risk
Due to polypharmacy and the rising popularity of so-called alternative medicines (SCAM), oncology patients are particularly at risk of drug-drug interactions (DDI) or herb-drug interactions (HDI). The aims of this study were to assess DDI and HDI in outpatients taking oral anticancer drugs.
All prescribed and non-prescribed medications, including SCAMs, were prospectively collected by hospital pharmacists during a structured interview with the patient. DDI and HDI were analyzed using four interaction software programs: Thériaque®, Drugs.com®, Hédrine, and Memorial Sloan Kettering Cancer Center (MSKCC) database. All detected interactions were characterized by severity, risk, and action mechanism. The need for pharmaceutical intervention to modify drug use was determined on a case-by-case basis.
A total of 294 patients were included, with a mean age of 67 years [55-79]. The median number of chronic drugs per patient was 8 [1-29] and 55% of patients used at least one SCAM. At least 1 interaction was found for 267 patients (90.8%): 263 (89.4%) with DDI, 68 (23.1%) with HDI, and 64 (21.7%) with both DDI and HDI. Only 13% of the DDI were found in Thériaque® and Drugs.com® databases, and 125 (2.5%) were reported with a similar level of risk on both databases. 104 HDI were identified with only 9.5% of the interactions found in both databases. 103 pharmaceutical interventions were performed, involving 61 patients (20.7%).
The authors concluded that potentially clinically relevant drug interactions were frequently identified in this study, showing that several databases and structured screening are required to detect more interactions and optimize medication safety.
These data imply that DDIs are more frequent than HDIs. This does, however, not tell us which are more important. One crucial difference between DDIs and HDIs is that the former are usually known to the oncology team who should thus be able to prevent them or deal with them appropriately; in contrast, HDIs are often not known to the oncology team because many patients fail to disclose the fact that they take herbal remedies. Some forget, some do not think of herbals as medicine, others may be worried about their physician’s reaction.
It follows that firstly, conventional healthcare practitioners should always ask about the usage of herbal remedies, and secondly, they need to be informed about which herbal remedy might interact with which drug. The first can easily be implemented into routine history-taking; the second is more problematic, not least because our knowledge about HDIs is still woefully incomplete. In view of this, it might often be wise to tell patients to stop taking herbal remedies while they are on prescription drugs.
Vertebral artery dissections (VAD) are a rare but important cause of ischemic stroke, especially in younger patients. Many etiologies have been identified, including motor vehicle accidents, cervical fractures, falls, physical exercise, and, as I have often discussed on this blog, cervical chiropractic manipulation. The goal of this study was to investigate the subgroup of patients who suffered a chiropractor-associated injury and determine how their prognosis compared to other-cause VAD.
The researchers, neurosurgeons from Chicago, conducted a retrospective chart review of 310 patients with vertebral artery dissections who presented at their institution between January 2004 and December 2018. Variables included demographic data, event characteristics, treatment, radiographic outcomes, and clinical outcomes measured using the modified Rankin Scale.
Overall, 34 out of our 310 patients suffered a chiropractor-associated injury. These patients tended to be younger (p = 0.01), female (p = 0.003), and have fewer comorbidities (p = 0.005) compared to patients with other-cause VADs. The characteristics of the injuries were similar, but chiropractor-associated injuries appeared to be milder at discharge and at follow-up. A higher proportion of the chiropractor-associated group had injuries in the 0-2 mRS range at discharge and at 3 months (p = 0.05, p = 0.04) and no patients suffered severe long-term neurologic consequences or death (0% vs. 9.8%, p = 0.05). However, when a multivariate binomial regression was performed, these effects dissipated and the only independent predictor of a worse injury at discharge was the presence of a cervical spine fracture (p < 0.001).
The authors concluded that chiropractor-associated injuries are similar to VADs of other causes, and apparent differences in the severity of the injury are likely due to demographic differences between the two populations.
The authors of the present paper are clear: “chiropractic manipulations are a risk factor for vertebral artery dissections.” This fact is further supported by a host of other investigations. For instance, the Canadian Stroke Consortium found that 28% of strokes following cervical artery dissection were preceded by chiropractic neck manipulation. Dziewas et al. obtained a similar rate in patients with vertebral artery dissections. Many chiropractors are in denial; however, this is merely due to their overt conflicts of interest.
My conclusions from the accumulated evidence are this:
Spinal manipulations of the upper spine should not be routinely used for any condition. Patients who nevertheless insist on having them must be made aware of the risks and give informed consent.
I have reported about the risks of chiropractic manipulation many times before. This is not because, as some seem to believe, I have an axe to grind but because the subject is important. This week, another case of stroke after chiropractic manipulation was in the news. Some will surely say that it is alarmist to mention such reports which lack lots of crucial details. Yet, as long as chiropractors do not establish a proper monitoring system where serious adverse effects of spinal manipulation are noted, I think it is important to record even incomplete cases in this fashion.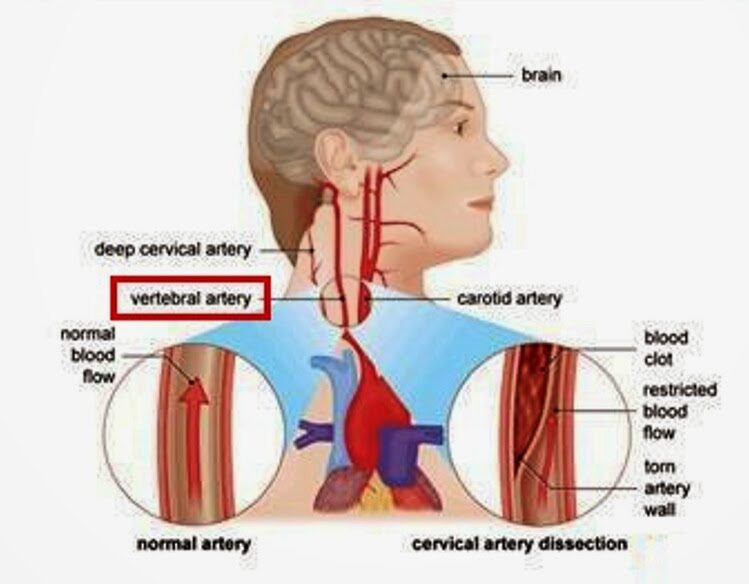
Barbara Shand is a working mom who lives in Alberta, Canada. She went to see a chiropractor because she had neck pain. “Near the very end of the appointment, the chiropractor asked: ‘Do you want your neck adjusted?’ I said: ‘Sure.’” “As soon as she did it, everything went black,” Shand recalls.
The patient was then rushed to a hospital by ambulance. “When I did open my eyes, I couldn’t focus. It was all blurry, I had massive vertigo, I didn’t know what was up or down,” Shand told the journalist. The diagnosis, Shand explains, was a right vertebral artery dissection, followed by a stroke. Mrs. Sands continues to struggle with coordination and balance.
The Alberta College and Association of Chiropractors acknowledges “there have been reported cases of stroke associated with visits to various healthcare practitioners, including those that provide cervical spine manipulation.” But they claim it is rare. They did not comment on the informed consent which, according to Shand’s description, was more than incomplete.
The fact that the ACAC admits that such events have happened before is laudable and a step in the right direction (some chiropractic organizations don’t even go that far). Yet, their caveat that such cases are rare is problematic. Without a monitoring system, nobody can tell how frequent they are! What we do see is merely the tip of a much bigger iceberg. There have been hundreds of cases like Mrs. Shand. The truth of the matter is this: Chiropractic neck manipulations are not supported by sound evidence of effectiveness for any condition. This means that even rare risks (if they are truly rare) would tilt the risk/benefit balance into the negative.
The conclusion is, I think, to avoid neck manipulations at all costs. Or, as one neurologist once put it:
don’t let the buggars touch your neck!
‘CLAMP DOWN ON THE BOGUS SCIENCE OF HOMEOPATHY’ is the title of a comment by Oliver Klamm in The Times today. Here is the background to his article.
In September 2020, the website of Homeopathy UK, www.homeopathy-uk.org, featured a page titled “Conditions Directory” with text that stated “Please find below a list of conditions where homeopathy can help …” followed by a list of medical conditions that included depression, diabetes, infertility, psoriasis and asthma. When consumers clicked-through the links to the conditions listed on that page, they were taken to separate pages for each that contained anecdotal descriptions from doctors detailing how they had applied homeopathic methods to the relevant conditions.
The UK Advertising Standards Authority received a complainant that challenged whether the ad discouraged essential treatment for conditions for which medical supervision should be sought, namely depression, diabetes, infertility, psoriasis and asthma.
The response of ‘Homeopathy UK’ said that, as a registered charity, they sought to share information about homeopathy for the benefit of others, rather than for commercial gain, and that they would always recommend that patients seeking homeopathic care did so under the supervision of a qualified medical practitioner…
The ASA upheld the complaint and argued as follows:
The CAP Code required that marketers must not discourage essential treatment for conditions for which medical supervision should be sought. For example, they must not offer specific advice on, diagnosis or treatment for such conditions unless that advice, diagnosis or treatment was conducted under the supervision of a suitably qualified medical professional. The ad referred to “depression”, “diabetes”, “infertility”, “psoriasis” and “asthma”, which we considered were conditions for which medical supervision should be sought. Any advice, diagnosis or treatment, therefore, must be conducted under the supervision of a suitably qualified medical professional. We acknowledged that the articles had been written by GMC-registered doctors, who we considered would be suitably qualified to offer advice, diagnosis or treatment. However, we noted that the ad and the articles to which it linked referred to homeopathy in general, rather than treatment by a specific individual. We understood that there were no minimum professional qualifications required to practice homeopathy, which could result in consumers being advised, diagnosed, or treated for the conditions listed in the ad by a practitioner with no medical qualification. We therefore considered Homeopathy UK would not be able to demonstrate that all such treatment would be conducted under the supervision of a suitably qualified health professional.
Furthermore, we understood that, although elsewhere on the website there were links to specific clinics, not all treatment would be conducted under the supervision of a suitably qualified health professional across those clinics. Because Homeopathy UK had not supplied evidence that treatment would always be carried out by a suitably qualified health professional. Also, because reference to the conditions listed in the ad, and discussed in the related articles, could discourage consumers from seeking essential treatment under the supervision of a suitably qualified health professional, we concluded that the ad had breached the Code.
On that point the ad breached CAP Code (Edition 12) rule 12.2 (Medicines, medical devices, health-related products and beauty products).
The ad must not appear again in the form complained about. We told Homeopathy UK to ensure their future marketing communications did not to refer to conditions for which advice should be sought from suitably qualified health professionals.
___________________________
Depression, diabetes, and asthma have few things in common. Just two characteristics stand out, in my view:
- they are potentially fatal;
- homeopathy is ineffective in changing their natural history.
- It was therefore high time that the ASA stopped this criminally dangerous nonsense of deluded homeopaths.
The article by Oliver Klamm concludes with the following wise words about homeopathy:
“For public officials and opinion formers, the time for appeasing this dangerous quackery should be long past.”
I have not often seen a paper reporting a small case series with such an impressively long list of authors from so many different institutions:
- Hospital of Lienz, Lienz, Austria.
- WissHom: Scientific Society for Homeopathy, Koethen, Germany; Umbrella Organization for Medical Holistic Medicine, Vienna, Austria; Vienna International Academy for Holistic Medicine (GAMED), Otto Wagner Hospital Vienna, Austria; Professor Emeritus, Medical University of Vienna, Department of Medicine I, Vienna, Austria. Electronic address: [email protected].
- Resident Specialist in Hygiene, Medical Microbiology and Infectious Diseases, Außervillgraten, Austria.
- St Mary’s University, London, UK.
- Umbrella Organization for Medical Holistic Medicine, Vienna, Austria.
- Shaare Zedek Medical Center, The Center for Integrative Complementary Medicine, Jerusalem, Israel.
- Apotheke Zum Weißen Engel – Homeocur, Retz, Austria.
- Reeshabh Homeo Consultancy, Nagpur, India.
- Umbrella Organization for Medical Holistic Medicine, Vienna, Austria; Vienna International Academy for Holistic Medicine (GAMED), Otto Wagner Hospital Vienna, Austria; Chair of Complementary Medicine, Medical Faculty, Sigmund Freud University Vienna, Austria; KLITM: Karl Landsteiner Institute for Traditional Medicine and Medical Anthropology, Vienna, Austria.
- WissHom: Scientific Society for Homeopathy, Koethen, Germany.
In fact, there are 12 authors reporting about 13 patients! But that might be trivial – so, let’s look at the paper itself. The aim of this study was to describe the effect of adjunctive individualized homeopathic treatment delivered to hospitalized patients with confirmed symptomatic SARS-CoV-2 infection.
Thirteen patients with COVID-19 were admitted. The mean age was 73.4 ± 15.0 (SD) years. The treating homeopathic doctor was instructed by the hospital on March 27, 2020, to adjunctively treat all inpatient COVID-19 patients homeopathically. The high potency homeopathic medicinal products were administered orally. Five globules were administered sublingually where they dissolved, three times a day. In ventilated patients in the ICU, medication was administered as a sip from a water beaker or 1 ml three times a day using a syringe. All ventilated patients exhibited dry cough resulting in respiratory failure. They were given Influenzinum, as were the patients at the general inpatient ward.
Twelve patients (92.3%) were speedily discharged without relevant sequelae after 14.4 ± 8.9 days. A single patient admitted in an advanced stage of septic disease died in the hospital. A time-dependent improvement of relevant clinical symptoms was observed in the 12 surviving patients. Six (46.2%) were critically ill and treated in the intensive care unit (ICU). The mean stay at the ICU of the 5 surviving patients was 18.8 ± 6.8 days. In six patients (46.2%) gastrointestinal disorders accompanied COVID-19.
The authors conclude that adjunctive homeopathic treatment may be helpful to treat patients with confirmed COVID-19 even in high-risk patients especially since there is no conventional treatment of COVID-19 available at present.
In the discussion section of the paper, the authors state this: “Given the extreme variability of pathology and clinical manifestations, a single universal preventive homeopathic medicinal product does not seem feasible. Yet homeopathy may have a relevant role to play precisely because of the number and diversity of its homeopathic medicinal products which can be matched with the diversity of the presentations. Patients with mild forms of disease can use homeopathic medicinal products at home using our simple algorithm. As this Case series suggests, adjunctive homeopathic treatment can play a valuable role in more serious presentations. For future pandemics, homeopathy agencies should be prepared by establishing rapid-response teams and efficacious lines of communication.”
There is nothing in this paper that would lead me to conclude that the homeopathic remedies had a positive effect on the natural history of the disease. All this article actually does do is this: it provides a near-perfect insight into the delusional megalomania of some homeopaths. These people are even more dangerous than I had feared.
The purpose of this study was to describe changes in opioid-therapy prescription rates after a family medicine practice included on-site chiropractic services. It was designed as a retrospective analysis of opioid prescription data. The database included opioid prescriptions written for patients seeking care at the family medicine practice from April 2015 to September 2018. In June 2016, the practice reviewed and changed its opioid medication practices. In April 2017, the practice included on-site chiropractic services. Opiod-therapy use was defined as the average rate of opioid prescriptions overall medical providers at the practice.
There was a significant decrease of 22% in the average monthly rate of opioid prescriptions after the inclusion of chiropractic services (F1,40 = 10.69; P < .05). There was a significant decrease of 32% in the prescribing rate of schedule II opioids after the inclusion of chiropractic services (F2,80 = 6.07 for the Group × Schedule interaction; P < .05). The likelihood of writing schedule II opioid prescriptions decreased by 27% after the inclusion of chiropractic services (odds ratio, 0.73; 95% confidence interval, 0.59-0.90). Changes in opioid medication practices by the medical providers included prescribing a schedule III or IV opioid rather than a schedule II opioid (F6,76 = 29.81; P < .05) and a 30% decrease in the daily doses of opioid prescriptions (odds ratio, 0.70; 95% confidence interval, 0.50-0.98).
The authors concluded that this study demonstrates that there were decreases in opioid-therapy prescribing rates after a family medicine practice included on-site chiropractic services. This suggests that inclusion of chiropractic services may have had a positive effect on prescribing behaviors of medical physicians, as they may have been able to offer their patients additional nonpharmaceutical options for pain management.
The authors are correct in concluding the inclusion of chiropractic services MAY have had a positive effect. And then again, it may not!
Cause and effect cannot be established by correlation alone.
CORRELATION IS NOT CAUSATION!
And even if the inclusion of chiropractic services caused the positive effect, it would not prove that chiropractic is effective in the management of pain. It would only mean that the physicians had an option that helped them to write fewer opioid prescriptions. Had they hired a crystal healer or a homeopath or a faith healer or any other practitioner of an ineffective therapy, the findings might have been very similar.
The long and short of it is this: if we want to use fewer opioids, there is only one way to achieve it: we must prescribe less.
Mind-body interventions (MBIs) are one of the top ten so-called alternative medicine (SCAM) approaches utilized in pediatrics, but there is limited knowledge on associated adverse events (AE). The objective of this review was to systematically review AEs reported in association with MBIs in children.
Electronic databases MEDLINE, Embase, CINAHL, CDSR, and CCRCT were searched from inception to August 2018. The authors included primary studies on participants ≤ 21 years of age that used an MBI. Experimental studies were assessed for whether AEs were reported on or not, and all other study designs were included only if they reported an AE.
A total of 441 were included as primary pediatric MBI studies. Of these, 377 (85.5%) did not explicitly report the presence/absence of AEs or a safety assessment. In total, there were 64 included studies: 43 experimental studies reported that no AE occurred, and 21 studies reported AEs. A total of 37 AEs were found, of which the most serious were grade 3. Most of the studies reporting AEs did not report on severity (81.0%) or duration of AEs (52.4%).
The authors concluded that MBIs are popularly used in children; however associated harms are often not reported and lack important information for meaningful assessment.
SCAM is far too often considered to be risk-free. This phenomenon is particularly stark if the SCAM in question does not involve physical or pharmacological treatments. Thus MBIs are seen and often waved through as especially safe. Consequently, many researchers do not even bother to monitor AEs in their clinical trials. This might be understandable, but it is nevertheless a violation of research ethics.
This new review is important in that it highlights these issues. It is high time that we stop giving researchers in SCAM the benefit of the doubt. They may or may not make honest mistakes when not reporting AEs. In any case, it is clear that they are not properly trained and supervised. All too often, we still see clinical trials run by amateurs who have little idea of methodology and even less of ethics. The harm this phenomenon does is difficult to quantify, but I fear it is huge.
The usage of so-called alternative medicine (SCAM) in pediatric settings has been high for some time. However, the risks of pediatric SCAM use remain under-investigated. Almost 20 years ago, I published this systematic review:
Unconventional therapies have become popular in paediatric and adolescent populations. It is therefore important to define their risks. The aim of this systematic review was to summarise the recent evidence. Computerised literature searches were carried out in five databases to identify all recent reports of adverse events associated with unconventional therapies in children. The reports were summarised in narrative and tabular form. The results show that numerous case reports and several case series have been published since 1990. Investigations of a more systematic nature are, however, rare. Most of the adverse events were associated with herbal medications. Inadequately regulated herbal medicines may contain toxic plant material, be contaminated with heavy metals, or be adulterated with synthetic drugs. The adverse events included bradycardia, brain damage, cardiogenic shock, diabetic coma, encephalopathy, heart rupture, intravascular haemolysis, liver failure, respiratory failure, toxic hepatitis and death. A high degree of uncertainty regarding a causal relationship between therapy and adverse event was frequently noted. The size of the problem and its importance relative to the well-documented risks of conventional treatments are presently unknown. Several unconventional therapies may constitute a risk to the health of children and adolescents. At present, it is impossible to provide reliable incidence figures. It seems important to be vigilant and investigate this area more systematically.
Nothing much has happened since in terms of systematic investigation. But now, a 3-year survey was carried out at the Dutch Pediatric Surveillance Unit. Pediatricians were asked to register cases of adverse events associated with pediatric SCAM usage.
In 3 years, 32 unique adverse events were registered. Twenty-two of these adverse events were indirect and not related to the specific SCAM therapy but due to delaying, changing, or stopping of regular treatment, a deficient or very restrictive diet, or an incorrect diagnosis by a SCAM therapist. These events were associated with many different SCAM therapies.
Nine events were deemed direct adverse events like bodily harm or toxicity and one-third of them occurred in infants. Only supplements, manual therapies, and (Chinese) herbs were involved in these nine events. In one case, there was a risk of a serious adverse event but the harm had not yet occurred.
The authors concluded that relatively few cases of adverse events associated with pediatric SCAM usage were found, mostly due to delaying or stopping conventional treatment. Nevertheless, parents, pediatricians, and SCAM providers should be vigilant for both direct and indirect adverse events in children using SCAM, especially in infants.
The number of cases seems small indeed, but there may be many further adverse events that went unreported. Here are 4 of the documented cases of severe and life-threatening consequences:
- An 8-year-old child with autoimmune hypothyroidism had his prescribed replaced with an ineffective herbal remedy.
- A 14-year-old child developed septic shock with multiple organ failure after receiving homeopathy for acute appendicitis.
- A 14-year-old child needed colectomy after ineffective naturopathic treatments for colitis.
- A 5-year-old developed secondary adrenal insufficiency after his eczema was treated with Chinese herbal remedies adulterated with large doses of corticosteroids.
In view of the risks – even if small – I suggest that, in pediatric settings, we employ only those SCAMs that are supported by solid evidence. And those are very few indeed.
Thread embedding acupuncture therapy (TEAT) involves the insertion of thread at specific points on the body surface. The claim is that TEAT provides a sustained stimulation of acupoints and is therefore superior to needle acupuncture. Initially, TEAT was used in China to treat obesity, today it is employed to treat many conditions, including musculoskeletal conditions such as ankle sprain, shoulder pain, lumbar intervertebral disc herniation, and plantar fasciitis. Its effectiveness is, however, doubtful and so is its safety.
This review evaluated the safety of thread embedding acupuncture therapy (TEAT) and discuss the prevention and treatment of some adverse events (AEs).
Databases, including China National Knowledge Infrastructure (CNKI), CBMdisc, Wanfang, VIP databases and PubMed, MEDLINE, EMBASE, and Web of Science, were searched from their inception to January 2020. Included were randomized controlled trials (RCTs) and case reports in which AEs with TEAT were reported. Cochrane Collaboration’s tool and RevMan V.5.3.3 software were used to evaluate the quality of the studies.
A total of 61 articles (45 RCTs and 16 case reports) with a total of 620 cases of AEs were included in this review. These studies were published in two countries: China and South Korea. Twenty-eight kinds of AEs were noted. The most common AEs were induration, bleeding and ecchymosis, redness and swelling, fever, and pain. They accounted for 75.35% of all AEs. Most AEs were mild.; The rarest AEs were epilepsy, irregular menstruation, skin ulcer, thread malabsorption, and fat liquefaction, with 1 case each. Not all of them had a clear causal relationship with TEAT. Most of the AEs were local reactions and systemic reactions accounted for only 1.27%. Although the included studies showed that AEs were very commonly encountered (11.09%), only 5 cases of severe AEs reported from 2013 to 2017 (0.1%) by using catgut thread, which is rarely employed nowadays with new absorbable surgical suture being more popular. All of the patients with severe AEs were recovered after symptomatic treatment with no sequelae.
The authors concluded that the evidence showed that TEAT is a relatively safe and convenient therapy especially since application of new absorbable surgical suture. Improving practitioner skills, regulating operations, and paying attention to the patients’ conditions may reduce the incidence of AEs and improve safety of TEAT.
TEAT was initially used in China only but recently it has become popular elsewhere as well. Therefore the question about its risks has become relevant. The present paper is interesting in that it demonstrates that AEs do occur with some regularity. The authors’ conclusion that TEAT is “relatively safe” is, however, not justified because:
- the total sample size was not large enough for a generalizable conclusion;
- only RCTs and case reports were included, whereas case series and case-control studies (which would provide more relevant data) were excluded or might not even exist;
- RCTs of acupuncture often fail to mention or under-report AEs;
- acupuncture papers from China are notoriously unreliable.
So, all we can conclude from the evidence presented here is that AEs after TEAT do occur and do not seem to be all that rare. As the efficacy of TEAT has not been shown beyond doubt, this must inevitably lead to the conclusion that the risk-benefit balance of TEAT is not positive. In turn, that means that TEAT cannot be recommended as a treatment for any condition.
On 17/2/2020 I posted this article:
The drop in cases and deaths due to COVID-19 infections in India has been attributed to India’s national policy of using homeopathy. Early in the epidemic, the national “Ministry of AYUSH, recommended the use of Arsenic album 30 as preventive medicine against COVID-19. Its prophylactic use has been advised in states like Karnataka, Tamil Nadu, Kerala, and Maharashtra. The ‘OFFICIAL HOMEOPATHY RESOURCE’ is now claiming that homeopathy is the cause of the observed outcome…
If you click on the link, you will find that the OFFICIAL HOMEOPATHY RESOURCE has now removed the original. No problem! Thanks to Alan Henness, we can still access it; he announced in a tweet that he has archived a copy. So, here is the full article again:
India’s National Policy of Using Homeopathic Medicine To Prevent COVID is Dramatically Working
A dramatic plunge in cases and deaths of COVID in India can be attributed to India’s national policy of using homeopathy.
Early in the epidemic, the national “Ministry of AYUSH, (medical alternatives), in its guidelines, issued an advisory to states across India recommending the use of a traditional homeopathic drug, Arsenic album 30 as a form of preventive medicine against COVID-19. Its prophylactic use has been advised in states like Karnataka, Tamil Nadu, Kerala and Maharashtra and in some places, it has been used in high-risk areas. In places like Bhopal, claims were raised when doctors said that mild COVID cases were successfully treated with homeopathy.” [Times of India]
And now the results of that policy and use are clear, even though scientists in the conventional paradigm are mystified as to why the drop is so dramatic. They know nothing about homeopathy and its history of successfully treating epidemics.
India has a population of 1 billion, 300 million people. Relative to this massive population the number of cases per day and especially the number of deaths per day are now exceptionally low. According to the Daily Mail:
“Scientists are trying to work out why coronavirus cases in India are falling when at one point it looked like the country might overtake the US as the worst-hit nation.
In September the country was reporting some 100,00 new cases per day, but that went into decline in October and is now sitting at around 10,000 per day – leaving experts struggling to explain why.”


But why?
Why did the original disappear?
The reason seems obvious:
Saturday’s official toll recorded another 2,600 deaths and 340,000 new infections in India, bringing the total number of cases to 16.5 million, second only to the US. There have been 190,000 deaths attributed to Covid in India since the start of the pandemic. These figures are dramatic but most likely they are gross underestimates of the truth.
The egg on the face of homeopathy gets bigger if we consider things like the COVID-19 advice from ‘HOMEOPATHY INTERNATIONAL’, or the fact that UK’s biggest provider of homeopathy training encouraged the use of homeopathic potions made with phlegm to protect against and treat Covid-19. The egg finally turns into a veritable omelette, once we learn that the leading academic journal in homeopathy, HOMEOPATHY, promoted the idea that homeopathic have a place in the fight against the pandemic – not just once but repeatedly – and that the leading UK homeopath, Elizabeth Thompson, recommended homeopathy for COVID-19 infections after herself falling ill with the virus.
No, I do not feel the slightest tinge of Schadenfreude, about all this. I am writing about it because I still hope that it will prevent some people from risking their health with useless therapies and perhaps even stop some charlatans to make ridiculously irresponsible claims about them. So, please do me a favor and heed my message:
