malpractice
This systematic review was aimed at determining if there has been a change in the reporting of adverse events associated with spinal manipulation in randomized clinical trials (RCTs) since 2016.
Databases were searched from March 2016 to May 2022: MEDLINE (Ovid), Embase, CINAHL, ICL, PEDro, and Cochrane Library. The following search terms and their derivatives were adapted for each platform: spinal manipulation; chiropractic; osteopathy; physiotherapy; naprapathy; medical manipulation and clinical trial.
Domains of interest (pertaining to adverse events) included: completeness and location of reporting; nomenclature and description; spinal location and practitioner delivering manipulation; methodological quality of the studies and details of the publishing journal. Frequencies and proportions of studies reporting on each of these domains were calculated. Univariable and multivariable logistic regression models were fitted to examine the effect of potential predictors on the likelihood of studies reporting on adverse events.
There were 5399 records identified by the electronic searches, of which 154 (2.9%) were included in the analysis. Of these, 94 (61.0%) reported adverse events with only 23.4% providing an explicit description of what constituted an adverse event. Reporting of adverse events in the abstract had increased (n=29, 30.9%) while reporting in the results section had decreased (n=83, 88.3%) over the past 6 years. Spinal manipulation was delivered to 7518 participants in the included studies. No serious adverse events were reported in any of these studies.
The authors concluded that, while the current level of reporting of adverse events associated with spinal manipulation in RCTs has increased since our 2016 publication on the same topic, the level remains low and inconsistent with established standards. As such, it is imperative for authors, journal editors and administrators of clinical trial registries to ensure there is more balanced reporting of both benefits and harms in RCTs involving spinal manipulation.
In fact, it is an ethical imperative to accurately report adverse effects. Not reporting adverse effects amounts to a violation of medical research ethics. Adverse effects of spinal manipulation occur in about 50% of all patients. This means that investigators reporting significantly lower figures are likely guilty of under-reporting. And under-reporting of adverse events is also a breach of ethical standards.
My conclusion thus is that the vast majority of trials of spinal manipulation are unethical and should be discarded.
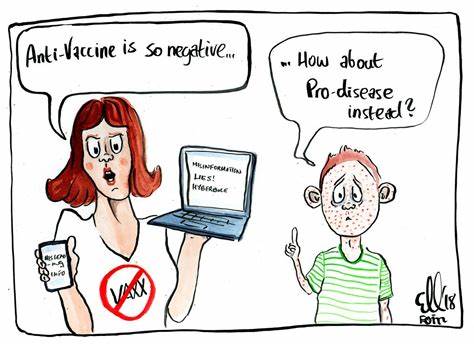
Numerous qualitative studies and a few quantitative studies have linked vaccine hesitancy or refusal with the belief in the efficacy of so-called alternative medicine (SCAM). Yet, large-scale data on this topic are scarce. In this study, the French researchers investigated the factors associated with the coverage rates of seven childhood vaccines or vaccine groups in the ninety-six metropolitan French departments. One of the factors investigated was the local interest in SCAM. In order to assess this interest, they built an Alternative Medicine Index based on departmental internet searches regarding SCAM—internet searches being a reliable indicator of the public’s actual interest in a given topic. They then conducted multiple regression analyses, which showed that this Index is a significant explanatory factor for the departmental variance in vaccination coverage rates, exceeding in importance the effect of other relevant local sociodemographic factors.
A further recent study from France adds to the picture. It presents the results of a survey conducted in July 2021 among a representative sample of the French mainland adult population (n = 3087). Using cluster analysis, the researchers identified five profiles of SCAM attitudes and found that even among the most pro-SCAM group, very few respondents disagreed with the idea that SCAM should only be used as a complement to conventional medicine. They then compared these SCAM attitudes to vaccine attitudes. Attitudes to SCAM had a distinct impact as well as a combined effect on attitudes to different vaccines and vaccines in general. They found that:
- attitudes to SCAM provide a very limited explanation of vaccine hesitancy;
- among the hesitant, pro-SCAM attitudes are often combined with other traits associated with vaccine hesitancy such as distrust of health agencies, radical political preferences, and low income.
Both SCAM endorsement and vaccine hesitancy are more prevalent among the socially disadvantaged. Drawing on these results, the researchers argue that, to better understand the relationship between SCAM and vaccine hesitancy, it is necessary to look at how both can reflect a lack of access and recourse to mainstream medicine and distrust of public institutions.
 The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
The fact that the enthusiasm for SCAM is associated with vaccine hesitancy has been discussed on this blog many times before, e.g.:
- Preference of so-called alternative medicine predicts negative attitudes to vaccination
- What are the reasons for opposing COVID vaccinations?
- Intelligence, Religiosity, SCAM, Vaccination Hesitancy – are there links?
- More information on homeopaths’ and anthroposophic doctors’ attitude towards vaccinations
- The anti-vaccination movement is financed by the dietary supplement industry
- Sorry, I was wrong about homeopathy and vaccination
- The UK Society of Homeopaths, a hub of anti-vaccination activists?
- HOMEOPATHY = “the complete alternative to vaccination” ?!?!
- Are anthroposophy-enthusiasts for or against vaccinations?
- Far too many chiropractors believe that vaccinations do not have a positive effect on public health
- Naturopaths’ counselling against vaccinations could be criminally negligent
- HOMEOPATHS AGAINST VACCINATION: “The decision to vaccinate and how you implement that decision is yours and yours alone”
- Use of alternative medicine is associated with low vaccination rates
- Integrative medicine physicians tend to harbour anti-vaccination views
- Vaccination: chiropractors “espouse views which aren’t evidence based”
What seems fairly clear to me is that a cross-correlation exists: an attitude against modern medicine and the ‘scientific establishment’ determines both the enthusiasm for SCAM and the aversion to vaccination. What is, however, far from clear to me is what we could do about it.
Yes, better education seems important – and that’s precisely what I aim at achieving with this blog. Sadly, judging from some of the comments we receive, it does not seem crowned with much success.
Any other ideas?
Menopausal symptoms are systemic symptoms that are associated with estrogen deficiency after menopause. Although widely practiced, homeopathy remains under-researched in menopausal syndrome in terms of quality evidence, especially in randomized trials. The efficacy of individualized homeopathic medicines (IHMs) was evaluated in this double-blind, randomized, placebo-controlled trial in the treatment of the menopausal syndrome.
Group 1 (n = 30) received IHMs plus concomitant care, while group 2 (n = 30) had placebos plus concomitant care. The primary outcome measures were the Greene Climacteric Scale (GCS) total score and the menopause rating scale (MRS) total score. The secondary endpoint was the Utian quality of life (UQOL) total score. Measurements were taken at baseline and every month up to 3 months.
Intention-to-treat sample (n = 60) was analyzed. Group differences were examined by two-way (split-half) repeated-measure analysis of variance, primarily taking into account all the estimates measured at monthly intervals, and secondarily, by unpaired t-tests comparing the estimates obtained individually every month. The level of significance was set at p < 0.025 two-tailed. Between-group differences were nonsignificant statistically—GCS total score (F1, 58 = 1.372, p = 0.246), MRS total score (F1, 58 = 0.720, p = 0.4), and UQOL total scores (F1, 58 = 2.903, p = 0.094). Some of the subscales preferred IHMs significantly against placebos—for example, MRS somatic subscale (F1, 56 = 0.466, p < 0.001), UQOL occupational subscale (F1, 58 = 4.865, p = 0.031), and UQOL health subscale (F1, 58 = 4.971, p = 0.030). Sulfur and Sepia succus were the most frequently prescribed medicines. No harm or serious adverse events were reported from either group.
The authors concluded that, although the primary analysis failed to demonstrate clearly that the treatment was effective beyond placebo, some significant benefits of IHMs over placebo could still be detected in some of the subscales in the secondary analysis.
The article was published in the recently re-named JICM, a journal that, when it was still called JCAM, featured regularly on this blog. As such, the paper is remarkable: who would have thought that this journal might publish a trial of homeopathy with a squarely negative result?
Yes, I know, the surprise is tempered by the fact that the authors make much in the conclusions of their article about the significant findings related to secondary analyses. Should we tell them that these results are all but irrelevant?
Better not!
It has been reported, at the German Medical Congress (DÄT) a year ago, that it was decided to delete the additional title of homeopathy from the model further training regulations of the German Medical Association. And Federal Health Minister Karl Lauterbach (SPD) tweeted applause: “Homeopathy has no place in modern medicine.”
Now the ‘ Bundesverband der Pharmaziestudierenden in Deutschland’ (BPhD), the German Pharmacists Organization, even goes a few steps further. The position paper distinguishes between evidence-based medicine (EBM) and unproven therapeutic methods. According to the BPhD, these include homeopathy, but also anthroposophy, traditional Chinese medicine, and traditional medicines.
Among other things, the BPhD is disturbed by the way homeopathy presents itself as an alternative, because an alternative means “a choice between two equally suitable possibilities” to achieve a goal, and this is not the case. Compared to evidence-based medicine (EBM), homeopathy is a “constructed, illusory concept” and “the principles of homeopathic teachings and principles” are to be rejected as “unscientific”. According to the BPhD, a designation as “alternative” for advertising purposes should no longer be allowed.
They would also like to see a demarcation from naturopathy; the clear distinction between homeopathy and phytopharmacy has been lacking up to now. The advertising attribute “natural” should therefore also be banned in order to prevent equalization in advertising, the position paper states.
Like doctors, pharmacy students point to the lack of proof of efficacy beyond the placebo effect. According to the BPhD, the dogma WER HEILT HAT RECHT, “he who heals is right” would “disregard all processes that work towards healing and glorify the result”. The “gold standard” of EBM – randomized, double-blind studies with placebo control – should in future also have to be fulfilled by homeopathic medicines, experience reports are not sufficient, it continues.
Homeopathic medicines are only registered as medicinal products without indication, which requires neither proof of efficacy nor clinical studies. The BPhD, therefore, demands that a warning be placed on the preparations that they have “no proven efficacy beyond the placebo effect”. Up to now, without this warning, patients have been “deceived about the efficacy”, and there is an “urgent need for detailed public information and counseling on homeopathy since its unjustified reputation poses a danger of not seeking treatment”. The BPhD also demands that the status of homeopathic medicines is withdrawn and that the pharmacy obligation for the preparations is abolished…
“In the health professions, no trivialization of unproven therapeutic procedures should be tolerated, as inadequate counseling or ignorance poses a danger to patients,” the BPhD said.
_________________________
When I first read this article – I translated and shortened it for those who cannot read German- I was truly dazzled. These are the suggestions that I have been making for around 20 years now, not specifically for Germany but for pharmacists in general. For many years, the Germans seemed the least likely to agree with me. But now they seem to be ahead of everyone else in Europe!
How come?
I suspect and hope that our recent initiative might have something to do with it.
Let’s hope that the pharmacists of other countries follow the German example.
‘Spagyric’ is a so-called alternative medicine (SCAM) based on the alchemy of Paracelsus (1493-1541). Paracelsus borrowed the term from “separate” (spao) and “combine” (ageiro) to indicate that spagyric preparations are based on the “separation”, “extraction” and “recombination” of the active ingredients of a substance. Plant, mineral as well as animal source materials are used.
The production of spagyric remedies is based on a complex process of maceration and fermentation of a plant extract in alcohol. It takes place in dark, thick-walled glass flasks that are hermetically sealed and kept at a controlled temperature of 37 °C for 28 days. The tincture thus obtained is then decanted and the drug residue is removed from the solution, completely dried, and burned to ash to recover the inorganic components of the plant material. The ash is subsequently dissolved in the alcoholic solution of maceration, and the finished spagyric preparation is left for 12 days before use.
Spagyric is not the most popular of all SCAMs but it certainly does have a significant following. One enthusiast claims that “spagyric essences work on a vibrational level in their action upon the emotional/mind and physical spheres and can be employed in numerous situations. Most people seek help to relieve physical symptoms. Even so, it is often necessary to address the emotional and psychological aspects which may predispose the illness or imbalance. In an era where many people are experiencing life-changing events, the ability to transition smoothly is essential for well-being and vitality. Guidance and help are required to maintain homeostasis. These medicines can help the patient to understand the root cause of their illness and learn to regain control of their lives. Some medicine systems appear to be less effective than in previous times. It has been suggested that the energetic frequency of both the earth and human organism are changing. Therefore these systems may no longer be a vibrational match for the changing frequencies. Spagyric Medicine is designed to ‘tune in with’ these current frequencies. Research suggests that the Spagyric essences may instigate improved health by energetically influencing DNA.”
After reading such weird statements, I ask myself, is there any evidence that spagyric remedies work? In my search for robust studies, I was unsuccessful. There does not seem to be a single controlled study on the subject. However, there are fragmentary reports of a study initiated and conducted by a now largely unknown healer named Karl Hann von Weyhern.
Von Weyhern (1882 – 1954) had taken a few semesters of pharmacy and medicine in Freiburg but remained without a degree. In 1930, he became a member of the NSDAP (Hitler’s Nazi party) and in 1940 he joined the SS. Around 1935, he settled in Munich as a non-medical practitioner (Heilpraktiker), and Heinrich Himmler who has a soft spot for SCAM enlisted as one of his patients. By then von Weyhern had by then made a steep career in the Nazi hierarchy, and he managed to convince Himmler that his spagyric remedies could cure tuberculosis, which was still rampant at the time. They decided to carry out experiments in this regard in the Dachau concentration camp.
Thus, von Weyhern was allowed to test spagyric remedies on forcibly recruited concentration camp prisoners. These experiments lasted for about one year and included around 150 patients who, according to von Weyhern’s iridology diagnosis, suffered from tuberculosis. Half of them were treated with spagyric remedies and the others with conventional treatments. At the end of the experiment, 27 persons were reportedly released into everyday concentration camp life as ‘fit for work’. How many of the 150 prisoners lost their lives due to these experiments is not known. Von Weyhern never filed a final report. It is to be feared that the death toll was considerable. [1]
After the war, von Weyhern denied belonging to the SS, claimed that he had ‘sacrificed himself’ for his patients in the concentration camp, merely had to pay a fine, and was ‘denazified’ in 1948. Subsequently, he resumed his work as a ‘Heilpraktiker’ in Olching, a village near Dachau. [1]
Of course, these infamous experiments cannot be blamed on spagyric medicine. Yet, I feel they are nevertheless important, not least because they seem to reveal the only thing remotely resembling something like evidence.
[1] Die Ärzte der Nazi-Führer: Karrieren und Netzwerke : Mathias Schmidt (Hg.), Dominik Groß (Hg.), Jens Westemeier (Hg.): Amazon.de: BooksHow often do we hear that chiropractic is safe because numerous trials reported no adverse events? This systematic review tested whether there has been a change in the reporting of adverse events associated with spinal manipulation in randomized clinical trials (RCTs) since 2016.
Databases were searched from March 2016 to May 2022: MEDLINE (Ovid), Embase, CINAHL, ICL, PEDro, and Cochrane Library. Domains of interest (pertaining to adverse events) included: completeness and location of reporting; nomenclature and description; spinal location and practitioner delivering manipulation; methodological quality of the studies and details of the publishing journal. Frequencies and proportions of studies reporting on each of these domains were calculated. Univariable and multivariable logistic regression models were fitted to examine the effect of potential predictors on the likelihood of studies reporting on adverse events.
5399 records were identified by the electronic searches, of which 154 (2.9%) were included in the analysis. Of these, 94 (61.0%) reported adverse events with only 23.4% providing an explicit description of what constituted an adverse event. Reporting of adverse events in the abstract has increased (n=29, 30.9%) while reporting in the results section has decreased (n=83, 88.3%) over the past 6 years. Spinal manipulation was delivered to 7518 participants in the included studies. No serious adverse events were reported in any of these studies.
The authors concluded as follows: while the current level of reporting of adverse events associated with spinal manipulation in RCTs has increased since our 2016 publication on the same topic, the level remains low and inconsistent with established standards. As such, it is imperative for authors, journal editors and administrators of clinical trial registries to ensure there is more balanced reporting of both benefits and harms in RCTs involving spinal manipulation.
This article is clearly relevant to our discussions about adverse events after spinal manipulation. However, I find it far too uncritical. This might be due to the affiliations of some of the authors:
- Integrative Spinal Research Group, Department of Chiropractic Medicine, University Hospital Balgrist and University of Zurich, Zurich, Switzerland.
- Department of Chiropractic, Faculty of Medicine, Health and Human Sciences, Macquarie University, Sydney, New South Wales, Australia.
Interestingly, the authors stated that they have no conflict of interest. Also interesting is the fact that they do not cite our paper from 2012. I, therefore, take the liberty of doing it:
Objective: To systematically review the reporting of adverse effects in clinical trials of chiropractic manipulation.
Data sources: Six databases were searched from 2000 to July 2011. Randomised clinical trials (RCTs) were considered, if they tested chiropractic manipulations against any control intervention in human patients suffering from any type of clinical condition. The selection of studies, data extraction, and validation were performed independently by two reviewers.
Results: Sixty RCTs had been published. Twenty-nine RCTs did not mention adverse effects at all. Sixteen RCTs reported that no adverse effects had occurred. Complete information on incidence, severity, duration, frequency and method of reporting of adverse effects was included in only one RCT. Conflicts of interests were not mentioned by the majority of authors.
Conclusions: Adverse effects are poorly reported in recent RCTs of chiropractic manipulations.
In percentage terms the results are similar. What is very different is that the authors of the new paper merely lament that the level remains low and inconsistent with established standards, while we make it clear in the abstract that adverse effect reporting is poor and in the paper identify this deficit as a violation against research ethics and thus as a form of scientific misconduct.
In view of all this, let me re-phrase the last sentence of the authors’ conclusion:
it is imperative for authors, journal editors, and administrators of clinical trial registries to ensure that researchers adhere to accepted ethical standards and that scientific misconduct no longer gets published.
Following the death from cancer of a 14-year-old Carinthian girl, the Klagenfurt public prosecutor’s office has launched an investigation against the girl’s parents. In February this year, the 14-year-old was taken to a hospital in Graz, Austria, where she died a few days later from cancer. The hospital filed charges because the tumor had been treated incorrectly with so-called alternative medicine (SCAM).
Investigations are underway on suspicion of torturing or neglecting underage, younger, or defenseless persons. Currently, the accused and witnesses are being questioned. The parents’ lawyer, Alexander Todor-Kostic, stated that the accusations were without any basis and claimed that the 14-year-old girl had decided of her own free will against being treated with chemotherapy and surgery. The parents respected this, allowed her alternative treatment methods, and acted in accordance with the applicable legal situation.
The girl had developed cancer the previous year that was not detected. Instead of seeing conventional oncologists for a reliable diagnosis and effective treatments, the parents consulted private doctors. Instead of chemotherapy, radiation, and surgery, the girl had deliberately chosen “alternative treatments” herself, the lawyer stressed.
Even though the case has been reported in several Austrian papers, I did not succeed in finding further details about it. In particular, it is unclear what type of cancer the girl had been suffering from and what type of SCAMs she received.
The Austrian skeptic Christian Kreil commented: “Sugar pills in the pharmacies, homeopathic advanced training for doctors, a proliferation of energetics offering every conceivable bullshit … the dead girl is the logical result of this esoteric foolishness covered by politics and chambers.”
I am afraid that he might have a point here: as we have discussed repeatedly on this blog, Austria is currently particularly prone to misinformation about SCAM. Here are a few examples of previous blog posts on this subject:
- Austrian osteopaths seem to violate legal, ethical and moral rules and conventions
- An open letter to the President of the Austrian Medical Association aims to stop medical quackery
- Has the ‘Vienna Medical Association’ taken leave of its senses?
- When politicians become snake-oil salesmen
- Michael Frass’ research into homeopathy for cancer: “numerous breaches of scientific integrity”
- A well-known opponent of vaccination has died of COVID after self-treatment with MMS
- The case of a boy tortured to death with homeopathy
- A truly perplexing homeopath – is it time for an official investigation?
Misinformation about SCAM can be lethal. This is one of the reasons why responsible information is so very important.
Seventeen years after S.K. lost his thyroid gland to cancer, he was promised a miracle by Kyung Chun Oh, an acupuncturist based in the Toronto area: acupuncture could regrow the vital organ. Oh told his patient it would only work if S.K. stopped the thyroid medication he’d been on since his surgery in 2003.
Within just a few months the patient had to be admitted to hospital with a life-threatening case of hypothyroidism. His thyroid had not regenerated. “It was fortunate that the patient did not die,” a college panel wrote in a disciplinary decision, suspending Oh’s license for 12 months. “Telling the patient that he should not take his thyroid medication was irresponsible and had disastrous repercussions.”
The panel found that Oh had engaged in professional misconduct in multiple ways:
- he had provided unnecessary treatment,
- he had failed to advise his patient to consult a medical doctor when he learned that S.K. was suffering
from symptoms that he knew or ought to have known indicated an urgent medical problem, - he had treated a condition that he ought to have known that he did not have the knowledge, skills, or judgment to treat,
- he had failed to keep records in accordance with the standards of the profession,
- he had falsified a record relating to his practice,
- he had made a claim about a treatment that could not be supported by reasonable professional opinion (the claim that acupuncture combined with cessation of thyroid medicine could regrow a surgically removed thyroid gland, and the claim that S.K.’s thyroid gland was regrowing).
This is clearly an extreme incidence of misconduct and one would hope that such cases occur only rarely. But looking at the points listed above, I get the feeling that similar yet less severe cases of misconduct happen regularly in the practices of SCAM practitioners:
- most so-called alternative medicine (SCAM) treatments are unnecessary,
- SCAM practitioners refer patients only rarely to doctors,
- SCAM practitioners often treat conditions that they fail to understand adequately,
- SCAM practitioners frequently make unreasonable claims.
It is not only practitioners of so-called alternative medicine (SCAM) who can be fraudulent charlatans. The study of medicine does not protect you from joining in. Here is an impressive case in point:
It has been reported that a former doctor convicted of fraudulently submitting nearly $120 million in claims related to the 1-800-GET-THIN Lap-Band surgery business has been sentenced to seven years in federal prison.
Julian Omidi, 58, of West Hollywood was sentenced Monday by U.S. District Court Judge Dolly M. Gee. The judge also imposed a five-year probation period on Surgery Center Management LLC, an Omidi-controlled Beverly Hills-based company. In the coming weeks, Gee is expected to hold a separate hearing to decide on restitution and forfeiture in the case, along with setting a fine for the Beverly Hills company.
“Mr. Omidi made millions at the expense of the multiple victim companies he defrauded, and he violated his oath to ‘do no harm’ by callously misleading patients about the need for a sleep study and subsequent weight loss surgery,” said Donald Alway, the assistant director in charge of the FBI’s Los Angeles field office.
Omidi controlled several entities in the GET-THIN network. Prosecutors say Omidi incentivized employees to ensure patients underwent sleep studies and then falsified the results to show that patients had obstructive sleep apnea to help them qualify for insurance coverage for the weight loss surgery. Those results were then filed with insurance companies to pre-approve the Lap-Band weight-loss surgeries. The 1-800-GET-THIN business received approximately $41 million for those procedures, according to prosecutors. While not all patients were approved to receive the surgery, prosecutors say GET-THIN would bill the patient roughly $15,000 for each sleep study, totaling $27 million in payments from insurance providers.
Omidi and his Beverly Hills-based company, Surgery Center Management, were found guilty of 28 counts of wire fraud, three counts of mail fraud, and one count of conspiracy to commit money laundering. Omidi was also found guilty of two counts of making false statements relating to healthcare matters, one count of aggravated identity theft, and two counts of money laundering after a 48-day trial in downtown Los Angeles.
“As found by the jury, the defendant Julian Omidi deliberately and repeatedly acted with an eye towards business and profits, rather than in the interest of GET-THIN’s medical patients, by inducing patients to undergo medical treatment premised on fraud rather than medical necessity, including surgeries that carry significant risks and life-long health impacts,” said U.S. Atty. Martin Estrada. A series of Los Angeles Times columns from 2010 to 2014 detailed how five patients died after they received Lap-Band surgeries at clinics affiliated with 1-800-GET-THIN. During a 2009 inspection, the Department of Health and Human Services found unsanitary conditions, inoperative scrub sinks, one-time-only equipment being reused, and several other deficiencies. The inspector shut down the clinic for a day, but further action was not taken at the time.
Omidi’s medical license was revoked in 2009, and he was arrested. In 2014, federal agencies seized more than $110 million from the 1-800-GET-THIN network in securities and funds.
______________________________
This is a spectacular case, of course. Yet, I fail to see how it differs in principle from the many instances we see on a daily basis in the realm of SCAM. Let me give you just a few examples:
- A chiropractor diagnoses subluxation and subsequently treats his patient with a series of spinal manipulations.
- A naturopath uses iridology to diagnose a weakness of the liver and subsequently treats it with herbal remedies.
- An acupuncturist diagnoses a blockage of chi and follows it up with a series of acupuncture sessions.
- A Heilpraktiker employs bioresonance to diagnose an intoxication which he then treats with a detox program.
The strategy is always the same:
- Charlatans use bogus diagnostic methods.
- They make bogus diagnoses with them.
- They then start expensive and often dangerous treatments.
- They make good money by defrauding the system.
Could someone please explain what the difference in principle is between the case of the fraudulent surgeon and the average SCAM practitioner?
I came across an article entitled “Consent for Paediatric Chiropractic Treatment (Ages 0-16)“. Naturally, it interested me. Here is the full paper; I have only inserted a few numbers in square brackets which refer to my comments below:
By law, all Chiropractors are required to inform you of the risks and benefits of chiropractic spinal manipulation and the other types of care we provide. Chiropractors use manual therapy alongside taking a thorough history, and doing a neurological, orthopaedic and chiropractic examination to both diagnose and to treat spinal, cranial and extremity dysfunction. This may include taking joints to the end range of function, palpating soft tissues (including inside the mouth and the abdomen), mobilisation, soft tissue therapy and very gentle manipulation [1]. Our Chiropractors have been educated to perform highly specific types of bony or soft tissue manipulation and we strive to follow a system of evidence-based care [2]. At the core of our belief system is “Do No Harm”. We recognise that infants and children are not tiny adults. The force of an adjustment used in a child is at least less than half of what we might use with a fully grown adult. Studies by Hawk et al (2016) and Marchand (2013) agreed that Chiropractors use 15 – 35 x less force in the under 3-month age group when compared to medical practitioners doing manipulation (Koch, 2002) [3]. We also use less force in all other paediatrics groups, especially when compared to adults (Marchand, 2013). In addition to using lower force, depth, amplitude and speed in our chiropractic adjustments [4], we utilise different techniques. We expect all children under the age of 16 years to be accompanied by a responsible adult during appointments unless prior permission to treat without a consenting adult e.g., over the age of 14 has been discussed with the treating chiropractor.
Risks
- Research into chiropractic care for children in the past 70 years has shown it to have a low risk of adverse effects (Miller, 2019) [5]. These effects tend to be mild and of short duration e.g., muscular or ligament irritation. Vorhra et al (2007) found the risk of severe of adverse effects (e.g. fracture, quadriplegia, paraplegia, and death) is very, very rare and was more likely to occur in individuals where there is already serious underlying pathology and missed diagnosis by other medical profession [6]. These particular cases occurred more than 25 years ago and is practically unheard of now since research and evidence-based care has become the norm [7].
- The most common side effect in infants following chiropractic treatment includes fussiness or irritability for the first 24 hours, and sleeping longer than usual or more soundly. (Miller and Benfield, 2008) [8]
- In older children, especially if presenting with pain e.g., in the neck or lower back, the greatest risk is that this pain may increase during examination due to increasing the length of involved muscles or ligaments [9]. Similarly, the child may also experience pain, stiffness or irritability after treatment (Miller & Benfield, 2008) [10]. Occasionally children may experience a headache.[11] We find that children experience side effects much less often than adults.[12]
Benefits
- Your child might get better with chiropractic care. [13] If they don’t, we will refer you on [14].
- Low risk of side effects and very rare risk of serious adverse effects [15].
- Drug-free health care. We are not against medication, but we do not prescribe [16].
- Compared with a medical practitioner, manual therapy carried out by a chiropractor is 20 x less likely to result in injury (Koch et al 2002, Miller 2009).[17]
- Children do not often require long courses of treatment (>3 weeks) unless complicating factors are present.[18]
- Studies have shown that parents have a high satisfaction rate with Chiropractic care [19].
- Physical therapies are much less likely to interfere with biomedical treatments. (McCann & Newell 2006) [20]
- You will have a better understanding of diagnosis of any complain and we will let you know what you can do to help.[21]
We invite you to have open discussions and communication with your treating chiropractor at all times. Should you need any further clarification please just ask.
References
- Hawk, C. Shneider, M.J., Vallone, S and Hewitt, E.G. (2016) – Best practises recommendations for chiropractic care of children: A consensus update. JMPT, 39 (3), 158-168.
- Marchand, A. (2013) – A Proposed model with possible implications for safety and technique adaptations for chiropractic spinal manipulative therapy for infants and children. JMPT, 5, 1-14
- Koch L. E., Koch, H, Graumann-Brunnt, S. Stolle, D. Ramirez, J.M., & Saternus, K.S. (2002) – Heart rate changes in response to mild mechanical irritation of the high cervical cord region in infants. Forensic Science International, 128, 168-176
- Miller J (2019) – Evidence-Based Chiropractic Care for Infants: Rational, Therapies and Outcomes. Chapter 11: Safety of Chiropractic care for Infants p111. Praeclarus Press
- Vohra, S. Johnston, B.C. Cramer, K, Humphreys, K. (2007) – Adverse events associated with paediatric spinal manipulation: A Systematic Review. Pediatrics, 119 (1) e275-283
- Miller, J and Benfield (2008) – Adverse effects of spinal manipulative therapy in children younger than 3 years: a retrospective study in a chiropractic teaching clinic. JMPT Jul-Aug;31(6):419-23.
- McCann, L.J. & Newell, S.J. (2006). Survey of paediatric complementary and alternative medicine in health and chronic disease. Archives of Diseases of Childhood, 91, 173-174
- Corso, M., Cancelliere, C. , Mior., Taylor-Vaise, A. Côté, P. (2020) – The safety of spinal manipulative therapy in children under 10 years: a rapid review. Chiropractic Manual therapy 25: 12
___________________________________
- “taking joints to the end range of function” (range of motion, more likely) is arguably not “very gently”;
- “we strive to follow a system of evidence-based care”; I do not think that this is possible because pediatric chiropractic care is hardy evidence-based;
- as a generalizable statement, this seems to be not true;
- ” lower force, depth, amplitude and speed”; I am not sure that there is good evidence for that;
- research has foremost shown that there might be significant under-reporting;
- to blame the medical profession for diagnoses missed by chiropractors seems odd;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- possibly because of under-reporting;
- your impressions are not evidence;
- your child might get even better without chiropractic care;
- referral rates of chiropractors tend to be low;
- possibly because of under-reporting;
- chiropractors have no prescription rights but some lobby hard for it;
- irrelevant if we consider the intervention useless and thus obsolete;
- any evidence for this statement?;
- satisfaction rates are no substitute for real evidence;
- that does not mean they are effective, safe, or value for money;
- this is perhaps the strangest statement of them all – do chiropractors think they are the optimal diagnosticians for all complaints?
_____________________________________
According to its title, the paper was supposed to deal with consent for chiropractic pediatric care. It almost totally avoided the subject and certainly did not list the information chiropractors must give to parents before commencing treatment.
Considering the arguments that the article did provide has brought me to the conclusion that chiropractors who treat children are out of touch with reality and seem in danger of committing child abuse.
