities for market expansion beyond the European stronghold in the upcoming years.
Leading Market Players Are:
- Columbia Nutritional
- Nordic Nutraceuticals
- Ramamani Iyengar Memorial Yoga Institute
- The Healing Company Ltd.
- John Schumacher Unity Woods Yoga Centre
- Sheng Chang Pharmaceutical Company
- Pure encapsulations LLC.
- Herb Pharm
- AYUSH Ayurvedic Pte Ltd.
Recent developments:
- In December 2023, Adoratherapy launched the Alkemie Chakra Healing Line, an aromatherapy range aimed at harmonizing the seven chakras.
- Coworth Park introduced the Hebridean Sound Treatment in October 2023, merging traditional Hebridean sounds with guided meditation to offer a novel, restorative wellness experience.
- The World Health Organization released draft guidelines in September 2023 for the safe, effective application of traditional medicines.
- Telehealth services, expanding significantly in August 2023, have broadened the reach of SCAM, enhancing patient access to these treatments.
Traditional herbal medicine (THM) is frequently used in pediatric populations. This is perticularly true in many low-income countries. Yet THM has been associated with a range of adverse events, including liver toxicity, renal failure, and allergic reactions. Despite these concerns, its impact on multi-organ dysfunction syndrome (MODS) risk has so far not been thoroughly investigated.
This study aimed to investigate the incidence and predictors of MODS in a pediatric intensive care unit (PICU) in Ethiopia, with a focus on the association between THM use and the risk of MODS. It was designed as a single-center prospective cohort study conducted at a PICU in the university of Gondar Comprehensive Specialized hospital, Northwest Ethiopia. The researchers enrolled eligible patients aged one month to 18 years admitted to the PICU during the study period. Data on demographic characteristics, medical history, clinical and laboratory data, and outcome measures using standard case record forms, physical examination, and patient document reviews. The predictors of MODS were assessed using Cox proportional hazards models, with a focus on the association between traditional herbal medicine use and the risk of MODS.
A total of 310 patients were included in the final analysis, with a median age of 48 months and a male-to-female ratio of 1.5:1. The proportion and incidence of MODS were 30.96% (95% CI:25.8, 36.6) and 7.71(95% CI: 6.10, 9.40) per 100-person-day observation respectively. Renal failure (17.74%), neurologic failure (15.16%), and heart failure (14.52%) were the leading organ failures identified. Nearly one-third of patients (32.9%) died in the PICU, of which 59.8% had MODS. The rate of mortality was higher in patients with MODS than in those without. The Cox proportional hazards model identified renal disease (AHR = 6.32 (95%CI: 3.17,12.61)), intake of traditional herbal medication (AHR = 2.45, 95% CI:1.29,4.65), modified Pediatric Index of Mortality 2 (mPIM 2) score (AHR = 1.54 (95% CI: 1.38,1.71), and critical illness diagnoses (AHR = 2.68 (95% CI: 1.77,4.07)) as predictors of MODS.
The authors concluded that the incidence of MODS was high. Renal disease, THM use, mPIM 2 scores, and critical illness diagnoses were independent predictors of MODS. A more than twofold increase in the risk of MODS was seen in patients who used TMH. Healthcare providers should be aware of risks associated with THM, and educate caregivers about the potential harms of these products. Future studies with larger sample sizes and more comprehensive outcome measures are needed.
I do fully agree with the authors about the high usage of herbal and other so-called alternative medicines by children. We have shown that, in the UK the average one-year prevalence rate was 34% and the average lifetime prevalence was 42%. We have furthermore shown that the evidence base for these treatments in children is weak, even more so than for general populations. Finally, we can confirm that adverse effects are far from rare and often serious.
It is therefore high time, I think, that national regulators do more to protect children from SCAM practitioners who are at best uncritical about their treatments and at worse outright dangerous.
The French ‘National Assembly’ has yesterday adopted a major law aimed at reinforcing the prevention and combat against sectarian aberrations in France. This marks a significant step forward in strengthening the protection of citizens against abuse and manipulation by charlatans, gurus and other sectarian movements.
This bill, the result of particularly fruitful work and debate in both chambers, reflects the Government’s commitment to meeting the expectations of the victims of these sectarian movements.
Some of the key measures voted through by parliamentarians include:
- The enshrinement in law of the powers of MIVILUDES (Interministerial Mission of Vigilance and Combat against Sectarian Aberrations);
- The reinforcement of the penal response with the creation of the offence of placing or maintaining in a state of psychological or physical subjection;
- The creation of an offence of incitement to abandon or refrain from treatment, or to adopt practices which clearly expose the person concerned to a serious health risk;
- Support for victims, with the extension of the categories of associations that can bring civil action;
- Information for the judiciary, with the introduction of an “amicus curiae” role for certain government departments in legal cases relating to cults.
Despite sometimes heated debates, particularly around article 4, fuelled by the opinion of the Conseil d’Etat, the adoption of this law by the National Assembly bears witness to a shared desire to protect the rights and freedoms of individuals while providing better protection for our fellow citizens against sectarian aberrations.
This bill is part of a multi-annual national strategy for 2023-2027 resulting from the conference on sectarian aberrations held in spring 2023. It is a major step towards strengthening the penal arsenal and protecting victims.
_______________
Sabrina Agresti-Roubache, Secretary of State for Citizenship and Urban Affairs, commented:
“Long-awaited by victim support associations, this text aims to strengthen our legal arsenal in the fight against sectarian aberrations. I’m delighted that all the articles have been adopted, particularly Article 4, which creates an offence of incitement to abandon or abstain from treatment. There have been some passionate debates in the Chamber, but I’d like to reiterate the basis of this bill: the State is not fighting against beliefs, opinions or religions, but against all forms of sectarian aberrations, these dangerous behaviors which represent a threat to our social cohesion and put lives at risk.”
_______________
Obviously, we shall have to see how the new law will be applied. But, in any case, it is an important step into the right direction and could put an end to much of so-called alternative medicine that endangers the health of French consumers.
Other nations should consicer following the Franch example.
Millions of US adults use so-called alternative medicine (SCAM). In 2012, 55 million adults spent $28.3 billion on SCAMs, comparable to 9% of total out-of-pocket health care expenditures. A recent analysis conducted by the US National Institutes of Health’s National Center for Complementary and Integrative Health (NCCIH) suggests a substantial increase in the overall use of SCAM by American adults from 2002 to 2022. The paper published in the Journal of the American Medical Association, highlights a surge in the use of SCAM particularly for pain management.
Data from the 2002, 2012, and 2022 National Health Interview Surveys (NHISs) were employed to evaluate changes in the use of 7 SCAMs:
- yoga,
- meditation,
- massage therapy,
- chiropractic,
- acupuncture,
- naturopathy,
- guided imagery/progressive muscle relaxation.
The key findings include:
- The percentage of individuals who reported using at least one of the SCAMs increased from 19.2% in 2002 to 36.7% in 2022.
- The use of yoga, meditation, and massage therapy experienced the most significant growth.
- Use of yoga increased from 5% in 2002 to 16% in 2022.
- Meditation became the most popular SCAM in 2022, with an increase from 7.5% in 2002 to 17.3% in 2022.
- Acupuncture saw an increase from 1% in 2002 to 2.2% in 2022.
- The smallest rise was noted for chiropractic, from 79 to 86%
The analyses also suggested a rise in the proportion of US adults using SCAMs specifically for pain management. Among participants using any SCAM, the percentage reporting use for pain management increased from 42% in 2002 to 49% in 2022.
Limitations of the survey include:
- decreasing NHIS response rates over time,
- possible recall bias,
- cross-sectional data,
- differences in the wording of the surveys.
The NCCIH researchers like such surveys and tend to put a positive spin on them, i.e. SCAM is becoming more and more popular because it is supported by better and better evidence. Therefore, SCAM should be available to everyone who wants is.
But, of course, the spin could also turn in the opposite direction, i.e. the risk/benefit balance for most SCAMs is either negative or uncertain, and their cost-benefit remains unclear – as seen regularly on this blog. Therefore, the fact that SCAM seems to be getting more popular is of increasing concern. In particular, more consideration ought to be given to the indirect risks of SCAM (think, for instance, only of the influence SCAM practitioners have on the vaccination rates) that we often discuss here but that the NCCIH conveniently tends to ignore.
Mercury is a highly toxic chemical that threatens the health of humans and the environment. When it is released into the environment, it enters the food chain where it accumulates, particularly in fish. Exposure to high levels of mercury can cause harm to the brain, lungs, kidneys and the immune system. For these reasons, dental amalgam fillings which contain mercury have long been criticized. This is particularly true in the realm of so-called alternative medicine (SCAM) where, as discussed repeatedly, amalgam has long been a subject of both concern and misinformation, e.g.:
- Is removal of dental amalgam a good idea?
- Dental Amalgam
- Three Trends In “Alternative Dentistry” Part 3: Amalgam Removal and Avoidance
- Three Trends In “Alternative Dentistry” Part 1: The Concept of Projections—Of Meridians and Temporo-Mandibular Joint Dysfunction (TMJD)
- Holistic dentistry?
In the EU, dental amalgam might soon be merely of historical interest.
It has been announced that the EU Parliament and Council reached a provisional political agreement on the Commission’s proposal to address the remaining uses of mercury in products in the EU in line with commitments set out in the EU’s Zero Pollution Ambition.
In spite of viable mercury-free alternatives, around 40 tonnes of mercury are still used in the EU annually for dental amalgam as current rules only forbid the use of dental amalgam for treating teeth in children under 15 years old as well as pregnant and breastfeeding women.
Negotiators agreed to phase out the use of dental amalgam in the EU by 1 January 2025 except if deemed strictly necessary by the dental practitioner based on the duly justified specific medical needs of the patient.
EU countries that have not yet adjusted their reimbursement system to cover alternatives, may postpone the phase-out up until 30 June 2026, to avoid negative repercussions for low-income individuals that would otherwise be socio-economically disproportionally affected by the phase-out.
The export of dental amalgam will also be prohibited from 1 January 2025, whereas the manufacturing and import into the EU will be banned from 1 July 2026.
After the agreement, rapporteur Marlene Mortler (EPP, Germany) said: “After an intensive week of negotiations, we were able to reach an agreement today to ban dental amalgam containing mercury. This is an important step towards a mercury-free future. I am very pleased with the result – because we have ensured that such dental amalgam may only be used in medically necessary cases. Some Member States have been granted an exemption in order to mitigate the socio-economic consequences of the amalgam phase-out. After all, the ban on dental amalgam must not mean that low-income EU citizens can no longer afford adequate dental treatment in these countries. Another key point of this agreement is the decision that lamps containing mercury may only be exported to countries outside the EU until 30 June 2026. This will ensure that products that are already banned in the EU are not sold to third countries and have environmentally harmful consequences there.”
The deal still has to be adopted by the EU Parliament and Council, after which the new law will be published in the EU Official Journal and enter into force 20 days later.
Proponents of so-called alternative medicine (SCAM) are often – as we had many opportunities to observe here on this blog – not impressed with the safety and efficacy of COVID vaccinations. This is despite the fact that several studies have demonstrated the huge number of lives saved by them, both at national and multi-country level in the earlier stages of the pandemic. I wonder whether the doubters will be convinced by new evidence.
This analysis estimates how many lives were directly saved by vaccinating adults against COVID in the Region, from December 2020 through March 2023.
The researchers estimated the number of lives directly saved by age-group, vaccine dose and circulating Variant of Concern (VOC) period, both regionally and nationally, using weekly data on COVID-19 mortality and COVID-19 vaccine uptake reported by 34 European areas and territories (CAT), and vaccine effectiveness (VE) data from the literature. They calculated the percentage reduction in the number of expected and reported deaths.
The authors found that vaccines reduced deaths by 57% overall (CAT range: 15% to 75%), representing ∼1.4 million lives saved in those aged ≥25 years (range: 0.7 million to 2.6 million): 96% of lives saved were aged ≥60 years and 52% were aged ≥80 years; first boosters saved 51%, and 67% were saved during the Omicron period.
The authors concluded that over nearly 2.5 years, most lives saved by COVID-19 vaccination were in older adults by first booster dose and during the Omicron period, reinforcing the importance of up-to-date vaccination among these most at-risk individuals. Further modelling work should evaluate indirect effects of vaccination and public health and social measures.
The authors feel that their results reinforce the importance of up-to-date COVID-19 vaccination, particularly among older age-groups. Communication campaigns supporting COVID-19 vaccination should stress the value of COVID-19 vaccination in saving lives to ensure vulnerable groups are up-to-date with vaccination ahead of periods of potential increased transmission.
Those SCAM proponents who are not convinced of the merits of COVID and other vaccinations will undoubtedly claim that this new analysis was biased and thus unreliable. Therefore, it seems worth stating that this work was supported by a US Centers for Disease Control cooperative agreement, who had no role in data analysis or interpretation. The authors affiliated with the World Health Organization (WHO) are alone responsible for the views expressed in this publication and they do not necessarily represent the decisions or policies of the WHO.
I had the rare pleasure to give an interview for the ‘Frankfurter Allgemeine’. As it was, of course, in German, I took the liberty to translate it for my non-German speaking readers:
You have researched so-called alternative medicine over several decades, including homeopathy. What is your conclusion?
We are talking about far more than 400 methods – to draw one conclusion about all of them
is completely impossible. Except perhaps for this one: if something sounds too good to be true, it probably is.
Does this apply to homeopathy?
Highly diluted homeopathic remedies are popular because they have no side-effects. But there is also no effect. They are touted as a panacea. This is certainly not the case, on the contrary, they are
ineffective. And any therapy that is ineffective and promoted as a panacea is also dangerous.
How do you explain the fact that so many people swear by homeopathy?
There are several reasons for this. In Germany, homeopathy has an unbroken tradition, it was, for instance, promoted by the Nazis and later in the Federal Republic of Germany. It has a reputation for being gentle and effective. It might be gentle, but it is certainly not effective. It is also supported by lobby groups such as the manufacturers. And most people who use it don’t even understand what it actually is.
In any case, the placebo effect helps. What’s so bad about that??
Nothing at all, on the contrary: it is to be advocated. When we talk about placebo effects, we subsume many things under this umbrella that do not actually belong to it, such as the extensive, empathetic conversation that homeopaths often have with their patients. Besides, a common cold goes away whether you treat it or not. If you then use homeopathy, you can easily get the impression that it worked. Every good, empathetic doctor tries to maximize the placebo effect. To put it bluntly: you don’t need a placebo to generate a placebo effect. Patients also benefit from it when I give an effective remedy with empathy. In addition they benefit from the specific effect of my therapy, which should make up the lion’s share of the therapeutic response. If I withhold the most important thing I mistreat my patient.
But there are diseases for which there are no good remedies.
I often hear that argument. But there is practically always something we can do that at least
improves symptoms. Otherwise you should also say that instead of lying and recommending homeopathy – and thinking that, although there is nothing in it and it doesn’t work, but the patient, being an idiot, should take it nevertheless. It is unethical to use placebos as much as it is to use homeopathy.
Neurophysiologically, the placebo effect is becoming better and better understood.
The Italian neuroscientist Fabrizio Benedetti in particular has done very good work. But he also warns that this does not justify the use of homeopathy, for example.
Are there any studies on whether the placebo effect of homeopathy with its esoteric superstructure is greater than that giving just a piece of sugar?
There are analyses of what makes a particularly effective placebo. From this, we can learn that effective therapies in evidence-based medicine must be applied with empathy and sufficient time in order to maximize the ever-present placebo effect. So-called alternative medicine often does this quite well, and we can learn something from it. But the reason is that it often has nothing else. Homeopaths are a serious danger because they see homeopathy as a panacea. If someone has homeopathically treated their cold “successfully” for years and then gets cancer, they might think of turning to homeopathy for their cancer. It sounds crazy, but many homeopaths do offer cancer treatments on the internet, for instance. That sends shivers down my spine.
How should doctors and pharmacists react to the demand for homeopathic remedies?
Pharmacists are not primarily salespeople, they are a medical profession – they have to adhere to ethical guidelines. In this respect, evidence-based information of their clients/patients is very important.
Thomas Benkert, President of the German Federal Chamber of Pharmacists, has stated that he would not be able to stop giving advice if he always had to explain the lack of proof of efficacy.
He should perhaps read up on what his ethical duty to patients is.
What if doctors or pharmacists themselves believe in the effect?
Belief should not play a role, but evidence should.
Are you pleased with Lauterbach’s plan to no longer reimburse homeopathy?
I think it’s a shame that he justifies it by saying it’s ineffective. That is true. But the justification should be that it’s esoteric nonsense and therefore ineffective – and dangerous.
In the end, the Bundestag will decide.
I think Lauterbach has a good chance because things have started to move. Medical associations in Germany have spoken out against the additional designation of homeopathy, for example, and overall the wind has changed considerably.
What is it like in the UK, where you live?
The UK healthcare system, NHS, said goodbye to reimbursement of homeopathy about five years ago, even before France. The pharmacists’ association has distanced itself very clearly from homeopathy. However, most pharmacists still sell the remedies and many continue to support them.
You have also had disputes with the current head of state, King Charles. How did that come about?
A few years ago, he commissioned a paper claiming that so-called alternative medicine could save the British health service a lot of money. I protested against this – Charles accused me of leaking it to The Times before it was published. My university launched an investigation, which eventually found me innocent, but it led to the demise of my department. That caused me to retire two years early.
So Charles managed to close down the only research unit in the world that conducted critical and systematic research into so-called alternative medicine. Most researchers in this field only want to confirm their own prejudices and not disprove hypotheses. This is a serious misunderstanding of how science works. If someone reports only positive results for their favorite therapy in all conditions, something is wrong.
Some people say that homeopathy should not be researched because nothing positive can come out of it anyway.
There are certainly some SCAMs that are so nonsensical that they should not be researched, as is currently the case with homeopathy. I put it this way because I have researched homeopathy myself and, from my point of view, the situation was not so crystal clear 30 years ago.
Would you say that you have approached the matter with a sufficiently open mind?
No one can be completely unbiased. That’s why it’s important to do science properly, then you minimize bias as much as possible. When I took up my position at Exeter in 1993, I was perhaps somewhat biased towards homeopathy in a positive sense, because I had learned and used it myself, as well as other alternative medicine methods. The fact that the results then turned out to be negative in the vast majority of cases initially depressed me. But I have to live with that.
Every researcher prefers positive results, also because they are easier to publish. It was clear to me that, if I had succeeded in proving homeopathy right, I wouldn’t get one Nobel Prize, but two. Who wouldn’t want that?
(The interview was conducted by Hinnerk Feldwisch-Drentrup.)
he German press reported yesterday that the country’s Health Minister Karl Lauterbach plans to remove homeopathic treatments from the benefits catalog of statutory health insurance companies. “Services that have no medically verifiable benefit should not be financed from contribution funds,” states a recommendation paper by the minister. “For this reason, we will remove the option for health insurance companies to include homeopathic and anthroposophic services in their statutes, thereby avoiding unnecessary expenditure by health insurance companies.” However, private supplementary insurance should still be possible.
Lauterbach had already announced last year that he would review the funding of homeopathic treatments. “Although homeopathy is not significant in terms of expenditure, it has no place in a science-based healthcare policy,” the SPD politician told “Der Spiegel” last October. The measure would save merely a maximum of ten million Euros. This is because firstly not all health insurance companies offer the option to reimburse homeopathy, and secondly, because not that many Germans use homeopathy.
____________________________
Before I was joined about a decade ago by a group of excellent and effective skeptics, I seemed to be a lone, lost voice in Germany cautioning against the misunderstanding that homeopathy and anthroposophical medicine were backed by evidence. Thus, you probably think that I am rejoicing at this spectacular success. At first glance, it does indeed seem to be great news for those who support evidence-based medicine. But sadly, I also have second thoughts.
We should, I think, be concerned that Lauterbach intends to leave homeopathic and anthroposophical remedies reimbursible via private supplementary insurance. Most Germans have such insurance which means that, despite Lauterbach’s grand announcement, very little will probably change. Homeopathy and anthroposophic medicine, both pure placebo therapies, will still be able to pretend to be real medicine.
Moreover, we should be concerned about Lauterbach’s reasoning. It is, of course, laudable to point out that homeopathic and anthroposophic remedies are not demonstrably effective. But clearly, this is only half of the truth. The full truth is that they are based on totally ridiculous assumptions, that, in other words, they fly in the face of science. Only if we manage to get this message across, will we inform the public responsibly, in my view.
A total ban then? No, personally, I don’t want to ban homeopathic or anthroposophical remedies. If someone loves esoteric nonsense or placebos, he/she should, in my view, be able to buy them. But he/she should use their own money for the purchase. We should remember that wasting notoriously scarce public funds from either statutory or private health insurances is not just uneconomical but foremost unethical.
This systematic review aimed to investigate the effectiveness of cupping therapy on low back pain (LBP). Medline, Embase, Scopus and WANFANG databases were searched for relevant cupping RCTs on low back pain articles up to 2023. A complementary search was manually made on 27 September for update screening. Full-text English and Chinese articles on all ethnic adults with LBP of cupping management were included. Studies looking at acute low back pain only were excluded. Two independent reviewers screened and extracted data, with any disagreement resolved through consensus by a third reviewer. The methodological quality of the included studies was evaluated independently by two reviewers using an adapted tool. Change-from-baseline outcomes were treated as continuous variables and calculated according to the Cochrane Handbook. Data were extracted and pooled into the meta-analysis by Review Manager software (version 5.4, Nordic Cochrane Centre).
Eleven trials involving 921 participants were included. Five studies were assessed as being at low risk of bias, and six studies were of acceptable quality. The findings reveal:
- High-quality evidence demonstrated cupping significantly improves pain at 2-8 weeks endpoint intervention (d=1.09, 95% CI: [0.35-1.83], p=0.004).
- There was no continuous pain improvement observed at one month (d=0.11, 95% CI: [-1.02-1.23], p=0.85) and 3-6 months (d=0.39, 95% CI: [-0.09-0.87], p=0.11).
- Dry cupping did not improve pain (d=1.06, 95% CI: [-0.34, 2.45], p=0.14) compared with wet cupping (d=1.5, 95% CI: [0.39-2.6], p=0.008) at the endpoint intervention.
- There was no evidence indicating the association between pain reduction and different types of cupping (p=0.2).
- Moderate- to low-quality evidence showed that cupping did not reduce chronic low back pain (d=0.74, 95% CI: [-0.67-2.15], p=0.30) and non-specific chronic low back pain (d=0.27, 95% CI: [-1.69-2.24], p=0.78) at the endpoint intervention.
- Cupping on acupoints showed a significant improvement in pain (d=1.29, 95% CI: [0.63-1.94], p<0.01) compared with the lower back area (d=0.35, 95% CI: [-0.29-0.99], p=0.29).
- A potential association between pain reduction and different cupping locations (p=0.05) was found.
- Meta-analysis showed a significant effect on pain improvement compared to medication therapy (n=8; d=1.8 [95% CI: 1.22 – 2.39], p<0.001) and usual care (n=5; d=1.07 [95% CI: 0.21- 1.93], p=0.01).
- Two studies demonstrated that cupping significantly mediated sensory and emotional pain immediately, after 24 hours, and 2 weeks post-intervention (d= 5.49, 95% CI [4.13-6.84], p<0.001).
- Moderate evidence suggested that cupping improved disability at the 1-6 months follow-up (d=0.67, 95% CI: [0.06-1.28], p=0.03).
- There was no immediate effect observed at the 2-8 weeks endpoint (d=0.40, 95% CI: [-0.51-1.30], p=0.39).
- A high degree of heterogeneity was noted in the subgroup analysis (I2 >50%).
The authors concluded that high- to moderate-quality evidence indicates that cupping significantly improves pain and disability. The effectiveness of cupping for LBP varies based on treatment durations, cupping types, treatment locations, and LBP classifications. Cupping demonstrated a superior and sustained effect on pain reduction compared with medication and usual care. The notable heterogeneity among studies raises concerns about the certainty of these findings. Further research should be designed with a standardized cupping manipulation that specifies treatment sessions, frequency, cupping types, and treatment locations. The real therapeutic effects of cupping could be confirmed using a sham device or objective outcome measurements. Studies with at least six- to twelve-month follow-ups are needed to investigate the long-term efficacy of cupping in managing LBP.
Confused?
No need, it’s really quite simple: cupping can, according to this review, be shown to have some short-lasting effect, provided the study is flawed and does not control for placebo effects.
Surprised?
No need! There is hardly a form of so-called alternative medicine (SCAM) that does not have a similarly small effect of back pain, if tested in equally dodgy studies. This is particularly true for those treatments that can act as a theatrical placebo, e.g. acupuncture or chiropractic.
So, should a back pain sufferer try cupping?
If he/she insists, why not? But please don’t use wet cupping (which can do quite a bit of harm). Dry cupping (without injuring the skin) is arguably better (less risk, less expense, possibility of home treatment by your partner) than chiropractic, osteopathy, acupuncture, or many other SCAMs.
My conclusions – as mentioned many times previously – are as follows:
- Most SCAMs help a little with back pain (and similar conditions) because they can have a powerful placebo effect.
- Conventional medicine is also not convincingly effective for back pain.
- If you insist on SCAM, it is best to use one that is relatively harmless and inexpensive.
Since the introduction of their new Education Standards in March 2023, the General Chiropractic Council (GCC) has been working with chiropractic education providers to support them in implementing the changes to their curricula. Recently, the GCC have stated this:
We expect students to be taught evidence-based practice: integrating individual clinical expertise, the best available evidence from current and credible clinical research, and the values and preferences of patients. Chiropractors are important members of a patient’s healthcare team, and interprofessional approaches enable the best outcomes. Programmes that meet these Standards will teach ethical, professional care and produce competent healthcare professionals who can serve the needs of patients.
These are indeed most encouraging words!
Basically, they are saying that chiropractic education will now have to be solidly based on the principles of evidence-based medicine (EBM) as well as sound medical ethics. Let me spell out what this really means. Chiropractic courses must teach that:
- The current and credible clinical evidence suggesting that spinal manipulations, the hallmark intervention of chiropractors, are effective is weak for back pain and negative or absent for all other conditions.
- The current and credible clinical evidence suggests that spinal manipulations, the hallmark intervention of chiropractors, can cause harm which in many instances is serious.
- The current and credible clinical evidence thus suggests that the risk/benefit balance for spinal manipulations, the hallmark intervention of chiropractors, is not positive.
- Medical ethics require that competent healthcare professionals inform their patients that spinal manipulations, the hallmark intervention of chiropractors, may not generate more good than harm which is the reason why they cannot employ these therapies.
So, the end of chiropractic in the UK is looming!
Unless, of course, the GCC’s words are not really meant to be translated into action. They could be just window dressing and politically correct bullshit. But that’ s really far too far fetched – after all they come from the GENERAL CHIROPRACTIC COUNCIL, known for its excellent track record, e.g.:
- The GCC “seems to be a little self-regulatory chiropractic bubble where chiropractors regulate chiropractors.”
- A 5-year strategy for UK chiropractors: not fit for purpose
- Chiro behaving badly… is the GCC fit for purpose?
- The UK General Chiropractic Council: fit for purpose?
- Farcical Chiropractic Council: Chiropractic Patient Satisfaction and Experience
- The General Chiropractic Council “regulates chiropractors to ensure the safety of patients” … well, you could have fooled me!
- Death of a chiropractic patient prompts a reaction by the UK General Chiropractic Council
