medical ethics
Germany seems to have a significant problem with anti-vaxxers. Today, only 68% of the population has had a COVID vaccination. In the UK and France, these figures are 72% and 75% respectively.
How come?
This study investigated the willingness to vaccinate of parents of minors and people without children who are minors. The investigation was based on a random sample of Germans (telephone survey, n = 2,014, collected between 12 November and 10 December 2020). The evaluation is primarily based on the sub-sample of people with minors in the household (n = 461).
Parents of minors consistently show a lower willingness to be vaccinated with a COVID-19 vaccine than respondents without minors (54.1% vs 71.1%). Fathers show a stronger willingness to be vaccinated than mothers. Furthermore, men are more willing to get their own child vaccinated with a COVID-19 vaccine than are women.
The authors concluded that among parents and especially mothers, a considerable misrepresentation of vaccination risks and frequent beliefs in vaccination conspiracy theories can be observed. Clear and easily understandable information on the effects and side effects of vaccination with a COVID-19 vaccine by relevant institutions and physicians is recommended.
And what has this to do with so-called alternative medicine (SCAM) and homeopathy?
In the results section of the paper, the authors report interesting additional findings (my translation):
In the total sample, a significantly higher willingness to vaccinate is associated with the rejection of “alternative healing methods”. There is also a significant correlation between the attitude towards homeopathy and one’s own willingness to vaccinate: if homeopathy is supported, the willingness to vaccinate is lower. This correlation between the attitude towards homeopathy and willingness to vaccinate is also evident in the sub-sample of parents. Among parents, it is again women who significantly more often have a positive attitude towards homeopathy than men, who more often do not think anything of it.
The authors also report that the parents were asked: “If a vaccine against the coronavirus is approved in Germany, would you get vaccinated?” CERTAINLY NOT was the answer of:
- 41% of homeopathy fans
- 10% of people who thought nothing at all about homeopathy
- 15% of participants who were not fully convinced by homeopathy
Yes, Germany seems to have a problem with the anti-vaccination brigade but it seems that at the heart of it is a problem with a homeopathy cult.
This article from AP News caught my attention. Here it is (I haven’t changed a word):
The flashy postcard, covered with images of syringes, beckoned people to attend Vax-Con ’21 to learn “the uncensored truth” about COVID-19 vaccines.
Participants traveled from around the country to a Wisconsin Dells resort for a sold-out convention that was, in fact, a sea of misinformation and conspiracy theories about vaccines and the pandemic. The featured speaker was the anti-vaccine activist who appeared in the 2020 movie “Plandemic,” which pushed false COVID-19 stories into the mainstream. One session after another discussed bogus claims about the health dangers of mask wearing and vaccines.
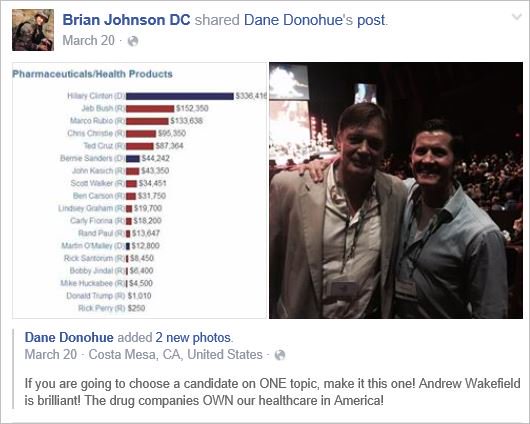
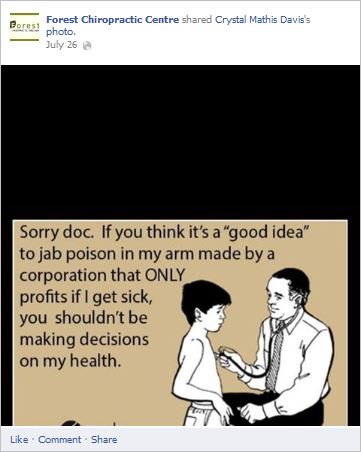
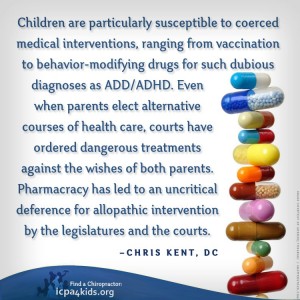
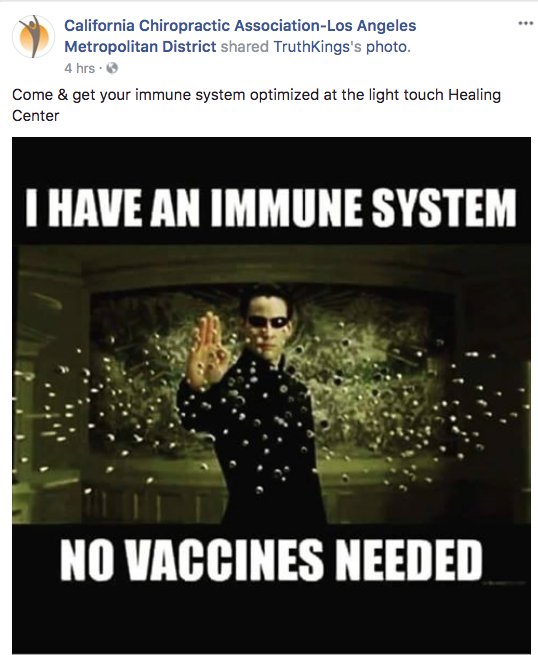
The convention was organized by members of a profession that has become a major purveyor of vaccine misinformation during the pandemic: chiropractors.
At a time when the surgeon general says misinformation has become an urgent threat to public health, an investigation by The Associated Press found a vocal and influential group of chiropractors has been capitalizing on the pandemic by sowing fear and mistrust of vaccines.
They have touted their supplements as alternatives to vaccines, written doctor’s notes to allow patients to get out of mask and immunization mandates, donated large sums of money to anti-vaccine organizations and sold anti-vaccine ads on Facebook and Instagram, the AP discovered. One chiropractor gave thousands of dollars to a Super PAC that hosted an anti-vaccine, pro-Donald Trump rally near the U.S. Capitol on Jan. 6.
They have also been the leading force behind anti-vaccine events like the one in Wisconsin, where hundreds of chiropractors from across the U.S. shelled out $299 or more to attend. The AP found chiropractors were allowed to earn continuing education credits to maintain their licenses in at least 10 states.
On this blog, I have often discussed that chiropractors tend to be anti-vax. It all goes back to their founding father, DD Palmer, who famously wrote:
- Vaccination and inoculation are pathological; chiropractic is physiological,
- and who in 1894, published his views on smallpox vaccination: ‘…the monstrous delusion … fastened on us by the medical profession, enforced by the state boards, and supported by the mass of unthinking people …’
- and who stated in 1896 that keeping tissue healthy is therefore the best prevention against infections; and this is best achieved by magnetic healing.
But that’s long ago! We are not like that anymore! … say the chiros of today.
Do you believe them?
If so, you might want to read this article by Jann Bellamy. Or alternatively, just look at some of my finds from the Internet:
The purpose of this survey was to quantify and describe the clinical practice beliefs and behaviors associated with US chiropractors. A 10% random sample of US chiropractors (n = 8975) was selected from all 50 state regulatory board lists and invited to participate in a survey. The survey consisted of a 7-item questionnaire; 6 items were associated with chiropractic ideological and practice characteristics and 1 item was related to the self-identified role of chiropractic in the healthcare system which was utilized as the dependent variable to identify chiropractic subgroups. Multinomial logistic regression with predictive margins was used to analyze which responses to the 6 ideology and practice characteristic items were predictive of chiropractic subgroups.
The survey instrument used in this study was developed by the authors and modeled after similar chiropractic identity analyses. The survey instrument included a total of 7 items intended to elicit divergent ideologies and practice behaviors. The figure below is a copy of the survey instrument.
A total of 3538 responses were collected (39.4% response rate). Respondents self-identified into three distinct subgroups based on the perceived role of the chiropractic profession in the greater healthcare system:
- 57% were spine/neuromusculoskeletal focused;
- 22% were primary care focused;
- 21% were vertebral subluxation focused.
Patterns of responses to the 6 ideologies and practice characteristic items were substantially different across the three professional subgroups.
The authors concluded that respondents self-identified into one of three distinct intra-professional subgroups. These subgroups can be differentiated along themes related to clinical practice beliefs and behaviors.
Here are the results in more detail as sated by the authors:
Regarding scope of examination (survey question 1), respondents reporting the scope of their clinical examination to only include spinal analysis for the assessment of vertebral subluxation had a 70% probability of belonging to the subluxation focused subgroup, a 20% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup. Conversely, respondents who reported the scope of their clinical examination only includes a differential diagnosis had a 0% probability of belonging to the vertebral subluxation focused subgroup, an 80% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 20% probability of belonging to the primary care focused subgroup.
Concerning conditions treated (survey question 2), respondents who reported predominantly treating vertebral subluxation as an encumbrance to health had an 80% probability of belonging to the vertebral subluxation focused subgroup, a 10% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup. In contrast, respondents reporting predominantly treating neuromusculoskeletal conditions had a 0% probability of belonging to the vertebral subluxation focused subgroup, a 90% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup.
Regarding the role of spinal manipulation for those with cancer (survey question 4), respondents reporting the role of spinal manipulation for those with cancer is to remove interference to innate intelligence had a 70% probability of belonging to the vertebral subluxation focused subgroup, a 20% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup. Respondents reporting there is no role of spinal manipulation in those with cancer also had a 10% probability of belonging to the subluxation focused subgroup, an 80% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup.
Regarding vaccination (survey question 5), respondents who strongly disagreed that vaccinations have had a positive effect on global public health had a 50% probability of belonging to the vertebral subluxation focused subgroup, an approximately 25% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and an approximately 25% probability of belonging to the primary care focused subgroup. In contrast, respondents who strongly agreed that vaccinations have had a positive effect on global public health had a 0% probability of belonging to the vertebral subluxation focused subgroup, a 90% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 10% probability of belonging to the primary care focused subgroup.
Concerning the detection of vertebral subluxation on x-ray (survey question 6), respondents who strongly agreed that x-ray is helpful in detecting vertebral subluxations had a 40% probability of belonging to the vertebral subluxation focused subgroup, a 40% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 20% probability of belonging to the primary care focused subgroup. Respondents who strongly disagreed that x-ray is helpful in detecting vertebral subluxations had a near 0% probability of belonging to the vertebral subluxation focused subgroup, an 80% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and slightly below a 20% probability of belonging to the primary care focused subgroup.
Regarding use of x-rays for new patients (survey question 7), respondents who reported prescribing x-rays for 0–20% of new patients had a 20% probability of belonging to the vertebral subluxation focused subgroup, a 60% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 20% probability of belonging to the primary care focused subgroup. Respondents reporting prescribing x-rays for 81–100% of new patients had a 40% probability of belonging to the vertebral subluxation focused subgroup, a 40% probability of belonging to the spine and neuromusculoskeletal focused subgroup, and a 20% probability of belonging to the primary care focused subgroup.
END OF QUOTE
While I am not sure that the division into the 3 subgroups is valid and suspect that there must be a substantial overlap between them, I must admit that the paper is rich in fascinating information. Generally speaking, I find all subgroups somewhat mysterious and would ask them the following questions:
Subgroup 1: why did you not study medicine or physiotherapy?
Subgroup 2: does it not bother you that your education and training are woefully insufficient for primary care?
Subgroup 3: is it not time to abandon the obsolete nonsense of your guru, the old charlatan DD Palmer?
Practitioners of so-called alternative medicine (SCAM) regularly claim with great pride that they treat the ROOT CAUSES of disease. The claim has at least 4 effects:
- It distracts from the true causes of disease which are often multifactorial.
- It attracts customers to SCAM.
- It implies that conventional medicine is at best symptomatic and thus far inferior to SCAM.
- It encourages the patients of SCAM practitioners to turn their backs on mainstream healthcare.
The notion that SCAM practitioners treat the root causes is based on the practitioners’ understanding of etiology:
- If a traditional acupuncturist, for instance, becomes convinced that all disease is the expression of an imbalance of life-forces, and that needling acupuncture points will re-balance these forces thus restoring health, he must automatically assume that he is treating the root causes of any condition.
- If a chiropractor believes that all diseases are due to ‘subluxations’ of the spine, it must seem logical to him that spinal ‘adjustment’ is synonymous with treating the root cause of whatever complaint his patient is suffering from.
- If a Bowen therapist is convinced that “the Bowen Technique aims to balance the whole person, not just the symptoms“, he is bound to be equally sure that the root cause of “practically any problem can potentially be addressed” by this intervention.
- If a homeopath is convinced that all illness stems from a weakness of the ‘vital force’ and that only homeopathic remedies can revitalize it, they are likely to believe that their remedies tackle the root cause of all diseases.
- Etc., etc.
So, are SCAM practitioners correct when they claim to treat the root causes of disease?
When a root cause has been eliminated, the disease has been eliminated by its root. Treating a root cause, therefore, means that the disease is permanently cured. The above question can therefore be re-phrased as follows:
Is there any SCAM that cures any disease permanently?
I think the answer is NO. (At least, I know none. I would, however, be most grateful if someone could name one together with the evidence)
Even demonstrably effective forms of SCAM are effective only in terms of alleviating the symptoms. The one with the best evidence is probably St John’s wort. It works fine for mild to moderate depression. Yet, it does not cure depression: if we discontinue the treatment, the depression is likely to return.
And what about conventional medicine? Does it offer any permanent cures?
I have been searching and have to admit that I cannot find many either. Here is my list so far of diseases that are potentially curable (meaning they are unlikely to come back once the treatment has stopped and excluding disease prevention) with conventional medicine – and again, I would be really grateful if readers could add to my preliminary list:
- Acute emergencies, like anaphylaxis, cardiac arrest, etc.
- Bacterial infections (well most of them)
- Cancer (some), like Hodgkin lymphoma
- Malnutrition like beriberi of iron-deficiency anemia
- Phobias (some)
- Fungal infections (some)
- Poisonings (some)
- Many surgical indications such as appendicitis, gall stones, carpal tunnel syndrome, etc.
Not a long list, I admit (but better than nothing!) – so, please help me to prolong it by adding diseases that I did not mention.
THANKS
Kratom (Mitragyna speciosa, Korth.) is an evergreen tree that is indigenous to Southeast Asia. It is increasingly being used as a recreational drug, to help with opium withdrawal, and as a so-called alternative medicine (SCAM) for pain, erectile dysfunction, as a mood stabilizer, and for boosting energy or concentration. When ingested, Kratom leaves produce stimulant and opioid-like effects (see also my previous post).
Kratom contains 7‑hydroxymitragynine, which is active on opioid receptors. The use of kratom carries significant risks, e.g. because there is no standardized form of administration as well as the possibility of direct damage to health and of addiction.
There are only very few clinical trials of Kratom. One small placebo-controlled study concluded that the short-term administration of the herb led to a substantial and statistically significant increase in pain tolerance. And a recent review stated that Kratom may have drug interactions as both a cytochrome P-450 system substrate and inhibitor. Kratom does not appear in normal drug screens and, especially when ingested with other substances of abuse, may not be recognized as an agent of harm. There are numerous cases of death in kratom users, but many involved polypharmaceutical ingestions. There are assessments where people have been unable to stop using kratom therapy and withdrawal signs/symptoms occurred in patients or their newborn babies after kratom cessation. Both banning and failure to ban kratom places people at risk; a middle-ground alternative, placing it behind the pharmacy counter, might be useful.
In Thailand, Kratom had been outlawed since 1943 but now it has become (semi-)legal. Earlier this year, the Thai government removed the herb from the list of Category V narcotics. Following this move, some 12,000 inmates who had been convicted when Kratom was still an illegal drug received amnesty. However, Kratom producers, traders, and even researchers will still require licenses to handle the plant. Similarly, patients looking for kratom-based supplements will need a valid prescription from licensed medical practitioners. Thai law still prohibits bulk possession of Kratom. Users are encouraged to handle only minimum amounts of the herb to avoid getting prosecuted for illegal possession.
In 2018, the US Food and Drug Administration stated that Kratom possesses the properties of an opioid, thus escalating the government’s effort to slow usage of this alternative pain reliever. The FDA also wrote that the number of deaths associated with Kratom use has increased to a total of 44, up from a total of 36 since the FDA’s November 2017 report. In the majority of deaths that the FDA attributes to Kratom, subjects ingested multiple substances with known risks, including alcohol.
In most European countries, Kratom continues to be a controlled drug. In the UK the sale, import, and export of Kratom are prohibited. Yet, judging from a quick look, it does not seem to be all that difficult to obtain Kratom via the Internet.
The global market for dietary supplements has grown continuously during the past years. In 2019, it amounted to around US$ 353 billion. The pandemic led to a further significant boost in sales. Evidently, many consumers listened to the sly promotion by the supplement industry. Thus they began to be convinced that supplements might stimulate their immune system and thus protect them against COVID-19 infections.
During the pre-pandemic years, the US sales figures had typically increased by about 5% year on year. In 2020, the increase amounted to a staggering 44 % (US$435 million) during the six weeks preceding April 5th, 2020 relative to the same period in 2019. The demand for multivitamins in the US reached a peak in March 2020 when sales figures had risen by 51.2 %. Total sales of vitamins and other supplements amounted to almost 120 million units for that period alone. In the UK, vitamin sales increased by 63 % and, in France, sales grew by around 40–60 % in March 2020 compared to the same period of the previous year.
Vis a vis such impressive sales figures, one should ask whether dietary supplements really do produce the benefit that consumers hope for. More precisely, is there any sound evidence that these supplements protect us from getting infected by COVID-19? In an attempt to answer this question, I conducted several Medline searches. Here are the conclusions of the relevant clinical trials and systematic reviews that I thus found:
- KSK (a polyherbal formulation from India’s Siddha system of medicine) significantly reduced SARS-CoV-2 viral load among asymptomatic COVID-19 cases and did not record any adverse effect, indicating the use of KSK in the strategy against COVID-19. Larger, multi-centric trials can strengthen the current findings.
- There is currently insufficient evidence to determine the benefits and harms of vitamin D supplementation as a treatment of COVID-19.
- Herbal supplements may help patients with COVID-19, zinc sulfate is likely to shorten the duration of olfactory dysfunction. DS therapy and herbal medicine appear to be safe and effective adjuvant therapies for patients with COVID-19. These results must be interpreted with caution due to the overall low quality of the included trials. More well-designed RCTs are needed in the future.
- No significant difference with vitamin-D supplementation on major health related outcomes in COVID-19.
- there is not enough evidence on the association between individual zinc status and COVID-19 infections and mortality.
- Omega-3 supplementation improved the levels of several parameters of respiratory and renal function in critically ill patients with COVID-19.
- A 5000 IU daily oral vitamin D3 supplementation for 2 weeks reduces the time to recovery for cough and gustatory sensory loss among patients with sub-optimal vitamin D status and mild to moderate COVID-19 symptoms. The use of 5000 IU vitamin D3 as an adjuvant therapy for COVID-19 patients with suboptimal vitamin D status, even for a short duration, is recommended.
- In this 2-sample MR study, we did not observe evidence to support an association between 25OHD levels and COVID-19 susceptibility, severity, or hospitalization. Hence, vitamin D supplementation as a means of protecting against worsened COVID-19 outcomes is not supported by genetic evidence.
- These antiviral and immune-modulating activities and their ability to stimulate interferon production recommend the use of probiotics as an adjunctive therapy to prevent COVID-19. Based on this extensive review of RCTs we suggest that probiotics are a rational complementary treatment for RTI diseases and a viable option to support faster recovery.
- In this randomized clinical trial of ambulatory patients diagnosed with SARS-CoV-2 infection, treatment with high-dose zinc gluconate, ascorbic acid, or a combination of the 2 supplements did not significantly decrease the duration of symptoms compared with standard of care.
- These findings neither support nor refute the claim that 3M3F alters the severity of COVID-19 or alleviates symptoms. More rigorous studies are required to properly ascertain the potential role of Chinese Herbal Medicine in COVID-19.
- NSO (Nigella sativa oil) supplementation was associated with faster recovery of symptoms than usual care alone for patients with mild COVID-19 infection. These potential therapeutic benefits require further exploration with placebo-controlled, double-blinded studies.
- The clinical application of LQ (Lianhua Qingwen Granules or Capsules ) on the treatment of COVID-19 has significant efficacy in improving clinical symptoms and reducing the rate of clinical change to severe or critical condition. Nevertheless, due to the limited quantity and quality of the included studies, more and higher quality trials with more observational indicators are expected to be published.
- The study identified some important potential traditional Indian medicinal herbs such as Ocimum tenuiflorum, Tinospora cordifolia, Achyranthes bidentata, Cinnamomum cassia, Cydonia oblonga, Embelin ribes, Justicia adhatoda, Momordica charantia, Withania somnifera, Zingiber officinale, Camphor, and Kabusura kudineer, which could be used in therapeutic strategies against SARS-CoV-2 infection.
- Shenhuang Granule is a promising integrative therapy for severe and critical COVID-19.
- Low-certainty or very low-certainty evidence demonstrated that oral CPM (Chinese patent medicine) may have add-on potential therapeutic effects for patients with non-serious COVID-19. These findings need to be further confirmed by well-designed clinical trials with adequate sample sizes.
- XYP (Xiyanping) injection is safe and effective in improving the recovery of patients with mild to moderate COVID-19. However, further studies are warranted to evaluate the efficacy of XYP in an expanded cohort comprising COVID-19 patients at different disease stages.
- Our meta-analysis of RCTs indicated that LH (Lianhuaqingwen) in combination with usual treatment may improve the clinical efficacy in patients with mild or moderate COVID-19 without increasing adverse events. However, given the limitations and poor quality of included trials in this study, further large-sample RCTs or high-quality real-world studies are needed to confirm our conclusions.
- Reduning injection might be effective and safe in patients with symptomatic COVID-19.
- In light of the safety and effectiveness profiles, LH (Lianhuaqingwen) capsules could be considered to ameliorate clinical symptoms of Covid-19.
- QPT (Qingfei Paidu Tang) was associated with a substantially lower risk of in-hospital mortality, without extra risk of acute liver injury or acute kidney injury among patients hospitalized with COVID-19.
- This community-based RCT found that the use of a herbal medicine therapy (Jinhaoartemisia antipyretic granules and Huoxiangzhengqi oral liquids) could significantly reduce the risks of the common cold among community-dwelling residents, suggesting that herbal medicine may be a useful approach for public health intervention to minimize preventable morbidity during COVID-19 outbreak.
- Based on unresolved controversies and inconclusive findings, it could be said that generally, a single and specific therapeutics to COVID-19 is still a mirage.
- Keguan-1-based integrative therapy was safe and superior to the standard therapy in suppressing the development of ARDS in COVID-19 patients.
Confused?
Me too!
Does the evidence justify the boom in sales of dietary supplements?
More specifically, is there good evidence that the products the US supplement industry is selling protect us against COVID-19 infections?
No, I don’t think so.
So, what precisely is behind the recent sales boom?
It surely is the claim that supplements protect us from Covid-19 which is being promoted in many different ways by the industry. In other words, we are being taken for a (very expensive) ride.
Exploring preventive therapeutic measures has been among the biggest challenges during the coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). A team of Indian and US researchers explored the feasibility and methods of recruitment, retention, and potential signal of efficacy, of selected homeopathic medicines as a preventive measure for developing COVID-19 in a multi-group study.
A six-group, randomized, double-blind, placebo-controlled prophylaxis study was conducted in a COVID-19 exposed population in a quarantine facility in Mumbai, India. Each group received one of the following:
- Arsenicum album 30c,
- Bryonia alba 30c,
- Arsenicum album 30c, Bryonia alba 30c, Gelsemium sempervirens 30c, and Influenzinum 30c
- coronavirus nosode CVN01 30c,
- Camphora 1M,
- placebo.
Six pills twice a day were administered for 3 days. The primary outcome measure used was testing recruitment and retention in this quarantined setting. Secondary outcomes were numbers testing positive for COVID-19 after developing symptoms of illness, the number of subjects hospitalized, and days to recovery.
Good rates of recruitment and retention were achieved. Of 4,497 quarantined individuals, 2,343 sought enrollment, with 2,294 enrolled and 2,233 completing the trial (49.7% recruitment, 97.3% retention). Subjects who were randomized to either Bryonia alba (group 2) or to the CVN01 nosode (group 4) signaled a numerically lower incidence of laboratory-confirmed COVID-19 and a shorter period of illness, with evidence of fewer hospitalizations than those taking placebo. The three other groups did not show signals of efficacy.
The authors concluded that this pilot study supports the feasibility of a larger randomized, double-blind, placebo-controlled trial. Bryonia alba 30c and CVN01 30c should both be explored in disease prevention or shortening the course of disease symptomatology in a COVID-19-exposed population.
Signals of efficacy?
Are they kidding us?
The results failed to be statistically significant!
Hence the conclusions should be rewritten as follows:
This pilot study supports the feasibility of a larger trial in India where people have been told by an irresponsible government to believe in homeopathy. None of the 5 homeopathic treatments generated encouraging findings and none should be explored further. Studies of this nature must be discouraged firstly because homeopaths would not accept the findings of a trial of non-individualized homeopathy, and secondly because such trials will further confuse the public who might think that homeopathy is worth trying.
So-called alternative medicine (SCAM) use has been increasingly prevalent among Americans, whereas its relationship with medical non-adherence is unknown. Using the National Health Interview Survey, this analysis evaluated the use of SCAM modalities and their association with cost-related nonadherence to medical care (CRN) among older Americans by gender strata.
Americans, aged 50 or above in the 2012 National Health Interview Survey, were included to evaluate the use of SCAM modalities and their association with CRN. SCAM modalities were categorized as the use of the following in the past 12 months:
- 1) herbal supplements;
- 2) chiropractic or osteopathic manipulations;
- 3) massage;
- 4) Yoga, tai chi, or qigong;
- 5) Mantra/mindfulness/spiritual meditation,
- 6) acupuncture;
- 7) mind-body therapy;
- 8) other SCAM modalities including homeopathy, naturopathy, traditional healers, energy healing therapy, biofeedback, hypnosis, and craniosacral therapy.
CRN was defined as needing medical care but not receiving it due to costs and/or having medical care delayed due to costs in the past 12 months. The investigators developed a multivariable logit model to assess the association of the use of SCAM modalities and CRN controlling for patients age, gender, race, ethnicity, insurance status (Medicare, Medicaid, VA/Tri-care, no-insurance, or private insurance), and comorbid conditions (diabetes, arthritis, back and neck problems, heart condition, stroke, lung and breathing problems, and cancer).
A total of 16,360 older Americans were included in the analysis, with 11,278 (68.9%) reporting at least one SCAM modality use, and 1,992 (12.2%) of them reported CRN. Among the 8 SCAM modalities, compared to those not using SCAM, those who used chiropractic were 94% more likely (p=0.01), those who used Mantra/mindfulness/spiritual meditation were 106% more likely (p<0.01), and those using other modalities were 42% more likely (p=0.07) to report CRN. In contrast, those who used mind-body therapy were 43% less likely (p=0.04) to report CRN. The other 4 modalities did not achieve statistically significant levels although the odds ratios were mostly greater than 1.
The authors argue that the differential association between the SCAM modality use and CRN suggested a complex relationship between the utilization of SCAM and patients’ non-adherence to medical care. It is possible that the out-of-pocket payments for those services significantly increased patients’ cost burden and thus made the use of other medical care unaffordable, and it’s also possible that those who already had low resources were more likely to seek SCAM to substitute for more expensive conventional care. Either of these scenarios would present a serious challenge.
The authors concluded that both men and women are more likely to report financial distress while using various SCAM modalities.
These findings are not easy to interpret. To me, they suggest that, in the US, many consumers have been persuaded to prioritize SCAM over conventional medicine, even if they can ill afford it. It throws a dim light on the US society where some folks seem to struggle to pay for what is essential while continuing to afford the superfluous.
In my view, in a just and non-decadent society, conventional healthcare must be free for everyone at the point of delivery, and SCAM is at best an extra that those who want it should pay out of their own pocket.
This comment came recently from our good friend Dana Ullman, and it made me think again about homeopathy and the ‘first do no harm’ principle.
- The first thing to note is that the Hippocratic oath does not contain this sentence.
- And the second thing to stress is that clinicians are doing harm regularly. The ‘first do no harm’ principle has long been understood to mean that clinicians should always take care that their actions generate more benefit than harm.
As we discussed all this in more detail before, I do not intend to dwell on it. Today, I rather consider three exemplary scenarios in order to investigate how the principle of doing more good than harm applies to homeopathy (or indeed any other form of so-called alternative medicine (SCAM)).
SCENARIO 1:
PATIENT WITH A SELF-LIMITING CONDITION
Let’s assume our patient has a cold and consults her physician who prescribes a homeopathic remedy. One could argue that no harm is done in such a situation. The treatment will not help beyond a placebo effect, but the cold will disappear in just a few days, and the patient will not suffer any side effects. This attitude is common but it disregards the following potential harms:
- The cost for the treatment.
- The possibility that our patient suffered for several days needlessly from cold symptoms that might be treatable.
- The possibility of our patient getting the erroneous impression that homeopathy is an effective therapy (because the cold did go away quickly) and therefore opts to use it for future, more serious illnesses.
What if the physician only prescribed homeopathy because the patient asked him to do so? Strictly speaking, the above-named issues still apply in this situation. The ethical thing would have been to inform the patient what the best evidence tells us (namely that homeopathy is a placebo therapy), provide assurance about the nature of the condition, and prescribe effective treatments as needed.
And what if the physician does all of these things and, in addition, prescribes homeopathy because the patient wants it? In this case, the possibility of harms 1 and 3 does still apply.
SCENARIO 2
PATIENT WITH A CHRONIC CONDITION
Consider a patient suffering from arthritis who consults her physician who prescribes homeopathic remedies as the sole therapy. In such a situation, the following harms apply:
- The cost for the treatment.
- The possibility that our patient suffers needlessly from symptoms that are treatable. As the symptoms can be serious, this would often amount to medical negligence.
What if the physician only prescribed homeopathy because the patient asked him to do so and the patient refuses conventional therapies? In such cases, it is the physician’s ethical duty to inform the patient about the best evidence as it pertains to homeopathy and conventional treatments for her condition. Failure to do so would amount to negligence. The patient is then free to decide, of course. But so is the physician; nobody can force him/her to prescribe ineffective treatments. If no consensus can be reached, the patient might have to change physician.
And what if the physician does inform the patient adequately but also prescribes homeopathy because the patient wants it? In this case, the possibility of harms 1 and 3 does still apply.
SCENARIO 3
PATIENT WITH A LIFE-THREATENING CONDITION
Consider a young man with testicular cancer who consults his doctor who prescribes homeopathic remedies as the sole therapy. In such a situation, the physician is grossly negligent and could be struck off because of negligence.
What if the physician prescribed homeopathy because the patient asked him to do so and refuses conventional therapies? In such a case, it is the ethical duty of the physician to inform the patient about the best evidence as it pertains to homeopathy and to the conventional treatment for his cancer. Failure to do so would amount to negligence. The patient is then free to decide, of course. But so is the physician; nobody can force him to prescribe ineffective treatments. If no consensus can be reached between the physician and the patient, the patient might have to change physician.
And what if the physician does inform the patient adequately makes sure he receives effective oncological treatments, but also prescribes homeopathy because the patient insists on it? In this case, the possibility of harms 1 and 3 does still apply.
These scenarios are, of course, rather schematic and, in everyday practice, many other factors might need considering. They nevertheless show that the ‘do more good than harm’ principle does not support homeopathy (or any other ineffective SCAM). In other words, the practice of homeopathy is not ethical.
But what if someone (like Dana Ullman) strongly believes in the effectiveness of homeopathy? In this case, he or she is not acting according to the best available evidence – and that, of course, is also unethical.
I have repeatedly likened so-called alternative medicine (SCAM) to a cult – not a religious cult, of course, but to a ‘health cult’. A health cult is defined as a system for the cure of disease based on dogma set forth by its promulgator. So, are you a member of a health cult?
In case you are a proponent of SCAM, you might be in danger. Here are a few questions you should ask yourself:
- Is your SCAM based on dogma, such as ‘LIKE CURES LIKE’ or ‘SUBLUXATIONS ARE THE CAUSE OF DISEASE?
- Does the cult demand you accept its dogma or doctrine as truth?
- Is it set forth by a single guru or promulgator?
- Is your SCAM supposed to cure all ills?
- Is belief used by proponents of your SCAM as a substitute for evidence?
- Does the SCAM determine your diet and/or lifestyle?
- Does the SCAM exploit you financially?
- Does your SCAM impose rigid rules and regulations?
- Does your SCAM practice deception?
- Does your SCAM have its own sources of information/propaganda?
- Does your SCAM cultivate its own lingo?
- Does your SCAM discourage or inhibit critical thinking?
- Are questions about the values of your SCAM discouraged or forbidden?
- Do the proponents of your SCAM reduce complexities into platitudinous buzz words?
- Do they assume that health problems are the result of not adhering to the dogma?
- Does your SCAM instill fear into members who consider leaving?
- Do the proponents of your SCAM depict conventional medicine as ineffective or harmful?
- Are you asked to recruit new members to your SCAM?
Please try to answer these questions honestly and self-critically.
If more than a handful turn out to be positive, you have, in my view, a reason to be concerned. In this case, I would recommend you go to a library and start reading a few books that provide critical analyses of SCAM.