neck-pain
One of the numerous conditions chiropractors, osteopaths, and other manual therapists claim to treat effectively is tension-type headache (TTH). For this purpose, they (in particular, chiropractors) often use high-velocity, low-amplitude manipulations of the neck. They do so despite the fact that the evidence for these techniques is less than convincing.
This systematic review evaluated the evidence about the effectiveness of manual therapy (MT) on pain intensity, frequency, and impact of pain in individuals with tension-type headache (TTH).
Medline, Embase, Scopus, Web of Science, CENTRAL, and PEDro were searched in June 2020. Randomized clinical trials that applied MT not associated with other interventions for TTH were selected. The level of evidence was synthesized using GRADE, and Standardized Mean Differences (SMD) were calculated for meta-analysis.
Fifteen studies were included with a total sample of 1131 individuals. The analyses show that high-velocity, low-amplitude techniques were not superior to no treatment in reducing pain intensity (SMD = 0.01, low evidence) and frequency (SMD = -0.27, moderate evidence). Soft tissue interventions were superior to no treatment in reducing pain intensity (SMD = -0.86, low evidence) and frequency of pain (SMD = -1.45, low evidence). Dry needling was superior to no treatment in reducing pain intensity (SMD = -5.16, moderate evidence) and frequency (SMD = -2.14, moderate evidence). Soft tissue interventions were not superior to no treatment and other treatments on the impact of headache.
The authors concluded that manual therapy may have positive effects on pain intensity and frequency, but more studies are necessary to strengthen the evidence of the effects of manual therapy on subjects with tension-type headache. Implications for rehabilitation soft tissue interventions and dry needling can be used to improve pain intensity and frequency in patients with tension type headache. High velocity and low amplitude thrust manipulations were not effective for improving pain intensity and frequency in patients with tension type headache. Manual therapy was not effective for improving the impact of headache in patients with tension type headache.
So, this review shows that:
- soft tissue interventions are better than no treatment,
- dry needling is better than no treatment.
These two results fail to impress me. Due to a placebo effect, almost any treatment should be better than no therapy at all.
ALMOST, because high-velocity, low-amplitude techniques were not superior to no treatment in reducing the intensity and frequency of pain. This, I feel, is an important finding that needs an explanation.
As it is only logical that high-velocity, low-amplitude techniques must also produce a positive placebo effect, the finding can only mean that these manipulations also generate a negative effect that is strong enough to cancel the positive response to placebo. (In addition, they can also cause severe complications via arterial dissections, as discussed often on this blog.)
Too complicated?
Perhaps; let me, therefore, put it simply and use the blunt words of a neurologist who once was quoted saying this:
DON’T LET THE BUGGARS TOUCH YOUR NECK!
Pancoast tumors, also called superior sulcus tumors, are a rare type of cancer affecting the lung apex. These tumors can spread to the brachial plexus and spine and present with symptoms that appear to be of musculoskeletal origin. Patients with an advanced Pancoast tumor may thus feel intense, constant, or radiating pain in their arms, around their chest wall, between their shoulder blades, or traveling into their upper back or armpit. In addition, a Pancoast tumor may cause the following symptoms:
- Swelling in the upper arm
- Chest tightness
- Weakness or loss of coordination in the hand muscles
- Numbness or tingling sensations in the hand
- Loss of muscle tissue in the arm or hand
- Fatigue
- Unexplained weight loss
This case report details the story of a 59-year-old Asian man who presented to a chiropractor in Hong Kong with a 1-month history of neck and shoulder pain and numbness. His symptoms had been treated unsuccessfully with exercise, medications, and acupuncture. He had a history of tuberculosis currently treated with antibiotics and a 50-pack-year history of smoking.
Cervical magnetic resonance imaging (MRI) revealed a small cervical disc herniation thought to correspond with radicular symptoms. However, when the patient did not respond to a brief trial of chiropractic treatment, the chiropractor referred the patient back to the chest hospital for further testing, which confirmed the diagnosis of a Pancoast tumor. The patient was then referred for medical care and received radiotherapy and chemotherapy. At 2 months’ follow-up, the patient noted feeling lighter with less severe neck and shoulder pain and numbness. He also reported that he could sleep longer but still had severe pain upon waking for 2–3 hours, which subsided through the day.
A literature review identified six previously published cases in which a patient presented to a chiropractor with an undiagnosed Pancoast tumor. All patients had shoulder, spine, and/or upper extremity pain.
The authors concluded that patients with a previously undiagnosed Pancoast tumor can present to chiropractors given that these tumors may invade the brachial plexus and spine, causing shoulder, spine, and/or upper extremity pain. Chiropractors should be aware of the clinical features and risk factors of Pancoast tumors to readily identify them and refer such patients for medical care.
This is an important case report, in my view. It demonstrates that symptoms treated by chiropractors, osteopaths, and physiotherapists on a daily basis can easily be diagnosed wrongly. It also shows how vital it is that the therapist reacts responsibly to the fact that his/her treatments are unsuccessful. Far too often, the therapist has an undeniable conflict of interest and will say: “Give it more time, and, in my experience, symptoms will respond.”
The chiropractor in this story was brilliant and did the unusual thing of not continuing to treat his patient. However, I do wonder: might he be the exception rather than the rule?
If you go on Twitter you will find that chiropractors are keen like mustard to promote the idea that, after a car accident, you should consult a chiropractor. Here is just one Tweet that might stand for hundreds, perhaps even thousands:
Recovering from a car accident? If you have accident-related injuries such as whiplash, chiropractic care may provide relief. Treatments like spinal manipulation and soft tissue therapy can aid in your recovery.
In case you don’t like Twitter, you could also go on the Internet where you find hundreds of websites that promote the same idea. Here are just two examples:
There is no question, chiropractors earn much of their living by treating patients suffering from whiplash (neck injury caused by sudden back and forth movement of the neck often causing neck pain and stiffness, shoulder pain, and headache) after a car accident with spinal manipulation.
Why?
There are two not mutually exclusive possibilities:
- They think it is effective.
- It brings in good money.
I have no doubt about the latter notion, yet I think we should question the first. Is there really good evidence that chiropractic manipulations are effective for whiplash?
When I was head of the PMR department at the University of Vienna, treating whiplash was my team’s daily bread. At the time, our strategy was to treat each patient according to the whiplash stage and to his/her individual signs and symptoms. Manipulations were generally considered to be contra-indicated. But that was about 30 years ago. Perhaps the evidence has now changed. Perhaps manipulation therapy has been shown to be effective for certain types of whiplash injuries?
To find out, I did a few Medline searches. These did, however, not locate compelling evidence for spinal manipulation as a treatment of any stage of whiplash injuries. Here is an example of the evidence I found:
In 2008, the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders (Neck Pain Task Force) found limited evidence on the effectiveness of manual therapies, passive physical modalities, or acupuncture for the management of whiplash-associated disorders (WAD) or neck pain and associated disorders (NAD). This review aimed to update the findings of the Neck Pain Task Force, which examined the effectiveness of manual therapies, passive physical modalities, and acupuncture for the management of WAD or NAD. Its findings show the following: Evidence from 15 evaluation studies suggests that for recent neck pain and associated disorders grades I-II, cervical and thoracic manipulation provides no additional benefit to high-dose supervised exercises.
But this is most puzzling!
Why do chiropractors promote their manipulations for whiplash, if there is no compelling evidence that it does more good than harm? Again, there are two possibilities:
- They erroneously believe it to be effective.
- They don’t care but are in it purely for the money.
Whatever it is – and obviously not all chiropractors would have the same reason – I must point out that, in both cases, they behave unethically. Not being informed about the evidence related to the interventions used clearly violates healthcare ethics, and so does financially not informing and exploiting patients.
Earlier this year, I started the ‘WORST PAPER OF 2022 COMPETITION’. You will ask what is there to win in this competition? I agree: a competition without a prize is no fun. Therefore, I suggest offering the winner (that is the author of the winning paper) one of my books that best fits his/her subject. I am sure this will over-joy him or her. And how do we identify the winner? I suggest that I continue blogging about nominated papers (I hope to identify about 10 in total), and towards the end of the year, I let my readers decide democratically.
In this spirit of democratic voting, let me suggest to you ENTRY No 6:
This study was to ascertain the efficacy of dry cupping therapy (DCT) and optimal cup application time duration for cervical spondylosis (CS). It was designed as a randomized clinical trial involving 45 participants with clinically diagnosed CS. The eligible subjects were randomly allocated into three groups, each having 15 participants. Each of the three groups, i.e., A, B, and C, received DCT daily for 15 days for 8 min, 10 min, and 12 min, respectively. All the participants were evaluated at the baseline, 7th, and 15th day of the trial using the neck disability index (NDI) as well as the visual analog scale (VAS).
The baseline means ± SD of NDI and VAS scores were significantly reduced in all three groups at the end of the trial. Although all three groups were statistically equal in terms of NDI, group C demonstrated greater efficacy in terms of VAS.
The authors concluded that the per-protocol analysis showed that dry cupping effectively alleviated neck pain across all treatment groups. Although this effect on neck disability index was statistically equal in all three groups, the 12-min protocol was more successful in reducing pain.
Who would design such a study and why?
- The authors claim they wanted to ascertain the efficacy of DCT. A trial is for testing, not ascertaining. And this study does certainly not test for efficacy.
- The groups were too small to generate a meaningful result of what, in fact, was an equivalence study.
- Intra-group changes in symptoms between baseline and time points during treatment are irrelevant in a controlled trial.
- The slightly better results of group C are most likely due to chance or non-specific effects (a longer application of a placebo would generate better outcomes that a shorter one).
- The study participants had cervical spondylosis, yet the conclusion is about neck pain. The two are not identical.
- The title of the paper promises that we learn something about the safety of DCT. Sadly, a trial with just 45 patients has no chance in hell to pick up adverse effects in a reliable way.
- As there is no control group, the study cannot tell us anything about possible specific effects of DCT.
The authors of the study have impressive affiliations:
- Department of Ilaj bil Tadbir, Luqman Unani Medical College Hospital and Research Center, Bijapur, India.
- Department of Ilaj bil Tadbir, National Institute of Unani Medicine, Bengaluru, India.
- Department of Moalajat, Luqman Unani Medical College Hospital and Research Center, Bijapur, India.
I would have hoped that researchers from national institutions and medical colleges should be able to design a trial that has at least a small chance to produce a meaningful finding. As it turns out, my hope was badly disappointed.
Naprapathy is an odd variation of chiropractic. To be precise, it has been defined as a system of specific examination, diagnostics, manual treatment, and rehabilitation of pain and dysfunction in the neuromusculoskeletal system. It is aimed at restoring the function of the connective tissue, muscle- and neural tissues within or surrounding the spine and other joints. The evidence that it works is wafer-thin. Therefore rigorous studies are of interest.
The aim of this study was to evaluate the cost-effectiveness of manual therapy compared with advice to stay active for working-age persons with nonspecific back and/or neck pain.
The two interventions were:
- a maximum of 6 manual therapy sessions within 6 weeks, including spinal manipulation/mobilization, massage, and stretching, performed by a naprapath (index group),
- information from a physician on the importance to stay active and on how to cope with pain, according to evidence-based advice, on 2 occasions within 3 weeks (control group).
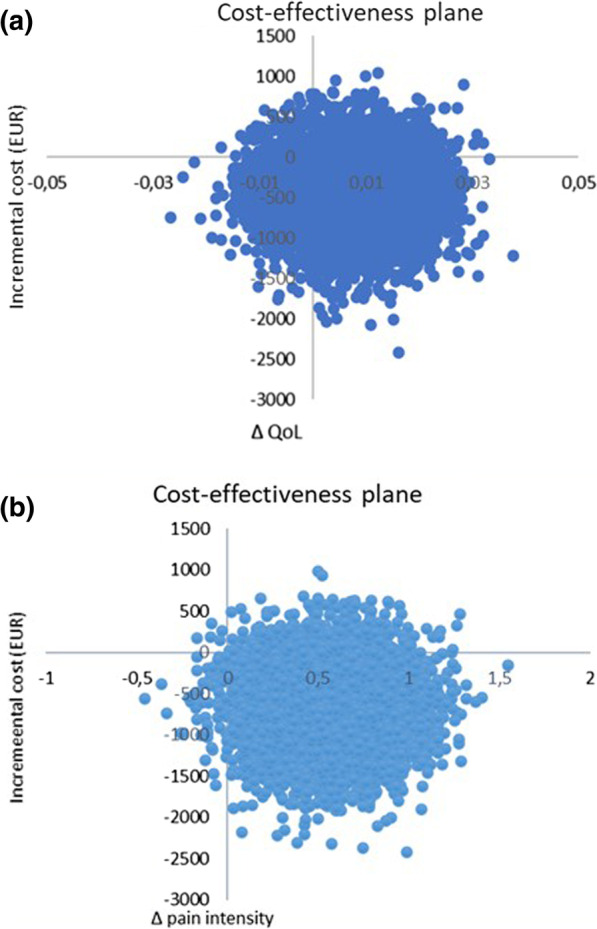
A cost-effectiveness analysis with a societal perspective was performed alongside a randomized controlled trial including 409 persons followed for one year, in 2005. The outcomes were health-related Quality of Life (QoL) encoded from the SF-36 and pain intensity. Direct and indirect costs were calculated based on intervention and medication costs and sickness absence data. An incremental cost per health-related QoL was calculated, and sensitivity analyses were performed.
The difference in QoL gains was 0.007 (95% CI – 0.010 to 0.023) and the mean improvement in pain intensity was 0.6 (95% CI 0.068-1.065) in favor of manual therapy after one year. Concerning the QoL outcome, the differences in mean cost per person were estimated at – 437 EUR (95% CI – 1302 to 371) and for the pain outcome the difference was – 635 EUR (95% CI – 1587 to 246) in favor of manual therapy. The results indicate that manual therapy achieves better outcomes at lower costs compared with advice to stay active. The sensitivity analyses were consistent with the main results.
Cost-effectiveness plane using bootstrapped incremental cost-effectiveness ratios for QoL and pain intensity outcomes
The authors concluded that these results indicate that manual therapy for nonspecific back and/or neck pain is slightly less costly and more beneficial than advice to stay active for this sample of working age persons. Since manual therapy treatment is at least as cost-effective as evidence-based advice from a physician, it may be recommended for neck and low back pain. Further health economic studies that may confirm those findings are warranted.
This is an interesting and well-conducted study. The differences between the groups seem small and of doubtful relevance. The authors acknowledge this fact by stating: “together with the clinical results from previously published studies on the same population the results suggest that manual therapy may be as cost-effective a treatment as evidence-based advice from a physician, for back and neck pain”. Moreover, the data do not convince me that the treatment per se was effective; it might have been the non-specific effects of touch and attention.
I have said it before: there is currently no optimal treatment for neck and back pain. Therefore, the findings even of rigorous cost-effectiveness studies will only generate lukewarm results.
Today, several UK dailies report about a review of osteopathy just published in BMJ-online. The aim of this paper was to summarise the available clinical evidence on the efficacy and safety of osteopathic manipulative treatment (OMT) for different conditions. The authors conducted an overview of systematic reviews (SRs) and meta-analyses (MAs). SRs and MAs of randomised controlled trials evaluating the efficacy and safety of OMT for any condition were included.
The literature searches revealed nine SRs or MAs conducted between 2013 and 2020 with 55 primary trials involving 3740 participants. The SRs covered a wide range of conditions including
- acute and chronic non-specific low back pain (NSLBP, four SRs),
- chronic non-specific neck pain (CNSNP, one SR),
- chronic non-cancer pain (CNCP, one SR),
- paediatric (one SR),
- neurological (primary headache, one SR),
- irritable bowel syndrome (IBS, one SR).
Although with different effect sizes and quality of evidence, MAs reported that OMT is more effective than comparators in reducing pain and improving the functional status in acute/chronic NSLBP, CNSNP and CNCP. Due
to the small sample size, presence of conflicting results and high heterogeneity, questionable evidence existed on OMT efficacy for paediatric conditions, primary headaches and IBS. No adverse events were reported in most SRs. The methodological quality of the included SRs was rated low or critically low.
The authors concluded that based on the currently available SRs and MAs, promising evidence suggests the possible effectiveness of OMT for musculoskeletal disorders. Limited and inconclusive evidence occurs for paediatric conditions, primary headache and IBS. Further well-conducted SRs and MAs are needed to confirm and extend the efficacy and safety of OMT.
This paper raises several questions. Here a just the two that bothered me most:
- If the authors had truly wanted to evaluate the SAFETY of OMT (as they state in the abstract), they would have needed to look beyond SRs, MAs or RCTs. We know – and the authors of the overview confirm this – that clinical trials of so-called alternative medicine (SCAM) often fail to mention adverse effects. This means that, in order to obtain a more realistic picture, we need to look at case reports, case series and other observational studies. It also means that the positive message about safety generated here is most likely misleading.
- The authors (the lead author is an osteopath) might have noticed that most – if not all – of the positive SRs were published by osteopaths. Their assessments might thus have been less than objective. The authors did not include one of our SRs (because it fell outside their inclusion period). Yet, I do believe that it is one of the few reviews of OMT for musculoskeletal problems that was not done by osteopaths. Therefore, it is worth showing you its abstract here:
The objective of this systematic review was to assess the effectiveness of osteopathy as a treatment option for musculoskeletal pain. Six databases were searched from their inception to August 2010. Only randomized clinical trials (RCTs) were considered if they tested osteopathic manipulation/mobilization against any control intervention or no therapy in human with any musculoskeletal pain in any anatomical location, and if they assessed pain as an outcome measure. The selection of studies, data extraction, and validation were performed independently by two reviewers. Studies of chiropractic manipulations were excluded. Sixteen RCTs met the inclusion criteria. Their methodological quality ranged between 1 and 4 on the Jadad scale (max = 5). Five RCTs suggested that osteopathy compared to various control interventions leads to a significantly stronger reduction of musculoskeletal pain. Eleven RCTs indicated that osteopathy compared to controls generates no change in musculoskeletal pain. Collectively, these data fail to produce compelling evidence for the effectiveness of osteopathy as a treatment of musculoskeletal pain.
It was published 11 years ago. But I have so far not seen compelling evidence that would make me change our conclusion. As I state in the newspapers:
OSTEOPATHY SHOULD BE TAKEN WITH A SIZABLE PINCH OF SALT.
The Anglo-European College of Chiropractic (AECC) has been promoting pediatric chiropractic for some time, and I have posted about the subject before (see, for instance, here). Now the AECC has gone one decisive step further. On the website, the AECC announced an MSc ‘Musculoskeletal Paediatric Health‘:
The MSc Musculoskeletal Paediatric Health degree is designed to develop your knowledge and skills in the safe and competent care of children of all ages. Our part-time, distance-based course blends live online classes with ready to use resources through our virtual learning environment. In addition, you will have the opportunity to observe in the AECC University College clinical services at our Bournemouth campus. The course covers topics in paediatric musculoskeletal practice with specific units on paediatric development, paediatric musculoskeletal examination, paediatric musculoskeletal interventions, and paediatric musculoskeletal management. You will address issues such as risk factors and public health, including breastfeeding, supine sleep in infancy, physical activity in children and conditions affecting the musculoskeletal health of children from birth. The paediatric specific topics are completed by other optional units such as professional development, evidence-based practice, and leadership and inter-professional collaboration. In the dissertation unit you will conduct a study relevant to musculoskeletal paediatric health.
Your learning will happen through a mix of live and recorded lectures, access to online reading materials, and access to the literature through our learning services. You will also engage with the contents taught through guided activities with your peers and staff. Clinical paediatric experience is recommended to fully engage with the course. For students with limited access to a suitable clinical environment to support their studies, or for student who wants to add to their clinical experience, we are able to offer a limited number of opportunities to observe and work alongside our clinical educators within the AECC University College clinical services. Assessments are tailor made to each unit and may include a variety of methods such as critical reviews, reflective accounts, portfolios and in the last year a research dissertation.
___________________________
The AECC emphasizes its commitment to being a leading higher education institution in healthcare disciplines, nationally and internationally recognised for quality and excellence. Therefore, it seems only fair to have another look at the science behind pediatric chiropractic. Specifically, is there any good science to show that would justify a Master of Science in ‘Musculoskeletal Paediatric Health’?
So, let’s have a look and see whether there are any good review articles supporting such a degree. Here is what I found with several Medline searches (date of the review on chiropractic for any pediatric conditions, followed by its conclusion + link [so that the reader can look up the evidence]):
2008
I am unable to find convincing evidence for any of the above-named conditions.
2009
Previous research has shown that professional chiropractic organisations ‘make claims for the clinical art of chiropractic that are not currently available scientific evidence…’. The claim to effectively treat otitis seems to
be one of them. It is time now, I think, that chiropractors either produce the evidence or abandon the claim.
2009
The … evidence is neither complete nor, in my view, “substantial.”
2010
2018
What seems to emerge is rather disappointing:
- There are no really new reviews.
- Most of the existing reviews are not on musculoskeletal conditions.
- All of the reviews cast considerable doubt on the notion that chiropractors should go anywhere near children.
But perhaps I was too ambitious. Perhaps there are some new rigorous clinical trials of chiropractic for musculoskeletal conditions. A few further searches found this (again year and conclusion):
2019
2018
I might have missed one or two trials because I only conducted rather ‘rough and ready’ searches, but even if I did: would this amount to convincing evidence? Would it be good science?
No! and No!
So, why does the AECC offer a Master of Science in ‘Musculoskeletal Paediatric Health’?
Search me!
…
…
It wouldn’t have something to do with the notion that it is good for business?
Or perhaps they just want to give science a bad name?
Anyone who has been following this blog will have noticed that we have our very own ‘resident chiro’ who comments every single time I post about spinal manipulation/chiropractic/back pain. He uses (mostly?) the pseudonym ‘DC’. Recently, DC explained why he is such an avid poster of comments:
” I read and occasionally comment on this blog for two main reasons. 1. In my opinion Ernst doesn’t do a balance reporting on the papers his shares regarding spinal manipulation and chiropractic. Thus, I offer additional insight, a more balanced perspective for the readers. 2. There are a couple of skeptics who occasionally post that do a good job of analyzing papers or topics and they do so in a respectful manner. I enjoy reading their comments. I will add a third. 3. Ernst, from what I can tell, doesn’t censor people just because they have a different view.”
So, DC aims at offering additional insights and a more balanced perspective. That would certainly be laudable and welcome. Yet, over the years, I have gained a somewhat different impression. Almost invariably, my posts on the named subjects cast doubt on the notion that chiropractic generates more good than harm. This, of course, cannot be to the liking of chiropractors, who therefore try to undermine me and my arguments. In a way, that is fair enough.
DC, however, seems to have long pursued a very specific and slightly different strategy. He systematically attempts to distract from the evidence and arguments I present. He does that by throwing in the odd red herring or by deviating from the subject in some other way. Thus he hopes, I assume, to distract from the point that chiropractic fails to generate more good than harm. In other words, DC is a tireless (and often tiresome) fighter for the chiropractic cause and reputation.
To check whether my impression is correct, I went through the last 10 blogs on spinal manipulation/ chiropractic/ back pain. Here are my findings (first the title of and link to the blog in question, followed by one of DC’s originals distractions)
No 1
Chiropractic: “a safe form of treatment”? (edzardernst.com)
“It appears conventional medicine has a greater number of AE. This is not surprising.”
correct!
real doctors treat really sick patients
So the probability of an AE increases based upon how sick a patient is? Is there research that supports that?
No 2
Malpractice Litigation Involving Chiropractic Spinal Manipulation (edzardernst.com)
It would be interesting to know more about these 38 cases that weren’t included since that’s almost half of the 86 cases. What percentage of those cases involved SMT by a non chiropractor?
“Query of the VerdictSearch online legal database for “chiropractor” OR “chiropractic” OR “spinal manipulation” within the 22,566 listed cases classified as “medical malpractice” yielded 86 cases. Of these, 48 cases met the inclusion criteria by featuring a chiropractic practitioner as the primary defendant.”
No 3
there are three basic types of disc herniation
contained herniation
non-contained herniation
sequestered herniation
Some add a forth which are:
disc protrusion
prolapsed disc
disc extrusion
sequestered disc
where the first two are considered incomplete (contained) and the last two are called complete (non-contained) but they are all classified as a disc herniation.
You’re welcome
No 4
Multidisciplinary versus chiropractic care for low back pain (edzardernst.com)
Elaborate on what you think was my mistake regarding clinical significance.
No 5
An evidence based approach has three legs. If you wish to focus on the research leg, what does the research reveal regarding maintenance care and LBP? Have you even looked into it?
No 6
Meditation for Chronic Low Back Pain Management? (edzardernst.com)
CRITERIA in assessing the credibility of subgroup analysis.
https://www.nature.com/articles/s41433-022-01948-0/tables/1
No 7
Acute Subdural Hemorrhage Following Cervical Chiropractic Manipulation (edzardernst.com)
sigh, my use of the word require was pointing out that different problems require different solutions.
You confuse a lack of concern with my critical analysis of what some use as evidence of serious harm.
I have only used one other identifier on this blog. Some objected to my use of the word Dr in that identifier so I changed it to DC as it wasn’t worth my time to argue with them (which of course DC still refers to Doctor but it seemed to appease them).
In healthcare and particularly in manual therapy we look at increasing comfort and function because most come to us because…wait for it…a loss of comfort and function.
Yes, there is the potential to cause harm, I have never said otherwise. Most case reports suggest that serious harm is due to an improper history and exam (although other reasons may exist such as improper technique). Thus, most cases appear to be preventable with a proper history, exam and technique. That, is a different problem that, yes, requires a different solution.
So yes, spinal manipulation isn’t “required” anymore than physical therapy, NSAIDs, etc for most cases. The question is: does the intervention increase comfort and function over doing nothing and is that justified due the potential risk of harm….benefit vs risk.
Now, i shall excuse my self to prepare for a research presentation that deals with a possible new contraindication to cSMT (because I have a lack of concern, right?)
No 8
Hmmm, let’s change that a bit…
The best approach is to consider the totality of the available evidence. By doing this, one cannot exclude the possibility that NSAIDs and opioids cause serious adverse effects. If that is so, we must abide by the precautionary principle which tells us to use other treatments that seem safer and at least as effective.
So based upon the totality of the available evidence, which is safer and at least as effective: cervical spinal manipulation vs NSAIDs/opioids?
No 9
Chiropractic spinal manipulation is not safe! (edzardernst.com)
getting the patient to sign something describing the risks. This is apparently something chiropractors don’t do before a neck manipulation.
Apparently?
No 10
Vertebral artery dissection in a pregnant woman after cervical spine manipulation (edzardernst.com)
Most case reports fail on one of two criteria, sometimes both.
1. No clear record of why the patient sought chiropractic care (symptoms that may indicate a VAD in progress or not)
2. Eliminating any other possible causes of the VAD especially in the week prior to SMT.
I would have to search but I recall a case report of a woman presenting for maintenance care (no head or neck symptoms at the time) and after cSMT was dx with a VAD. Asymptomatic VADs are very rare thus there is a high probability that cSMT induced the VAD in that case, IMO.
Although not published I had a dialogue with a MD where a patient underwent a MRI, had cSMT the next day and developed new symptoms thus another MRI was shortly done and was dx with a VAD. I encouraged her to publish the case but apparently she did not.
There was a paper published that looked at the quality of these case reports, most are poor.
__________________________________
I might be mistaken but DC systematically tries to distract from the fact that chiropractic does not generate more good than harm and that there is a continuous flow of evidence suggesting it does, in fact, the exact opposite. He (I presume he is male) might not even do this consciously in which case it would suggest to me that he is full of quasi-religious zeal and unable to think critically about his own profession and creeds.
Reviewing the material above, I also realized that, by engaging with DC (and other zealots of this type), it is I who often gives him the opportunity to play his game. Therefore, I will from now on try harder to stick to my own rules that say:
- Comments must be on-topic.
- I will not post comments which are overtly nonsensical.
- I will not normally enter into discussions with people who do not disclose their full identity.
Neck pain affects a vast number of people and leads to reduced quality of life and high costs. Clinically, it is a difficult condition to manage, and the effect sizes of the currently available treatments are moderate at best. Activity and manual therapy are first-line treatment options in several guidelines. But how effective are they really?
This study investigated the combination of home stretching exercises and spinal manipulative therapy in a multicentre randomized controlled clinical trial, carried out in a multidiscipline range of primary care clinics.
The treatment modalities utilized were spinal manipulative therapy combined with home stretching exercises compared to home stretching exercises alone. Both groups received 4 treatments for 2 weeks. The primary outcome was pain, where the subjective pain experience was investigated by assessing pain intensity (NRS – 11) and the quality of pain (McGill Pain Questionnaire). Neck disability and health status were secondary outcomes, measured using the Neck Disability Indexthe EQ-5D, respectively.
One hundred thirty-one adult subjects were randomized to one of the two treatment groups. All subjects had experienced persistent or recurrent neck pain the previous 6 months and were blinded to the other group intervention. The clinicians provided treatment for subjects in both groups and could not be blinded. The researchers collecting data were blinded to treatment allocation, as was the statistician performing data analyses. An intention-to-treat analysis was used.
Sixty-six subjects were randomized to the intervention group, and 65 to the control group. For NRS – 11, a B-coefficient of – 0,01 was seen, indication a 0,01 improvement for the intervention group in relation to the control group at each time point with a p-value of 0,305. There were no statistically significant differences between groups for any of the outcome measures.
Four intense adverse events were reported in the study, three in the intervention group, and one in the control group. More adverse incidents were reported in the intervention group, with a mean pain intensity (NRS-11) of 2,75 compared to 1,22 in the control group. There were no statistically significant differences between the two groups.
The authors concluded that there is no additional treatment effect from adding spinal manipulative therapy to neck stretching exercises over 2 weeks for patients with persistent or recurrent neck pain.
This is a rigorous and well-reported study. It suggests that adjuvant manipulations are not just ineffective for neck pain, but also cause some adverse effects. This seems to confirm many previously discussed investigations concluding that chiropractors do not generate more good than harm for patients suffering from neck pain.
Static or motion manual palpation tests of the spine are commonly used by chiropractors and osteopaths to assess pain location and reproduction in low back pain (LBP) patients. But how reliable are they?
The purpose of this review was to evaluate the reliability and validity of manual palpation used for the assessment of LBP in adults. The authors systematically searched five databases from 2000 to 2019 and critically appraised the internal validity of studies using QAREL and QUADAS-2 instruments.
A total of 2023 eligible articles were identified, of which 14 were at low risk of bias. Evidence suggests that reliability of soft tissue structures palpation is inconsistent, and reliability of bony structures and joint mobility palpation is poor. Preliminary evidence was found to suggest that gluteal muscle palpation for tenderness may be valid in differentiating LBP patients with and without radiculopathy.
The authors concluded that the reliability of manual palpation tests in the assessment of LBP patients varies greatly. This is problematic because these tests are commonly used by manual therapists and clinicians. Little is known about the validity of these tests; therefore, their clinical utility is uncertain. High quality validity studies are needed to inform the clinical use of manual palpation tests.
I have repeatedly drawn attention to the fact that the diagnostic methods used by chiropractors and osteopaths are of uncertain or disproven validity (see for instance here, or here). Why is that important?
Imagine you consult a chiropractor or osteopath. Simply put, this is what is likely to happen:
- They listen to your complaint.
- They do a few tests which are of dubious validity.
- They give you a diagnosis that is meaningless.
- They treat you with manual therapies that are neither effective nor safe.
- You pay.
- They persuade you that you need many more sessions.
- You pay regularly.
- When eventually your pain has gone away, they persuade you to have useless maintenance treatment.
- You pay regularly.
In a nutshell, they have very little to offer … which explains why they attack everyone who dares to disclose this.