spinal manipulation
The literature on malpractice in medicine is huge: more than 33 000 articles listed in Medline. By contrast, the literature on malpractice in alternative medicine hardly exists. An exception is this recent article. I therefore thought I share it with you and provide a few comments:
START OF QUOTE
According to the (US) National Practitioner Data Bank, between September 1, 1990 and January 29, 2012, a total of 5,796 chiropractic medical malpractice reports were filed. Lawsuits with the highest payouts in any medical field are related to misdiagnosis, failure to diagnose and delayed diagnosis of a severe medical condition.
Common reasons for chiropractic malpractice lawsuits:
Chiropractor causes stroke: Numerous cases have been documented in which a patient suffers a stroke after getting his or her neck manipulated, or adjusted. Especially forceful rotation of the neck from side to side can overextend an artery that runs along the spine, which can result in a blockage of blood flow to the brain. Strokes are among the most serious medical conditions caused by chiropractic treatment, and can result in temporary or permanent paralysis, and even death.
Herniated disc following adjustment: Although many patients seek the medical attention of a chiropractor after they have experienced a herniated disc, chiropractors can actually be the cause of the problem. Usually a herniated disc is caused by wear and tear, but a sudden heavy strain, increased pressure to the lower back or twisting motions can cause a sudden herniated disc. The stress that chiropractors exercise in their adjustments have been known to be the root cause of some herniated discs.
Sexual misconduct: The American Chiropractic Association has assembled a code of ethics “based upon the acknowledgement that the social contract dictates the profession’s responsibilities to the patient, the public and the profession.” Sexual misconduct is among the top ten reasons that patients file lawsuits against chiropractors. Often, chiropractic practices are unfamiliar to many new patients and can be misinterpreted as inappropriate even though they are absolutely normal, so it is important that patients familiarize themselves with common chiropractic methods of healing.
END OF QUOTE
In this context, a study of chiropractic from Canada might be interesting. It highlights the conclusions from Canadian courts: informed consent is an ongoing process that cannot be entirely delegated to office personnel… A further study showed that valid consent procedures are either poorly understood or selectively implemented by chiropractors. Arguably, not obtaining informed consent amounts to malpractice.
In our book, this is what we conclude about informed consent by alternative therapists in general: Genuine informed consent is unattainable for most CAM modalities. This presents a serious and intractable ethical problem for CAM practitioners. Attempts to square this circle by watering down or redefining the criteria for informed consent are ethically indefensible. The concept of informed consent and its centrality in medical ethics therefore renders most CAM practice unacceptable. Conventional healthcare subscribes to the ethical principle ‘no consent, no treatment’: we are not aware of the existence of any good reasons to excuse CAM from this dictum.
I fear that, if we were to count the lack of informed consent by chiropractors (and other alternative practitioners) as malpractice, the numbers would be astronomical. Or, to put it differently, the often-cited relatively low malpractice rate in chiropractic is due to the omission of the vast majority of malpractice cases.
Systematic research on complaints about chiropractors, osteopaths, and physiotherapists is rare. We have often heard chiropractors claim that complaints against them are extremely rare events.
But is this true?
Two recent investigations might go some way towards answering this question.
The aim of the first investigation was to understand differences in the frequency and nature of formal complaints about Australian practitioners in these professions in order to inform improvements in professional regulation and education.
This retrospective cohort study analysed all formal complaints about all registered chiropractors, osteopaths, and physiotherapists in Australia lodged with health regulators between 2011 and 2016. Based on initial assessments by regulators, complaints were classified into 11 issues across three domains: performance, professional conduct, and health. Differences in complaint rate were assessed using incidence rate ratios. A multivariate negative binomial regression model was used to identify predictors of complaints among practitioners in these professions.
Patients and their relatives were the most common source of complaints about chiropractors, osteopaths and physiotherapists. Concerns about professional conduct accounted for more than half of the complaints about practitioners in these three professions. Regulatory outcome of complaints differed by profession. Male practitioners, those who were older than 65 years, and those who practised in metropolitan areas were at higher risk of complaint. The overall rate of complaints was higher for chiropractors than osteopaths and physiotherapists (29 vs. 10 vs. 5 complaints per 1000 practice years respectively, p < 0.001). Among chiropractors, 1% of practitioners received more than one complaint – they accounted for 36% of the complaints within their profession. Overall, nearly half of the complaints (47.7%) involved chiropractors, even though chiropractors make up less than one-sixth (13.9%) of the workforce across these three professions.
The authors concluded that their study demonstrates differences in the frequency of complaints by source, issue and outcome across the chiropractic, osteopathic and physiotherapy professions. Independent of profession, male sex and older age were significant risk factors for complaint in these professions. Chiropractors were at higher risk of being the subject of a complaint to their practitioner board compared with osteopaths and physiotherapists. These findings may assist regulatory boards, professional associations and universities in developing programs that avert patient dissatisfaction and harm and reduce the burden of complaints on practitioners.
The aim of the second study was to describe claims reported to the Danish Patient Compensation Association and the Norwegian System of Compensation to Patients related to chiropractic from 2004 to 2012.
All finalized compensation claims involving chiropractors reported to one of the two associations between 2004 and 2012 were assessed for age, gender, type of complaint, decisions and appeals. Descriptive statistics were used to describe the study population. The results show that 338 claims were registered in Denmark and Norway between 2004 and 2012 of which 300 were included in the analysis. 41 (13.7%) were approved for financial compensation. The most frequent complaints were worsening of symptoms following treatment (n = 91, 30.3%), alleged disk herniations (n = 57, 19%) and cases with delayed referral (n = 46, 15.3%). A total financial payment of €2,305,757 (median payment €7,730) were distributed among the forty-one cases with complaints relating to a few cases of cervical artery dissection (n = 11, 5.7%) accounting for 88.7% of the total amount.
The authors concluded that chiropractors in Denmark and Norway received approximately one compensation claim per 100.000 consultations. The approval rate was low across the majority of complaint categories and lower than the approval rates for general practioners and physiotherapists. Many claims can probably be prevented if chiropractors would prioritize informing patients about the normal course of their complaint and normal benign reactions to treatment.
In their discussion section the authors make the following comments: A particular concern after cervical SMT is dissection of the vertebral and carotid arteries. Seventeen claims concerning CAD were reported in this data, 14 in Denmark and three in Norway, and 11 of these were approved for financial compensation (64.7% approval rate) representing by far the highest approval rate across all complaint categories… chiropractors generally seem to receive more claims per consultation than GPs and physiotherapists, the approval rate is substantially lower and a similar trend is observed in Norway. However, it is also evident that approved claims within chiropractic bear a higher financial burden than their peers. These numbers are clearly highly influenced by the cases related to CAD. Several reasons might explain a higher complaint rate within chiropractic but this remains speculation and we do not have hard evidence supporting any of the following suggestions: (1) chiropractic treatment might be perceived as more aggressive than that of GPs and physiotherapists (2) maybe scepticism towards chiropractic among medical physicians and physiotherapists could encourage more patient complaints (3) a higher out-of-pocket expense for chiropractic services compared with GP and physiotherapist services might influence the higher number of complaints (4) chiropractors do not adequately inform patients about normal side effects and reactions and patients regard these as serious and relevant for compensation claims (5) chiropractors encourage patients to report AE more frequently than GPs and physiotherapists.
So, are complaints against chiropractors rarities?
I don’t think so.
THE CONVERSATION recently carried an article shamelessly promoting osteopathy. It seems to originate from the University of Swansea, UK, and is full of bizarre notions. Here is an excerpt:
To find out more about how osteopathy could potentially affect mental health, at our university health and well-being academy, we have recently conducted one of the first studies on the psychological impact of OMT – with positive results.
For the last five years, therapists at the academy have been using OMT to treat members of the public who suffer from a variety of musculoskeletal disorders which have led to chronic pain. To find out more about the mental health impacts of the treatment, we looked at three points in time – before OMT treatment, after the first week of treatment, and after the second week of treatment – and asked patients how they felt using mental health questionnaires.
This data has shown that OMT is effective for reducing anxiety and psychological distress, as well as improving patient self-care. But it may not be suitable for all mental illnesses associated with chronic pain. For instance, we found that OMT was less effective for depression and fear avoidance.
All is not lost, though. Our results also suggested that the positive psychological effects of OMT could be further optimised by combining it with therapy approaches like acceptance and commitment therapy (ACT). Some research indicates that psychological problems such as anxiety and depression are associated with inflexibility, and lead to experiential avoidance. ACT has a positive effect at reducing experiential avoidance, so may be useful with reducing the fear avoidance and depression (which OMT did not significantly reduce).
Other researchers have also suggested that this combined approach may be useful for some subgroups receiving OMT where they may accept this treatment. And, further backing this idea up, there has already been at least one pilot clinical trial and a feasibility study which have used ACT and OMT with some success.
Looking to build on our positive results, we have now begun to develop our ACT treatment in the academy, to be combined with the osteopathic therapy already on offer. Though there will be a different range of options, one of these ACT therapies is psychoeducational in nature. It does not require an active therapist to work with the patient, and can be delivered through internet instruction videos and homework exercises, for example.
Looking to the future, this kind of low cost, broad healthcare could not only save the health service money if rolled out nationwide but would also mean that patients only have to undergo one treatment.
END OF QUOTE
So, they recruited a few patients who had come to receive osteopathic treatments (a self-selected population full of expectation and in favour of osteopathy), let them fill a few questionnaires and found some positive changes. From that, they conclude that OMT (osteopathic manipulative therapy) is effective. Not only that, they advocate that OMT is rolled out nationwide to save NHS funds.
Vis a vis so much nonsense, I am (almost) speechless!
As this comes not from some commercial enterprise but from a UK university, the nonsense is intolerable, I find.
Do I even need to point out what is wrong with it?
Not really, it’s too obvious.
But, just in case some readers struggle to find the fatal flaws of this ‘study’, let me mention just the most obvious one. There was no control group! That means the observed outcome could be due to many factors that are totally unrelated to OMT – such as placebo-effect, regression towards the mean, natural history of the condition, concomitant treatments, etc. In turn, this also means that the nationwide rolling out of their approach would most likely be a costly mistake.
The general adoption of OMT would of course please osteopaths a lot; it could even reduce anxiety – but only that of the osteopaths and their bank-managers, I am afraid.
We recently discussed the deplorable case of Larry Nassar and the fact that the ‘American Osteopathic Association’ stated that intravaginal manipulations are indeed an approved osteopathic treatment. At the time, I thought this was a shocking claim. So, imagine my surprise when I was alerted to a German trial of osteopathic intravaginal manipulations.
Here is the full and unaltered abstract of the study:
Introduction: 50 to 80% of pregnant women suffer from low back pain (LBP) or pelvic pain (Sabino und Grauer, 2008). There is evidence for the effectiveness of manual therapy like osteopathy, chiropractic and physiotherapy in pregnant women with LBP or pelvic pain (Liccardione et al., 2010). Anatomical, functional and neural connections support the relationship between intrapelvic dysfunctions and lumbar and pelvic pain (Kanakaris et al., 2011). Strain, pressure and stretch of visceral and parietal peritoneum, bladder, urethra, rectum and fascial tissue can result in pain and secondary in muscle spasm. Visceral mobility, especially of the uterus and rectum, can induce tension on the inferior hypogastric plexus, which may influence its function. Thus, stretching the broad ligament of the uterus and the intrapelvic fascia tissue during pregnancy can reinforce the influence of the inferior hypogastric plexus. Based on above facts an additional intravaginal treatment seems to be a considerable approach in the treatment of low back pain in pregnant women.
Objective: The purpose of this study was to compare the effect of osteopathic treatment including intravaginal techniques versus osteopathic treatment only in females with pregnancy-related low back pain.
Methods: Design: The study was performed as a randomized controlled trial. The participants were randomized by drawing lots, either into the intervention group including osteopathic and additional intravaginal treatment (IV) or a control group with osteopathic treatment only (OI). Setting: Medical practice in south of Germany.
Participants 46 patients were recruited between the 30th and 36th week of pregnancy suffering from low back pain.
Intervention Both groups received three treatments within a period of three weeks. Both groups were treated with visceral, mobilization, and myofascial techniques in the cervical, thoracic and lumbar spine, the pelvic and the abdominal region (American Osteopathic Association Guidelines, 2010). The IV group received an additional treatment with intravaginal techniques in supine position. This included myofascial techniques of the M. levator ani and the internal obturator muscles, the vaginal tissue, the pubovesical and uterosacral ligaments as well as the inferior hypogastric plexus.
Main outcome measures As primary outcome the back pain intensity was measured by Visual Analogue Scale (VAS). Secondary outcome was the disability index assessed by Oswestry-Low-Back-Pain-Disability-Index (ODI), and Pregnancy-Mobility-Index (PMI).
Results: 46 participants were randomly assigned into the intervention group (IV; n = 23; age: 29.0 ±4.8 years; height: 170.1 ±5.8 cm; weight: 64.2 ±10.3 kg; BMI: 21.9 ±2.6 kg/m2) and the control group (OI; n = 23; age: 32.0 ±3.9 years; height: 168.1 ±3.5 cm; weight: 62.3 ±7.9 kg; BMI: 22.1 ±3.2 kg/m2). Data from 42 patients were included in the final analyses (IV: n=20; OI: n=22), whereas four patients dropped out due to general pregnancy complications. Back pain intensity (VAS) changed significantly in both groups: in the intervention group (IV) from 59.8 ±14.8 to 19.6 ±8.4 (p<0.05) and in the control group (OI) from 57.4 ±11.3 to 24.7 ±12.8. The difference between groups of 7.5 (95%CI: -16.3 to 1.3) failed to demonstrate statistical significance (p=0.93). Pregnancy-Mobility-Index (PMI) changed significantly in both groups, too. IV group: from 33.4 ±8.9 to 29.6 ±6.6 (p<0.05), control group (OI): from 36.3 ±5.2 to 29.7 ±6.8. The difference between groups of 2.6 (95%CI: -5.9 to 0.6) was not statistically significant (p=0.109). Oswestry-Low-Back-Pain-Disability-Index (ODI) changed significantly in the intervention group (IV) from 15.1 ±7.8 to 9.2 ±3.6 (p<0.05) and also significantly in the control group (OI) from 13.8 ±4.9 to 9.2 ±3.0. Between-groups difference of 1.3 (95%CI: -1.5 to 4.1) was not statistically significant (p=0.357).
Conclusions: In this sample a series of osteopathic treatments showed significant effects in reducing pain and increasing the lumbar range of motion in pregnant women with low back pain. Both groups attained clinically significant improvement in functional disability, activity and quality of life. Furthermore, no benefit of additional intravaginal treatment was observed.
END OF QUOTE
My first thoughts after reading this were: how on earth did the investigators get this past an ethics committee? It cannot be ethical, in my view, to allow osteopaths (in Germany, they have no relevant training to speak of) to manipulate women intravaginally. How deluded must an osteopath be to plan and conduct such a trial? What were the patients told before giving informed consent? Surely not the truth!
My second thoughts were about the scientific validity of this study: the hypothesis which this trial claims to be testing is a far-fetched extrapolation, to put it mildly; in fact, it is not a hypothesis, it’s a very daft idea. The control-intervention is inadequate in that it cannot control for the (probably large) placebo effects of intravaginal manipulations. The observed outcomes are based on within-group comparisons and are therefore most likely unrelated to the treatments applied. The conclusion is as barmy as it gets; a proper conclusion should clearly and openly state that the results did not show any effects of the intravaginal manipulations.
In summary, this is a breathtakingly idiotic trial, and everyone involved in it (ethics committee, funding body, investigators, statistician, reviewers, journal editor) should be deeply ashamed and apologise to the poor women who were abused in a most deplorable fashion.
The RCC is a relatively new organisation. It is a registered charity claiming to promote “professional excellence, quality and safety in chiropractic… The organisation promotes and supports high standards of education, practice and research, enabling chiropractors to provide, and to be recognised for providing, high quality care for patients.”
I have to admit that I was not impressed by the creation of the RCC and lately have not followed what they are up to – not a lot, I assumed. But now they seem to plan a flurry of most laudable activities:
The Royal College of Chiropractors is developing a range of initiatives designed to help chiropractors actively engage with health promotion, with a particular focus on key areas of public health including physical activity, obesity and mental wellbeing.
Dr Mark Gurden, Chair of the RCC Health Policy Unit, commented:
“Chiropractors are well placed to participate in public health initiatives. Collectively, they have several million opportunities every year in the UK to support people in making positive changes to their general health and wellbeing, as well as helping them manage their musculoskeletal health of course.
Our recent AGM & Winter Conference highlighted the RCC’s intentions to encourage chiropractors to engage with a public health agenda and we are now embarking on a programme to:
- Help chiropractors recognise the importance of their public health role;
- Help chiropractors enhance their knowledge and skills in providing advice and support to patients in key areas of public health through provision of information, guidance and training;
- Help chiropractors measure and recognise the impact they can have in key areas of public health.
To take this work forward, we will be exploring the possibility of launching an RCC Public Health Promotion & Wellbeing Society with a view to establishing a new Specialist Faculty in due course.”
END OF QUOTE
A ‘Public Health Promotion & Wellbeing Society’. Great!
As this must be new ground for the RCC, let me list a few suggestions as to how they could make more meaningful contributions to public health:
- They could tell their members that immunisations are interventions that save millions of lives and are therefore in the interest of public health. Many chiropractors still have a very disturbed attitude towards immunisation: anti-vaccination attitudes still abound within the chiropractic profession. Despite a growing body of evidence about the safety and efficacy of vaccination, many chiropractors do not believe in vaccination, will not recommend it to their patients, and place emphasis on risk rather than benefit. In case you wonder where this odd behaviour comes from, you best look into the history of chiropractic. D. D. Palmer, the magnetic healer who ‘invented’ chiropractic about 120 years ago, left no doubt about his profound disgust for immunisation: “It is the very height of absurdity to strive to ‘protect’ any person from smallpox and other malady by inoculating them with a filthy animal poison… No one will ever pollute the blood of any member of my family unless he cares to walk over my dead body… ” (D. D. Palmer, 1910)
- They could tell their members that chiropractic for children is little else than a dangerous nonsense for the sake of making money. Not only is there ‘not a jot of evidence‘ that it is effective for paediatric conditions, it can also cause serious harm. I fear that this suggestion is unlikely to be well-received by the RCC; they even have something called a ‘Paediatrics Faculty’!
- They could tell their members that making bogus claims is not just naughty but hinders public health. Whenever I look on the Internet, I find more false than true claims made by chiropractors, RCC members or not.
- They could tell their members that informed consent is not an option but an ethical imperative. Actually, the RCC do say something about the issue: The BMJ has highlighted a recent UK Supreme Court ruling that effectively means a doctor can no longer decide what a patient needs to know about the risks of treatment when seeking consent. Doctors will now have to take reasonable care to ensure the patient is aware of any material risks involved in any recommended treatment, and of any reasonable alternative or variant treatments. Furthermore, what counts as material risk can no longer be based on a responsible body of medical opinion, but rather on the view of ‘a reasonable person in the patient’s position’. The BMJ article is available here. The RCC feels it is important for chiropractors to be aware of this development which is relevant to all healthcare professionals. That’s splendid! So, chiropractors are finally being instructed to obtain informed consent from all their patients before starting treatment. This means that patients must be told that spinal manipulation is associated with very serious risks, AND that, in addition, ~ 50% of all patients will suffer from mild to moderate side effects, AND that there are always less risky and more effective treatments available for any condition from other healthcare providers.
- The RCC could, for the benefit of public health, establish a compulsory register of adverse effects after spinal manipulations and make the data from it available to the public. At present such a register does not exist, and therefore its introduction would be a significant step in the right direction.
- The RCC could make it mandatory for all members to adhere to the above points and establish a mechanism of monitoring their behaviour to make sure that, for the sake of public health, they all do take these issues seriously.
I do realise that the RCC may not currently have the expertise and know-how to adopt my suggestions, as these issues are rather new to them. To support the RCC in their praiseworthy endeavours, I herewith offer to give one or more evidence-based lectures on these subjects (at a date and place of their choice) in an attempt to familiarise the RCC and its members with these important aspects of public health. I also realise that the RCC may not have the funds to pay professorial lecture fees. Therefore, in the interest of both progress and public health, I offer to give these lectures for free.
I can be contacted via this blog.
“In at least one article on chiropractic, Ernst has been shown to be fabricating data. I would not be surprised if he did the same thing with homeopathy. Ernst is a serial scientific liar.”
I saw this remarkable and charming Tweet yesterday. Its author is ‘Dr’ Avery Jenkins. Initially I was unaware of having had contact with him before; but when I checked my emails, I found this correspondence from August 2010:
Dr. Ernst:
Would you be so kind as to provide the full text of your article? Also, when would you be available for an interview for an upcoming feature article?
Thank you.
Avery L. Jenkins, D.C.
I put his title in inverted commas, because it turns out he is a chiropractor and not a medical doctor (but let’s not be petty!).
‘Dr’ Avery Jenkins runs a ‘Center for Alternative Medicine’ in the US: The Center has several features which set it apart from most other alternative medicine facilities, including the Center’s unique Dispensary. Stocked with over 300 herbs and supplements, the Dispensary’s wide range of natural remedies enables Dr. Jenkins to be the only doctor in Connecticut who provides custom herbal formulations for his patients. In our drug testing facility, we can provide on-site testing for drugs of abuse with immediate result reporting. Same-day appointments are available. Dr. Jenkins is also one of the few doctors in the state who has already undergone the federally-mandated training which will be necessary for all Department of Transportation Medical Examiners by 2014. Medical examinations for your Commercial Drivers License will take only 25 minutes, and Dr. Jenkins will provide you with all necessary paperwork.
The good ‘doctor’ also publishes a blog, and there I found a post from 2016 entirely dedicated to me. Here is an excerpt:
.. bias and hidden agendas come up in the research on alternative medicine and chiropractic in particular. Mostly this occurs in the form of journal articles using research that has been hand-crafted to make chiropractic spinal manipulation appear dangerous — when, in fact, you have a higher risk of serious injury while driving to your chiropractor’s office than you do of any treatment you receive while you’re there.
A case in point is the article, “Adverse effects of spinal manipulation: a systematic review,” authored by Edzard Ernst, and published in the Journal of the Royal Society of Medicine in 2007. Ernst concludes that, based on his review, “in the interest of patient safety we should reconsider our policy towards the routine use of spinal manipulation.”
This conclusion throws up several red flags, beginning with the fact that it flies in the face of most of the already-published, extensive research which shows that chiropractic care is one of the safest interventions, and in fact, is safer than medical alternatives.
For example, an examination of injuries resulting from neck adjustments over a 10-year period found that they rarely, if ever, cause strokes, and lumbar adjustments by chiropractors have been deemed by one of the largest studies ever performed to be safer and more effective than medical treatment.
So the sudden appearance of this study claiming that chiropractic care should be stopped altogether seems a bit odd.
As it turns out, the data is odd as well.
In 2012, a researcher at Macquarie University in Australia, set out to replicate Ernst’s study. What he found was shocking.
This subsequent study stated that “a review of the original case reports and case series papers described by Ernst found numerous errors or inconsistencies,” including changing the sex and age of patients, misrepresenting patients’ response to adverse events, and claiming that interventions were performed by chiropractors, when no chiropractor was even involved in the case.
“In 11 cases of the 21…that Ernst reported as [spinal manipulative therapy] administered by chiropractors, it is unlikely that the person was a qualified chiropractor,” the review found.
What is interesting here is that Edzard Ernst is no rookie in academic publishing. In fact, he is a retired professor and founder of two medical journals. What are the odds that a man with this level of experience could overlook so many errors in his own data?
The likelihood of Ernst accidentally allowing so many errors into his article is extremely small. It is far more likely that Ernst selected, prepared, and presented the data to make it fit a predetermined conclusion.
So, Ernst’s article is either extremely poor science, or witheringly inept fraud. I’ll let the reader draw their own conclusion.
Interestingly enough, being called out on his antics has not stopped Ernst from disseminating equally ridiculous research in an unprofessional manner. Just a few days ago, Ernst frantically called attention to another alleged chiropractic mishap, this one resulting in a massive brain injury.
Not only has he not learned his lesson yet, Ernst tried the same old sleight of hand again. The brain injury, as it turns out, didn’t happen until a week after the “chiropractic” adjustment, making it highly unlikely, if not impossible, for the adjustment to have caused the injury in the first place. Secondly, the adjustment wasn’t even performed by a chiropractor. As the original paper points out, “cervical manipulation is still widely practiced in massage parlors and barbers in the Middle East.” The original article makes no claim that the neck adjustment (which couldn’t have caused the problem in the first place) was actually performed by a chiropractor.
It is truly a shame that fiction published by people like Ernst has had the effect of preventing many people from getting the care they need. I can only hope that someday the biomedical research community can shed its childish biases so that we all might be better served by their findings.
END OF QUOTE
Here I will not deal with the criticism a Australian chiropractor published in a chiro-journal 5 years after my 2007 article (which incidentally was not primarily about chiropractic but about spinal manipulation). Suffice to say that my article did NOT contain ‘fabricated’ data. A full re-analysis would be far too tedious, for my taste (especially as criticism of it has been discussed in all of 7 ‘letters to the editor’ soon after its publication)
- Adverse effects of spinal manipulation. [J R Soc Med. 2007]
- Adverse effects of spinal manipulation. [J R Soc Med. 2007]
- Adverse effects of spinal manipulation. [J R Soc Med. 2007]
- Adverse effects of spinal manipulation. [J R Soc Med. 2007]
- Adverse effects of spinal manipulation. [J R Soc Med. 2007]
- Adverse effects of spinal manipulation. [J R Soc Med. 2007]
- Adverse effects of spinal manipulation. [J R Soc Med. 2007]
I will, however, address ‘Dr’ Avery Jenkins’ second allegation related to my recent (‘frantic’) blog-post. I will do this by simply copying the abstract of the paper in question:
Background: Multivessel cervical dissection with cortical sparing is exceptional in clinical practice. Case presentation: A 55-year-old man presented with acute-onset neck pain with associated sudden onset right-sided hemiparesis and dysphasia after chiropractic* manipulation for chronic neck pain. Results and Discussion: Magnetic resonance imaging revealed bilateral internal carotid artery dissection and left extracranial vertebral artery dissection with bilateral anterior cerebral artery territory infarctions and large cortical-sparing left middle cerebral artery infarction. This suggests the presence of functionally patent and interconnecting leptomeningeal anastomoses between cerebral arteries, which may provide sufficient blood flow to salvage penumbral regions when a supplying artery is occluded. Conclusion: Chiropractic* cervical manipulation can result in catastrophic vascular lesions preventable if these practices are limited to highly specialized personnel under very specific situations.
*my emphasis
With this, I rest my case.
The only question to be answered now is this: TO SUE OR NOT TO SUE?
What do you think?
Gosh, we in the UK needed that boost of jingoism (at least, if you are white, non-Jewish and equipped with a British passport)! But it’s all very well to rejoice at the news that we have a new little Windsor. With all the joy and celebration, we must not forget that the blue-blooded infant might be in considerable danger!
I am sure that chiropractors know what I am talking about.
KISS (Kinematic Imbalance due to Suboccipital Strain) is a term being used to describe a possible causal relation between imbalance in the upper neck joints in infants and symptoms like postural asymmetry, development of asymmetric motion patterns, hip problems, sleeping and eating disorders. Chiropractors are particularly fond of KISS. It is a problem that chiropractors tend to diagnose in new-borns.
This website explains further:
The kinematic imbalances brought on by the suboccipital strain at birth give rise to a concept in which symptoms and signs associated with the cervical spine manifest themselves into two easily recognizable clinical presentations. The leading characteristic is a fixed lateroflexion [called KISS I] or fixed retroflexion [KISS II]. KISS I may be associated with torticollis, asymmetry of the skull, C–scoliosis of the neck and trunk, asymmetry of the gluteal area and of the limbs, and retardation of the motor development of one side. KISS II, on the other hand, displays hyperextension during sleep, occipital flattening that may be asymmetrical, hunching of the shoulders, fixed supination of the arms, orofacial muscular hypotonia, failure to lift the trunk from a ventral position, and difficulty in breast feeding on one side. [34] The leading trademarks of both KISS I and KISS II are illustrated in Figure 1. [31]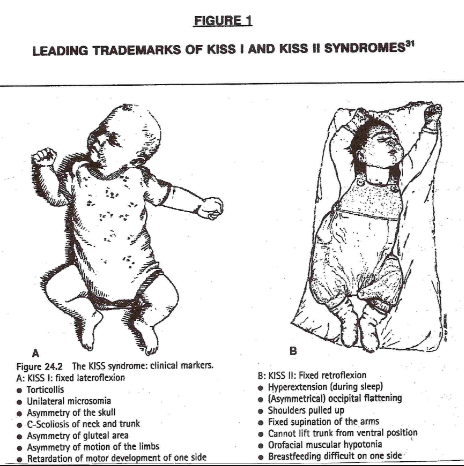
In essence, these birth experiences lay the groundwork for rationalizing the wisdom of providing chiropractic healthcare to the pediatric population…
END OF QUOTE
KISS must, of course, be treated with chiropractic spinal manipulation: the manual adjustment is the most common, followed by an instrument adjustment. This removes the neurological stress, re-balances the muscles and normal head position. Usually a dramatic change can be seen directly after the appropriate adjustment has been given…
Don’t frown! We all know that we can trust our chiropractors.
Evidence?
Do you have to insist on being a spoil-sport?
Alright, alright, the evidence tells a different story. A systematic review concluded that, given the absence of evidence of beneficial effects of spinal manipulation in infants and in view of its potential risks, manual therapy, chiropractic and osteopathy should not be used in infants with the KISS-syndrome, except within the context of randomised double-blind controlled trials.
And this means I now must worry for a slightly different reason: we all know that the new baby was born into a very special family – a family that seems to embrace every quackery available! I can just see the baby’s grandfather recruiting a whole range of anti-vaccinationists, tree-huggers, spoon-benders, homeopaths, faith healers and chiropractors to look after the new-born.
By Jove, one does worry about one’s Royals!
I have often criticised papers published by chiropractors.
Not today!
This article is excellent and I therefore quote extensively from it.
The objective of this systematic review was to investigate, if there is any evidence that spinal manipulations/chiropractic care can be used in primary prevention (PP) and/or early secondary prevention in diseases other than musculoskeletal conditions. The authors conducted extensive literature searches to locate all studies in this area. Of the 13.099 titles scrutinized, 13 articles were included (8 clinical studies and 5 population studies). They dealt with various disorders of public health importance such as diastolic blood pressure, blood test immunological markers, and mortality. Only two clinical studies could be used for data synthesis. None showed any effect of spinal manipulation/chiropractic treatment.
The authors concluded that they found no evidence in the literature of an effect of chiropractic treatment in the scope of PP or early secondary prevention for disease in general. Chiropractors have to assume their role as evidence-based clinicians and the leaders of the profession must accept that it is harmful to the profession to imply a public health importance in relation to the prevention of such diseases through manipulative therapy/chiropractic treatment.
In addition to this courageous conclusion (the paper is authored by a chiropractor and published in a chiro journal), the authors make the following comments:
Beliefs that a spinal subluxation can cause a multitude of diseases and that its removal can prevent them is clearly at odds with present-day concepts, as the aetiology of most diseases today is considered to be multi-causal, rarely mono-causal. It therefore seems naïve when chiropractors attempt to control the combined effects of environmental, social, biological including genetic as well as noxious lifestyle factors through the simple treatment of the spine. In addition, there is presently no obvious emphasis on the spine and the peripheral nervous system as the governing organ in relation to most pathologies of the human body.
The ‘subluxation model’ can be summarized through several concepts, each with its obvious weakness. According to the first three, (i) disturbances in the spine (frequently called ‘subluxations’) exist and (ii) these can cause a multitude of diseases. (iii) These subluxations can be detected in a chiropractic examination, even before symptoms arise. However, to date, the subluxation has been elusive, as there is no proof for its existence. Statements that there is a causal link between subluxations and various diseases should therefore not be made. The fourth and fifth concepts deal with the treatment, namely (iv) that chiropractic adjustments can remove subluxations, (v) resulting in improved health status. However, even if there were an improvement of a condition following treatment, this does not mean that the underlying theory is correct. In other words, any improvement may or may not be caused by the treatment, and even if so, it does not automatically validate the underlying theory that subluxations cause disease…
Although at first look there appears to be a literature on this subject, it is apparent that most authors lack knowledge in research methodology. The two methodologically acceptable studies in our review were found in PubMed, whereas most of the others were identified in the non-indexed literature. We therefore conclude that it may not be worthwhile in the future to search extensively the non-indexed chiropractic literature for high quality research articles.
One misunderstanding requires some explanations; case reports are usually not considered suitable evidence for effect of treatment, even if the cases relate to patients who ‘recovered’ with treatment. The reasons for this are multiple, such as:
- Individual cases, usually picked out on the basis of their uniqueness, do not reflect general patterns.
- Individual successful cases, even if correctly interpreted must be validated in a ‘proper’ research design, which usually means that presumed effect must be tested in a properly powered and designed randomized controlled trial.
- One or two successful cases may reflect a true but very unusual recovery, and such cases are more likely to be written up and published as clinicians do not take the time to marvel over and spend time on writing and publishing all the other unsuccessful treatment attempts.
- Recovery may be co-incidental, caused by some other aspect in the patient’s life or it may simply reflect the natural course of the disease, such as natural remission or the regression towards the mean, which in human physiology means that low values tend to increase and high values decrease over time.
- Cases are usually captured at the end because the results indicate success, meaning that the clinical file has to be reconstructed, because tests were used for clinical reasons and not for research reasons (i.e. recorded by the treating clinician during an ordinary clinical session) and therefore usually not objective and reproducible.
- The presumed results of the treatment of the disease is communicated from the patient to the treating clinician and not to a third, neutral person and obviously this link is not blinded, so the clinician is both biased in favour of his own treatment and aware of which treatment was given, and so is the patient, which may result in overly positive reporting. The patient wants to please the sympathetic clinician and the clinician is proud of his own work and overestimates the results.
- The long-term effects are usually not known.
- Further, and most importantly, there is no control group, so it is impossible to compare the results to an untreated or otherwise treated person or group of persons.
Nevertheless, it is common to see case reports in some research journals and in communities with readers/practitioners without a firmly established research culture it is often considered a good thing to ‘start’ by publishing case reports.
Case reports are useful for other reasons, such as indicating the need for further clinical studies in a specific patient population, describing a clinical presentation or treatment approach, explaining particular procedures, discussing cases, and referring to the evidence behind a clinical process, but they should not be used to make people believe that there is an effect of treatment…
For groups of chiropractors, prevention of disease through chiropractic treatment makes perfect sense, yet the credible literature is void of evidence thereof. Still, the majority of chiropractors practising this way probably believe that there is plenty of evidence in the literature. Clearly, if the chiropractic profession wishes to maintain credibility, it is time seriously to face this issue. Presently, there seems to be no reason why political associations and educational institutions should recommend spinal care to prevent disease in general, unless relevant and acceptable research evidence can be produced to support such activities. In order to be allowed to continue this practice, proper and relevant research is therefore needed…
All chiropractors who want to update their knowledge or to have an evidence-based practice will search new information on the internet. If they are not trained to read the scientific literature, they might trust any article. In this situation, it is logical that the ‘believers’ will choose ‘attractive’ articles and trust the results, without checking the quality of the studies. It is therefore important to educate chiropractors to become relatively competent consumers of research, so they will not assume that every published article is a verity in itself…
END OF QUOTES
YES, YES YES!!!
I am so glad that some experts within the chiropractic community are now publishing statements like these.
This was long overdue.
How was it possible that so many chiropractors so far failed to become competent consumers of research?
Do they and their professional organisations not know that this is deeply unethical?
Actually, I fear they do and did so for a long time.
Why then did they not do anything about it ages ago?
I fear, the answer is as easy as it is disappointing:
If chiropractors systematically trained to become research-competent, the chiropractic profession would cease to exist; they would become a limited version of physiotherapists. There is simply not enough positive evidence to justify chiropractic. In other words, as chiropractic wants to survive, it has little choice other than remaining ignorant of the current best evidence.
This week, I find it hard to decide where to focus; with all the fuzz about ‘Homeopathy Awareness Week’ it is easy to forget that our friends, the chiros are celebrating Chiropractic Awareness Week (9-15 April). On this occasion, the British Chiropractic Association (BCA), for instance, want people to keep moving to make a positive impact on managing and preventing back and neck pain.
Good advice! In a recent post, I even have concluded that people should “walk (slowly and cautiously) to the office of their preferred therapist, have a little rest there (say hello to the staff perhaps) and then walk straight back home.” The reason for my advice is based on the fact that there is precious little evidence that the spinal manipulations of chiropractors make much difference plus some worrying indications that they may cause serious damage.
It seems to me that, by focussing their PR away from spinal manipulations and towards the many other things chiropractors sometimes do – they often call this ‘adjunctive therapies’ – there is a tacit admission here that the hallmark intervention of chiros (spinal manipulation) is of dubious value.
A recent article entitled ‘Spinal Manipulative Therapy and Other Conservative Treatments for Low Back Pain: A Guideline From the Canadian Chiropractic Guideline Initiative’ seems to confirm this impression. Its objective was to develop a clinical practice guideline on the management of acute and chronic low back pain (LBP) in adults. The specific aim was to develop a guideline to provide best practice recommendations on the initial assessment and monitoring of people with low back pain and address the use of spinal manipulation therapy (SMT) compared with other commonly used conservative treatments.
The topic areas were chosen based on an Agency for Healthcare Research and Quality comparative effectiveness review, specific to spinal manipulation as a non-pharmacological intervention. The panel updated the search strategies in Medline and assessed admissible systematic reviews and randomized controlled trials. Evidence profiles were used to summarize judgments of the evidence quality and link recommendations to the supporting evidence. Using the Evidence to Decision Framework, the guideline panel determined the certainty of evidence and strength of the recommendations. Consensus was achieved using a modified Delphi technique. The guideline was peer reviewed by an 8-member multidisciplinary external committee.
For patients with acute (0-3 months) back pain, we suggest offering advice (posture, staying active), reassurance, education and self-management strategies in addition to SMT, usual medical care when deemed beneficial, or a combination of SMT and usual medical care to improve pain and disability. For patients with chronic (>3 months) back pain, we suggest offering advice and education, SMT or SMT as part of a multimodal therapy (exercise, myofascial therapy or usual medical care when deemed beneficial). For patients with chronic back-related leg pain, we suggest offering advice and education along with SMT and home exercise (positioning and stabilization exercises).
The authors concluded that a multimodal approach including SMT, other commonly used active interventions, self-management advice, and exercise is an effective treatment strategy for acute and chronic back pain, with or without leg pain.
I find this paper most interesting and revealing. Considering that it originates from the ‘Canadian Chiropractic Guideline Initiative’, it is remarkably shy about recommending SMT – after all their vision is “To enhance the health of Canadians by fostering excellence in chiropractic care.” They are thus not likely to be overly critical of the treatment chiropractors use most, i. e. SMT.
Perhaps this is also the reason why, in their conclusion, they seem to have rather a large blind spot, namely the risks of SMT. I have commented on this issue more often than I care to remember. Most recently, I posted this:
The reason why my stance, as expressed on this blog and elsewhere, is often critical about certain alternative therapies is thus obvious and transparent. For none of them (except for massage) is the risk/benefit balance positive. And for spinal manipulation, it even turns out to be negative. It goes almost without saying that responsible advice must be to avoid treatments for which the benefits do not demonstrably outweigh the risks.
HAPPY CHIROPRACTIC AWARENESS WEEK EVERYONE!
Chiropractic for kids? Yes, many chiropractors advocate (and earn good money with) it, yet it has been pointed out ad nauseam that the claim of being able of treating paediatric conditions is bogus (in fact, the BCA even lost a famous court case over this issue). But evidence does rarely seem to stop a chiro on a mission!
This website shows us how UK chiropractors plan to educate colleagues in ‘paediatric chiropractic’.
START OF QUOTE
INSPIRAL PAEDIATRIC SEMINARS ……..KIDS DYNAMIC DEVELOPMENT
- Join us for an exciting weekend of learning and skills development, in a supportive, enjoyable environment
- Learn the latest in Chiropractic Paediatrics from two world class leaders whose seminars receive rave reviews & letters of gratitude
- Increase your confidence and certainty in working with families in your community
- Fri 7th September 2-6pm, Sat 8th 9-6pm, Sun 9th 9-1pm I
- Investment £649 Earlybird ends August 15th Late fee £679
- Inclusions: Notes, Lunch on Saturday, onsite parking Park Inn Hotel, Bath Rd, Sipson, Heathrow UB7 0DU
NEURODEVELOPMENT
The seminar offers a neurological approach to healthy development in babies & children. It provides clinically relevant assessment, adjusting & clinical decision making. The focus will be on a Chiropractic wellness paradigm with a collaborative approach to promote healthy outcomes across the infant to adolescent years.
SAFE ADJUSTING
This is a hands-on program with a focus on neuro – developmentally appropriate adjusting of the spine and cranial dural system for health. We address some of the leading challenges with infant health and development, and teach exciting home care plans to facilitate optimum development.
YOUR TEACHERS
Genevieve & Rosemary Keating are leaders in Chiropractic paediatric health, learning & development.
Both are experienced Chiropractors, Facilitators, Diplomates of the American Chiropractic Neurology Board and Master Practitioners of Neuro Linguistics.
Rosemary holds a Masters in Chiropractic Paediatrics, and Genevieve is completing her PhD in Early Childhood Development.
END OF QUOTE
The event is hosted and organised by the ‘United Chiropractic Association UK’ (UCA), an organisation with a mission to ensure the public has access to vitalistic chiropractic care, which claims that chiropractors provide care that is safe. Because the techniques used by chiropractors are acquired over years of study and experience, chiropractors have an enviable safety record. In fact, in the words of a classic New Zealand study, chiropractic care is “remarkably safe.” Chiropractors use the latest methods. After years of study, licensing examinations and continuing education seminars, chiropractors in the United Kingdom are at the top of their game, using proven techniques and natural methods to help you get well and stay well.
The UCA is firmly rooted in the gospel of the founding fathers (D D Palmer, B J Palmer etc.): Chiropractic is concerned with the preservation and restoration of health, and focuses particular attention on the subluxation. A subluxation is a complex of functional and/or structural and/or pathological articular changes that compromise neural integrity and may influence organ system function and general health. A subluxation is evaluated, diagnosed, and managed through the use of chiropractic procedures based on the best available rational and empirical evidence. Subluxation is a fundamental axiom of the Chiropractic profession. The World Federation of Chiropractors (WFC) policy statement reaffirms the use of the term vertebral subluxation and it is defined succinctly and accepted by the World Health Organisation (WHO).
Thus, the UCA seems to subscribe to both principles of the Palmers. The first is subluxation and the second is profit.
_________________________________________________________________________________
Now, now, now – I must not be so sarcastic.
Try something constructive, Edzard!
You are absolutely correct, Edzard.
Here it is, my constructive contribution to this event:
I herewith offer the UCA to give two lectures during their course; one about the importance of critical thinking in healthcare, and one reviewing the evidence for and against chiropractic for paediatric conditions.
